Abstract
Background
Radioiodine (RAI) treatment for hyperthyroidism is a very common modality, chosen by physicians worldwide. The outcome of the therapy, however, is not always predictable. While rendering a patient hypo- or euthyroid is meant as a therapeutic success, the latter does not require lifelong hormonal supplementation. The aim of our study is to determine predictors of euthyreosis in patients who underwent RAI treatment.
Methods
Medical records of 144 patients who had undergone RAI therapy were examined. Laboratory and clinical data were analyzed statistically. Ultrasonography findings, such as thyroid volume, nodules’ size and characteristics had been collected at the beginning of treatment and 6 months after the administration of radioiodine 131I−. Moreover, scintigraphy results were taken into account. Multivariate logistic regression analysis model has been used to find predictors of euthyroidism after 12 months of follow-up. The predictors of normal thyroid function have also been analyzed separately for patients with GD (Graves’ disease) and TMNG (toxic multinodular goiter).
Results
The analysis showed that age (OR 1,06; 95%CI 1.025-1.096, p = 0,001), thyroid gland volume (OR 1,04; 95%CI 1,02-1,06; p < 0.001) and iodine uptake level (OR 0,952; 95%CI 0,91-0,98; p = 0,004) were significant factors of achieving normal thyroid function after RAI therapy. According to multivariate logistic regression analysis, in GD patients only age has been shown to be a significant factor (OR 1,06; 95%CI 1,001-1,13; p = 0.047), while in TMNG patients’ age (OR 1,04; 95%CI 1–1,09; p = 0.048), thyroid gland volume (OR 1.038; 95%CI 1.009-1.068; p = 0.009) and iodine uptake level (OR 0.95; 95%CI 0.9–0.99; p = 0.02) all have been proven to be significant predictors of achieving euthyroidism.
Conclusions
The more advanced age, larger volume of thyroid gland and lower iodine uptake level are predictors of euthyreosis after RAI treatment.
Similar content being viewed by others
Background
Hyperthyroidism is one of the most prevalent thyroid disorders, affecting 0.5–2% of women (tenfold more than man) in iodine-replete environments [1]. The most common causes of this condition are Graves’ disease (GD), toxic multinodular goiter (TMNG) and thyroid adenoma (TA) [1, 2]. Currently, there are three possible approaches to treatment of hyperthyroidism: antithyroid drugs (ATDs), radioiodine (RAI) therapy, and thyroidectomy. In case of GD, RAI therapy remains the most popular choice of the physicians in the United States, while ATDs are preferred in Europe, Latin America and Japan [3, 4]. RAI therapy is increasingly used as a first-line treatment of hyperthyroidism as data accumulates proving its efficacy and safety [5, 6]. According to the American Society of Endocrinology, radioiodine treatment may be used in case of all three major causes of hyperthyroidism, depending on the disease’s progression [7]. The outcome of RAI therapy, however, is difficult to predict. An optimal dose that would both eliminate the risk of developing hypothyroidism and maximize the chance of curing hyperthyroidism is individual and difficult to determine [8] (Fig. 1).
The success of RAI therapy in hyperthyroidism – meant as rendering the patient hypo- or euthyroid - correlates strongly with the activity of administered radioiodine [7]. There are several studies comparing the efficacy of treatment using a fixed dose versus a calculated dose, showing little differences between the two approaches [9,10,11,12,13,14]. Thus, the choice of the method depends solely on the physician [7]. Undoubtedly, the outcome of the RAI therapy is not fully predictable and may result in hypothyroidism, euthyroidism or unchanged hyperthyroidism [7]. In an attempt to determine possible factors that could influence the outcome of the treatment, several studies have been conducted, proving e.g. gender, age, presence of ophthalmopathy and serum free T3 concentration to be relevant [11,12,13, 15,16,17,18].
Radioiodine therapy is the only non-operative treatment modality that provides a possibility of rendering a patient euthyroid without the necessity of further pharmacological management. There are, however, not much data on the predictors of achieving euthyreosis in the patients after RAI therapy, presence of which may facilitate the choice of treatment [19,20,21]. Thus, in our research we aim to find predictors of specifically euthyreosis in patients who underwent the RAI treatment.
