Abstract
Background
Bladder cancer (BC) and Renal cell carcinoma (RCC) are the most common urogenital cancers among both sexes, with a yearly global incidence of around 500 000 each. Both BC and RCC have been linked to diabetes. Poor glycemic control (malglycemia) is a serious consequence of diabetes and a possible consequence of systemic treatments used in BC and RCC. The objective of this study was to investigate the prevalence of diabetes and use of hospital-based care for malglycemia in people with BC or RCC.
Methods
This Swedish retrospective population-based register study used national health-data registers for longitudinal data on cancer incidence covering 15 years, use of hospital-based health care, and filled prescriptions of outpatient medications. Study endpoints included co-prevalence of diabetes in individuals with BC/RCC, healthcare resource utilization due to malglycemia, use of systemic corticosteroids, and changes in diabetes management for people with concomitant type 2 diabetes.
Results
We identified 36,620 and 15,581 individuals diagnosed with BC and RCC, respectively, between 2006 and 2019. The proportion of individuals registered with diabetes was 24% in BC and 23% in RCC. An association between BC/RCC and poor glycemic control was found, although the number of malglycemic events in hospital-based care were few (65/59 per 1000 individuals with diabetes and BC/RCC respectively with at least one event). An earlier switch to insulin-based diabetes management was observed in BC/RCC compared to matched individuals with type 2 diabetes but no cancer. The results also indicated an association between steroid treatment and poor glycemic control, and that systemic corticosteroids were more common among people with BC/RCC compared to diabetes controls.
Conclusion
The high prevalence of diabetes and increased use of systemic corticosteroid treatment observed in this large national study highlights the need for specific clinical management, risk-assessment, and monitoring of individuals with BC/RCC and diabetes.
Similar content being viewed by others
Introduction
Bladder cancer (BC) and renal cell carcinoma (RCC) are the two most common genitourinary cancers that affect both sexes. Globally, there are 570,000 new cases of BC and it accounts for 2% of all cancers. The corresponding numbers for RCC are 430,000 and 3% [1]. The highest rates have been observed in North America, Australia, and Europe [2].
Epidemiologic associations with diabetes mellitus have been shown for genitourinary cancers [3,4,5]. People with diabetes had a 50% increased risk of renal cancer regardless of other risk factors in a Swedish population-based retrospective cohort [6]. Links between bladder cancer risk and diabetes vary, with some data indicating associations [7,8,9,10,11]. However, concomitant prevalence of the illnesses in patients is common [12]. According to a population based cross-sectional analysis of cancer patients diagnosed within 3 years of the study, 8–18% of all patients had a coexisting diabetes diagnosis [13]. However, it is not clear whether the association stems from common risk factors such as obesity, ageing or use of specific drugs, or if there is a direct link between the diseases, or some combination [14, 15]. Nevertheless, the growing global prevalence of diabetes, with 537 million adults in 2021 [16], induces an increased focus on population-based research on prevalence and treatment patterns for BC, RCC and concomitant diabetes.
Diabetes in cancer patients is associated with a poorer quality of-life [17], higher all-cause mortality [4, 18] and higher hospitalization rate [19]. In patients with RCC specifically, a previous meta-analysis showed that the presence of both type 1 and type 2 diabetes was associated with poor overall and cancer-specific survival [20]. In patients with non-muscle invasive BC and diabetes a poor glycemic control is associated with disease progression and poor outcomes in terms of diabetes complications [21]. Moreover, people with cancer and diabetes may have a lower adherence to their diabetes medication [22]. This increases the risk for malglycemia, defined here as hypoglycemia, hyperglycemia or glycemic variability. Malglycemia is a serious condition related to an increased risk for diabetes complications and mortality as well as a lower quality of life [23, 24].
In recent decades targeted and immunomodulating cancer therapies such as the widely used anti-angiogenic tyrosine kinase inhibitors (TKI) and immune checkpoint inhibitors (ICI) have been introduced in the treatment of advanced stages of BC and RCC [25, 26]. For both classes of drugs, endocrine side effects have been reported [27]. Anti-angiogenic TKIs used in RCC may affect glucose metabolism and insulin signaling [27, 28], with both hypo- and hyperglycemia as reported side effects [29, 30]. ICIs may also impact the endocrine system through mechanisms that are currently not completely understood [27]. As a consequence, a new spectrum of immune-mediated adverse events including glycemic alterations, and even autoimmune type-1 diabetes, may affect cancer patients treated with ICI therapy [31]. Notably, ICI-induced toxicity is generally managed by administration of high dose corticosteroids [32, 33]. Beyond this role, systemic corticosteroids have a broad use in cancer treatment but can also increase the risk for hyperglycemia in people with and without diabetes [32]. Therefore, malglycemia may be worth specific attention in these cancer populations, whether as a comorbidity, a direct adverse event of a treatment or indirect consequence due to toxicity management. Studies investigating the magnitude of this problem and the related healthcare utilization are needed.
