Abstract
Background
Despite the increased fracture risk, bone mineral density (BMD) is variable in type 1 (T1D) and type 2 (T2D) diabetes mellitus. We aimed at comparing independent BMD predictors in T1D, T2D and control subjects, respectively.
Methods
Cross-sectional case-control study enrolling 30 T1D, 39 T2D and 69 age, sex and body mass index (BMI) – matched controls that underwent clinical examination, dual-energy X-ray absorptiometry (BMD at the lumbar spine and femoral neck) and serum determination of HbA1c and parameters of calcium and phosphate metabolism.
Results
T2D patients had similar BMD compared to T1D individuals (after adjusting for age, BMI and disease duration) and to matched controls, respectively. In multiple regression analysis, diabetes duration – but not HbA1c- negatively predicted femoral neck BMD in T1D (β= -0.39, p = 0.014), while BMI was a positive predictor for lumbar spine (β = 0.46, p = 0.006) and femoral neck BMD (β = 0.44, p = 0.007) in T2D, besides gender influence. Age negatively predicted BMD in controls, but not in patients with diabetes.
Conclusions
Long-standing diabetes and female gender particularly increase the risk for low bone mass in T1D. An increased body weight partially hinders BMD loss in T2D. The impact of age appears to be surpassed by that of other bone regulating factors in both T1D and T2D patients.
Similar content being viewed by others
Background
Diabetes mellitus is a chronic whole-body disease leading to a wide range of complications, such as cardiovascular disease, retinopathy, nephropathy, neuropathy and also “sweet bone” disease [1]. Although the underlying pathophysiological background is very different, type 1 (T1D) and type 2 diabetes (T2D) are both associated with an increased fracture risk - which is multifactorial and only partially explained by falls and bone mineral density (BMD) [2]. The most consistent effect is upon the hip fracture risk, ranging between 2.4- and 7-fold increase in T1D [3] and being two to three times higher in T2D compared to the general population [1].
Diabetic osteopathy in T1D and T2D is characterized by low serum vitamin D, negative calcium balance, low bone turnover and high sclerostin levels [4]. However, bone mass may differ to some extent in T1D when compared to T2D [5], but not in all studies [6]. Low BMD occurs early after disease onset due to the deleterious effects of insulinopenia upon bone turnover and bone mass accrual in T1D, remaining rather stable afterwards [7]. Reported BMD in T2D varies from unaltered bone density [8, 9] to a paradoxically higher BMD [5] compared to controls. Low bone mass was also found in the later stages of T2D, possibly linked to microvascular disease [10].
Skeletal fragility is nevertheless described in both T1D and T2D, independently of BMD [2]. Advanced glycation end products (AGEs) alter the structure of the collagen, promote oxidative stress and inflammation, and also contribute to low bone turnover [1, 3]. The effect of glycemic control - reflected by HbA1c levels - upon bone is inconsistent, with some studies reporting an elevated fracture risk with increasing HbA1c [11, 12], while bone density evolution appears rather independent of HbA1c levels [5, 6]. In T2D, the protective effect of an increased body weight and hyperinsulinemia upon bone are counterbalanced by the negative impact of increased visceral adiposity and insulin resistance, an inadequate adaptation of bone strength to increased mechanical load, the long duration of disease evolution and various anti-diabetic drugs (e.g., thiazolidinediones or sodium-glucose cotransporter type 2 inhibitors – SGLT-2) [1].
We aimed at investigating independent predictors of BMD in T1D and T2D patients compared to controls with regard to general and diabetes - specific parameters.
