Abstract
Background
A high level of PD-L1 expression is the most relevant predictive parameter for response to immune checkpoint inhibitor (CPI) therapy in urinary bladder cancer. Existing data on the relationship between PD-L1 expression and the natural course of disease are controversial and sparse.
Methods
To expand our understanding of the relationship between PD-L1 expression and parameters of cancer aggressiveness, PD-L1 was analyzed on tissue microarrays containing 2710 urothelial bladder carcinomas including 512 patients with follow-up data who underwent radical cystectomy and follow-up therapies in the pre-immune checkpoint inhibitor therapy era.
Results
Tumor cell positivity in ≥10% of cells were seen in 513 (20%) and an immune cell positivity occurred in 872 (34%) of 2566 interpretable cancers. PD-L1 positivity in tumor cells increased from pTaG2 low grade (0.9% positive) to pTaG3 high grade (4.1%; p = 0.0255) and was even higher in muscle-invasive (pT2–4) carcinomas (29.3%; p < 0.0001). However, within pT2–4 carcinomas, PD-L1 positivity was linked to low pT stage (p = 0.0028), pN0 (p < 0.0001), L0 status (p = 0.0005), and a better prognosis within 512 patients with cystectomy who never received CPIs (p = 0.0073 for tumor cells and p = 0.0086 for inflammatory cells). PD-L1 staining in inflammatory cells was significantly linked to PD-L1 staining in tumor cells (p < 0.0001) and both were linked to a positive p53 immunostaining (p < 0.0001).
Conclusion
It cannot be fully excluded that the strong statistical link between PD-L1 status and favorable histological tumor features as well as better prognosis could influence the outcome of studies evaluating CPIs in muscle-invasive urothelial carcinoma.
Similar content being viewed by others
Background
Urothelial carcinoma of the urinary bladder belongs to the ten most common malignant cancer types worldwide [1]. About 80% of patients present with non-invasive low-grade (pTa) or minimally invasive (pT1) stage urothelial bladder carcinomas. These carcinomas are characterized by a good prognosis and can be treated by transurethral resection. The treatment of patients with muscle-invasive urothelial carcinomas usually involves radiotherapy or radical cystectomy and neoadjuvant chemotherapy. Outcome of these patients is variable, but almost 50% develop metastasis and eventually die from their disease [2].
As in many other cancer types, immune checkpoint inhibitors (CPI) have become increasingly important for bladder cancer treatment (summarized in [3]). Atezolizumab, Nivolumab, Pembrolizumab, Avelumab, and Durvalumab have all been FDA approved for treatment of locally advanced or metastatic urothelial carcinoma of the bladder and the upper urinary tract (summarized in [4]). Although CPI are effective in metastatic urothelial bladder cancer, just a small proportion of treated patients will find a clear benefit while a high number of patients will be exposed to potentially significant side effects and toxicity with little improvement of quality of life or survival (summarized in [5]). A high level of programmed cell death 1 Ligand 1 (PD-L1) expression in cancers is the most relevant predictive parameter for response to CPI therapy and therefore used for decision making on whether or not CPI treatment is given [6]. In this context, the relationship of PD-L1 expression with tumor progression or disease outcome in patients not treated by CPIs is of interest. A significant link between PD-L1 expression and the natural history of the disease could influence the perception on the therapeutic success of CPI therapy. Data on this subject are controversial. At least 13 studies on 36–248 patients have analyzed the relationship between PD-L1 expression in either tumor cells or immune cells and parameters of urothelial cancer aggressiveness that were unrelated to CPI therapy and found links between high PD-L1 expression and favorable tumor features [7], unfavorable features [8,9,10,11,12,13] or failed to find relationships to prognostic parameters [14,15,16,17,18,19].
In an attempt to further expand our understanding of the relationship between PD-L1 expression and cancer aggressiveness, we investigated PD-L1 expression by immunohistochemistry (IHC) in a large cohort of 2710 bladder cancer patients including 512 patients with follow-up data who underwent radical cystectomy and follow-up therapies in the pre-CPI era. For optimal standardization, all analyses were done in a tissue microarray (TMA) format.
