Abstract
Background
Paraganglioma of genitourinary tract is uncommon, and origin from ureter is even rarer. We aim to present a case of paraganglioma from ureter in a 48-year-old female patient, who presented with gross hematuria.
Case presentation
We present a 48-year-old female who complained of gross hematuria for one week. A left ureteral tumor was found by image study. However, hypertension was unexpectedly recorded during diagnostic ureteroscopy survey. Due to persisted gross hematuria and bladder tamponade, she underwent left nephroureterectomy with bladder cuff resection. Blood pressure surged again when the tumor was surgically approached. Ureteral paraganglioma was confirmed according to pathological report. After the surgery, the patient recovered well, and no more gross hematuria was noted. She is now under regular follow-up at our outpatient clinic.
Conclusion
Ureteral paraganglioma should be kept in mind not only when blood pressure fluctuates during operation, but also before we manipulate the ureteral tumor when gross hematuria is the only sign. Whenever the presumption of paraganglioma is raised, laboratory evaluation and anatomical or even functional imaging should be considered. The concomitant anesthesia consultation before the surgery should not be deferred, either.
Similar content being viewed by others
Background
Paraganglioma of urinary tract is rare, and it is reported to mostly originate from bladder, kidney and prostate [1]. Among these cases, the ureteral paraganglioma is even rarer, and only 6 cases have been reported [1,2,3,4,5,6]. When paraganglioma is suspected, the laboratory work-up and imaging study will be considered to rule out this disease. However, there are still some clinical dilemmas that may mask this crucial disease. In such situation, we may ignore the diagnosis and encounter difficulties in treatment. Herein, we present a case of ureteral paraganglioma in a 48-year-old female patient, who complained of severe gross hematuria for one week.
Case presentation
A 48-year-old female, who denied any systemic diseases, presented with severe gross hematuria and voiding difficulty for one week and came to the emergent department of our hospital for help.
Tracing back her history, she had visited regional hospital for gross hematuria several weeks ago before she came to us. Urinary bladder tamponade was noted and manual bladder irrigation with blood clots evacuation was also performed. Further imaging with contrast-enhanced computed tomography (CT) scan showed left hydronephrosis, and a round, well-defined retroperitoneum mass was noted adhering to left upper ureter, lying at left para-aortic region and the aortic bifurcation level. It was measured about 4.3 cm, and displaced the ureter medially, and the ovarian vein anteriorly. It also indented on the psoas muscle. The mass showed homogenously vivid after contrast enhanced. Massive blood clots were found within renal pelvis and bladder. Diagnostic semi-rigid ureteroscopy was arranged, and serpentine blood clots were found within left ureter. However, the ureteroscopy could not pass the compression site, where the sharp angulation existed. Unexpectedly, blood pressure surged when they tried to pass the stricture site with ureteroscope. The diagnostic ureteroscopy was incomplete and double J stent was placed for hydronephrosis. She was then referred to our hospital for further management.
At our emergency department, fever up to 39.2’c was recorded, but the blood pressure was within normal range (112/71 mmHg). The accompanied symptoms include dysuria, urinary frequency, and urgency. Basic hemogram revealed leukocytosis and elevated CRP level, but there was no deterioration of renal function. Meanwhile, pyuria was also recorded through urine analysis.
Reviewing her CT at regional hospital, we could see left hydronephrosis with a left retroperitoneal tumor about 4.3 cm adhering to and compressing left upper ureter with massive blood clots in bladder (Fig. 1). We also noticed that blood pressure surge during the ureteroscopy, so the presumption of paraganglioma was raised. Therefore, we tried to collect urine vanillylmandelic acid (VMA) and catecholamine for metabolic workup. Nevertheless, it was due to severe hematuria and bladder tamponade that we could not complete this study.
Fever gradually subsided after adequate antibiotics treatment. However, gross hematuria persisted with intermittent Foley catheter obstructed by blood clots. Manual bladder irrigation with blood clots evacuation was performed several times but in vain. Accordingly, her hemoglobin level dropped from 11 to 8 g/dL, so adequate blood transfusion was also given. During the clinical course before further surgical intervention, her blood pressure was kept within normal range.