Methods
Study design and subjects
Patients diagnosed with diabetes (T1D and T2D) were consecutively recruited during routine follow-up visits for disease monitoring in the Diabetes, Nutrition and Metabolic Diseases Clinic of “Sf. Spiridon” Clinical Emergency Hospital Iasi (Romania) between January and December 2017. Patients aged between 18 and 80 years old were included if they had a well-established diagnosis of diabetes according to standardized criteria [13] in their original medical record (HbA1c > 6.5 % on two separate tests; T1D: new-onset hyperglycemia accompanied by ketonuria at debut, low serum levels of insulin and peptide C and requiring insulin treatment for control and survival - antibodies to glutamic acid decarboxylase were also tested where the clinical phenotype was rather non-specific, such as slow onset of symptoms, BMI ≥ 25 kg/m2 or age over 40 with normal BMI and requiring insulin treatment from the time of diagnosis [14]; T2D: two fasting blood sugar levels ≥ 126 mg/dl or an oral glucose tolerance test showing serum glucose ≥ 200 mg/dl accompanied by a phenotype of insulin resistance and not requiring insulin), were more than 1 year after disease onset, were receiving antidiabetic treatment (without any changes in medication type in the past six months), were at their first bone evaluation, and had an estimated glomerular filtration rate (eGFR) ≥ 60 ml/min/1.73 m2 (serum creatinine was measured and eGFR was calculated using the CKD-EPI equation). Age, sex and body mass index (BMI) 1:1 matched apparently healthy volunteer controls (CTL) referred by the general practitioner to the outpatient department in our hospital for general investigations were enrolled in the same period as the patients. Exclusion criteria for both groups were represented by calcium and vitamin D supplementation, bone active therapy (antiresorptive/bone-forming therapy), liver disease, moderate and severe chronic kidney disease (CKD; stage G3 to end-stage renal disease), history of parathyroid or rheumatological disease, oral corticosteroid use > 5 mg prednisone equivalent in the past 3 months or endogenous hypercortisolism, hypo- and hyperthyroidism, inflammatory bowel disease, hypogonadism (other than menopause), smoking (both regular and heavy) and heavy drinking (more than 2 drinks per day or more than 15 drinks per week for men and more than 1 drink per day or more than 8 drinks per week for women). Subjects exhibiting hyperglycemia (an abnormal fasting blood sugar, impaired glucose tolerance or diabetes) were further excluded from the CTL group.
Sixty-nine patients (30 T1D and 39 T2D) and 69 age, sex and BMI-matched CTL that were willing to participate and met the study inclusion and exclusion criteria were recruited in the Diabetes and Endocrinology outpatient clinics, after giving written informed consent and were enrolled in this cross-sectional case-control study. The study adhered to the Declaration of Helsinki and was approved by the institutional Ethics Committee.
Evaluation and measurements
Complete medical history (anamnesis and medical charts) was recorded for all patients and CTL. The presence of microvascular complications was defined as: [1] nephropathy: positive albumin:creatinine ratio (≥ 30 mg/g) on two or more occasions, [2] retinopathy: positive ophthalmologic fundus examination, [3] polineuropathy: clinical measurement of vibration. Macrovascular complications were defined based on the recorded history of coronary heart disease, stroke, myocardial infarction, or peripheral vascular disease, respectively.
After clinical examination (height and weight were recorded and BMI was calculated as weight (kg) divided by square height (m)), all patients underwent dual-energy X-ray absorptiometry (DXA; Hologic Delphi A, software version 12.7.3.2 Hologic Inc., USA) scanning to measure BMD at the lumbar spine and hip (femoral neck was reported due to lower values compared to total hip, according to the recommendations of the ISCD [15]). Coefficient of variation was 0.39 % for lumbar anterior-posterior spine and 1 % for femoral neck BMD. Measurements were made by two trained technicians certified by the International Society for Clinical Densitometry (ISCD), according to standard protocol and with daily calibration. Least significant change (LSC) was 0.008 g/cm2 for lumbar BMD and 0.0104 g/cm2 for femoral neck BMD, respectively. According to the Adult Official Positions of the ISCD [15], T-scores were reported for postmenopausal women and men ≥ 50 years of age (“low bone mass” was defined as T-score <-1 in this category) while Z-scores were recorded for premenopausal women and men < 50 years (“low bone mass” was defined as Z-score ≤-2). Also, if there was a more than 1.0 T-score difference between adjacent vertebrae, the questioned vertebra was excluded from the analysis, while the BMD of the remaining vertebrae was used to derive T-score [15]. Menopause was defined as more than 12 months since natural cessation of menstrual cycles.
On the same day as the clinical and DXA examinations, blood samples were collected after overnight fasting in all study participants. Biochemical analysis of standard clinical parameters included HbA1c determination (ion-exchange high-performance liquid chromatography (HPLC) method), serum calcium and phosphate (colorimetry; Cobas 6000 analyzer, Roche), serum thyroid stimulating hormone (TSH) and parathyroid hormone (PTH) (intact PTH second-generation chemiluminescent enzyme immunometric assay; Immulite 2000 Immunoassay System, Siemens).