Materials and methods
Tissue microarrays (TMA)
The TMA method allows the analysis of a large number of molecular-genetic alterations on one TMA set. The TMAs used in this study were first employed in a study on the prognostic role of GATA3 expression in bladder cancer [20]. The TMA set were constructed from one 0.6 mm sample each from 2710 urothelial bladder tumors. The tumors were collected from the Institute of Pathology, University Hospital Hamburg, Germany, Institute of Pathology, Charité Berlin, Germany, Department of Pathology, Academic Hospital Fuerth, Germany, or Department of Pathology, Helios Hospital Bad Saarow, Germany, and/or treated at Department of Urology, University Hospital Hamburg, Germany, Department of Urology, Charité Berlin, Germany, Department of Urology, Helios Hospital Bad Saarow, Germany, Department of Urology, Albertinen Hospital, Hamburg, Germany, and Department of Urology and Urological Oncology, Pomeranian Medical University, Szczecin, Poland. Patients with pTa/pT1 disease were treated by transurethral bladder tumor resection with or without postoperative or adjuvant instillation therapy. Patients with pT2 carcinomas on the biopsy were treated by radical cystectomy, out of which 462 were pT2, 615 were pT3, and 298 were pT4. Available clinical follow up data and histopathological data were grade, tumor stage (pT), status of venous (V) and lymphatic (L) invasion, and lymph node status (pN) (Table 1), as well as clinical follow up data (overall survival; OS: time between cystectomy and death) from 512 patients with pT2–4 carcinomas treated by cystectomy (median: 13 months; range: 1–141 months) who had either died or appeared for their last follow-up visit before the approval of the first CPI for bladder cancer therapy (2017) in Germany and in Poland. The grading of pTa tumors included both a classification according to WHO 2004 [21] and Mostofi 1973 [22] which were valid at the time of the respective diagnoses. A centralized review of the cases was not done. Data on p53 immunostaining were available from a previous study [23]. The tissues were fixed in 4% buffered formalin and then embedded in paraffin. The TMA manufacturing process has previously been described in detail [24, 25]. The use of archived remnants of diagnostic tissues for TMA manufacturing, their analysis for research purposes, and patient data were according to local laws (HmbKHG, §12, article 1) and analysis had been approved by the local ethics committee (Ethics commission Hamburg, WF-049/09). All work has been carried out in compliance with the Helsinki Declaration.
Immunohistochemistry
For this study we used identical methods for immunohistochemical evaluation of PD-L1 as previously described [26]. Freshly cut TMA sections were immunostained in one experiment and 1 day. Slides were deparaffinized with xylol, rehydrated through a graded alcohol series, and exposed to heat-induced antigen retrieval for 5 minutes in an autoclave at 121 °C in a pH 7.8 Tris-EDTA-Citrat (TEC) puffer, Endogenous peroxidase activity was blocked with Dako REAL Peroxidase-Blocking Solution (Agilent Technologies, Santa Clara, CA, USA; #S2023) for 10 minutes. Primary antibody specific against PD-L1 protein (recombinant rabbit monoclonal, MS Validated Antibodies, Hamburg, Germany, clone MSVA-711R; #2083-711R) was applied at 37 °C for 60 minutes at a dilution of 1:150. Bound antibody was then visualized using the EnVision Kit (Agilent Technologies, Santa Clara, CA, USA; #K5007) according to the manufacturer’s directions. The sections were counterstained with hemalaun. In tumor cells, a cut-off of ≥10% positive tumor cells defined PD-L1 positivity. In immune cells, PD-L1 staining was semiquantitatively assessed as “negative” (no staining), “few positive” (few cells stained), and “many positive” (many cells stained). Examples of these categorize are shown in supplementary Fig. 1.
Statistics
Statistical calculations were performed with JMP16® software (SAS®, Cary, NC, USA). Contingency tables were created, and Chi2-tests were performed to test for associations between pathological or other molecular parameters and PD-L1 immunostaining. Overall survival curves were calculated according to Kaplan-Meier. The Log-Rank test was applied to detect significant differences between groups and p-value of ≤0.05 was assumed to be statistically significant.
Results
Technical issues
A total of 2566 (95%) of 2710 urothelial carcinomas were interpretable for PD-L1 immunostaining. Non-informative spots were caused by a lack of unequivocal tumor cells on the TMA spots or absence of entire tissue spots on the TMA.
PD-L1 immunohistochemistry in urothelial carcinomas
A membranous staining in ≥10% of cancer cells was seen in 513 (20%) and immune cell staining was seen in 872 (34%) of the 2566 (822 pTa and 1744 pT2–4) interpretable cancers. Representative images are given in Fig. 1.
