Abstract
Background
Medically-tailored meal programs that provide home-delivered medically-appropriate food are an emerging intervention when type 2 diabetes co-occurs with food insecurity (limited or uncertain access to nutritious food owing to cost). We sought to understand the experiences of medically-tailored meal program participants.
Methods
We conducted semi-structured interviews with participants in a randomized trial of medically-tailored meals (NCT02426138) until reaching content saturation. Participants were adults (age > 20 years) with type 2 diabetes in eastern Massachusetts, and the interviews were conducted from April to July 2017. Interviews were transcribed verbatim and coded by two independent reviewers. We determined emergent themes using content analysis.
Results
Twenty individuals were interviewed. Their mean age was 58 (SD: 13) years, 60.0% were women, 20.0% were non-Hispanic black, and 15.0% were Hispanic. Key themes were 1) satisfaction and experience with medically-tailored meals 2) food preferences and cultural appropriateness, 3) diabetes management and awareness, and 4) suggestions for improvement and co-interventions. Within these themes, participants were generally satisfied with medically-tailored meals and emphasized the importance of receiving culturally appropriate food. Participants reported several positive effects of medically-tailored meals, including improved quality of life and ability to manage diabetes, and stress reduction. Participants suggested combining medically-tailored meals with diabetes self-management education or lifestyle interventions.
Conclusions
Individuals with diabetes and food insecurity expressed satisfaction with the medically-tailored meal program, and reported that participation reduced stress and the burden of diabetes management. Suggestions to help ensure the success of medically-tailored meal programs included a strong emphasis on culturally acceptability and accommodating taste preferences for provided foods, and combining medically-tailored meals with diabetes education or lifestyle intervention.
Trial registration
ClinicalTrials.gov NCT02426138.
Similar content being viewed by others
Background
Food insecurity, defined as insufficient access to enough food for an active, healthy life [1], is a common problem for individuals with diabetes mellitus [2,3,4,5]. Approximately one in five individuals with diabetes report food insecurity, and this prevalence rises among those with hemoglobin A1c > 9.0%, a common threshold indicating poor glycemic control [4]. Food insecurity represents an important barrier to diabetes management as dietary adherence is central to diabetes care [6]. Food insecurity is associated with higher risk for diabetes complications, such as coronary heart disease and chronic kidney disease [7, 8]. Perhaps for these reasons, food insecurity is associated with substantially higher healthcare use and costs in individuals with diabetes [9, 10].
Food insecurity has been viewed as a prominent intervention target in the clinical care of diabetes [11, 12], and evidence supporting strategies that can successfully reduce food insecurity and improve health outcomes continues to grow [11]. Among these promising strategies is medically-tailored meal delivery (MTM): home delivery of fully prepared meals specifically tailored to the medical needs of the individual — including not only diabetes but other comorbidities, such as congestive heart failure or end-stage renal disease [13, 14]. Compared with other food insecurity interventions, such as referrals to community human services resources or provision of a healthy ‘box’ of ingredients at a food pantry, MTM offers additional potential benefits. By delivering fully prepared meals, MTM addresses barriers such as lack of transportation, and lack of time and/or knowledge needed to prepare meals that adhere to complex diets.
Emerging research shows that MTM can lead to improved dietary quality [14, 15], and is associated with improved healthcare use and cost [13]. However, as use of these programs in the healthcare context is new, much remains to be learned regarding how best to design the programs to maximize their clinical benefit.
In this study, we used a qualitative research approach to query participants in a randomized clinical trial regarding their experience with MTM. Our goal was to understand elements of the program that worked well, and elements that could be improved, in order to foster greater clinical benefit and facilitate more widespread implementation.
