Abstract
Background
Gitelman syndrome (GS) is an inherited autosomal recessive renal tubular disorder characterized by low levels of potassium and magnesium in the blood, decreased excretion of calcium in the urine, and elevated blood pH. GS is caused by an inactivating mutation in the SLC12A3 gene, which is located on the long arm of chromosome 16 (16q13) and encodes a thiazide-sensitive sodium chloride cotransporter (NCCT).
Case presentation
A 45-year-old man with Graves’ disease complicated by paroxysmal limb paralysis had a diagnosis of thyrotoxic periodic paralysis for 12 years. However, his serum potassium level remained low despite sufficiently large doses of potassium supplementation. Finally, gene analysis revealed a homozygous mutation in the SLC12A3 gene. After his thyroid function gradually returned to normal, his serum potassium level remained low, but his paroxysmal limb paralysis resolved.
Conclusions
GS combined with hyperthyroidism can manifest as frequent episodes of periodic paralysis; to date, this comorbidity has been reported only in eastern Asian populations. This case prompted us to more seriously consider the possibility of GS associated with thyroid dysfunction.
Similar content being viewed by others
Background
Gitelman syndrome (GS) is an inherited autosomal recessive renal tubular disorder characterized by low levels of potassium and magnesium in the blood, decreased excretion of calcium in the urine, and elevated blood pH. GS is caused by an inactivating mutation in the SLC12A3 gene, which is located on the long arm of chromosome 16 (16q13) and encodes a thiazide-sensitive sodium chloride cotransporter (NCCT). Graves’ disease (GD) is a common cause of hyperthyroidism. In our department, we diagnosed a patient with GD and GS.
Case presentation
The patient was a 45-year-old male with a 12-year history of paroxysmal weakness of the limbs. He was diagnosed with hypokalemic periodic paralysis in 2005 and hyperthyroidism in 2008. He had taken antithyroid drugs on an irregular basis since 2008 but had not undergone proper biochemical examination. Whenever he felt that his weakness was becoming severe, he would self-prescribe potassium chloride. In June 2017, the extent of his lower limb weakness increased such that he could no longer walk. He took potassium chloride without improvement. Subsequently, he was admitted to another hospital. His temperature was 36.7 °C, and his pulse was 96 beats/min. The muscle strength in his lower limbs was grade II [1], and that in his upper limbs was grade III. His limb muscle tone was normal. His electrolyte and blood marker levels were as follows: K+, 1.4 mmol/l; Na+, 138 mmol/l, Cl−, 97 mmol/l; Ca2+, 2.61 mmol/l; free triiodothyronine (FT3) 6.96 pmol/l (1.86–6.44); free thyroxine (FT4) 38.96 mIU/l (11.45–22.14); thyroid-stimulating hormone (TSH) < 0.01 mIU/l (0.4–4.5); thyroglobulin antibody (TgAb) 16.61 IU/ml (0–150); and thyrotropin receptor antibody (TRAb) 22.36 mIU/l (0–5). Thyroid ultrasound demonstrated diffuse thyromegaly with a rich blood supply. The patient was diagnosed with GD and hypokalemic periodic paralysis and was treated with propylthiouracil (PTU) and potassium chloride. However, 2 days later, despite improvement of his weakness, his temperature increased to 41 °C, and he experienced cough and expectoration. Computed tomography (CT) imaging of his lungs revealed pneumonia. He was subsequently treated with cefazolin and transferred to our hospital 2 days later.