Methods
Patients
In our study, we included 144 patients transferred for RAI treatment at the Nuclear Medicine Department of the Central Clinical Hospital of the Ministry of the Interior and Administration in Warsaw. All of them were diagnosed with either GD or TMNG. Data regarding the patients with TMNG were collected from the years 2015 and 2016, whereas in case of GD patients, we included data from years 2013–2016. Subjects, who had undergone 2nd RAI treatment, were also included. Thyroid ultrasound examination was performed before radioiodine administration and 6 months after the procedure. Following factors were defined and compared: volume of the thyroid gland, presence and dimensions of nodules. Moreover, results of scintigraphy were taken into consideration: iodine uptake, distribution, type of nodules (‘hot’ or ‘cold’). All the drugs proven to affect the activity of the thyroid gland (e.g. beta-blockers, amiodarone, antithyroid drugs), if taken by the patient, were also noted.
The fixed doses of 131I− administered to patients varied between 610 and 790 MBq. All antithyroid drugs, if given, were withdrawn 1 week before radioiodine administration. Patients were subsequently observed for 12 months. Before the procedure, as well as after 2 weeks and 1, 2 and 6 months the serum concentrations of TSH, free T3 and free T4 were measured. Information regarding thyrostatic drugs or hormonal replacement therapy given during the observation period - in order to achieve euthyreosis - was also recorded. After 12 months, patients were divided into three groups: (1) patients with hypothyroidism, (2) patients who achieved euthyreosis (without medication), (3) patients with persistent hyperthyroidism. Patients were also divided into two etiological subgroups: subjects with Graves’ disease and with toxic multinodular goiter. Euthyreosis was meant as the serum concentrations of free T4, free T3 and TSH in the range of laboratory norms. RAI therapy rendered hypothyroidism if after the 12-month observation period hormonal replacement therapy was needed to achieve normal levels of thyroid hormones. On the other hand, hyperthyroidism was meant as the free T4 and T3 serum concentrations elevated or normal and TSH level decreased, which required antithyroid drugs’ administration.
We performed both univariate and multivariate logistic regression analysis for factors such as age, gender, thyroid volume, ATD treatment 2 weeks before iodine administration, fT3 concentration at presentation and iodine uptake. Predictors of achieving normal thyroid function were searched in three groups: (1) all the patients, (2) GD patients, (3) TMNG patients.
We also made follow-up calls to gather data on the patients’ thyroid status 12 months after radioiodine administration. Among the contacted patients, only in 8 the thyroid status changed between the 6th and 12th month post-therapy. In 6 cases patients previously rendered euthyroid, turned hypothyroid, whereas in 2 persistently hyperthyroid subjects, a normal thyroid function was achieved, without the 2nd dose of radioiodine.
Statistical analysis
We used the program Statistica 13 (StatSoft Polska LTD) for the statistical analysis. The p-value below 0.05 was assumed as statistically significant. In order to determine the statistical significance, we used various tests according to the distribution of variables and their characteristics (Student’s t-test, Mann Whitney U test, chi-square test, Kruskal-Wallis ANOVA test). ROC curves were used for optimization of the threshold setting for selected predictors. We also used the logistic regression, Cox proportional hazards model analysis (12-months observation) to determine independent predictors of achieving normal thyroid function.
Results
All the important clinical data are presented in Table 1. After 12 months of follow-up, 81 patients were rendered hypothyroid (group 1), requiring further hormonal supplementation, 52 achieved euthyreosis (group 2) and 11 remained in the state of hyperthyroidism (group 3). There were 98 females and 46 males in the studied group. Majority of the patients (eighty-one) were diagnosed with toxic nodular goiter and sixty-three with Graves’ disease. Among the patients, who achieved normal thyroid function after the therapy, only 8 were diagnosed with GD. Age of patients varied significantly from 53.5 ± 16.3 and 50.9 ± 16.4 in hypo- and hyperthyroid groups respectively to 67.3 ± 12.7 among subjects who achieved normal thyroid function. Among the patients who underwent thyroidectomy in the past, none became euthyroid after the treatment.