Methods
Data source and study sample
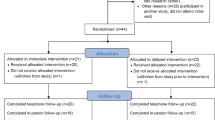
Participants in this study were drawn from the Community Servings: Food as Medicine randomized crossover clinical trial (NCT02426138). The trial has been previously described in detail [15]. In brief, this was a 24-week randomized crossover trial that evaluated the effect of receiving 12 weeks of home delivered medically-tailored meals on dietary quality, conducted from June 2015 to July 2017. Eligible participants were adults (age > 18 years) diagnosed with type 2 diabetes who had a hemoglobin A1c > 8.0% in the last year and reported food insecurity as assessed by the 2-item ‘hunger vital sign’ (n = 42) [15]. The ‘hunger vital sign’ is a validated 2-item indicator of food insecurity status, which asks an individual whether “Within the past 12 months [they] worried whether [their] food would run out before [they] got money to buy more” and whether “within the past 12 months the food [they] bought just didn’t last and [they] didn’t have money to get more.” [16, 17] Meals were prepared from scratch at Community Servings (https://www.servings.org/), a not-for-profit, community-based, medically-tailored meal delivery organization. Frozen and/or refrigerated fully-prepared meals were delivered weekly by delivery truck, with their composition determined by a registered dietician nutritionist to be appropriate for the medical needs of the individual. Ten meals, representing approximately half of the weekly food intake of the participant, were provided each week as single delivery. An example of a day’s worth of meals is provided as Additional file 1: Table S1. Because this trial was designed to test the effect of meal receipt itself on dietary quality, nutritional education was not provided, though it is a component of typical MTM programs outside of clinical trials. After completing the 12 weeks of medically-tailored meals (MTM) provided in the trial, individuals were invited to participate in a qualitative telephone interview to discuss their experience with receiving MTM. Interviews were conducted from April to July 2017.
The study protocol was approved by the Human Research Committee at Partners HealthCare. Written informed consent was obtained from all participants for trial participation, and verbal consent for participation in the qualitative telephone interview was obtained separately.
Availability of data and materials
Because this study relies on transcripts of oral interviews reflecting personal experiences, and thus cannot be de-identifed without fundamentally altering the data itself, data cannot be made publicly available. Data are available from the authors on reasonable request and with the agreement of the study institutional review board if assurances of protection of participant confidentiality can be made.
Qualitative data collection and analysis
Our goal was to conduct structured in-depth interviews with a sufficient number of trial participants to receive adequate feedback regarding their experience with an MTM intervention. We first developed an interview guide (Additional file 1: Table S2) using an iterative process that incorporated the perspectives of study team members and participants, and drew from past work in this patient population [18]. The interview guide was designed to assess participants’ experience and satisfaction with the program and to identify areas of improvement. We then conducted semi-structured telephone interviews with study participants, using purposeful selection to enhance age, gender, and racial/ethnic diversity of those interviewed. We continued contacting participants until content saturation was reached. We anticipated content saturation would be reached after interviewing approximately 1/3 to 1/2 of intervention participants [19]. As described below, coding of interviews occurred during data collection, to determine whether new codes were being added. As we approached 20 interviews, the number of new codes added per interview decreased substantially, leading us to conclude content saturation had been reached. The interviews queried the participants about the meals received and their perceptions of the influence of the meals on diabetes management. We sought suggestions regarding how the meals could be improved and alternative resources that may assist with diabetes management for individuals with diabetes and food insecurity. Interviews lasted approximately 20 min (range: 15 to 40 min). The interviewer (NS) used reflective probes to motivate participants to elaborate on their comments. Interviews were audio-recorded with permission from participants, and recordings were transcribed verbatim. We provided participants with a $20 store gift card for their participation.
Quantitative data
In addition to collecting qualitative data, we extracted sociodemographic and clinical information from the trial baseline examination and questionnaire to better describe the study sample. Details of these assessment procedure have been previously described [15]. We measured height, weight, and blood pressure using calibrated instruments and a standardized measurement technique; we also performed phlebotomy for laboratory assessment of hemoglobin A1c and serum lipid levels.