After discussing with the patient, emergent excision of left retroperitoneal mass, which compressed and adhered to upper ureter, and possible nephroureterectomy with bladder cuff excision was arranged.
Under the impression of paraganglioma, though laboratory workup failed to be completed, we informed this situation to the anesthesiologist and made sure blood pressure was under cautious monitoring. During the operation, a round tumor was found adhesive onto left upper ureter, and severe adhesion between the tumor and gonadal vein was also identified. Extremely high blood pressure (> 200 mmHg) was detected during tumor manipulation even after multiple antihypertensive agents given by anesthesiologists. After tumor blood supply ligation, blood pressure restored to normal range rapidly. The patient recovered smoothly after the operation, and no hypertension was recorded after the surgery. The hemoglobin level also came back to normal range. Finally, she was discharged 9 days after the operation.
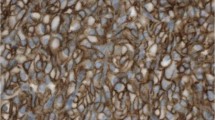
For the surgical finding, we found the specimen was a 4 × 3.5 × 3 cm elastic mass, which attached to left ureter, compatible with CT findings (Fig. 2). Microscopically, the tumor cells originated from outer muscle layer and adventitia of left ureter (Fig. 3). The neoplastic cells are round to polygonal with abundant eosinophilic granular to clear cytoplasm. The tumor cells are positive for Chromogranin A and Synaptophysin.
Six months after the surgery, the level of 24 h-urine catecholamines were within normal range. The follow-up computed tomography also revealed no recurrence of retroperitoneal tumor.
Discussion
Paraganglioma, which is also described as pheochromocytoma by previous articles of bladder, has been first described in 1953 by Zimmerman [7], and it stands for a very rare subtype of bladder tumor. It represents only 0.06% of bladder tumor and 1% of all pheochromocytoma [8]. The onset age is around 20–40 years old, and is more prevalent in women than in men [9]. On top of that, paraganglioma of ureteric origin is rarer, and only six cases around the world have been reported [1,2,3,4,5,6]. These cases are listed in Table 1.
The previous reports showed that the ureteral paraganglioma could be measured from 3.5 to 6 cm and could be located from renal hilum to the site of insertion to bladder.
The postoperative follow-up time of all six cases was around 1–2 years, and no tumor recurrence was found according to these studies.
For paraganglioma arising from genitourinary tract, bladder is the most common site of growth. The malignancy rate of these tumors has been described as 15–20%.
Among these cases of GU tract paraganglioma, they could be adequately managed by surgical excision [1].
The majority of initial presentation is hypertension or related symptoms and can be followed by hydronephrosis. Gross hematuria as initial symptom is relatively rare and differential diagnosis remains a challenge in clinical practice. The uncommon presentation in our case could be explained through the view of histopathology, by which the origin of the tumor from muscle layer of ureter might explain this phenomenon.
Since hypertension is the most common symptom in previous reports, it is crucial to raise such a presumption whenever fluctuating blood pressure is recorded when evaluating the disease, especially during manipulation of the tumor. We’ve learned a lesson from our case that although normo-tensive status was detected in most times in the clinical course, blood pressure surged during diagnostic ureteroscopy stood for a critical hint, through which ureteral paraganglioma should be considered.
From previous studies, we realized that plasma metanephrines are the most accurate parameter for detection of pheochromocytoma, whose sensitivity can reach 99%, and urinary fractionated metanephrines, with 97% sensitivity, are the most accurate parameters for detection of pheochromocytoma, and they perform better than urinary VMA from our case, whose sensitivity is only 77% [10]. The choice of urinary VMA instead of plasma metanephrines or urinary metanephrines in our case came from the limit of practice in our clinical laboratory section. However, we believe that plasma metanephrines or urine metanephrines are the first choice of assessing possible pheochromocytoma if it is available clinically. In our case, we did try to make more specific diagnosis of ureteral paraganglioma, but urgent surgical intervention was indicated owing to persisted hematuria and refractory blood clots evacuation at bedside, let alone her hemoglobin level dropped quickly. In this case, the clinical course and surgical indication was and should be explained comprehensively to the patient, since the operation for ureteral paraganglioma is more risky than usual NU.