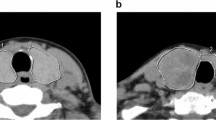
Ultrasonography examination and laboratory tests
All the data regarding ultrasonography and scintigraphy findings refer to the patients’ results before the RAI treatment, unless otherwise indicated. The effect of the therapy was strongly connected with the volume of the thyroid gland before RAI administration (p < 0.001). While patients with smaller initial thyroid volume (22.6 ± 13 cm3) were more prone to entering the state of hypothyroidism after the procedure, the larger thyroid glands (54 ± 31.7 cm3) predisposed to persistent hyperthyroidism. Among patients who had been rendered euthyroid, medium values (41.9 ± 22.2 cm3) of the thyroid glands were observed. Naturally, thyroid glands’ volumes were significantly larger in the TMNG group than in GD patients (p < 0.001).
Similarly, an association was found between the outcome of treatment and the size of thyroid gland 6 months after therapy (p < 0.001). Smaller volumes of thyroid gland (8.4 ± 12.6 cm3) were typical for patients, who presented with hypothyroidism, medium-sized thyroids (23 ± 16.4 cm3) for normal hormonal function and the largest volumes of the gland (29.7 ± 20.1 cm3) were characteristic for persistent hyperthyroidism.
Diffused nodules, found during ultrasound examination, occurred much more often in the patients from the 2nd group (84,6%) compared to individuals who entered the state of hypothyroidism (54,9%) or hyperthyroidism (50%) after treatment. On the other hand, presence of thyroid lobes reaching jugular incision was one of the factors contributing to failure of the therapy. Thyroid masses at the level of the thoracic inlet were present in 27,3% of patients with post-therapeutic hyperthyroidism, 19,2% patients with euthyroidism and only 3,7% with hypothyroidism.
An interesting relationship between the iodine uptake level and the outcome of the therapy was found. Patients with lower iodine uptake (30.2 ± 11.3%) had a significantly greater (p < 0.001) chance of entering the state of euthyroidism. Both remaining outcome groups had clearly higher iodine uptake levels (36.4 ± 13.4% for hypothyroidism and 54.3 ± 16.6% for hyperthyroidism). Patients with GD showed significantly higher iodine uptake levels (40.1 ± 14.3%) than patients with TMNG (32.2 ± 13.4%) (p < 0.001).
Among laboratory thyroid function tests, only TSH concentration at the beginning of the therapy seemed to be a significant factor contributing to predicting the outcome of therapy. Patients with lower concentrations (0.6 ± 1) were more prone to persisting hyperthyroidism (p = 0.035), medium concentrations (0.9 ± 1.7) pointed to normal hormonal function, while the highest values usually resulted in hypothyroidism (1.5 ± 2.6). There were no significant differences in TSH concentrations between GD and TMNG groups.
Results of uni- and multivariate logistic regression analyses are presented in Tables 2, 3 and 4. According to multivariate logistic regression analysis, there are three factors, contributing to achieving normal hormonal level 12 months after the therapy – age (OR 1.06; 95% CI 1.025–1.096; p = 0.001), thyroid volume (OR 1.04; 95% CI 1.02–1.06; p < 0.001) and iodine uptake (OR 0.95; 95% CI 0.91–0.98; p = 0.004). Similar results occurred in case of TMNG patients. Older patients (OR 1.04; 95% CI 1–1.09; p = 0.048), with larger thyroid glands (OR 1.038; 95% CI 1.009–1.068; p = 0.009) and lower iodine uptake levels (OR 0.95; 95% CI 0.9–0.99; p = 0.02) had bigger chances of achieving an euthyroid state. This is, however, not a case in GD patients, in whom only higher age was proven a significant factor of normal thyroid function (OR 1.06; 95% CI 1.001–1.13; p = 0.047).
Moreover, we performed Cox proportional hazards model analysis for determining predictors of normal hormonal function after 12 months of observation (Tables 5 and 6). It has shown age, thyroid volume and radioiodine uptake to be statistically significant, however, only in the overall patients’ population.