Statistical analysis
SPSS (SPSS Statistics version 20.0 for Windows) was employed for statistical analysis. Data are expressed as mean ± SEM (standard error of the mean). Comparisons between groups (T1D versus T2D, T1D versus controls and T2D versus controls, respectively) were made using Student’s t-test (for normally distributed data) or the non-parametric Mann-Whitney U test (for skewed data), after checking for normal distribution (Shapiro-Wilk test). Analysis of variance (ANOVA) was employed for comparisons between 3 or more categories. The analysis of covariance (ANCOVA) was used to calculate age, BMI and diabetes duration - adjusted BMD values in T1D compared to T2D (least square means ± standard error are reported). Multiple regression analysis was performed to assess independent predictors of bone mass in T1D, T2D and matched-CTL, respectively, as follows: continuous variables potentially influencing BMD variation, such as age, diabetes duration, HbA1c, BMI and PTH, as well as categorical variables (introduced after binary coding 0/1), such as gender (male = 0, female = 1) were introduced as independent variables in regression models with lumbar BMD and femoral neck BMD as the outcome variables, respectively. The level of significance was established for p-value < 0.05.
Results
Despite being younger and having a mean BMI within the normal reference range, T1D patients had a longer duration of diabetes and a poor glycemic control with more diabetes complications compared to the older, rather obese but with improved glycemic control T2D patients (Table 1). Serum calcium, phosphate, PTH and thyroid status were similar between T1D and T2D patients, although serum PTH had the tendency to be higher in T2D subjects (Table 1). All T1D patients were receiving exogenous insulin treatment, while all T2D patients were under metformin treatment: 16 were following metformin monotherapy, 13 were taking metformin together with a sulfonylurea drug and 10 associated incretin therapy to metformin (none were using thiazolidinediones or sodium-glucose co-transporter-2 inhibitors).
BMD values at the lumbar spine and femoral neck were similar between T1D and T2D patients, and also between T1D patients and controls and between T2D patients and controls, in the whole group and according to sex, respectively (Table 2). After adjusting for age, BMI and disease duration, BMD did not vary significantly between T1D and T2D patients, respectively (Table 2). However, fewer patients in the T2D group exhibited low bone mass compared to matched controls, while the number of low bone mass subjects was similar in T1D patients and matched controls (Table 2).
BMD predictors in T1D, T2D and controls
General (age, gender, BMI and PTH) and diabetes - specific parameters (disease duration, HbA1c) were introduced as independent variables in multiple regression analysis with lumbar and femoral neck BMD as outcome variables, respectively (Table 3). Gender independently predicted BMD across all models: compared to men, female sex was an independent risk factor for low BMD in T1D, T2D patients and controls, respectively. In T1D patients, diabetes duration was also a negative independent predictor of femoral neck BMD, while BMI was a positive independent predictor of both lumbar and femoral neck BMD in the T2D group - but not in controls. Age was a negative independent predictor of BMD in controls (both T1D and T2D controls), but not in patients with diabetes (Table 3).
Subgroup analysis
The presence of diabetic complications
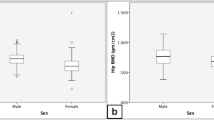
T1D patients with diabetes complications (n = 12) had similar lumbar BMD values compared to T1D patients without complications (n = 18) and controls (n = 30), respectively (p = 0.47); however, they tended to have a rather lower femoral neck BMD, but the differences did not reach statistical significance (0.764 g/cm2 in T1D patients with complications versus 0.858 g/cm2 in T1D patients without complications versus 0.829 g/cm2 in matched controls, respectively, p = 0.21). More so, T1D patients with diabetes complications had longer disease duration (20.5 ± 3.3 versus 10.1 ± 1.68 years, p = 0.012) compared to T1D patients without complications, despite similar HbA1c and BMI (data not shown). BMD did not differ significantly between T2D patients with (n = 9) and without (n = 30) complications and controls (n = 39), respectively (Fig. 1).