When the patient was admitted to our department, his limb weakness had significantly improved. He had a temperature of 38.8 °C, a pulse of 96 beats/min, a breathing rate of 20 respirations/min, a blood pressure of 106/68 mmHg, and grade II thyroid enlargement. Vascular murmur was audible in the thyroid. The muscle strength in his limbs was grade V, and his limb muscle tone was normal. The patient’s biochemical parameters were as follows (the reference values are different from those used in the previous department): [blood count] leukocytes 13.10 × 109/l, neutrophils 11.99 × 109/l and hemoglobin 13.3 g/dl; [serum electrolytes] K+ 2.110 mmol/l, Na+ 131.6 mmol/l, Cl− 91.1 mmol/l, Ca2+ 1.850 mmol/l, and Mg2+ 0.540 mmol/l; [thyroid function and thyroid antibodies] triiodothyronine (T3) 1.40 mmol/l (1.34–2.75), thyroxine (T4) > 300 nmol/l (78.38–157.40), FT3 5.32 pmol/l (3.60–6.00), FT4 51.23 pmol/l (7.86–14.41), TSH 0.01 mIU/l (0.34–5.65), thyroid peroxidase antibody (TPOAb) 36.33 IU/ml (0–30), TRAb 9.011 IU/ml (0–30), TgAb 6.04% (< 30%), and thyroid microsomal antibody (TMAB) 6.48% (< 20%); and creatine kinase (CK) 1398 U/l (38–174) and CK-MB 29 U/l (0.0–25.0). The patient’s liver and kidney functions were normal. We treated him with cefazolin, propranolol, PTU and potassium chloride. The patient’s vital signs and strength normalized after 3 days, and his leukocyte count had decreased to 5.97 × 109/l, his neutrophils had decreased to 3.59 × 109/l, and his CK had decreased to 40 U/l. However, his serum potassium level remained low despite 24 g/d of potassium supplementation. Additionally, the patient had hypomagnesemia and metabolic alkalosis (the results are shown in Tables 1 and 2). Further testing showed that his renin activity (supine) was 5.17 ng/ml/h (reference value 0.15–2.33), his aldosterone level was 436.10 pg/ml (10–160), his random urinary calcium/creatinine ratio was 0.23, his osteocalcin level was 1.06 ng/ml (6.00–48.00), his parathyroid hormone level was 11.22 pg/ml (6.0–80.0) and his calcitonin level was 4.87 pg/ml (0.00–18.00).
Based on these results, we suspected that the patient did not have thyrotoxic periodic paralysis (TPP) but rather GS. Therefore, we sent a blood sample to Beijing Huada Company for sequencing. The Next Generation Sequencing (NGS) was used. The sequencing protocol was based on the Roche Nimblegen SeqCap EZ Choice XL Library for exon trapping. A total of 25 genes (Table 3) known to be associated with hypokalemia were targeted and the total size of target regions was 11.8 M. Libraries were prepared with the Kapa Hyper Prep kit and sequencing was carried out by Illumina NextSeq500 System. The sequencing data were compared to the human genome by BWA (0.7.12-r1039) software (http://bio-bwa.sourceforge.net/), and ANNOVAR (Date: 2015-06-17) was used to annotate the mutation sites based on dbSNP, Clinvar, ExAC, and 1000 genomes, among others. We found a homozygous mutation in the SLC12A3 gene (Exon12 1562-1564delTCA) with an amino acid change of 522delIle, which was first reported as a compound heterozygous mutation.by Vargas-Poussou [2]. The mutation was confirmed by sanger sequencing. No other phenotypes were found, including those for Bartter syndrome, hypokalemic periodic paralysis,Liddle syndrome, hyperaldosteronism, and apparent mineralocorticoid excess. The diagnosis was changed to GD with GS. Moreover, we obtained blood samples from the patient’s mother and son (his father had passed away) who did not have hypokalemia and hyperthyroidism. Both of them were proved as heterozygous mutation carriers by sanger sequencing. The sequencing chromatograms are shown in Figs. 1 and 2. The patient had three brothers and one sister, but we were unable to obtain blood samples from them.
In addition to antithyroid drugs (methimazole 30 mg/d), we gave the patient potassium chloride (3 g/d), potassium citrate (6 g/d), and magnesium potassium aspartate (1.788 g/d). At the follow-up visit, we found that the patient often forgot to take his medicine. The results for thyroid function and electrolyte levels before and after treatment are listed in Table 4, which indicated that the patient’s thyroid function had improved. Hypothyroidism occurred during the course of treatment, but the patient’s thyroid function returned to normal after we reduced the dose of methimazole. The patient refused the recommendation to undergo I131 therapy. His serum potassium level remained low despite a sufficiently large daily dose of potassium, but no paroxysmal paralysis occurred after discharge.
Discussion and conclusions
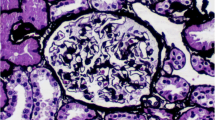
More than 400 SLC12A3 variations have been identified to date. The prevalence of GS among Japanese populations is 10.3/10000 [3, 4]. The incidence rates of GD and Hashimoto’s thyroiditis (HT) among the Chinese population are 120/100000/year and 100/100000/year, respectively [5]. The prevalence rates of both autoimmune thyroid disease (AITD) and GS among East Asian populations are higher than those among European populations [6]. Through a Chinese and English literature review, we identified 17 cases of AITD complicated with GS from nine papers (18 cases including ours) [7,8,9,10,11,12,13,14,15,16,17]. The cases included seven males (aged 20~ 45 years) and 11 females (aged 14~ 50 years). Among the patients, 13 had GD, 3 had HT, and two had antibody-positive AITD. All patients with GD and HT developed hypokalemic periodic paralysis. Twelve patients underwent genetic analysis, and all mutations were located in the SLC12A3 gene; four patients were homozygotes, one was a heterozygote, and five were complex heterozygotes. One patient did not have any detectable mutation, and the mutation type for one patient was not mentioned. The details of these cases are listed in Tables 5 and 6. Except for our case, the mutations in all cases were single base substitutions; two of the mutations were T60 M [18], which is a common variation among Chinese individuals. Six patients underwent renal biopsy, and all of the patients had juxtaglomerular complex (JGC) hyperplasia. Patient 6 had clinical and pathological features of GS but a wild-type SLC12A3 gene; therefore, the patient may have had acquired GS caused by autoimmune disease [19, 20]. Interestingly, we noticed that all the reported cases were from eastern Asia, possibly because of the high prevalence of GS and AITD in East Asian populations.