PD-L1 expression in urothelial carcinomas. The panels show pT2–4 urothelial carcinomas with strong PD-L1 staining in tumor cells only (A), weak PD-L1 staining in tumor cells and prominent positivity in immune cells (B), strong PD-L1 staining in immune cells only (C), and complete absence of PD-L1 staining (D). Examples of pTa tumors show a prominent PD-L1 positivity of peritumoral macrophages (E) and absence of PD-L1 staining (F)
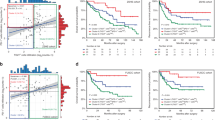
Associations between PD-L1 tumor and immune cell staining and histopathological tumor parameters are shown in Table 2. The rate of PD-L1 positivity in tumor cells increased from pTaG2 low grade (0.9% positive) to pTaG2 high grade (3.2%) and to pTaG3 (4.1%; p = 0.0255), and was even higher in muscle-invasive (pT2–4) carcinomas (2.1% positive for all pTa vs. 29.3% for pT2–4; p < 0.0001). PD-L1 positivity was associated with higher grade in pT2–4 carcinomas (p = 0.0154). However, in these muscle-invasive cancers both tumoral and inflammatory cell PD-L1 positivity was linked to low pT stage (p = 0.0028 for tumoral cells / p = 0.0013 for inflammatory cells), absence of nodal metastasis (p < 0.0001 each), and absence of lymphangiosis carcinomatosa (p = 0.0005 / p = 0.0419). PD-L1 staining in inflammatory cells was significantly linked to PD-L1 staining in tumor cells (Fig. 2a, p < 0.0001). Accordingly, PD-L1 positivity in inflammatory cells was higher in pT2–4 (44.8%) than in pTa tumors (12.5%; p < 0.0001; Table 2). PD-L1 positivity in tumor cells and in inflammatory cells was also significantly associated with a positive p53 immunostaining (p < 0.0001 each; Fig. 2b-c).
To estimate the impact of PD-L1 immunostaining in tumor and inflammatory cells on patient prognosis we analyzed the relationship between PD-L1 immunostaining and OS (time between cystectomy and death) in 512 patients with muscle-invasive carcinomas who had never been treated with CPIs. In these analyses, both PD-L1 positivity in inflammatory and tumor cells was significantly linked to a prolonged OS in comparison to patients with PD-L1 negative tumor and inflammatory cells (p = 0.0073 for tumor cells and p = 0.0086 for inflammatory cells; Fig. 3).
Discussion
Our analysis of PD-L1 staining in more than 2500 urothelial carcinomas provided seemingly controversial results. PD-L1 positivity in both tumor cells and inflammatory cells was linked to high grade of malignancy and invasive tumor growth but – within muscle-invasive cancer – strongly related to features of less aggressive tumor behavior and a better patient prognosis estimated by a longer overall survival.
Earlier studies investigating PD-L1 expression in tumor cells have often focused on muscle-invasive (pT2–4) urothelial carcinomas. Our positivity rate of 29% in pT2-pT4 tumors is in the lower range of published data where PD-L1 positivity ranged from 9 to 88% in studies analyzing 10 to 936 pT2–4 carcinomas [26,27,28,29]. Reasons that are typically considered for discrepant results in IHC studies include different antibodies, staining protocols, and criteria to define positivity [30]. However, for PD-L1, multiple studies have shown that the most commonly used antibodies can all result in similar data within studies [31,32,33,34] and that even the use of laboratory developed PD-L1 tests yield similar results as Food and Drug Administration (FDA) approved companion diagnostics [30]. For the PD-L1 assay used in this study, we had earlier demonstrated a similar staining behavior as for several established PD-L1 antibodies such as clones E1L3N, SP142, and SP263 [26]. It is of note that a high variability of PD-L1 data also exists in studies using the same antibodies [15, 29]. The quantity of tissue analyzed per patient, section age and difficulties in the distinction of intraepithelial or peri-epithelial PD-L1 positive macrophages from true PD-L1 positive cancer cells might also contribute to the data diversity of PD-L1 IHC in the literature [26, 35, 36].
Our rate of 45% of muscle-invasive urothelial carcinomas with detectable PD-L1 positivity in tumor associated immune cells is also in the lower range of the 33 to 74% reported in the literature [7, 26]. Whether PD-L1 expression is more relevant if it occurs in tumor cells or in immune cells is unresolved [37,38,39]. The significant association between PD-L1 positivity in tumor cells and high levels of PD-L1 positive macrophages demonstrates that both mechanisms for immune cell suppression are commonly activated together. Their similar associations with histopathological features also suggest that the biological effect of PD-L1 is not highly dependent of the PD-L1 positive cell types.