BMD values according to the presence of complications in type 1 and type 2 diabetes patients compared to controls. BMD = bone mineral density, T1D = type 1 diabetes mellitus, T2D = type 2 diabetes mellitus. T1D patients with complications – n = 12, T1D patients without complications – n = 18, T2D patients with complications – n = 9, T2D patients without complications – n = 30, T1D controls – n = 30, T2D controls – n = 39
Drugs in T2D
In the T2D group, we compared BMD across different treatment categories. Although patients taking metformin + sulfonylurea tended to have a rather lower bone density compared to the other subgroups, lumbar BMD (1.03 ± 0.05 versus 0.95 ± 0.05 versus 1.04 ± 0.04, p = 0.42) and femoral neck BMD (0.84 ± 0.04 versus 0.8 ± 0.05 versus 0.86 ± 0.04, respectively) did not differ significantly among metformin monotherapy (n = 16), metformin + sulfonylurea (n = 13) and metformin + incretin therapy (n = 10), respectively.
Discussion
T1D and T2D patients had similar BMD compared to controls, respectively. Diabetes duration, but not HbA1c, was found to negatively predict femoral neck BMD in T1D, but not T2D patients. In the T2D group, BMI was an independent predictor of bone density, while female gender was negatively associated with low BMD in both T1D and T2D, independently of other factors. Unlike patients with diabetes, age was the other major independent predictor of bone mass in controls, in addition to gender.
Albeit BMD underestimates fracture risk in patients with diabetes, it still remains the cornerstone in bone evaluation in this particular group due to high accessibility and low costs [16]. Data reporting BMD values in T1D and T2D patients are very heterogenous and rather inconsistent with regard to BMD predictive factors.
An older meta-analysis [5] reported negative Z-scores for T1D patients and positive Z-scores for T2D subjects, thus concluding that T1D is associated with lower bone mass, while T2D patients generally have higher BMD. More recent studies reported, however, similar BMD values both between patients with diabetes and controls and between T1D and T2D patients, respectively [6, 17]. Another recent study performed investigating bone mass in long-standing (longer than 50 years) T1D patients with good glycemic control and low rates of vascular complications reported similar or even better BMD expressed as Z-score compared to age-, gender- and race-matched population [18]. We found lower bone mass scores at the femoral neck in T1D women compared to T2D women and controls; nevertheless, the differences did not reach statistical significance, probably due to the limited number of patients. Also, more women in the T2D group were postmenopausal compared to the T1D group, and this may account for the lack of a statistical difference regarding BMD between types of diabetes. More so, the different stages of evolution and disease management captured in various studies, the potentially erroneous diabetes classification and also the adjustment for various confounding variables may account for the variability of reported data. The early and rather acute insulinopenia associated with diabetes onset impairs bone mass accrual and negatively impacts peak bone mass. Thus, bone mass acquisition is hampered in the early stages of T1D [3]. Nonetheless, bone density was demonstrated to stabilize or even increase after exogenous insulin treatment is well installed, with studies reporting age – and gender - expected bone density measurements [19]. More so, T1D patients with low bone mass are reported to follow lower insulin dose regimens compared to those with normal bone mass [20].
Disease duration - and not age – proved to be one of the main independent predictors of low femoral neck BMD in T1D patients in our study, suggesting that diabetes-related factors, such as diabetes duration, may be more important for bone. Indeed, T1D patients experiencing diabetes-specific complications had a longer disease history and also the tendency towards lower femoral neck BMD. Low rates of vascular complications have been linked to preserved BMD in long-lasting T1D [18]. According to recent consensus in the field, diabetes-specific risk factors for fracture include age, low BMD, the presence of complications of diabetes, disease duration, previous fractures and glycemic control (particularly in T1D with HbA1c > 8–9 %) [21]. Our results are in agreement with other studies reporting long-lasting disease as a risk factor for fragility fractures [11, 22]. The presence of micro- and macrovascular complications is associated with low BMD [5, 6] and was also reported to increase fracture risk [22, 23]. Microvascular complications as a result of collagen glycation and impaired bone turnover due to AGEs are thought to compromise bone quality and material properties, thereby significantly increasing fracture risk [2, 24, 25]. Although we and others [26] failed to find any significant BMD variation according to the presence of complications, microvascular damage is demonstrated to alter bone microarchitecture, possibly via VEGF linking diabetic complications and skeletal health. This explains the disproportionate fracture risk in T1D versus T2D, compared to differences in BMD [27]. Complications are also associated with longer disease history, an independent factor for low BMD, once again supporting the link between bone mass and microarchitecture changes and the long exposure to diabetic milieu. Similar to other studies [6, 20], we failed to find a significant effect of HbA1c (which shows only the severity of recent diabetes dysregulation) upon BMD. However, we did not assess fracture risk, as long standing poor glycemic control is known to be associated with increased fracture risk, independently of bone mass [20].