ROC curves were also depicted for these predictors to verify their accuracy in predicting the chances of rendering a patient euthyroid (Table 7). With this method we can obtain cut-off values with maximal sensitivity and specificity. For age as a stimulant, the optimal cut-off value was 58 with sensitivity of 86.5% and specificity – 56.5% (AUC: 0.752, AUC CI: 0.627–0.83, p < 0.001). In case of the thyroid volume (also a stimulating factor) the sensitivity and specificity were 58 and 80% respectively (AUC: 0.732, AUC CI: 0.646–0.819, p < 0.001) for the size of 35 cm3. Iodine uptake level was treated as a negative predictor and its threshold was set as 31% with the sensitivity – 65.3% and specificity of 70.3% (AUC: 0.666, AUC CI: 0.574–0.759, p < 0.001). ROC curves have also been depicted for subgroups of patients with GD and TMNG – results are presented in Tables 8 and 9.
In contrast to above-mentioned findings, type of nodule did not vary significantly between the presented groups. Following factors were also verified regarding potential contribution to the outcome of therapy, using logistic regression analysis: gender, antithyroid drugs and beta-blockers’ usage before the treatment, thyroidectomy in the past, radioiodine distribution in the gland, administered dose and type of nodules. No statistically important correlation, however, was noted.
Discussion
Treatment with radioiodine has been one of the most important therapeutic modalities in case of hyperthyroidism for many years [7]. Many physicians prefer to use large quantities of the isotope in order to achieve early hypothyroidism and avoid the necessity of administering another dose of 131I−. Prompting stability with hormonal supplementation in case of hypothyroid patients is a common clinical practice, however, makes the patient fully dependent on the medications. There have been studies aiming to depict an optimal dose of 131I− that would maximize the chances of rendering a patient euthyroid, however, they did not take into consideration other factors predictive of such an outcome [22, 23]. In our study we have presented three such predictors: iodine uptake level, subjects’ age and the thyroid gland volume.
The statistical analysis showed that pre-therapeutic RAI uptake level correlated inversely with the chances of achieving euthyreosis in our patients. In further analysis, it has been shown, however, that it only occurs in case of TMNG patients and not in the GD group. This finding is partially in concordance with the study by M.A. Walter et al., where an inverse correlation was presented in both GD and TMNG patients [24]. There have also been studies proving low RAIU to contribute to a successful outcome of the therapy, meant by hypo- or euthyroidism, however, exclusively in GD [16, 17]. On the other hand, RAIU> 50% also has been shown to increase the incidence of hypothyroidism in case of patients with solitary pretoxic or toxic adenomas treated with radioiodine 131I− [18]. Moreover, in patients with toxic goiter and high radioiodine uptake, RAI therapy resulted in a failure more frequently than in subjects with lower or moderate RAIU levels [25]. Authors suggested that this phenomenon could be attributed to the stunning effect, although normally such a situation occurs, when larger quantities of radioiodine are administered. It could be also explained by the fact that patients with larger RAIU levels could have a more active disease, which results in lower susceptibility to thyroid ablation with radioiodine. The reason for developing hyperthyroidism in patients with very high iodine uptake levels may be due to progressive destruction of the thyroid gland with subsequent release of the free hormones.
Etiology of the hyperthyroidism also contributes to the outcome of the therapy. We have shown that patients with TMNG have more predictors of achieving euthyroidism than patients with GD. Moreover, it seems that TMNG patients were more prone to achieving normal thyroid function than subjects in the GD group. This finding is in accord with observations made by other researchers [20]. It has also been shown that, conversely, in patients with GD hypothyroidism is a more frequent outcome of RAI therapy than in subjects with TMNG [12, 20]. The explanation of our finding could be that the extranodal tissue in TMNG exhibits less iodine uptake. As a consequence, it does not suffer as much damage as the nodules, which allows the gland to maintain its function after the therapy has ended [10]. In other words, ablated thyroid tissue in GD patients may not able to maintain its hormonal function after the radioiodine treatment.