PD-L1 positivity in tumor cells was significantly linked to favorable tumor phenotype and better prognosis in pT2–4 carcinomas. This observation is controversial to most findings from earlier studies. Associations of PD-L1 staining in tumor cells with pT, pN, L-status or clinical outcome have been analyzed in at least 8 cohorts of muscle-invasive urothelial cell carcinomas [7, 8, 10, 14, 40,41,42,43]. Only one of these studies have identified significant associations between PD-L1 positivity and favorable tumor parameters (low pT and absence of nodal metastasis) in a cohort of 139 urothelial carcinomas [7]. One additional study showed prolonged overall survival for tumors with PD-L1 positive tumor cells in a subset of 156 pTa to pT4 carcinomas that were not treated by CPI [44]. However, five other studies did not find a relationship between PD-L1 status and tumor aggressiveness in cohorts of 64 to 96 carcinomas [14, 40,41,42,43], and two further studies even reported a link between high PD-L1 levels and histological parameters of aggressive urothelial cancers in 236 and 248 carcinomas [8, 10]. It is of note that PD-L1 positivity has also been linked to favorable tumor features and good prognosis (in the absence of CPI therapy) in other tumor entities such as for example oral and lung squamous cell carcinomas [45, 46], and gastric cancer [47]. In contrast, most studies on kidney [48], breast [49], lung [50], and colorectal cancer [51] have linked PD-L1 positivity to adverse prognosis and unfavorable tumor features.
The strong association between p53 positivity and PD-L1 staining found in this study is in line with reports describing a similar link in other tumor entities such as for example triple negative breast cancer [52], endometrial cancer [53], hepatocellular carcinoma [54], and oral squamous cell carcinomas [55]. p53 is known to play an important role in DNA damage pathways, which also belong to the relevant mechanisms inducing up-regulation of PD-L1 expression (summarized in [56]). Cortez et al. [57] suggested a possible mechanism, as they described an influence of p53 on PD-L1 expression via the microRNA miR-34 and observed that tumors with TP53 mutations had low miR-34 expression but higher PD-L1 levels. Another potential explanation lies in the high level of genomic instability in TP53 mutated tumors which is typically linked to high level nuclear atypia, a high mutation rate and – consequently – higher immunogenicity of tumor cells [58]. Elevated immunogenicity of tumor cells could lead to a relevant immune response that causes a lower pT stage and fewer metastases although a fraction of these tumors upregulate PD-L1 in an attempt to evade the immune response (summarized in [59]). Such a scenario could also explain the seemingly paradoxical link of PD-L1 expression with high grade (severe nuclear atypia are reflective of high genomic instability and high mutation rate) and low pT/pN stage, possibly caused by effects of the immune response which is only incompletely suppressed by tumoral PD-L1 expression.
The very low rate of PD-L1 positivity in tumor cells seen in pTa tumors (2% PD-L1 positive) in this study is consistent with results from our earlier study investigating PD-L1 expression across 118 different tumor entities, and data from Inman et al. [10, 26]. In these studies, on 44 and 426 pTa tumors PD-L1 staining was found in 2 and 7% of all pTa tumors. The much lower rate of PD-L1 positivity in non-invasive than invasive urothelial carcinomas may be due to the rather limited interaction of pTa tumor cells with the immune system, as these cells are separated from the tumor associated stroma by a basal membrane.
Our study also suffers from limitations. The number of tumors examined is still too small. Especially when investigating subgroups such as muscle-invasive tumors without CPI, a higher number of cases than 512 would be desirable. Further limitations are the lack of information’s about additional tumor treatment (e.g. adjuvant or neoadjuvant chemotherapy), the retrospective nature of our analysis, and the absence of standardized continuous clinical follow-up evaluation of our patients. Future international collaborative studies should be designed to evaluate the role of PD-L1 in larger cohorts of urothelial carcinomas.
Conclusion
The data of this large-scale study demonstrate a seemingly paradoxical link between PD-L1 positivity, high grade, and invasive tumor growth while PD-L1 positivity is tightly related to favorable tumor features and better prognosis within the clinically most relevant group of pT2–4 carcinomas. Therefore, it cannot be fully excluded that a link between PD-L1 status and the natural course of the disease may potentially influence the outcome of studies evaluating CPIs.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available from the corresponding author on request.