T2D patients in the current study had similar BMD compared to matched controls, although fewer patients in the diabetes group exhibited low bone mass. T2D patients are generally reported to have increased BMD compared to reference populations, although not in all studies [5, 28]. Potential disease misclassification, lack of a matched control group and inability to adjust for covariates are important sources of bias and heterogeneity [28]. Diabetes duration is an important confounder: the osteoanabolic effects of the hyperinsulinemia secondary to insulin resistance may explain the apparently higher bone density in early T2D, while insulinopenia in T1D and late T2D is accompanied by sarcopenia and low bone mass [1]. Despite using metformin which is known to positively impact bone mass and reduce fracture risk [29, 30], the T2D patients in the current study had a rather long disease history of approximately 10 years, with one quarter also experiencing complications. A diabetes duration longer than 5 years is a risk factor for low bone mass [31] and the presence of microvascular complications in T2D is associated with lower cortical volumetric BMD and altered bone microarchitecture, namely increased cortical porosity and diminished cortical thickness at the radius [32]. BMD did not differ in patients with complicated T2D compared to T2D patients without complications in the current study. At the same time, our T2D patients had a good glycemic control, while an increased HbA1c is associated with increased BMD according to the meta-analysis of Ma et al.[28]. Other meta-analyses failed to find a significant correlation of HbA1c with BMD in T2D [5]. Also, BMD progressively increases with clinical cutoffs for fasting glucose (normal, impaired and overt T2D) [33]. However, this increased BMD may be explained by the diminished bone mineral area of these patients, which also exhibit low bone turnover as assessed by serum markers, such as osteocalcin or cross-laps [33].
An increased BMI is a protective factor against osteoporosis in all populations [34] (including patients with diabetes [34]), via the increased mechanical loading. Obesity is a risk factor for insulin resistance and diabetes [35], being at the same time associated with higher areal and volumetric BMD and improved cortical bone structure [1, 35]. It also contributes to higher BMD in T2D patients, as demonstrated by the current study and also by many others [28]. At the same time, diabetes and obesity are associated with systemic inflammation and adipokine dysregulation, all contributing to impaired bone metabolism [36]. Despite variable BMD, alterations in cortical bone microarchitecture are reported in T2D patients, explaining the higher fracture risk compared to the reference population [37].
None of the patients in our study were under anti-diabetic therapy known to negatively impact bone mass, such as thiazolidinediones or SGLT-2 inhibitors. While all T2D patients were using the “bone-friendly” metformin, the subgroup also using a sulfonylurea drug tended to have a rather lower BMD, without reaching statistical significance. This is still to be clarified as the mechanisms of action of the sulfonylurea class of medication upon bone remain unelucidated up to present [38].
Age and gender (female sex was associated with a lower BMD compared to men, independently of other factors) were the main independent BMD predictors in the reference populations in our study. Interestingly, the effect of age, unanimously recognized as a risk factor for low bone mass, was not detected in the T1D and T2D patients in our study. It is possible that other factors surpass the effect of aging upon BMD in diabetes, particularly in young or obese patients.
Our study is limited by the relatively small number of patients, lack of assessment of bone microarchitecture, bone turnover markers or fracture risk. The effect of vitamin D levels, known to be altered in individuals with diabetes [4], was also not assessed. Nonetheless, the presence of matched control groups for T1D and T2D subjects, respectively, together with the evaluation of BMD predictors in patients with diabetes versus matched healthy individuals are important study strengths.