In Sweden, the large number of health data registers run by the National Board of Health and Welfare (NBHW) provides unique opportunities for longitudinal research. These highly qualitative registers with a long history constitute the foundation of a successful Swedish research tradition in the field of clinical epidemiology, and cover health data for the entire population. Combining data from these registers creates an opportunity to link incidence of cancer to health care resource utilization on an individual level.
The primary objective of this study was to investigate the co-prevalence of diabetes (either type 1 or type 2 diabetes) in people with BC or RCC in Sweden and health care resource utilization due to malglycemia. The secondary objective was to explore patterns of systemic corticosteroids use in people with BC or RCC, and changes in diabetes management for those with type 2 diabetes.
Materials and methods
This is a retrospective, longitudinal, population-based register study. The study dataset included longitudinal data on cancer incidence covering 15 years, use of hospital-based health care (visits in outpatient specialist care and inpatient admissions), and filled prescriptions of outpatient medications. The main study period included incident cancers between 2006 and 2019, with additional retrospective information on diabetes diagnoses from 1997 and onwards. Observational individual-level data covered the period January 1, 2006 to December 31, 2020.
The study used three health data registers at the NBHW in Sweden: the Swedish Cancer Register (SCR), the National Patient Register (NPR), and the National Prescribed Drug Register (NPDR). It also used demographic information from the Register of the Total Population (RTB) at Statistics Sweden.
Study population
This longitudinal study contains a study population of patients diagnosed with BC or RCC, respectively, as well as a sub-population diagnosed with type 1 or type 2 diabetes before cancer diagnosis together with matched controls. Data were record linked using personal identity numbers. A more detailed description of register sources and study database can be found in the Supplementary A. The persons were followed from the date they received their cancer diagnosis until end of the study period, emigration or death, which ever came first and then censored.
People with BC were included based on a registration in the SCR with a first time International Classification of Diseases and Related Health Problems version 10 (ICD-10) code C67 between 2006 and 2019. Correspondingly, the RCC population was defined as a first time ICD-10 code C64.
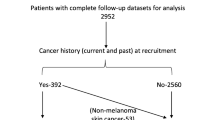
Diabetes together with its index date were defined as any registration of ICD-10 codes E10, E11 or E14 in inpatient or specialized outpatient care in the NPR (1997–2019) or filled prescriptions of glucose lowering medication (ATC code A10) in the NPDR (2005–2019). Using this information, a proportion of people with BC or RCC were classified with diabetes and given a diabetes index date. The subset of individuals that developed diabetes before they were diagnosed with cancer were matched 1:5 for control persons from a total diabetes population on year of birth, sex, and year of index date for diabetes. People with diabetes were further categorized as having type 1 or type 2 diabetes using information from the NPR and NPDR. More information on population selection criteria is reported in Supplementary B.
Study endpoints
The study analyzed four endpoints (two primary and two secondary) for people with BC or RCC (cancer for short in the following). The primary endpoints were:
-
1.
Co-prevalence of cancer and diabetes.
-
2.
The incidence of poor glycemic control defined as the fraction of cancer cohorts with health care use related to malglycemia with reference to patterns in controls with diabetes but no cancer.
The co-prevalence of cancer and diabetes was defined as the fraction of the total population diagnosed with cancer years 2006–2019 that at the time of cancer diagnosis (also referred to as cancer index date) had, or subsequently developed diabetes during study follow-up. Health care use related to malglycemia was defined as hospitalizations or outpatient specialist visits with hypoglycemia or hyperglycemia as main or secondary diagnosis (ICD-10 codes E160, E161, E162 or R739). The primary endpoints are reported for the whole study population with cancer. The second primary endpoint is also reported for the subgroup of individuals with diabetes before they were diagnosed with cancer compared to matched diabetes controls.
The secondary endpoints of this study were:
-
3.
The use of systemic corticosteroid treatment and its association with health care use related to malglycemia.
-
4.
The change in diabetes management as measured by newly prescribed insulin in people with type 2 diabetes and cancer (type 1 diabetes need insulin by default).