Abbreviations
- CPI:
-
Immune checkpoint inhibitor
- FDA:
-
Food and Drug Administration
- IHC:
-
Immunohistochemistry
- L:
-
Lymphatic invasion
- pT:
-
Pathological tumor stage
- TMA:
-
Tissue microarray
- OS:
-
Overall survival
- PD-L1:
-
Programmed cell death 1 Ligand 1
- pN:
-
Pathological lymph node status
- V:
-
Venous invasion
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Knowles MA, Hurst CD. Molecular biology of bladder cancer: new insights into pathogenesis and clinical diversity. Nat Rev Cancer. 2015;15(1):25–41.
Shiravand Y, Khodadadi F, Kashani SMA, Hosseini-Fard SR, Hosseini S, Sadeghirad H, Ladwa R, O'Byrne K, Kulasinghe A. Immune checkpoint inhibitors in Cancer therapy. Curr Oncol. 2022;29(5):3044–60.
Twomey JD, Zhang B. Cancer immunotherapy update: FDA-approved checkpoint inhibitors and companion diagnostics. AAPS J. 2021;23(2):39.
Kwon WA, Seo HK. Emerging agents for the treatment of metastatic urothelial cancer. Investig Clin Urol. 2021;62(3):243–55.
Ding X, Chen Q, Yang Z, Li J, Zhan H, Lu N, Chen M, Yang Y, Wang J, Yang D. Clinicopathological and prognostic value of PD-L1 in urothelial carcinoma: a meta-analysis. Cancer Manag Res. 2019;11:4171–84.
Wahlin S, Nodin B, Leandersson K, Boman K, Jirstrom K. Clinical impact of T cells, B cells and the PD-1/PD-L1 pathway in muscle invasive bladder cancer: a comparative study of transurethral resection and cystectomy specimens. Oncoimmunology. 2019;8(11):e1644108.
Wang B, Pan W, Yang M, Yang W, He W, Chen X, Bi J, Jiang N, Huang J, Lin T. Programmed death ligand-1 is associated with tumor infiltrating lymphocytes and poorer survival in urothelial cell carcinoma of the bladder. Cancer Sci. 2019;110(2):489–98.
Nakanishi J, Wada Y, Matsumoto K, Azuma M, Kikuchi K, Ueda S. Overexpression of B7-H1 (PD-L1) significantly associates with tumor grade and postoperative prognosis in human urothelial cancers. Cancer Immunol Immunother. 2007;56(8):1173–82.
Inman BA, Sebo TJ, Frigola X, Dong H, Bergstralh EJ, Frank I, Fradet Y, Lacombe L, Kwon ED. PD-L1 (B7-H1) expression by urothelial carcinoma of the bladder and BCG-induced granulomata: associations with localized stage progression. Cancer. 2007;109(8):1499–505.
Bellmunt J, Mullane SA, Werner L, Fay AP, Callea M, Leow JJ, Taplin ME, Choueiri TK, Hodi FS, Freeman GJ, et al. Association of PD-L1 expression on tumor-infiltrating mononuclear cells and overall survival in patients with urothelial carcinoma. Ann Oncol. 2015;26(4):812–7.
Al Nabhani S, Al Harthy A, Al Riyami M, Al Sinawi S, Al Rashdi A, Al Husseni S, Kumar S. Programmed death-ligand 1 (PD-L1) expression in bladder Cancer and its correlation with tumor grade, stage, and outcome. Oman Med J. 2022;37(6):e441.
Davick JJ, Frierson HF, Smolkin M, Gru AA. PD-L1 expression in tumor cells and the immunologic milieu of bladder carcinomas: a pathologic review of 165 cases. Hum Pathol. 2018;81:184–91.
Chen X, Chen H, Lin R, Li Y, Guo Y, Chen Q, Zhang Y, Cai G, Hu M, Chen G. Correlation between PD-L1 expression of the tumour cells and lymphocytes infiltration in the invasive front of urothelial carcinoma. J Clin Pathol. 2022;
Grantzau T, Toft BG, Melchior LC, Elversang J, Stormoen DR, Omland LH, Pappot H. PD-L1 expression and FGFR-mutations among Danish patients diagnosed with metastatic urothelial carcinoma: a retrospective and descriptive study. APMIS. 2022;130(8):498–506.
Mahmoud AM, Frank I, Orme JJ, Lavoie RR, Thapa P, Costello BA, Cheville JC, Gupta S, Dong H, Lucien F. Evaluation of PD-L1 and B7-H3 expression as a predictor of response to adjuvant chemotherapy in bladder cancer. BMC Urol. 2022;22(1):90.