Data Analysis
Transcripts were coded and analyzed using the content analysis approach [20]. We used an integrated inductive-deductive technique to construct our coding framework [21]. The interview guide and an initial review of the data were used to create a preliminary list of codes and sub-codes. This approach allowed us to produce an organized framework, while giving us the flexibility to include new codes as they emerged. Each transcript was coded, using NVivo 11 software (QSR International, Melbourne, AU), independently by two investigators: the interviewer and the principal investigator of the study. The two coders met weekly to ensure consistency and transparency in the coding. Discrepancies were resolved through reflection and dialogue until consensus was reached. Relevant quotations were selected to illustrate key points within each theme.
Results
Participant characteristics
We reached content saturation after interviewing twenty individuals from the Community Servings: Food as Medicine randomized crossover clinical trial (NCT02426138). This represented approximately half of the total number of trial participants. The mean age of the included individuals was 58 (SD: 13) years, and 60.0% were women (Table 1). Twenty percent of the participants were non-Hispanic black, and 15.0% were Hispanic. The mean of the participants’ income, expressed as a percentage of the federal poverty guideline for their year of study enrollment and household size, was 147% (SD: 54%; as an example, for a single individual in 2016, the federal poverty guideline income threshold was $11,880). The mean duration of diabetes among participants was 13 (SD: 10) years, the mean baseline hemoglobin A1c was 8.0% (SD: 1.6%) and mean body mass index was 34.7 kg/m2 (SD: 6.2 kg/m2).
Satisfaction and experience with MTM
Overall, participants reported being satisfied with the MTM program (illustrative quotes are in the main text with additional quotes in Table 2). One participant said “I was glad that I was able to participate, and that the drivers provided the ease with the meals, and it’s exciting to get meals weekly. It kind of alleviated the headache of either buying or cooking. You know? And when you knew it was a delivery day, you had peace of mind for the rest of the week [laughter].” Participants noted positive interactions with the study staff. Regarding meal delivery, many participants were pleased with the convenience of home-delivered, medically-tailored meals, though a small number expressed difficulty coordinating meal deliveries due to their work schedule. Of note, this program did not require participants to be homebound. Most participants were satisfied with the amount of food they received over the course of the study, stating the food typically lasted for 5 days, the intended amount of time. Regarding the amount of food for a given meal, most participants found the portion size adequate and reported feeling full after finishing a meal.
Food preferences and cultural appropriateness
Most participants enjoyed receiving medically-tailored meals. Many of the participants were satisfied with the quality of the food offered during the intervention, often describing their meals as “healthy” and “balanced”. One said, “I thought they were very well prepared. They were tasty and they were healthy, obviously. And it just helped to be able to get a full healthy meal all in one, with one thing. Like, “Here’s everything you need for one healthy meal [laughter].” Participants also reported being pleased with the variety of food options that were provided throughout the intervention.
Participants emphasized certain aspects of the meals that promoted acceptability. In particular, participants favored familiarity, selection, and healthfulness of the meals. Most participants recognized that the meals provided were appropriate for those with diabetes. However, some did not, which underscores the importance of nutritional education in conjunction with MTM. One participant said, “Some of the meals, I didn’t even know what they were. Even though it gave you the name, I didn’t know really what it was. I think it was some of the grain meals, and it was a meat and it was lamb or something. There were a few things I didn’t like because I don’t eat.”
Given the diversity of the study sample, we explored whether the meals met the cultural needs of the participants. Most participants reported that meals were acceptable, but some expressed interest in receiving meals representative of their country of origin or cultural background. Overall, participants emphasized the importance of having food options that reflected their culture and thus felt familiar and appropriate, with one noting “As I said I am from Haiti. Sometimes some food they gave me, I eat them, they’re good for my body. But I think maybe if they can maybe add a little bit more island food, that would be much better.” Participants reported that culturally acceptable meals may facilitate sustaining adherence to a healthy diet after MTM participation ends, as this would make it easier to incorporate healthier food into their usual diet.