In our study we also found that the more advanced age in the patients was a significant predictor of achieving euthyreosis. As other studies usually focus on depicting factors contributing to the success of RAI therapy (and not euthyreosis exclusively), we had little material to compare our results with [11, 12, 26,27,28,29,30,31,32]. Nonetheless, some papers have shown that younger patients were more likely to present persistent hyperthyroidism after RAI therapy [9, 18, 26, 33]. The reason behind it may be that younger thyroid tissue is more resistant to radiation than in older patients [18]. Similar observations were made by other researchers, who found early age of onset of hyperthyroidism to be a negative predictor of the treatment success [12, 34]. This, however, was strongly connected to the severity of hyperthyroidism, rather than with the young age itself. Schneider et al. also noted a positive correlation between the older age and the success of RAI treatment having performed univariate analysis, but after multivariate analysis patients’ age was no longer significant [27]. Moreover, there have also been studies proving younger individuals to have an increased risk of presenting hypothyroidism [19, 28, 29].
There are certain factors that, undoubtedly, have an effect on the outcome of 131I− therapy, e.g. use of ATDs, corticosteroids, goiter size, severity of hyperthyroidism, low-iodine diet or smoking habits. We must not forget, however, that these modulators are influenced by age and an overall condition of the patient. Thus, the patient’s advanced age and the final result of treatment are linked, though in an indirect manner [35]. Our result could be attributed to the fact, that 84.6% of patients who responded positively to the treatment, were diagnosed with TMNG, which prevalence increases in elderly patients and is more frequent than GD [7].
We have also proven that individuals with larger volumes of thyroid were more prone to achieving euthyreosis than patients with smaller glands. In contrast, many studies showed an inverse correlation between thyroid gland size and a successful outcome of treatment (again hypo- or euthyroid) [12, 32, 33, 36,37,38]. On the other hand, no significant impact of the above-mentioned factor was noted in other researches or results turned out to be statistically insignificant after performing regression analysis [9, 11, 20, 27, 39, 40]. Differences between various papers may be explained by lack of an objective method of measuring thyroid gland size. Clinical examination or scintigraphy are less precise than ultrasound [41, 42]. Marković et al. suggested that an influence of the gland size on the outcome of therapy was present in case of normo-echogenic glands only [21]. Our data show that 22.6 cm3 was the mean volume for hypothyroid outcome group and is in concordance with results presented by Catarina Machado et al. (24.3 cm3) [43]. Similarly, mean thyroid volume of persistently hyperthyroid patients’ (54 cm3) was comparable with findings by Pfeilschifter et al., who observed failure of RAI therapy in individuals with thyroid’s volume larger than 50 cm3 [19].
Since the focus in this paper is on the predictors of achieving euthyreosis exclusively, the literature review was severely narrowed as the great number of the scientific papers depict factors contributing to overall success of the RAI therapy. It is, undoubtedly, one of the limitations of our discussion. We also need to mention that although a group of 144 patients is big enough to draw statistically significant conclusions, in order to make our findings more credible, a larger cohort should be examined – preferably in a prospective study. Moreover, it needs to be underlined that even after rendering a patient euthyroid, there is a low risk of converting to hypothyroid state in the subsequent years after therapy, especially in patients pretreated with ATDs, eventually requiring hormonal supplementation [44]. Lack of control group is another limitation.
As a follow-up to this research, we consider using the measurements of the effective thyroidal half-life and uptake of 131I− as shown by Kobe C. et al. [45]. This approach has been shown to provide high therapy success rates in patients with GD [46]. It seems that this individual dosimetric approach not only gives a more precise data on the radiation exposure, but also may be more beneficial than the classical dosimetric methods.