Faraj SF, Munari E, Guner G, Taube J, Anders R, Hicks J, Meeker A, Schoenberg M, Bivalacqua T, Drake C, et al. Assessment of tumoral PD-L1 expression and intratumoral CD8+ T cells in urothelial carcinoma. Urology. 2015;85(3):703 e701–6.
de Jong JJ, Stoop H, Nieboer D, Boormans JL, van Leenders G. Concordance of PD-L1 expression in matched urothelial bladder cancer specimens. Histopathology. 2018;73(6):983–9.
Nechifor-Boila IA, Loghin A, Nechifor-Boila A, Decaussin-Petrucci M, Voidazan S, Chibelean BC, Martha O, Borda A. PD-L1 Expression in Muscle Invasive Urothelial Carcinomas as Assessed via Immunohistochemistry: Correlations with Specific Clinical and Pathological Features, with Emphasis on Prognosis after Radical Cystectomy. Life (Basel). 2021;11(5)
Plage H, Samtleben H, Hofbauer S, Kornienko K, Weinberger S, Bruch PG, Elezkurtaj S, Roßner F, Schallenberg S, Kluth M, et al. GATA3 expression loss is linked to stage progression but is unrelated to prognosis in muscle-invasive urothelial carcinoma of the bladder. Hum Pathol. 2022;
Eble JN, Organization WH, Cancer IAfRo. Pathology and genetics of Tumours of the urinary system and male genital Organs. IARC Press; 2004.
Mostofi FK. International histological classification of Tumours - histological typing of urinary bladder Tumours. World Health Organization; 1973.
Schallenberg S, Plage H, Hofbauer S, Furlano K, Weinberger S, Bruch PG, Rossner F, Elezkurtaj S, Kluth M, Lennartz M, et al. Altered p53/p16 expression is linked to urothelial carcinoma progression but largely unrelated to prognosis in muscle-invasive tumors. Acta Oncol. 2023;62(12):1880–9.
Bubendorf L, Nocito A, Moch H, Sauter G. Tissue microarray (TMA) technology: miniaturized pathology archives for high-throughput in situ studies. J Pathol. 2001;195(1):72–9.
Kononen J, Bubendorf L, Kallioniemi A, Bärlund M, Schraml P, Leighton S, Torhorst J, Mihatsch MJ, Sauter G, Kallioniemi OP. Tissue microarrays for high-throughput molecular profiling of tumor specimens. Nat Med. 1998;4(7):844–7.
Moller K, Knoll M, Bady E, Schmerder MJ, Rico SD, Kluth M, Hube-Magg C, Blessin NC, Mandelkow T, Lennartz M, et al. PD-L1 expression and CD8 positive lymphocytes in human neoplasms: a tissue microarray study on 11,838 tumor samples. Cancer Biomark. 2023;36(2):177–91.
Brunelli M, Tafuri A, Cima L, Cerruto MA, Milella M, Zivi A, Buti S, Bersanelli M, Fornarini G, Vellone VG, et al. MDM2 gene amplification as selection tool for innovative targeted approaches in PD-L1 positive or negative muscle-invasive urothelial bladder carcinoma. J Clin Pathol. 2022;75(1):39–44.
Holland BC, Sood A, Delfino K, Dynda DI, Ran S, Freed N, Alanee S. Age and sex have no impact on expression levels of markers of immune cell infiltration and immune checkpoint pathways in patients with muscle-invasive urothelial carcinoma of the bladder treated with radical cystectomy. Cancer Immunol Immunother. 2019;68(6):991–7.
Kintsler S, Cassataro MA, Drosch M, Holenya P, Knuechel R, Braunschweig T. Expression of programmed death ligand (PD-L1) in different tumors. Comparison of several current available antibody clones and antibody profiling. Ann Diagn Pathol. 2019;41:24–37.
Torlakovic E, Lim HJ, Adam J, Barnes P, Bigras G, Chan AWH, Cheung CC, Chung JH, Couture C, Fiset PO, et al. "interchangeability" of PD-L1 immunohistochemistry assays: a meta-analysis of diagnostic accuracy. Mod Pathol. 2020;33(1):4–17.
Shi L, Zhang SJ, Chen J, Lu SX, Fan XJ, Tong JH, Chow C, Tin EK, Chan SL, Chong CC, et al. A comparability study of immunohistochemical assays for PD-L1 expression in hepatocellular carcinoma. Mod Pathol. 2019;32(11):1646–56.
Pinato DJ, Mauri FA, Spina P, Cain O, Siddique A, Goldin R, Victor S, Pizio C, Akarca AU, Boldorini RL, et al. Clinical implications of heterogeneity in PD-L1 immunohistochemical detection in hepatocellular carcinoma: the blueprint-HCC study. Br J Cancer. 2019;120(11):1033–6.