Diabetes management and awareness
Participants reflected on how the medically-tailored meals allowed them access to nutritious meals they otherwise would not have been able to afford. One summarized, “I understand that it does better on this diet. But these are foods that I would not be able to afford to make for myself, or be physically capable of making for myself. The question’s a little more complicated than that. I mean, I understand diabetes and I understand what foods work and what don’t work. But being that I have a spinal cord injury and can’t really cook a lot for myself, and shop a lot for myself, and don’t have an income, I guess the answer is yes [the question being asked is if the program helps the individual adhere to a healthy diet], but it’s not like I don’t know what foods are appropriate. I can see these foods and the foods that I’m eating are appropriate for fighting diabetes and keeping it under control. But I wasn’t unaware of that, I just needed someone to be able to help me to do this.”
Furthermore, they described an element of ‘modeling’ such that having experience with diabetes-appropriate food helped them to understand appropriate portions and food components in a healthy meal. One participant noted “Well, I really like how much food they give it to me and they teach me how much I have to eat every single time I have to eat,” while another said, “I liked the portion control because there was everything that you needed on that plate, and it wasn’t a big portion but it did make you full. And that’s what I liked best about it. And it taught me how to go out and buy certain things that were on the plate so that I could eat separately.”
Participants commented on multiple sources of expense in their lives, including both diabetes-specific expenses such as medication and supplies, along with basic necessities such as housing. Participants reported that participation in the medically-tailored meal program was helpful for overcoming these barriers, since they did not have to allot as much of their own resources to food. This meant that they could better budget for other elements of diabetes management, such as affording medications, or simply other household necessities. “Oh, you don’t know, honey, you don’t know. I was down. I cut out a lot. I cut out the channels on the television, the computer because we’re living on limited income, and they take a third of it for our rent, a third of it for if you have half the package with the Internet and everything. So it did help me. At the end of the month, I could put my hand in my pocket and have $10. And that’s a good feeling.” Participants also reported that the support of the program reinforced their efforts in diabetes self-management, and may have augmented self-efficacy.
Participants noted several benefits they perceived from program participation, aside from diabetes management itself. Participants were relieved of the stress and burden of following a complicated diet. Also, since they no longer had to worry about obtaining nutritious food, participants reported being better able to manage other responsibilities in their lives, and to allocate their attention to managing diabetes.
Regarding diabetes management, participants reported improvements in weight, and in biomarkers of diabetes control, such as hemoglobin A1c, with one saying, “So what I’ll tell you was when I started my [A1C] level was so high. And when I started this program they had to teach me how much food I have to eat and all the protein I have to get. And then through the program my A1C went down. And my PCP, they tell me everything that was perfect and that she’s so happy, and I’m so happy right now I know how I have to eat.” Despite these benefits, some participants continued to struggle with other obstacles that made it difficult to manage their diabetes, including physical disability, medication regimens, and financial pressures not alleviated by MTM. Attempts to address these additional barriers will likely be important components of future interventions.
Suggestions for improvement and co-interventions
Participants had several suggestions regarding how to make MTM programs effective, and how to combine MTM with other interventions to help manage their diabetes. Participants strongly emphasized the importance of having food that reflects their cultural background and preferences regarding seasoning and palatability. Beyond meal provision, individuals believed combining MTM interventions with diabetes self-management education or lifestyle intervention could have a synergistic effect on improving diabetes management. Diabetes support groups and adding physical activity and fitness components were also suggestions for future interventions. Finally, assistance with other financial barriers to diabetes management beyond food – in particular medications – was noted as an important area for future programs.