It is well known that pathological evaluation for malignant pheochromocytoma or paraganglioma is difficult. The Ki-67 stain, and Pheochromocytoma of the Adrenal gland Scaled Score (PASS) score is what we can facilitate in order to offer more accurate follow-up [11]. Grossly, we identified an ovoid, firm and well-circumscribed tumor through the specimen. Its immunohistochemical panel of Ki-67 is less than 1% (Fig. 4). Ki-67 is known to be quite variable in both benign and malignant pheochromocytomas, through which both groups can express less than 1% historeactivity [11]. In addition, histologic features from PASS score also offer a number of clues for us to separate the aggressiveness of the tumor. Whether it is benign or malignant, small nests (“zellbellen”) can be observed in all pheochromocytomas. In our case, the tumor was comprised of large nests, and there was no central or confluent tumor necrosis. High cellularity didn’t exist, and no cellular monotony was identified. On top of that, tumor cell spindling was not observed, and mitotic figures was less than 3/10 high-power fields. There was no extension of tumor into adipose tissue. Neither vascular nor capsular invasion was found. At last, no profound nuclear pleomorphism or nuclear hyperchromasia was noted (Fig. 5). Through the above histologic features, the PASS score indicated a benign fashion (PASS < 4) [11]. Furthermore, the cytokeratin stain was negative, which exclude the origin from epithelial cell of ureter.
After the operation, image follow-up at clinic is important for us to evaluate any signs of recurrence or metastases. We can learn from former studies that the survey and follow-up of paraganglioma include anatomical and functional imaging. The former includes CT and magnetic resonance image (MRI), which could reveal the contour and content with high sensitivity. The latter is composed of [123I]-metaiodobenzylguanidine single photon emission computed tomography (123I-MIBG SPECT), which provides high specificity for paraganglioma identification, and positron emission tomography (PET) with radiopharmaceuticals such as 6-[18F]-fluorodopamine (18F-FDA) and [18F]-fluoro-dihydroxyphenylalanine (18F-FDOPA). They have also been used to locate paraganglioma and can also be seen as a routine functional imaging of paraganglioma. What’s more, comparing to 123I-MIBG SPECT, [18F]-fluoro-2-deoxy-D-glucose (18F-FDG) PET seemed to detect metastases better with high specificity. The uptake of 18F-FDG could indicate hereditary syndrome that underlies the paraganglioma [12].
More recently, the European Association of Nuclear Medicine recommended functional imaging for paraganglioma with ligands like 18F-fluorodopamine, 18F-dihydroxy-phenalalinine (DOPA), 18F-FDG or 68Ga-DOTATOC/DOTATATE/DOTANOC. The 18F-FDG stands out with a sensitivity of 80–100%, but with less specificity to detect extra-adrenal disease. Ga-DOTATOC and 18F-DOPA have been shown to be more accurate than 123I-MIBG, especially in small lesions and in extra-adrenal diseases [13, 14].
Preoperative diagnosis of paraganglioma may sometimes fall into dilemma if clinical symptoms are occult and laboratory study is limited. In our intraoperative hypertension is the only hint to indicate paraganglioma, and we also failed to gain the result of urinary VMA due to severe hematuria and we also couldn’t check urine metanephrines due to the limitation of facility. Other prompt and clinically feasible survey of paraganglioma may be needed in the future if urgent surgical intervention is inevitable.