The use of systemic corticosteroid was defined as ≥ 1 filled prescription of any drug with the ATC-code H02AB. Endpoint 3 is reported for the whole population of people with cancer. Endpoint 4 is reported for the subgroup of individuals with cancer and type 2 diabetes who were not using insulin at the time of diagnosis of cancer. Results were compared to that of matched diabetes controls.
Statistical analysis
Baseline characteristics for all individuals were summarized using standard descriptive measures. This included number and proportion for categorical variables and mean with standard deviation, or median with interquartile range (IQR) for continuous variables. Endpoints were analyzed using the following methods:
The co-prevalence of cancer and diabetes (endpoint 1) was reported as the proportion with observed diabetes before the cancer index-date, as diabetes at any time during the study period, and as type 2 diabetes after the cancer diagnosis. The incidence of poor glycemic control (endpoint 2) was reported as rates per 1,000 individuals and rates per 10,000 person-years, for comparison between study groups and generalizability to other populations.
Endpoint 3, the use of systemic corticosteroid treatment and its association with health care use related to malglycemia, was described by the cumulative number of events per 1000 persons after first observed filled prescription of systemic corticosteroids following cancer diagnosis for BC or RCC with diabetes. This was compared to matched controls with diabetes but without cancer. Cox proportional hazard regression analysis was used to explore time to first hospitalization due to poor glycemic control after cancer diagnosis and its associations with systemic corticosteroid treatment. The analysis was performed controlling for sex, age, diabetes, and spread of cancer at diagnosis measured by presence of metastases according to the American Joint Committee on Cancer (AJCC) TNM staging system [34]. More information of the classification of malignant tumors can be found in Supplementary B.
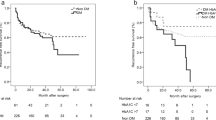
The time to start of insulin-based diabetes treatment (endpoint 4) was analyzed in people with BC or RCC and type 2 diabetes and compared with matched controls with no cancer but with type 2 diabetes using Kaplan–Meier analysis. The equality of survivor functions was tested using a logrank test. Methodological considerations are included in Supplementary A.
A sensitivity analysis explored the impact on results of a broader inclusion of malignancies affecting the urinary tract (ICD 10 codes C66, C67, and C68), which did not alter the results. These results are available on request from the corresponding author.
Data were analyzed using STATA MC version 15.1 and R version 4.2.0 with the survival and dplyr packages.
Results
The study population consisted of 36,620 individuals diagnosed with BC and 15,581 individuals diagnosed with RCC between 2006 and 2019. The national incidence of BC and RCC between 2006 and 2019 by gender, age-group and diabetes status are presented in Supplementary C Table S.1. More men than women had BC (75% men) and RCC (63% men). Descriptive statistics are presented in Table 1.
For BC, the total number of person-years between 2006 and 2020 was 446,225 of which 200,782 occurred after the cancer diagnosis (45%). Corresponding numbers for RCC was 192,186 person-years, of which 87,871 occurred after the cancer diagnosis (46%). The mean follow-up was 5.5 years for BC (IQR: 2 to 8 years) and 5.6 years for RCC (IQR: 2 to 8 years). The median follow-up was 4 years for BC and 5 years for RCC. Supplementary figures S.3 (BC) and S.4 (RCC) show population flowcharts for people with cancer and diabetes including exclusions due to emigration and the number of deaths observed in subgroups. Individuals with the same date registered for cancer diagnosis and death (BC n = 131, 0.4%; RCC n = 396, 2.5%) were censored in the time to event analyzes. In total, 19,237 persons with BC and 8,832 persons with RCC were alive and resident in Sweden at the end of the study period (31st of December 2020).
The proportion of individuals registered with diabetes at any time during the study period were similar among persons with BC (23%, n = 8,279) and RCC (24%, n = 3,752), as shown in Table 1. It was more common to be diagnosed with diabetes before the cancer diagnosis, with some differences between men and women. In the BC group, 18% of men and 12% of women had a registered diagnosis of diabetes before cancer diagnosis. For RCC, the corresponding numbers were 18 vs 16%. Baseline characteristics divided by gender are presented in Supplementary C, Table S.2 and S.3.
Resource utilization in outpatient and inpatient hospital-based care due to poor glycemic control is presented in Table 2. These results include visits or admissions with a main or secondary diagnosis associated with malglycemia registered after cancer index date for the study population and diabetes controls. The subgroup with cancer and diabetes included only individuals with pre-existing diabetes at the time of cancer index date. More information on individuals with diabetes diagnosis after cancer diagnosis is presented in Supplementary C Table S.4. The results in Table 2 show a significantly larger resource utilization of hospital-based care due to poor glycemic control among people with diabetes and cancer compared to diabetes controls. The number of individuals with at least one visit or admission due to poor glycemic control in hospital-based care per 1000 individuals with diabetes were 59 in the BC group and 65 in the RCC group. This can be compared with 47 and 52 per 1000 individuals for the diabetes controls of BC and RCC, respectively. Time to malglycemic event after cancer diagnosis for the BC and RCC group by diabetes and tumor status is further illustrated in Tables S.5/6 and figure S.5-S.10 in Supplementary C and D.