Nevertheless, we still lack sufficient data to demonstrate whether AITD is more likely to occur in patients with GS. Patients with GS may undergo more extensive testing, including thyroid functional analysis, compared to healthy individuals, which may facilitate the identification of additional abnormalities. Although sufficient data are available regarding the induction of hypokalemia and hypomagnesemia by hyperthyroidism, research on the long-term effects of hypokalemia and hypomagnesemia on the thyroid is lacking. Iodine and magnesium metabolism have been found to be closely linked [21]. One study showed that long-term high dietary magnesium can lead to abnormal thyroid function. Another study suggested that hypomagnesemia may lead to rapid relapse of GD [22]. In contrast, increasing magnesium supplementation has also been shown to promote normalization of thyroid morphology and function [23].
Autoimmune thyroid diseases (AITDs) are complex genetic diseases. The genes contributing to AITD can be divided into two categories: immunomodulatory genes, including the human leukocyte antigen (HLA), cytotoxic T lymphocyte-related antigen 4 (CTLA-4), protein tyrosine phosphatase, nonreceptor type 22 (PTPN22), CD40, CD25, and Fc receptor-like 3 (FCRL3) genes, and thyroid-specific genes, including the thyroid-stimulating hormone receptor (TSHR) gene and the thyroglobulin (Tg) gene. However, no studies have indicated that a correlation exists between these genes and the SLC12A3 gene.
In conclusion, GS combined with hyperthyroidism (or other AITDs) can cause hypokalemic periodic paralysis. Our patient was misdiagnosed with hypokalemic TPP for a long time, indicating that the possibility of GS should be considered in clinical cases with hyperthyroidism and persistent hypokalemia.
Abbreviations
- AITD:
-
autoimmune thyroid disease
- CT:
-
computed tomography
- FT3:
-
free triiodothyronine
- GD:
-
Graves’ disease
- GS:
-
Gitelman syndrome
- HT:
-
Hashimoto’s thyroiditis
- JGC:
-
juxtaglomerular complex
- PTU:
-
propylthiouracil
- TgAb:
-
thyroglobulin antibody
- TMAB:
-
thyroid microsomal antibody
- TPOAb:
-
thyroid peroxidase antibody
- TRAb:
-
thyrotropin receptor antibody
- TSH:
-
thyroid-stimulating hormone
- WBC:
-
white blood cell
References
Frese E, Brown M, Norton BJ. Clinical reliability of manual muscle testing. Middle trapezius and gluteus medius muscles Phys Ther. 1987;67(7):1072–6.
Vargas-Poussou R, Dahan K, Kahila D, Venisse A, Riveira-Munoz E, Debaix H, et al. Spectrum of mutations in Gitelman syndrome. J Am Soc Nephrol. 2011;22(4):693–703.
Tago N, Kokubo Y, Inamoto N, et al. A high prevalence of Gitelman's syndrome mutations in Japanese. Hyperten Res. 2004;27:327–31.
Melander O, Orhomelander M, Bengtsson K, et al. Genetic variants of thiazide-sensitive NaCl-cotransporter in Gitelman's syndrome and primary hypertension. Hypertension. 2000;36:389–94.
McLeod DS, Cooper DS. The incidence and prevalence of thyroid autoimmunity. Endocrine. 2012;42:252–65.
Nyström HF, Jansson S, Berg G. Incidence rate and clinical features of hyperthyroidism in a long-term iodine sufficient area of Sweden (Gothenburg) 2003-2005. Clin Endocrinol. 2013;78:768–76.
Dong H, Lang Y, Shao Z, Lin L, Shao L. Coexistence of Gitelman’s syndrome and thyroid disease:SLCl2A3 gene analysis in two patients. Chin J Endocrinol Metab. 2010;26:395–8 (in Chinese).