Discussion
Semi-structured interviews of medically-tailored meal delivery program participants revealed that participants perceived several positive effects, including improved quality of life, ability to manage diabetes, and stress reduction. Participants also had suggestions of improvement for future interventions. Participants suggested combining MTM and diabetes self-management education, or a lifestyle intervention, and providing additional financial assistance, particularly with medications. Regarding the meals in particular, participants emphasized the importance of receiving food that was culturally appropriate with acceptable taste and familiar ingredients.
This study is consistent with and expands our knowledge of medically-tailored meal delivery programs and corresponding health outcomes. Prior studies have suggested that meal delivery programs can improve dietary quality [14, 15], reduce aspects of distress related to living with illness [14], and improve symptoms [22], largely based on quantitative assessments of these features. This study adds a qualitative understanding of the results of MTM participation. In addition, it offers direction for those looking to enhance MTM programs by making them more effective for achieving clinical outcomes.
This study has several implications for future research. Critically, it highlights the opportunity for joint intervention, particularly in combining MTM with education and/or lifestyle interventions. These types of joint interventions may offer a more comprehensive package to those individuals living with diabetes and food insecurity. The skills learned in the lifestyle component of the intervention could potentially enhance the sustainability of intervention effects after conclusion of meal delivery. The study also highlights substantial financial barriers those with food insecurity face, even apart from access to food. Addressing the multitude of health-related social needs faced by these individuals offers additional avenues to improve health and diabetes outcomes. Two key areas for investigation that were not discussed by participants include social isolation and the duration of intervention. With regard to social isolation, prior work on non-tailored home meal delivery, which typically includes daily meal delivery with a home visiting component, has shown reduced loneliness as a benefit of the intervention [23, 24]. For MTM programs, which typically have less frequent (e.g., once weekly) delivery and may not have an explicit home visiting component, it is unclear if these same effects occur. The appropriate duration of intervention for MTM is also unclear. Prior work from our group has shown that, when limits are not imposed, participation occurs for approximately 12 months [25]. Whether shorter or longer durations would be beneficial remains to be determined. Finally, responses from this study highlight the need to examine patient-reported outcomes in MTM program evaluation. Focusing solely on clinical biomarkers or healthcare utilization likely overlooks important benefits perceived by the participants. Whether current instruments that assess patient-reported outcomes are adequate to this task, or instruments specific to the circumstances of the patient populations that receive MTM interventions are required, is an important question for future study.
The results of this study should be interpreted in light of several limitations. This study only analyzed a portion of participants in one MTM program, from a circumscribed geographic area. Though sufficient to reach content saturation and diverse in racial/ethnic background, these results nevertheless may not generalize to other settings. Additionally, while the experience with the intervention reported in the interviews was strongly positive, with concerns raised primarily about food preferences, those who had more negative experiences may not have wanted to be interviewed. However, we regard these findings as hypothesis generating for future studies. A key factor that this study did not fully address was the effect of MTM on households, as opposed to individuals. In this study, the majority of participants lived alone, but because food insecurity is experienced at the household level, the experience of other household members is certainly relevant. Effects on the household may be especially relevant when members are caring for young children. These limitations were balanced by key strengths, including in-depth qualitative examination of a participants in a novel intervention program, and direct feedback from participants to improve future MTM.
Though further research, particularly longer and larger-scale randomized trials, is needed to demonstrate the effectiveness of MTM interventions for health outcomes, it is also important to consider how widespread implementation may be achieved if effectiveness is established. Recent innovations in healthcare financing provide a pathway to sustainability as a covered health insurance benefit [26]. Medicaid demonstration projects in several U.S. states are incorporating MTM into their programs [26,27,28], and recent changes to the Medicare Advantage program also offers opportunities to make MTM more available to beneficiaries [29].
Conclusions
Medically-tailored meal delivery programs are a promising approach to managing a difficult clinical problem—how to improve health in those with both diabetes and food insecurity. Medically-tailored meal programs offer the potential to improve not only biomarkers, but also patient-reported outcomes that are important components of quality of life. Themes identified in this qualitative evaluation can be incorporated in future interventions to help improve health in vulnerable individuals with diabetes.