Conclusions
In summary, in our research we depicted predictors of achieving euthyreosis after treatment with a fixed dose of 131I− in hyperthyroid patients. The more advanced age, larger volume of thyroid gland and lower iodine uptake values contribute to rendering the patient euthyroid. In our opinion, physicians should take these three factors into consideration, while discussing the treatment modality with the patient, especially in case of TMNG diagnosis. It seems that subjects with higher RAIU levels should require special attention, since high failure rates are prevalent among them. Perhaps larger doses of radioiodine or longer pre-treatment with ATDs to prompt stabilization could be beneficial in these cases. In patients with e.g. smaller thyroid volumes, individual dosimetric methods may be useful to maximize the chances of achieving therapeutic success. GD patients with mild intensity of the disease could benefit from a longer use of ATDs before transferring them for radioiodine treatment, as older age seems to contribute to rendering a normal thyroid function in these patients. Further studies on predictors of normal thyroid function in the individual dosimetric approach, would help elucidate, whether the same factors also play a role in achieving euthyroidism, using this method.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ATDs:
-
Antithyroid drugs
- AUC:
-
Area under cruve
- CI:
-
Confidence interval
- GD:
-
Graves’ disease
- HR:
-
Hazard ratio
- OR:
-
Odds ratio
- RAIU:
-
Radioiodine uptake
- ROC:
-
Receiver operating characteristic
- (f)T3:
-
(Free) triiodothyronine
- (f)T4:
-
(Free) thyroxine
- TA:
-
Toxic adenoma
- TMNG:
-
Toxic multinodular goiter
- TSH:
-
Thyroid-stimulating hormone
References
Vanderpump MP. The epidemiology of thyroid disease. Br Med Bull. 2011;99:39–51.
Singer PA, Cooper DS, Levy EG, Ladenson PW, Braverman LE, Daniels G, et al. Treatment guidelines for patients with hyperthyroidism and hypothyroidism. Standards of care committee, American Thyroid Association. JAMA. 1995;273(10):808–12.
Burch HB, Burman KD, Cooper DS. A 2011 survey of clinical practice patterns in the management of graves’ disease. J Clin Endocrinol Metab. 2012;97(12):4549–58.
Wartofsky L, Glinoer D, Solomon B, Nagataki S, Lagasse R, Nagayama Y, et al. Differences and similarities in the diagnosis and treatment of graves’ disease in Europe, Japan, and the United States. Thyroid. 1991;1(2):129–35.
Lee HS, Hwang JS. The treatment of graves’ disease in children and adolescents. Ann Pediatr Endocrinol Metab. 2014;19(3):122–6.
Wang J, Qin L. Radioiodine therapy versus antithyroid drugs in graves’ disease: a meta-analysis of randomized controlled trials. Br J Radiol. 2016;89(1064):20160418.
Ross DS, Burch HB, Cooper DS, Greenlee MC, Laurberg P, Maia AL, et al. 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis. Thyroid. 2016;26(10):1343–421.
Weetman AP. Radioiodine treatment for benign thyroid diseases. Clin Endocrinol. 2007;66(6):757–64.
Leslie WD, Ward L, Salamon EA, Ludwig S, Rowe RC, Cowden EA. A randomized comparison of radioiodine doses in graves’ hyperthyroidism. J Clin Endocrinol Metab. 2003;88(3):978–83.
Jarløv AE, Hegedüs L, Kristensen LO, Nygaard B, Hansen JM. Is calculation of the dose in radioiodine therapy of hyperthyroidism worth while? Clin Endocrinol. 1995;43(3):325–9.
Allahabadia A, Daykin J, Holder RL, Sheppard MC, Gough SC, Franklyn JA. Age and gender predict the outcome of treatment for graves’ hyperthyroidism. J Clin Endocrinol Metab. 2000;85(3):1038–42.
Allahabadia A, Daykin J, Sheppard MC, Gough SC, Franklyn JA. Radioiodine treatment of hyperthyroidism-prognostic factors for outcome. J Clin Endocrinol Metab. 2001;86(8):3611–7.
Catargi B, Leprat F, Guyot M, Valli N, Ducassou D, Tabarin A. Optimized radioiodine therapy of graves’ disease: analysis of the delivered dose and of other possible factors affecting outcome. Eur J Endocrinol. 1999;141(2):117–21.
Howarth D, et al. Determination of the optimal minimum radioiodine dose in patients with graves’ disease: a clinical outcome study. Eur J Nucl Med. 2001;28:1489–95.
Manohar K, Mittal BR, Bhoil A, Bhattacharya A, Dutta P, Bhansali A. Factors predicting treatment failure in patients treated with iodine-131 for graves’ disease. World J Nucl Med. 2013;12(2):57–60.