The association between poor glycemic control and different person characteristics, both at baseline and over time, were further explored in a Cox regression (see Table 3). As expected, having a diabetes diagnosis significantly increased the risk of experiencing an event of malglycemia requiring hospital-based care as main or secondary diagnosis for both the BC and RCC group. For RCC, a more advanced tumor status at diagnosis had a significant impact on malglycemic events. A similar pattern was observed for the BC group, but the association was not significant. The use of steroid treatment, captured by filled prescriptions of systemic corticosteroids, was significantly associated with events of poor glycemic control for patients with and without diabetes in both the BC and RCC group, as well as diabetes controls.
About half of the persons with cancer had been treated with steroids at any time during the study period, before or after cancer index date (see Table 1). Further analysis investigated steroid treatment patterns after cancer diagnosis in association with poor glycemic control, presented in Table 4 and in Figures S.11-S.13 in Supplementary D. The number of individuals per 1000 with at least one filled prescription of systemic corticosteroids after cancer index date were 458 in the BC group with diabetes compared with 247 among the matched diabetes controls. The corresponding figures were 405 for the RCC group compared with 256 for matched diabetes controls. The proportion of individuals with filled prescriptions of systemic corticosteroids were significantly larger among study persons with cancer and diabetes compared to diabetes controls. This was also the case for individuals with filled prescriptions of systemic corticosteroids and at least one visit or admission for malglycemia (24 and 36 per 1000 individuals in the BC and RCC groups with diabetes, respectively, compared with 17 and 20 per 1000 individuals in the control groups for BC and RCC, respectively). The number per 1000 individuals with malglycemic events within two years from systemic corticosteroid treatment after cancer index date were 11 in the BC group with diabetes and 15 in the RCC group with diabetes, which was significantly larger compared to diabetes controls with systemic corticosteroid treatment.
Cumulative events of malglycemia registered in hospital-based care after cancer index date and filled prescriptions of systemic corticosteroids are presented in Figs. 1 and 2. The cumulative events are presented for the BC and RCC group with diabetes together with diabetes controls for the study period. The decreasing number at risk during the study period is due to limited follow-up for some individuals and time of death. Each bar represents the cumulative number of malglycemic events per 1000 individuals still in follow-up at that specific time. The figures illustrate a higher rate of malglycemic events within the first years after systemic corticosteroid treatment for people with diabetes and cancer compared to diabetes controls. There is a shift during the last years of follow-up where the cumulative events of malglycemia were higher among diabetes controls. This is probably due to few individuals remaining in the cancer group, which is illustrated by the number at risk.
Cumulative number of malglycemic events per 1,000 persons (prevalence) after first observed filled prescription of steroids after cancer diagnosis among persons with BC. The events shown in the figure are weighted to represent events per 1,000 persons fulfilling these criteria and still in follow-up in the given year
Cumulative number of malglycemic events per 1,000 persons (prevalence) after first observed filled prescription of steroids after cancer diagnosis among persons with RCC. The events shown in the figure are weighted to represent events per 1,000 persons fulfilling these criteria and still in follow-up in the given year
Figures 3 and 4 present survival time analyzes of time to start of insulin-based therapy for patients with type 2 diabetes and BC or RCC. People with cancer and type 2 diabetes were compared with type 2 diabetes controls. The analysis started at the diagnosis of cancer for the cases and only include individuals with type 2 diabetes with no insulin treatment at that time. Two other study setups are included in Supplementary D: time from 1997 with first observed diabetes (Figure S.14-S.15) and starting on July 1, 2005 when the Swedish prescription register where introduced (Figure S.16-S.17). The results show a significantly faster increase in the proportion with insulin treatment over time among individuals with cancer and type 2 diabetes compared with type 2 diabetes controls.