Availability of data and materials
Because this study relies on transcripts of oral interviews reflecting personal experiences, and thus cannot be de-identifed without fundamentally altering the data itself, data cannot be made publically available. Data is available from the authors on reasonable request and with the agreement of the study institutional review board if assurances of protection of participant confidentiality can be made.
Abbreviations
- MTM:
-
Medically-tailored meal
References
USDA. Food Security Status of U.S. Households in 2018. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/key-statistics-graphics.aspx#foodsecure. Accessed 18 Sept 2019.
Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and nutrition examination survey (NHANES) 1999-2002. J Gen Intern Med. 2007;22:1018–23.
Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr. 2010;140:304–10.
Berkowitz SA, Baggett TP, Wexler DJ, Huskey KW, Wee CC. Food insecurity and metabolic control among U.S. adults with diabetes. Diabetes Care. 2013;36:3093–9.
Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff Proj Hope. 2015;34:1830–9.
American Diabetes Association. 1. Improving Care and Promoting Health in Populations: Standards of Medical Care in Diabetes—2018. Diabetes Care. 2018;41(Supplement 1):S7–12.
Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005-2012. PLoS One. 2017;12:e0179172.
Crews DC, Kuczmarski MF, Grubbs V, Hedgeman E, Shahinian VB, Evans MK, et al. Effect of food insecurity on chronic kidney disease in lower-income Americans. Am J Nephrol. 2014;39:27–35.
Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food Insecurity and Health Care Expenditures in the United States, 2011-2013. Health Serv Res. 2018;53(3):1600-20. https://doi.org/10.1111/1475-6773.12730. Epub 2017 Jun 13. PubMed PMID: 28608473; PubMed Central PMCID: PMC5980147.
Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24:399–404.
Gottlieb LM, Wing H, Adler NE. A systematic review of interventions on patients’ social and economic needs. Am J Prev Med. 2017;53:719–29.
Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities--addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374:8–11.
Berkowitz SA, Terranova J, Hill C, Ajayi T, Linsky T, Tishler LW, et al. Meal delivery programs reduce the use of costly health care in dually eligible Medicare and Medicaid beneficiaries. Health Aff Proj Hope. 2018;37:535–42.
Palar K, Napoles T, Hufstedler LL, Seligman H, Hecht FM, Madsen K, et al. Comprehensive and medically appropriate food support is associated with improved HIV and diabetes health. J Urban Health Bull N Y Acad Med. 2017;94:87–99.
Berkowitz SA, Delahanty LM, Terranova J, Steiner B, Ruazol MP, Singh R, Shahid NN, Wexler DJ. Medically Tailored Meal Delivery for Diabetes Patients with Food Insecurity: a Randomized Cross-over Trial. J Gen Intern Med. 2019;34(3):396-404. https://doi.org/10.1007/s11606-018-4716-z. Epub 2018 Nov 12. PubMed PMID: 30421335; PubMed Central PMCID: PMC6420590.
Hager ER, Quigg AM, Black MM, Coleman SM, Heeren T, Rose-Jacobs R, et al. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126:e26–32.
Makelarski JA, Abramsohn E, Benjamin JH, Du S, Lindau ST. Diagnostic accuracy of two food insecurity screeners recommended for use in health care settings. Am J Public Health. 2017;107:1812–7.
Berkowitz SA, Eisenstat SA, Barnard LS, Wexler DJ. Multidisciplinary coordinated care for type 2 diabetes: a qualitative analysis of patient perspectives. Prim Care Diabetes. 2018;12:218–23.
Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods. 2006;18:59–82.
Weber R. Basic Content Analysis. 2455 teller road, thousand oaks California 91320 United States of America: SAGE publications, Inc.; 1990. https://doi.org/10.4135/9781412983488.
Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res. 2007;42:1758–72.