Liu M, Jing D, Hu J, Yin S. Predictive factors of outcomes in personalized radioactive iodine ((131)I) treatment for graves’ disease. Am J Med Sci. 2014;348(4):288–93.
Zaman MU, Fatima N, Zaman U, Sajjad Z, Zaman A, Tahseen R. Predictive value of pyramidal lobe, percentage thyroid uptake and age for ablation outcome after 15 mCi fixed dose of radioiodine-131 in graves’ disease. Indian J Nucl Med. 2015;30(4):309–13.
Ceccarelli C, Bencivelli W, Vitti P, Grasso L, Pinchera A. Outcome of radioiodine-131 therapy in hyperfunctioning thyroid nodules: a 20 years’ retrospective study. Clin Endocrinol. 2005;62(3):331–5.
Pfeilschifter J, Elser H, Haufe S, Ziegler R, Georgi P. Impact of pretreatment variables on the outcome of standardized 131I therapy with 150 gray in graves’ disease. Nuklearmedizin. 1997;36(3):81–6.
Lewis A, Atkinson B, Bell P, Courtney H, McCance D, Mullan K, et al. Outcome of 131I therapy in hyperthyroidism using a 550MBq fixed dose regimen. Ulster Med J. 2013;82(2):85–8.
Markovic V, Eterovic D. Thyroid echogenicity predicts outcome of radioiodine therapy in patients with graves’ disease. J Clin Endocrinol Metab. 2007;92(9):3547–52.
Blair AL, Lowe DC, Hadden DR, Weaver JA, Montgomery DA. Long term follow up of patients treated for hyperthyroidism with low dose radioactive iodine. Ulster Med J. 1980;49(1):71–8.
Peters H, Fischer C, Bogner U, Reiners C, Schleusener H. Radioiodine therapy of graves’ hyperthyroidism: standard vs. calculated 131iodine activity. Results from a prospective, randomized, multicentre study. Eur J Clin Investig. 1995;25(3):186–93.
Walter MA, Christ-Crain M, Eckard B, Schindler C, Nitzsche EU, Müller-Brand J, et al. Radioiodine therapy in hyperthyroidism: inverse correlation of pretherapeutic iodine uptake level and post-therapeutic outcome. Eur J Clin Investig. 2004;34(5):365–70.
Kristoffersen US, Hesse B, Rasmussen AK, Kjaer A. Radioiodine therapy in hyperthyroid disease: poorer outcome in patients with high 24 hours radioiodine uptake. Clin Physiol Funct Imaging. 2006;26(3):167–70.
Tamatea JA, Conaglen JV, Elston MS. Response to radioiodine therapy for thyrotoxicosis: disparate outcomes for an indigenous population. Int J Endocrinol. 2016;2016:7863867.
Schneider DF, Sonderman PE, Jones MF, Ojomo KA, Chen H, Jaume JC, et al. Failure of radioactive iodine in the treatment of hyperthyroidism. Ann Surg Oncol. 2014;21(13):4174–80.
Boelaert K, Syed AA, Manji N, Sheppard MC, Holder RL, Gough SC, et al. Prediction of cure and risk of hypothyroidism in patients receiving 131I for hyperthyroidism. Clin Endocrinol. 2009;70(1):129–38.
Metso S, Jaatinen P, Huhtala H, Luukkaala T, Oksala H, Salmi J. Long-term follow-up study of radioiodine treatment of hyperthyroidism. Clin Endocrinol. 2004;61(5):641–8.
Erem C, Kandemir N, Hacihasanoglu A, Ersöz HO, Ukinc K, Kocak M. Radioiodine treatment of hyperthyroidism: prognostic factors affecting outcome. Endocrine. 2004;25(1):55–60.
Knapska-Kucharska M, Oszukowska L, Lewiński A. Analysis of demographic and clinical factors affecting the outcome of radioiodine therapy in patients with hyperthyroidism. Arch Med Sci. 2010;6(4):611–6.
Peters H, Fischer C, Bogner U, Reiners C, Schleusener H. Treatment of graves’ hyperthyroidism with radioiodine: results of a prospective randomized study. Thyroid. 1997;7(2):247–51.