Conclusions
Female sex and long-standing diabetes particularly increase the risk for low BMD in T1D, with special concern for the femoral neck. An increased BMI partially contributes to BMD preservation in T2D, independently of age; however, appreciating bone mass to its real extent is rather difficult in T2D due to various contributing factors to bone changes.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AGEs:
-
Advanced glycation end products
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CKD:
-
Chronic kidney disease
- CTL:
-
Control group
- DXA:
-
Dual energy X-ray absorptiometry
- eGFR:
-
Estimated glomerular filtration rate
- ISCD:
-
International Society for Clinical Densitometry.
- PTH:
-
Parathyroid hormone.
- SGLT2:
-
Sodium-glucose co-transporter-2.
- T1D:
-
Type 1 diabetes mellitus.
- T2D:
-
Type 2 diabetes mellitus.
- TSH:
-
Thyroid stimulating hormone.
References
Shanbhogue V V., Mitchell DM, Rosen CJ, Bouxsein ML. Type 2 diabetes and the skeleton: New insights into sweet bones. The Lancet Diabetes and Endocrinology. 2016;4:159–73. https://doi.org/10.1016/S2213-8587(15)00283-1.
Lekkala S, Taylor EA, Hunt HB, Donnelly E. Effects of Diabetes on Bone Material Properties. Current Osteoporosis Reports. 2019;17:455–64. https://doi.org/10.1007/s11914-019-00538-6.
Starup-Linde J, Hygum K, Harsløf T, Langdahl B. Type 1 diabetes and bone fragility: Links and risks. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2019;12:2539–47. https://doi.org/10.2147/DMSO.S191091.
Wongdee K, Krishnamra N, Charoenphandhu N. Derangement of calcium metabolism in diabetes mellitus: negative outcome from the synergy between impaired bone turnover and intestinal calcium absorption. Journal of Physiological Sciences. 2017;67:71–81. https://doi.org/10.1007/s12576-016-0487-7.
Vestergaard P. Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes - A meta-analysis. Osteoporos Int. 2007;18:427–44. https://doi.org/10.1007/s00198-006-0253-4.
Leidig-Bruckner G, Grobholz S, Bruckner T, Scheidt-Nave C, Nawroth P, Schneider JG. Prevalence and determinants of osteoporosis in patients with type 1 and type 2 diabetes mellitus. BMC Endocr Disord. 2014;14. https://doi.org/10.1186/1472-6823-14-33.
Starup-Linde J, Lykkeboe S, Gregersen S, Hauge EM, Langdahl BL, Handberg A, et al. Bone structure and predictors of fracture in type 1 and type 2 diabetes. J Clin Endocrinol Metab. 2016;101:928–36. https://doi.org/10.1210/jc.2015-3882.
Asokan AG, Jaganathan J, Philip R, Soman RR, Sebastian ST, Pullishery F. Evaluation of bone mineral density among type 2 diabetes mellitus patients in South Karnataka. J Nat Sci Biol Med. 2017;8:94–8. https://doi.org/10.4103/0976-9668.198363.
Agius R, Galea R, Fava S. Bone mineral density and intervertebral disc height in type 2 diabetes. J Diabetes Complications. 2016;30:644–50. https://doi.org/10.1016/j.jdiacomp.2016.01.021.
Viégas M, Costa C, Lopes A, Griz L, Medeiro MA, Bandeira F. Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J Diabetes Complications. 2011;25:216–21. https://doi.org/10.1016/j.jdiacomp.2011.02.004.
Leanza G, Maddaloni E, Pitocco D, Conte C, Palermo A, Maurizi AR, et al. Risk factors for fragility fractures in type 1 diabetes. Bone. 2019;125:194–9. https://doi.org/10.1016/j.bone.2019.04.017.
Li C-I, Liu C-S, Lin W-Y, Meng N-H, Chen C-C, Yang S-Y, et al. Glycated Hemoglobin Level and Risk of Hip Fracture in Older People with Type 2 Diabetes: A Competing Risk Analysis of Taiwan Diabetes Cohort Study. J Bone Miner Res. 2015;30:1338–46. https://doi.org/10.1002/jbmr.2462.
American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14-S31. https://doi.org/10.2337/dc20-S002.
Butler AE, Misselbrook D. Distinguishing between type 1 and type 2 diabetes. BMJ. 2020;370:m2998. https://doi.org/10.1136/bmj.m2998.