Hummel SL, Karmally W, Gillespie BW, Helmke S, Teruya S, Wells J, et al. Home-Delivered Meals Postdischarge From Heart Failure Hospitalization. Circ Heart Fail. 2018. https://www.ahajournals.org/doi/full/10.1161/CIRCHEARTFAILURE.117.004886. Accessed 27 Sept 2018.
Thomas KS, Akobundu U, Dosa D. More than a meal? A randomized control trial comparing the effects of home-delivered meals programs on participants’ feelings of loneliness. J Gerontol B Psychol Sci Soc Sci. 2016;71:1049–58.
Campbell AD, Godfryd A, Buys DR, Locher JL. Does participation in home-delivered meals programs improve outcomes for older adults?: results of a systematic review. J Nutr Gerontol Geriatr. 2015;34:124–67.
Berkowitz SA, Terranova J, Randall L, Cranston K, Waters DB, Hsu J. Association Between Receipt of a Medically Tailored Meal Program and Health Care Use. JAMA Intern Med. 2019;179(6):786–93.
Verma S. CMS Approves North Carolina’s Innovative Medicaid Demonstration To Help Improve Health Outcomes. https://www.healthaffairs.org/do/10.1377/hblog20181024.406020/full/. Accessed 30 Oct 2018.
Medically-Tailored-Meals-Pilot-Program. https://www.dhcs.ca.gov/services/ltc/Pages/Medically-Tailored-Meals-Pilot-Program.aspx. Accessed 12 Sept 2019.
MassHealth Demonstration Waiver. Mass.gov. https://www.mass.gov/masshealth-demonstration-waiver. Accessed 12 Sep 2019.
Willink A, DuGoff EH. Integrating medical and nonmedical services — the promise and pitfalls of the CHRONIC care act. N Engl J Med. 2018;378:2153–5.
Acknowledgments
The authors thank the participants of the study and the Diabetes Research Center at Massachusetts General Hospital for serving as the study site. An interim version of these findings was reported at the 2018 American Heart Association EPI Lifestyle Scientific Sessions in New Orleans, LA.
Funding
Funding for this study was provided by the Blue Cross Blue Shield of Massachusetts Foundation, BNY Mellon, the Diabetes Research Center and Division of General Internal Medicine at Massachusetts General Hospital, and the National Institute of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Number K23DK109200. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding organizations had no role in the design of the study or collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
SAB conceived of the study, interpreted the data, and drafted the manuscript. NS conceived of the study, collected and interpreted the data, and drafted the manuscript. DJW, JT, and LMD conceived of the study and revised the manuscript critically for intellectual content. BS, MR, and RS, assisted with collection and interpretation of the data and revised the manuscript critically for intellectual content. All authors give approval of the manuscript version to be submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol (which included both the initial trial and the qualitative follow-up study reported in this manuscript) was approved by the Human Research Committee at Partners HealthCare. Informed written consent was obtained from all participants for trial participation, and verbal consent for participation in the qualitative telephone interview was obtained separately. The ethics committee approved the use of verbal consent for the qualitative follow-up study. Verbal consent was obtained for publication of quotes under the condition that the quotes used would not compromise anonymity.
Consent for publication
Not applicable.
Competing interests
Jean Terranova is an employee of Community Servings. Deborah Wexler reports serving on a Data Monitoring Committee for Novo Nordisk. Linda Delahanty serves on advisory boards for Omada Health, JanaCare, and WW International. All other authors declare they have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Table S1.
Example of 1 day of medically-tailored meals. Table S2. Telephone interview guide.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Berkowitz, S.A., Shahid, N.N., Terranova, J. et al. “I was able to eat what I am supposed to eat”-- patient reflections on a medically-tailored meal intervention: a qualitative analysis. BMC Endocr Disord 20, 10 (2020). https://doi.org/10.1186/s12902-020-0491-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-020-0491-z