Discussion
Findings from previous studies have suggested that cancer can lead to poorer diabetes-related outcomes as well as vice versa [35, 36]. There are several underlying mechanisms that have been proposed to explain the relationship between diabetes and cancer. Hyperglycemia, insulin resistance, elevated insulin, and insulin-like growth factor-1 (IGF-1) levels, inflammatory cytokines, dyslipidemia, increased leptin, and decreased adiponectin have all been attributed to the increased risk of cancer in patients with diabetes [37]. Further oxidative stress through the production of superoxide and reactive oxygen species (ROS) [38, 39] strongly influences the expression of genes and signal transduction pathways that play a crucial role in tumor development [40]. These factors can affect gene expression and signaling pathways involved in tumor growth, as well as interfere with cell proliferation and apoptosis [41] all of which may contribute to a poorer cancer prognosis and outcome.
The increased risk of a worsened diabetes outcome following a cancer diagnosis may partly be attributed to cancer-management interventions. Corticosteroids reduces insulin sensitivity which may cause aggravating hyperglycemia, and chemotherapeutic agents, such as L-asparginase, directly inhibits insulin release. Further, direct cancer effects, such as cancer cachexia is associated with increased insulin resistance and impaired glucose tolerance, and cachexia-associated cytokines, such as tumor necrosis factor and interleukin- 6 are associated with the development of insulin resistance [42].
The proportion of individuals registered with diabetes was 23 and 24% respectively in the BC and RCC Swedish population of this study. As a reference, the prevalence of diabetes in the general population in Sweden is about 7% among adults and 12% among people 65 years and older [43,44,45]. A higher prevalence of diabetes among people with BC and RCC has also been shown in previous studies from Italy and the US [11, 46].
Furthermore, the prevalence of diabetes at diagnosis of both BC and RCC was higher in men compared to women in this study. This seems in line with a higher prevalence of diabetes among males in Sweden, with female representing about 42% to 46% of the total diabetes population [4, 45]. The small difference observed here in the RCC study sample (18 in men and 16% in women) is in line with the proportions reported for the general population. However, previous studies on RCC have reported a higher prevalence of diabetes among women compared to men [46]. Diabetes in women was also reported to confer a significantly greater risk of kidney cancer relative to men [5]. The difference in diabetes occurrence observed for the BC population in this study (18% in men and 12% in women) seems not to be a reflection of the difference in the gender distribution of diabetes in Sweden, pointing possibly to other reasons.
An association between BC/RCC and poor glycemic control was found in this study, although the number of malglycemic events in hospital-based care were few in absolute numbers. The number of events per 1000 individuals was 96 in the BC group with diabetes and 107 in the RCC group with diabetes. The low numbers may indicate that malglycemic events leading to hospital-care is relatively uncommon among patients with BC or RCC. Still, events of poor glycemic control can be serious and even life threating and therefore deserving close attention and management, especially in the context of frail cancer patient populations. A lower adherence to diabetes medication in people with both diabetes and cancer [22] might also have influenced the outcome in terms of malglycemia.
Information on escalation of diabetes management in terms of insulin therapy can increase the understanding of health care utilization due to poor glycemic control over disease duration and time. The results from this study showed that the proportion with insulin treatment increased significantly faster over time among individuals with cancer and type 2 diabetes compared with type 2 diabetes controls. Initiation of insulin-based therapy among individuals with type 2 diabetes may be an indication of poorer glycemic control.
A considerable and increasing proportion of BC and RCC patients receive systemic therapies in the context of their cancer that can directly and indirectly impact glucose and insulin metabolism. Therefore, they may require specific clinical management, risk-assessment and monitoring in this regard. The results also indicated an association between steroid treatment and poor glycemic control. Since a larger share of the BC/RCC group have used steroid treatment compared to controls, this might fully or partially explain the higher prevalence of poor glycemic control among individuals with cancer.
This study used national individual-level data with high coverage [47] and a long follow-up of 15 years, which gives a solid base for analyzing healthcare resource utilization and patient pathways. The study data represent broad BC and RCC populations which include patients in all phases of the disease. This complements studies focusing on patients at later stages of the disease. Data show that people with BC or RCC and concomitant diabetes have higher health care utilization for treatment of malglycemia compared with people with diabetes and no cancer. A limitation of the study data is the lack of information on less severe malglycemic events not requiring hospital-based care and data on steroid treatment used within inpatient care. This may possibly have underestimated the incidence of malglycemia in the study population, but it is likely that most severe cases are captured.
Cancer patients with co-prevalent diabetes are an important group from a health care planning perspective as it will likely increase in the future. Whether or not the positive association with diabetes and the risk of several cancer forms is genuine [15], a growing prevalence of diabetes in the general population [48] implies increased number of people at risk of concomitant disease. Moreover, the incidence of many cancer forms is increasing partly due to screening, improved diagnostics, and an aging population. Thus, it is important to expand the knowledge about patients with concomitant cancer and diabetes including the healthcare utilization linked to the management of this specific patient population.