Buttner R, Gosney JR, Skov BG, Adam J, Motoi N, Bloom KJ, Dietel M, Longshore JW, Lopez-Rios F, Penault-Llorca F, et al. Programmed death-ligand 1 immunohistochemistry testing: a review of analytical assays and clinical implementation in non-small-cell lung Cancer. J Clin Oncol. 2017;35(34):3867–76.
Ratcliffe MJ, Sharpe A, Midha A, Barker C, Scott M, Scorer P, Al-Masri H, Rebelatto MC, Walker J. Agreement between programmed cell death Ligand-1 diagnostic assays across multiple protein expression cutoffs in non-small cell lung Cancer. Clin Cancer Res. 2017;23(14):3585–91.
Mirlacher M, Kasper M, Storz M, Knecht Y, Durmuller U, Simon R, Mihatsch MJ, Sauter G. Influence of slide aging on results of translational research studies using immunohistochemistry. Mod Pathol. 2004;17(11):1414–20.
Torhorst J, Bucher C, Kononen J, Haas P, Zuber M, Kochli OR, Mross F, Dieterich H, Moch H, Mihatsch M, et al. Tissue microarrays for rapid linking of molecular changes to clinical endpoints. Am J Pathol. 2001;159(6):2249–56.
Trimble P, Walleck C. Trauma nursing: past, present, and future. Md Med J. 1988;37(7):547–50.
Chen DS, Mellman I. Elements of cancer immunity and the cancer-immune set point. Nature. 2017;541(7637):321–30.
Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39(1):1–10.
Baras AS, Drake C, Liu JJ, Gandhi N, Kates M, Hoque MO, Meeker A, Hahn N, Taube JM, Schoenberg MP, et al. The ratio of CD8 to Treg tumor-infiltrating lymphocytes is associated with response to cisplatin-based neoadjuvant chemotherapy in patients with muscle invasive urothelial carcinoma of the bladder. Oncoimmunology. 2016;5(5):e1134412.
Erlmeier F, Seitz AK, Hatzichristodoulou G, Stecher L, Retz M, Gschwend JE, Weichert W, Kubler HR, Horn T. The role of PD-L1 expression and Intratumoral lymphocytes in response to perioperative chemotherapy for urothelial carcinoma. Bladder Cancer. 2016;2(4):425–32.
Necchi A, Lo Vullo S, Giannatempo P, Raggi D, Perrone F, Nicolai N, Catanzaro M, Biasoni D, Torelli T, Piva L, et al. Association of Androgen Receptor Expression on tumor cells and PD-L1 expression in muscle-invasive and metastatic urothelial carcinoma: insights for clinical research. Clin Genitourin Cancer. 2018;16(2):e403–10.
Pichler R, Fritz J, Lackner F, Sprung S, Brunner A, Horninger W, Loidl W, Pircher A, Heidegger I. Prognostic value of testing PD-L1 expression after radical cystectomy in high-risk patients. Clin Genitourin Cancer. 2018;16(5):e1015–24.
Tretiakova M, Fulton R, Kocherginsky M, Long T, Ussakli C, Antic T, Gown A. Concordance study of PD-L1 expression in primary and metastatic bladder carcinomas: comparison of four commonly used antibodies and RNA expression. Mod Pathol. 2018;31(4):623–32.
Cooper WA, Tran T, Vilain RE, Madore J, Selinger CI, Kohonen-Corish M, Yip P, Yu B, O'Toole SA, McCaughan BC, et al. PD-L1 expression is a favorable prognostic factor in early stage non-small cell carcinoma. Lung Cancer. 2015;89(2):181–8.
Kogashiwa Y, Yasuda M, Sakurai H, Nakahira M, Sano Y, Gonda K, Ikeda T, Inoue H, Kuba K, Oba S, et al. PD-L1 expression confers better prognosis in locally advanced Oral squamous cell carcinoma. Anticancer Res. 2017;37(3):1417–24.
Wu Y, Cao D, Qu L, Cao X, Jia Z, Zhao T, Wang Q, Jiang J. PD-1 and PD-L1 co-expression predicts favorable prognosis in gastric cancer. Oncotarget. 2017;8(38):64066–82.
Moller K, Fraune C, Blessin NC, Lennartz M, Kluth M, Hube-Magg C, Lindhorst L, Dahlem R, Fisch M, Eichenauer T, et al. Tumor cell PD-L1 expression is a strong predictor of unfavorable prognosis in immune checkpoint therapy-naive clear cell renal cell cancer. Int Urol Nephrol. 2021;53(12):2493–503.