Aoi N, Nakayama T, Tahira Y, et al. Two novel genotypes of the thiazide-sensitive Na-cl cotransporter (SLC12A3) gene in patients with Gitelman's syndrome. Endocrine. 2007;31:149–53.
Xinyu Xu, Min sun, Xiaoyun Liu, et al. clinical feature and genetic analysis of Gitelman’s syndrome accompanied by autoimmune thyroid disease. Chin J Endocrinol Metab. 2013;29:50–54. (in Chinese).
Mizokami T, Hishinuma A, Kogai T, et al. Graves’ disease and Gitelman syndrome. Clin Endocrinol. 2016;84:149–50.
Zha B, Zheng P, Liu J, Huang X. Coexistence of Graves' disease in a 14-year-old young girl with Gitelman syndrome. Clin Endocrinol. 2015;83:995.
Xiao X, Liao E, Zhang H, Mao J, Pingan H. Gitelman syndrome with Graves's disease: a case report. Chin J Endocrinol Metab. 2006;22:91–2 (in Chinese).
Yayi He, Bingyin Shi, Xiaoyan Wu, et al. Gitelman syndrome complicated with hyperthyroidism and IgA nephropathy patients. Chin J Nephrol 2010;26:70. (in Chinese).
Li M, Li T, He Y, Shi B. Nursing care of 2 patients with Gitelman syndrome comlicated with hyperthyroidism and IgA nephropathy. J Nurs Sci. 2015;30:33–4.
Shuiyu Ji, Xiang Zhao. Hashimoto's thyroiditis complicated with Gitelman syndrome: a case report. Chin J Nephrol. 2013;29:76. (in Chinese).
Zhenwen Zhang, Yan Zhu, Yan Wang, et al. A case of hyperthyroidism complicated with Gitelman syndrome. Chin J Postgraduates of Med 2010;33:76–77. (in Chinese).
Yu Duan, Lan Luo, Chunyu Zhang, et al. Gitelman syndrome combined with primary hypothyroidism. Chin J General Practitioners 2009;8:269–270. (in Chinese).
Ma J, Ren H, Lin L, et al. Genetic features of Chinese patients with Gitelman syndrome: sixteen novel SLC12A3 mutations identified in a new cohort. Am J Nephrol. 2016;44:113–21.
Ren H, Wang WM, Chen XN, et al. Renal involvement and followup of 130 patients with primary Sjogren's syndrome. J Rheumatol. 2008;35:278–84.
Schwarz C, Barisani T, Bauer E, Druml W. A woman with red eyes and hypokalemia: a case of acquired Gitelman syndrome. Wien Klin Wochenschr. 2006;118:239–42.
Chandra AK, Goswami H, Sengupta P. Effects of magnesium on cytomorphology and enzyme activities in thyroid of rats. Indian J Exp Biol. 2014;52:787–92.
Klatka M, Grywalska E, Partyka M, Charytanowicz M, Rolinski J. Impact of methimazole treatment on magnesium concentration and lymphocytes activation in adolescents with Graves' disease. Biol Trace Elem Res. 2013;153:155–70.
Moncayo R, Moncayo H. The WOMED model of benign thyroid disease: acquired magnesium deficiency due to physical and psychological stressors relates to dysfunction of oxidative phosphorylation. BBA Clin. 2015;3:44–64.
Acknowledgments
The authors thank the patient and his family for their participation.
Availability of the data and materials
All data and materials maintaining patient privacy are fully available without restriction. People can request these materials by sending an email to zhouhaiyang4000@163.com.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 81660138).
Author information
Authors and Affiliations
Contributions
HZ, XL, YQ, BM, JZ, and SH diagnosed the patient and performed the investigations and the follow-up. HZ, XL, SL, ZH, and HY analyzed the data. HZ and XL reviewed the literature, drafted the manuscript, and reviewed the manuscript for final publication. YM and ZL critically revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interest
The authors declare that they have no competing interests.
Ethics approval and consent to participate
This study was performed according to the Helsinki Declaration. Written informed consent to participate in the study was obtained from the patient and his mother. The patient’s son was 17 years old, and written informed consent was obtained from him and his parents as legal guardians.
Consent for publication
Written informed consent was obtained from the patient and his mother for publication of the details of the case report. The patient’s son was 17 years old, and written informed consent was obtained from him and his parents as legal guardians.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Zhou, H., Liang, X., Qing, Y. et al. Complicated Gitelman syndrome and autoimmune thyroid disease: a case report with a new homozygous mutation in the SLC12A3 gene and literature review. BMC Endocr Disord 18, 82 (2018). https://doi.org/10.1186/s12902-018-0298-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12902-018-0298-3