The present study focused on BC and RCC, two genitourinary malignancies affecting both females and males. These are among the cancer diagnoses where an increasing proportion of patients are getting exposed to oncological treatment that may deserve specific management and attention in the context of a comorbidity such as diabetes. In addition to systemic corticosteroids that cancer patients may often receive, anti-angiogenic TKIs (RCC) and ICIs (both BC and RCC) can, directly or indirectly, impact glycemic equilibrium. In particular, ICIs have recently been introduced in the adjuvant setting for both BC and RCC, expanding the proportion of patients getting the chance to obtain a clinical benefit but also, inevitably, to experience undesired consequences on glycemic control. This study provides prevalence estimates of the Swedish BC and RCC patient populations with diabetes and the impact of malglycemic events on healthcare consumption for these groups. Its time frame mainly consists of the period before the extensive use of targeted and immunomodulating cancer therapies.
A high prevalence of diabetes in individuals with BC or RCC together with increased use of systemic corticosteroid treatment and higher risk for poor glycemic control compared with diabetes controls were observed in this large national study. This highlights the need for specific clinical management, risk-assessment, and monitoring of individuals with BC or RCC, and concomitant diabetes in order to decrease the risk of poorer diabetes and cancer-related outcomes.
Availability of data and materials
Subject-level data from national registers hosted by Swedish national authorities are available for research after formal evaluation of the research protocol by the Swedish Ethical Review Authority and by the respective national authorities providing data. Permission to conduct research are granted on a case by case basis to a limited number of named persons.
Abbreviations
- BC:
-
Bladder cancer
- RCC:
-
Renal cell carcinoma
- TKI:
-
Anti-angiogenic tyrosine kinase inhibitors
- ICI:
-
Immune checkpoint inhibitors
- NBHW; Socialstyrelsen:
-
The National Board of Health and Welfare
- SCR:
-
The Swedish Cancer Register
- NPR:
-
The National Patient Register
- NPDR:
-
The National Prescribed Drug Register
- RTB:
-
The Register of the Total Population
- ICD-10:
-
International Classification of Diseases and Related Health Problems version 10
- IQR:
-
Interquartile range
- AJCC:
-
The American Joint Committee on Cancer
References
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics 2002. CA Cancer J Clin. 2005;55(2):74–108.
Saginala K, Barsouk A, Aluru JS, Rawla P, Padala SA, Barsouk A. Epidemiology of Bladder Cancer. Med Sci (Basel). 2020;8(1):15.
Shikata K, Ninomiya T, Kiyohara Y. Diabetes mellitus and cancer risk: review of the epidemiological evidence. Cancer Sci. 2013;104(1):9–14.
Bjornsdottir HH, Rawshani A, Rawshani A, Franzén S, Svensson A-M, Sattar N, et al. A national observation study of cancer incidence and mortality risks in type 2 diabetes compared to the background population over time. Sci Rep. 2020;10:17376.
Ohkuma T, Peters SAE, Woodward M. Sex differences in the association between diabetes and cancer: a systematic review and meta-analysis of 121 cohorts including 20 million individuals and one million events. Diabetologia. 2018;61(10):2140–54.
Lindblad P, Chow WH, Chan J, Bergström A, Wolk A, Gridley G, et al. The role of diabetes mellitus in the aetiology of renal cell cancer. Diabetologia. 1999;42(1):107–12.
Zhu Z, Zhang X, Shen Z, Zhong S, Wang X, Lu Y, et al. Diabetes mellitus and risk of bladder cancer: a meta-analysis of cohort studies. PLoS ONE. 2013;8(2):e56662.
Fang H, Yao B, Yan Y, Xu H, Liu Y, Tang H, et al. Diabetes mellitus increases the risk of bladder cancer: an updated meta-analysis of observational studies. Diabetes Technol Ther. 2013;15(11):914–22.
Larsson SC, Orsini N, Brismar K, Wolk A. Diabetes mellitus and risk of bladder cancer: a meta-analysis. Diabetologia. 2006;49(12):2819–23.
Cantiello F, Cicione A, Salonia A, Autorino R, De Nunzio C, Briganti A, et al. Association between metabolic syndrome, obesity, diabetes mellitus and oncological outcomes of bladder cancer: a systematic review. Int J Urol. 2015;22(1):22–32.
Turati F, Polesel J, Di Maso M, Montella M, Libra M, Grimaldi M, et al. Diabetes mellitus and the risk of bladder cancer: an Italian case-control study. Br J Cancer. 2015;113(1):127–30.