The International Society for Clinical Densitometry. 2019 Official Positions- Adult. https://iscd.org/learn/official-positions/adult-positions.
Ferrari SL, Abrahamsen B, Napoli N, Akesson K, Chandran M, Eastell R, et al. Diagnosis and management of bone fragility in diabetes: an emerging challenge. Osteoporosis International. 2018;29:2585–96. https://doi.org/10.1007/s00198-018-4650-2.
DeShields SC, Cunningham TD. Comparison of osteoporosis in US adults with type 1 and type 2 diabetes mellitus. J Endocrinol Invest. 2018;41:1051–60. https://doi.org/10.1007/s40618-018-0828-x.
Maddaloni E, D’Eon S, Hastings S, Tinsley LJ, Napoli N, Khamaisi M, et al. Bone health in subjects with type 1 diabetes for more than 50 years. Acta Diabetol. 2017;54:479–88. https://doi.org/10.1007/s00592-017-0973-2.
Hamilton EJ, Drinkwater JJ, Paul Chubb SA, Rakic V, Kamber N, Zhu K, et al. A 10-Year Prospective Study of Bone Mineral Density and Bone Turnover in Males and Females with Type 1 Diabetes. J Clin Endocrinol Metab. 2018;103:3531–9. https://doi.org/10.1210/jc.2018-00850.
Alhuzaim ON, Lewis EJH, Lovblom LE, Cardinez M, Scarr D, Boulet G, et al. Bone mineral density in patients with longstanding type 1 diabetes: Results from the Canadian Study of Longevity in Type 1 Diabetes. J Diabetes Complications. 2019;33(11):107324. https://doi.org/10.1016/j.jdiacomp.2018.12.009.
Napoli N, Incalzi RA, De Gennaro G, Marcocci C, Marfella R, Papalia R, et al. Bone fragility in patients with diabetes mellitus: A consensus statement from the working group of the Italian Diabetes Society (SID), Italian Society of Endocrinology (SIE), Italian Society of Gerontology and Geriatrics (SIGG), Italian Society of Orthopaedics and Traumatology (SIOT). Nutr Metab Cardiovasc Dis. 2021;31:1375–90. https://doi.org/10.1016/j.numecd.2021.01.019.
Dhaliwal R, Foster NC, Boyle C, Al Mukaddam M, Weinstock RS, Rickels MR, et al. Determinants of fracture in adults with type 1 diabetes in the USA: Results from the T1D Exchange Clinic Registry. J Diabetes Complications. 2018;32:1006–11. https://doi.org/10.1016/j.jdiacomp.2018.08.016.
Thayakaran R, Perrins M, Gokhale KM, Kumaran S, Narendran P, Price MJ, et al. Impact of glycaemic control on fracture risk in 5368 people with newly diagnosed Type 1 diabetes: a time-dependent analysis. Diabet Med. 2019;36:1013–9. https://doi.org/10.1111/dme.13945.
Yamamoto M, Sugimoto T. Advanced Glycation End Products, Diabetes, and Bone Strength. Current Osteoporosis Reports. 2016;14:320–6. https://doi.org/10.1007/s11914-016-0332-1.
Shah VN, Harrall KK, Shah CS, Gallo TL, Joshee P, Snell-Bergeon JK, et al. Bone mineral density at femoral neck and lumbar spine in adults with type 1 diabetes: a meta-analysis and review of the literature. Osteoporos Int. 2017;28:2601–10. https://doi.org/10.1007/s00198-017-4097-x.
Hu Y, Li X, Yan X, Huang G, Dai R, Zhou Z. Bone mineral density spectrum in individuals with type 1 diabetes, latent autoimmune diabetes in adults, and type 2 diabetes. Diabetes Metab Res Rev. 2021;37(3):e3390. https://doi.org/10.1002/dmrr.3390.
Keenan HA, Maddaloni E. Bone Microarchitecture in Type 1 Diabetes: It Is Complicated. Current Osteoporosis Reports. 2016;14:351–8. https://doi.org/10.1007/s11914-016-0338-8.