Zhang M, Sun H, Zhao S, Wang Y, Pu H, Wang Y, Zhang Q. Expression of PD-L1 and prognosis in breast cancer: a meta-analysis. Oncotarget. 2017;8(19):31347–54.
Zhang M, Li G, Wang Y, Wang Y, Zhao S, Haihong P, Zhao H, Wang Y. PD-L1 expression in lung cancer and its correlation with driver mutations: a meta-analysis. Sci Rep. 2017;7(1):10255.
Wang S, Yuan B, Wang Y, Li M, Liu X, Cao J, Li C, Hu J. Clinicopathological and prognostic significance of PD-L1 expression in colorectal cancer: a meta-analysis. Int J Color Dis. 2021;36(1):117–30.
Xing AY, Liu L, Liang K, Wang B. p53 missense mutation is associated with immune cell PD-L1 expression in triple-negative breast Cancer. Cancer Investig. 2022;40(10):879–88.
Arafa M, Shebl AM, Salama A, ElZahaf E, Ashamallah SA, Foda AA, Awad AE, Shalaby A. Correlation of PD-L1 immunohistochemical expression with microsatellite instability and p53 status in endometrial carcinoma. Eur J Obstet Gynecol Reprod Biol X. 2022;16:100172.
Kan G, Dong W. The expression of PD-L1 APE1 and P53 in hepatocellular carcinoma and its relationship to clinical pathology. Eur Rev Med Pharmacol Sci. 2015;19(16):3063–71.
Ahmadi N, Gao K, Chia N, Kwon MS, Palme CE, Gupta R, Clark J. Association of PD-L1 expression in oral squamous cell carcinoma with smoking, sex, and p53 expression. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;128(6):631–8.
Jiang M, Jia K, Wang L, Li W, Chen B, Liu Y, Wang H, Zhao S, He Y, Zhou C. Alterations of DNA damage response pathway: biomarker and therapeutic strategy for cancer immunotherapy. Acta Pharm Sin B. 2021;11(10):2983–94.
Cortez MA, Ivan C, Valdecanas D, Wang X, Peltier HJ, Ye Y, Araujo L, Carbone DP, Shilo K, Giri DK, et al. PDL1 regulation by p53 via miR-34. J Natl Cancer Inst. 2016;108(1)
Xue X, Dong L, Burke E, Xue L, Lu YJ. The interaction of p53 and DNA repair gene mutations and their impact on tumor mutation burden and immune response in human malignancies. Am J Cancer Res. 2022;12(4):1866–83.
Han Y, Liu D, Li L. PD-1/PD-L1 pathway: current researches in cancer. Am J Cancer Res. 2020;10(3):727–42.
Acknowledgements
We are grateful to Laura Behm, Inge Brandt, Maren Eisenberg, and Sünje Seekamp for excellent technical assistance.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
HP, SS, MK, RS, TS, GS: contributed to conception, design, data collection, data analysis and manuscript writing. HP, ML, NCB, SM, FR, SE, AHM, HS, SK, DH: participated in pathology data analysis and data interpretation. KF, HP, SH, SW, BR, AFr, AFe, MdM, FR, SE, AHM, HS, MF, MR, MS, KK, TE, SH, SK, NA, TK, DH, HZ, KK; JW: collection of samples. RS, MK: data analysis. HP, SS, TS, RS, GS: study supervision. All authors agree to be accountable for the content of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Patient’s consent to participate was not required according to local laws (HmbKHG, §12, article 1), because patient samples were anonymized for the study. The use of archived remnants of diagnostic tissues for manufacturing of TMAs and their analysis for research purposes as well as patient data analysis has been approved by local laws (HmbKHG, §12, article 1) and by the local ethics committee (Ethics commission Hamburg, WF-049/09). All work has been carried out in compliance with the Helsinki Declaration.
Consent for publication
Not applicable.
Competing interests
The recombinant rabbit monoclonal PD-L1 antibody, MSVA-711R was from MS Validated Antibodies GmbH, Hamburg, Germany (owned by a family member of GS). All other authors have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Plage, H., Furlano, K., Hofbauer, S. et al. PD-L1 expression in tumor and inflammatory cells is associated with favorable tumor features and favorable prognosis in muscle-invasive urothelial carcinoma of the bladder not treated by immune checkpoint inhibitors. BMC Urol 24, 96 (2024). https://doi.org/10.1186/s12894-024-01482-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-024-01482-z