Edwards BK, Noone AM, Mariotto AB, Simard EP, Boscoe FP, Henley SJ, et al. Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120(9):1290–314.
Ko C, Chaudhry S. The need for a multidisciplinary approach to cancer care. J Surg Res. 2002;105(1):53–7.
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, et al. Diabetes and Cancer: A Consensus Report. CA Cancer J Clin. 2010;60(4):207–21.
Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ. 2015;350:g7607.
International Diabetes Federation (IDF). IDF Diabetes Atlas 10th edition. 2021 [2024–06–25]. Available from: https://www.diabetesatlas.org/en/.
Bowker SL, Pohar SL, Johnson JA. A cross-sectional study of health-related quality of life deficits in individuals with comorbid diabetes and cancer. Health Qual Life Outcomes. 2006;4:17.
Barone BB, Yeh HC, Snyder CF, Peairs KS, Stein KB, Derr RL, et al. Long-term all-cause mortality in cancer patients with preexisting diabetes mellitus: a systematic review and meta-analysis. JAMA. 2008;300(23):2754–64.
Karlin NJ, Kosiorek HE, Castro JC, Cook CB. Risk of hospitalization in patients with diabetes mellitus who have solid-organ malignancy. Future Science. 2016;2(3):FSO129.
Chen L, Li H, Gu L, Ma X, Li X, Gao Y, et al. The Impact of Diabetes Mellitus on Renal Cell Carcinoma Prognosis: A Meta-Analysis of Cohort Studies. Medicine (Baltimore). 2015;94(26):e1055.
Huang W-L, Huang K-H, Huang C-Y, Pu Y-S, Chang H-C, Chow P-M. Effect of diabetes mellitus and glycemic control on the prognosis of non-muscle invasive bladder cancer: a retrospective study. BMC Urol. 2020;20(1):117.
Tan X, Feng X, Chang J, Higa G, Wang L, Leslie D. Oral antidiabetic drug use and associated health outcomes in cancer patients. J Clin Pharm Ther. 2016;41(5):524–31.
Lee SJ, Kim JH, Park SJ, Ock SY, Kwon SK, Choi YS, et al. Optimal glycemic target level for colon cancer patients with diabetes. Diabetes Res Clin Pract. 2017;124:66–71.
Hershey D. Importance of glycemic control in cancer patients with diabetes: Treatment through end of life. Asia Pac J Oncol Nurs. 2017;4(4):313–8.
ESMO. Bladder Cancer Treatment Recommendations. 2020 [2020–08–24]. Available from: https://www.esmo.org/guidelines/genitourinary-cancers/bladder-cancer/eupdate-bladder-cancer-treatment-recommendations.
Escudier B, Porta C, Schmidinger M, Rioux-Leclercq N, Bex A, Khoo V, et al. Renal cell carcinoma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-updagger. Annals of oncology : official journal of the European Society for Medical Oncology. 2019;30(5):706–20.
Shariff AI, Syed S, Shelby RA, Force J, Clarke JM, D’Alessio D, et al. Novel cancer therapies and their association with diabetes. J Mol Endocrinol. 2019;62(2):R187–99.
Fallahi P, Ferrari SM, Elia G, Ragusa F, Paparo SR, Camastra S, et al. THERAPY OF ENDOCRINE DISEASE: Endocrine-metabolic effects of treatment with multikinase inhibitors. Eur J Endocrinol. 2021;184(1):R29–40.
Choueiri TK, Hessel C, Halabi S, Sanford B, Michaelson MD, Hahn O, et al. Cabozantinib versus sunitinib as initial therapy for metastatic renal cell carcinoma of intermediate or poor risk (Alliance A031203 CABOSUN randomised trial): Progression-free survival by independent review and overall survival update. Eur J Cancer. 2018;94:115–25.
Billemont B, Medioni J, Taillade L, Helley D, Meric JB, Rixe O, et al. Blood glucose levels in patients with metastatic renal cell carcinoma treated with sunitinib. Br J Cancer. 2008;99(9):1380–2.
Leiter A, Carroll E, De Alwis S, Brooks D, Shimol JB, Eisenberg E, et al. Metabolic disease and adverse events from immune checkpoint inhibitors. Eur J Endocrinol. 2021;184(6):857–65.
Fong AC, Cheung NW. The high incidence of steroid-induced hyperglycaemia in hospital. Diabetes Res Clin Pract. 2013;99(3):277–80.