Conclusion
Clinical presentation of ureteral tumor with gross hematuria raises the suspicion of urothelial carcinoma other than paraganglioma. However, the differential diagnosis of paraganglioma should be kept in mind if blood pressure surged when manipulating around the main tumor during ureteroscopy or even surgical manipulation. Even if gross hematuria is the only sign at first, this diagnosis of paraganglioma shouldn’t be omitted. Besides, anatomical or even functional study should always be done before invasive procedure if it is clinical available. Careful anesthesia consultation should not be omitted before the surgery. After the operation, the follow-up image study, renal function and urine test should also be monitored.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- NU:
-
Nephroureterectomy
- CT:
-
Computed tomography
- CRP:
-
C-reactive protein
- VMA:
-
Vanillylmandelic acid
- PASS:
-
Pheochromocytoma of the Adrenal gland Scaled Score
- MRI:
-
Magnetic resonance image
- MIBG:
-
Metaiodobenzylguanidine
- SPECT:
-
Single photon emission computed tomography
- PET:
-
Positron emission tomography
- FDA:
-
Fluorodopamine
- FDOPA:
-
Fluoro-dihydroxyphenylalanine
- DOPA:
-
Dihydroxy-phenalalinine
- FDG:
-
Fluoro-2-deoxy-D-glucose
References
Chavali L, Rao BM. Paraganglioma of ureter: a case report with review of literature. J Dr NTR Univ Health Sci. 2017. https://doi.org/10.4103/2277-8632.208001.
Allen SD, Karafin L, Kendall AR. Non-visualization of the kidney due to a ureteral pheochromocytoma. J Urol. 1971;105(4):571–4.
Cabañas VY, Faulconer RJ, Fekete AM. Pheochromocytoma presenting as a ureterocele. J Urol. 1973;110(4):389–90.
Kumar P, Natarajan K, Hegde P. Paraganglionoma of ureter. Internet J Urol. 2009;7(1).
Awasthi N, Kumari N, Krishnani N, Goel A. Functional paraganglioma of ureter: an unusual case. Indian J Pathol Microbiol. 2011;54(2):405.
Wang JYZ. Primary retroperitoneal paraganglioma mimicking a ureteral tumor: a case report and literature review. Postgrad Med. 2020. https://doi.org/10.1080/00325481.2020.1763633.
Zimmerman IJ, Biron RE, MacMahon HE. Pheochromocytoma of the urinary bladder. N Engl J Med. 1953;249(1):25–6.
Li WYB, Che J, et al. Diagnosis and treatment of extra-adrenal pheochromocytoma of urinary bladder: case report and literature review. Int J Clin Exp Med. 2013;6:832–9.
Male MYT, Tao J, Chen Z, Peng E. Differentiating nonfunctional paraganglioma of the bladder from urothelial carcinoma of the bladder: pitfalls and breakthroughs. Biomed Res Int. 2019;2019:1097149.
Lenders JWM, Pacak K, Walther MM, Linehan WM, Mannelli M, Friberg P, et al. Biochemical diagnosis of pheochromocytoma: which test is best? JAMA. 2002;287(11):1427–34.
Thompson LD. Pheochromocytoma of the Adrenal gland Scaled Score (PASS) to separate benign from malignant neoplasms: a clinicopathologic and immunophenotypic study of 100 cases. Am J Surg Pathol. 2002;26(5):551–66.
Timmers HJ, Chen CC, Carrasquillo JA, Whatley M, Ling A, Eisenhofer G, et al. Staging and functional characterization of pheochromocytoma and paraganglioma by 18F-fluorodeoxyglucose (18F-FDG) positron emission tomography. J Natl Cancer Inst. 2012;104(9):700–8.
Taieb D, Hicks RJ, Hindie E, Guillet BA, Avram A, Ghedini P, et al. European association of nuclear medicine practice guideline/society of nuclear medicine and molecular imaging procedure standard 2019 for radionuclide imaging of phaeochromocytoma and paraganglioma. Eur J Nucl Med Mol Imaging. 2019;46(10):2112–37.
Calissendorff J, Juhlin CC, Bancos I, Falhammar H. Pheochromocytomas and abdominal paragangliomas: a practical guidance. Cancers. 2022. https://doi.org/10.3390/cancers14040917.
Acknowledgements
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
T-HC and Z-HL designed the research and analyzed the data. C-WH made the histochemical stain and interpretated the histopathology of the specimen. Revision was done by T-HC and Z-HL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and the accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cheng, TH., Lu, ZH. & Hsu, CW. Gross hematuria as the presentation of ureteral paraganglioma: a case report and literature review. BMC Urol 23, 21 (2023). https://doi.org/10.1186/s12894-023-01185-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-023-01185-x