Alexander EK, Larsen PR. High dose of (131) I therapy for the treatment of hyperthyroidism caused by graves’ disease. J Clin Endocrinol Metab. 2002;87(3):1073–7.
Yamashita Y, Yamane K, Tamura T, Okubo M, Kohno N. Onset age is associated with outcome of radioiodine therapy in graves’ disease. Endocr J. 2004;51(2):127–32.
Bonnema SJ, Hegedüs L. Radioiodine therapy in benign thyroid diseases: effects, side effects, and factors affecting therapeutic outcome. Endocr Rev. 2012;33(6):920–80.
Reinhardt MJ, Brink I, Joe AY, Von Mallek D, Ezziddin S, Palmedo H, et al. Radioiodine therapy in graves’ disease based on tissue-absorbed dose calculations: effect of pre-treatment thyroid volume on clinical outcome. Eur J Nucl Med Mol Imaging. 2002;29(9):1118–24.
Chiovato L, Fiore E, Vitti P, Rocchi R, Rago T, Dokic D, et al. Outcome of thyroid function in graves’ patients treated with radioiodine: role of thyroid-stimulating and thyrotropin-blocking antibodies and of radioiodine-induced thyroid damage. J Clin Endocrinol Metab. 1998;83(1):40–6.
Jensen BE, Bonnema SJ, Hegedüs L. Glucocorticoids do not influence the effect of radioiodine therapy in graves’ disease. Eur J Endocrinol. 2005;153(1):15–21.
Sabri O, Zimny M, Schulz G, Schreckenberger M, Reinartz P, Willmes K, et al. Success rate of radioiodine therapy in graves’ disease: the influence of thyrostatic medication. J Clin Endocrinol Metab. 1999;84(4):1229–33.
Walter MA, Christ-Crain M, Schindler C, Müller-Brand J, Müller B. Outcome of radioiodine therapy without, on or 3 days off carbimazole: a prospective interventional three-group comparison. Eur J Nucl Med Mol Imaging. 2006;33(6):730–7.
van Isselt JW, de Klerk JM, van Rijk PP, van Gils AP, Polman LJ, Kamphuis C, et al. Comparison of methods for thyroid volume estimation in patients with graves’ disease. Eur J Nucl Med Mol Imaging. 2003;30(4):525–31.
Jarløv AE, Hegedüs L, Gjørup T, Hansen JE. Accuracy of the clinical assessment of thyroid size. Dan Med Bull. 1991;38(1):87–9.
Machado C, Tavares P, Monteiro S, Rocha G, Silva F, Oliveira JM, et al. Outcome of radioiodine therapy in patients with hyperthyroidism. Endocr Abstr. 2017;49:EP1351. https://doi.org/10.1530/endoabs.49.EP1351.
Nygaard B, Hegedüs L, Ulriksen P, Nielsen KG, Hansen JM. Radioiodine therapy for multinodular toxic goiter. Arch Intern Med. 1999;159(12):1364–8.
Kobe C, Eschner W, Wild M, Rahlff I, Sudbrock F, Schmidt M, et al. Radioiodine therapy of benign thyroid disorders: what are the effective thyroidal half-life and uptake of 131I? Nucl Med Commun. 2010;31(3):201–5.
Kobe C, Eschner W, Sudbrock F, Weber I, Marx K, Dietlein M, et al. Graves’ disease and radioiodine therapy: is success of ablation dependent on the achieved dose above 200 Gy? Nuklearmedizin. 2008;47:13–7.
Acknowledgments
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AS together with TG designed the study, gathered the patient data and were major contributors in writing the manuscript. BK interpreted the data and performed the statistical analysis, designed the study. TB provided the patient data and was responsible for the paper’s revision. EF contributed to manuscript writing and revision. All authors approved the study.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study has been approved by the Bioethical Committee of the Medical University of Warsaw – approval No. AKBE/245/2019.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Stachura, A., Gryn, T., Kałuża, B. et al. Predictors of euthyreosis in hyperthyroid patients treated with radioiodine 131I−: a retrospective study. BMC Endocr Disord 20, 77 (2020). https://doi.org/10.1186/s12902-020-00551-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-020-00551-2