Agarwal K, Yousaf N, Morganstein D. Glucocorticoid use and complications following immune checkpoint inhibitor use in melanoma. Clin Med (Lond). 2020;20(2):163–8.
National Cancer Institute (NIH). Cancer Staging. 2022 [2022–06–28]. Available from: https://www.cancer.gov/about-cancer/diagnosis-staging/staging.
Arreskov AB, Olsen MA, Pouplier SS, Siersma V, Andersen CL, Friis S, et al. The impact of cancer on diabetes outcomes. BMC Endocr Disord. 2019;19(1):60.
Lu Y, Tao J. Diabetes Mellitus and Obesity as Risk Factors for Bladder Cancer Prognosis: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2021;12:699732.
Shahid RK, Ahmed S, Le D, Yadav S. Diabetes and Cancer: Risk, Challenges, Management and Outcomes. Cancers (Basel). 2021;13(22):5735.
Yu T, Robotham JL, Yoon Y. Increased production of reactive oxygen species in hyperglycemic conditions requires dynamic change of mitochondrial morphology. Proc Natl Acad Sci U S A. 2006;103(8):2653–8.
Aggeli IK, Theofilatos D, Beis I, Gaitanaki C. Insulin-induced oxidative stress up-regulates heme oxygenase-1 via diverse signaling cascades in the C2 skeletal myoblast cell line. Endocrinology. 2011;152(4):1274–83.
Valko M, Rhodes CJ, Moncol J, Izakovic M, Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact. 2006;160(1):1–40.
Valko M, Leibfritz D, Moncol J, Cronin MT, Mazur M, Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int J Biochem Cell Biol. 2007;39(1):44–84.
Hwangbo Y, Kang D, Kang M, Kim S, Lee EK, Kim YA, et al. Incidence of Diabetes After Cancer Development: A Korean National Cohort Study. JAMA Oncol. 2018;4(8):1099–105.
International Diabetes Federation Europe (IDF). IDF Europe members: Sweden. https://idf.org/our-network/regions-members/2020 [2020–11–02]. Available from: https://idf.org/our-network/regions-members/europe/members/160-sweden.html.
Statistical database. Population statistics year 2020 [Online database accessed 2022–09–08] [database on the Internet]. Statistics Sweden. Available from: https://www.statistikdatabasen.scb.se/pxweb/en/ssd/START__BE__BE0101__BE0101A/BefolkningNy/.
NDR-knappen [in Swedish. Online database accessed 2022–09–08] [database on the Internet]. Swedish National Diabetes Register. Available from: https://www.ndr.nu/#/knappen.
Habib SL, Prihoda TJ, Luna M, Werner SA. Diabetes and risk of renal cell carcinoma. J Cancer. 2012;3:42–8.
Barlow L, Westergren K, Holmberg L, Talback M. The completeness of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48(1):27–33.
Jansson SP, Fall K, Brus O, Magnuson A, Wandell P, Ostgren CJ, et al. Prevalence and incidence of diabetes mellitus: a nationwide population-based pharmaco-epidemiological study in Sweden. Diabet Med. 2015;32(10):1319–28.
Acknowledgements
Not applicable.
Funding
Funding for this study was provided by Pfizer AB, Stockholm, Sweden and Merck AB, Stockholm, Sweden to the Swedish Institute for Health Economics, Lund, Sweden.
Pfizer AB,Merck AB,Stockholm,Sweden
Author information
Authors and Affiliations
Contributions
All authors (EA, GB, FN, AS, JA, PK, KSC) confirm that they meet the International Committee of Medical Journal Editors (ICJME) uniform requirements for authorship and that they have contributed to: design and collection of data; or critical analysis and interpretation of the data; and drafting/critically revising the article. All authors (EA, GB, FN, AS, JA, PK, KSC) share the final responsibility for the content of the manuscript and the decision to submit the manuscript for publication. EA, GB and KSC performed material preparation, data collection and analysis, and wrote the first draft of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Swedish Ethical Review Authority approved of the study (Dnr 2021–00633). The need for informed consent was deemed unnecessary according to national regulations and the Swedish Ethical Review Authority. All experiments were performed in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
FN, AS and JA are employees of Pfizer Inc and may own stock or stock options. EA, GB and KSC are employees of the Swedish Institute for Health Economics. PK no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Andersson, E., Brådvik, G., Nilsson, F.O.L. et al. Prevalence of diabetes and hospitalization due to poor glycemic control in people with bladder cancer or renal cell carcinoma in Sweden. BMC Urol 24, 148 (2024). https://doi.org/10.1186/s12894-024-01536-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-024-01536-2