Ma L, Oei L, Jiang L, Estrada K, Chen H, Wang Z, et al. Association between bone mineral density and type 2 diabetes mellitus: A meta-Analysis of observational studies. European Journal of Epidemiology. 2012;27:319–32. https://doi.org/10.1007/s10654-012-9674-x.
Vestergaard P, Rejnmark L, Mosekilde L. Relative fracture risk in patients with diabetes mellitus, and the impact of insulin and oral antidiabetic medication on relative fracture risk. Diabetologia. 2005;48:1292–9. https://doi.org/10.1007/s00125-005-1786-3.
Borges JLC, Bilezikian JP, Jones-Leone AR, Acusta AP, Ambery PD, Nino AJ, et al. A randomized, parallel group, double-blind, multicentre study comparing the efficacy and safety of Avandamet (rosiglitazone/metformin) and metformin on long-term glycaemic control and bone mineral density after 80 weeks of treatment in drug-naïve type 2 diabetes mellitus patients. Diabetes, Obes Metab. 2011;13:1036–46. https://doi.org/10.1111/j.1463-1326.2011.01461.x.
Jang M, Kim H, Lea S, Oh S, Kim JS, Oh B. Effect of duration of diabetes on bone mineral density: A population study on East Asian males. BMC Endocr Disord. 2018;18(1):61. https://doi.org/10.1186/s12902-018-0290-y.
Shanbhogue V V., Hansen S, Frost M, Jørgensen NR, Hermann AP, Henriksen JE, et al. Compromised cortical bone compartment in type 2 diabetes mellitus patients with microvascular disease. Eur J Endocrinol. 2016;174:115–24. https://doi.org/10.1530/EJE-15-0860.
Mitchell A, Fall T, Melhus H, Wolk A, Michaëlsson K, Byberg L. Type 2 Diabetes in Relation to Hip Bone Density, Area, and Bone Turnover in Swedish Men and Women: A Cross-Sectional Study. Calcif Tissue Int. 2018;103:501–11. https://doi.org/10.1007/s00223-018-0446-9.
Hariri AF, Almatrafi MN, Zamka AB, Babaker AS, Fallatah TM, Althouwaibi OH, et al. Relationship between Body Mass Index and T -Scores of Bone Mineral Density in the Hip and Spine Regions among Older Adults with Diabetes: A Retrospective Review. J Obes. 2019;2019:9827403. https://doi.org/10.1155/2019/9827403.
Walsh JS, Vilaca T. Obesity, Type 2 Diabetes and Bone in Adults. Calcified Tissue International. 2017;100:528–35. https://doi.org/10.1007/s00223-016-0229-0.
Palermo A, Tuccinardi D, Defeudis G, Watanabe M, D’Onofrio L, Lauria Pantano A, et al. BMI and BMD: The Potential Interplay between Obesity and Bone Fragility. Int J Env Res Public Heal. 2016;13(6):544. https://doi.org/10.3390/ijerph13060544.
Kasperk C, Georgescu C, Nawroth P. Diabetes Mellitus and Bone Metabolism. Experimental and Clinical Endocrinology and Diabetes. 2017;125:213–7. https://doi.org/10.1055/s-0042-123036.
Gilbert MP, Pratley RE. The impact of diabetes and diabetes medications on bone health. Endocrine Reviews. 2015;36:194–213. https://doi.org/10.1210/er.2012-1042.
Acknowledgements
The authors thank Adrian Aancute and Valentin Zaharia for excellent bone density scanning and imaging.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SCB - Investigation, Formal analysis, Data curation, Writing- original draft; LL – Investigation, Writing – Original draft; CP - Conceptualization, Investigation, Writing – Review and editing; DB - Formal analysis, Writing – review and editing; LM - Conceptualization, Investigation, Validation; MCU - Conceptualization, Writing – Review and editing, Supervision. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research was performed in accordance with the Declaration of Helsinki and informed consent was obtained from all subjects prior to their participation in the study. The study was approved by the Ethics Committee of the “Grigore T. Popa” University of Medicine and Pharmacy Iasi, Romania.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bilha, S.C., Leustean, L., Preda, C. et al. Bone mineral density predictors in long-standing type 1 and type 2 diabetes mellitus. BMC Endocr Disord 21, 156 (2021). https://doi.org/10.1186/s12902-021-00815-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-021-00815-5