Abstract
Purpose
Repair of long-segment ureteral defect (LSUD) is challenging. Currently available procedures carry some potential complications. We modified the ileal graft by tapering the wall and stripping the mucosa to combat associated pitfalls and first reported the medium-term outcomes of 4 patients.
Material and methods
From September 2019 to October 2020, tapered demucosalized ileum (TDI) was used for LSUD reconstruction in 4 patients on the right (2 males and 2 females). Two patients were with panureteral avulsion and 2 with high-risk urothelial carcinoma in the distal ureter. TDI was made by tapering 1/2–2/3 of the antimesenteric ileal wall and stripping the mucosa with a blunt/blunt operating scissor. Follow-up modalities included serum creatinine, electrolytes, ultrasonography, CT urogram, renal scintigraphy, and ureteroscopy.
Results
Mean operation time was 443 min (range 360–550) and blood loss was negligible. The mean follow-up period was 29 months (range 23–36). Vesicoureteral reflux and related pyelonephritis occurred in 1 patient, necessitating a repair operation (Clavien-Dindo grade IIIb). No strictures, obstructions, metabolic disorders, or electrolyte imbalances were observed in the remaining patients. In carcinoma patients, ureteroscopy in month 18 post-operation revealed ileal mucosal regrowth in the form of dwarf isolated islands. All renal units maintained adequate drainage and function during the follow-up.
Conclusions
Ileal wall tapering and mucosa stripping confined to the muscularis mucosae level will not result in shrinkage, fibrosis, or stricture formation of the ileal ureter. The present work provides evidence for further application of TDI in the replacement of LSUD in patients.
Similar content being viewed by others
Background
Long-segment ureteral defect (LSUD) is a rare urological scenario, mainly caused by iatrogenic injuries, malignancy, tuberculosis, or extensive retroperitoneal fibrosis [1]. Reconstruction to restore ureteral continuity is challenging and probably involves substitution. Currently, available substitutes comprise the ileum, reconfigured colon, and appendix [2, 3]. Ileal ureter replacement has been widely used by urologists as its versatile usage, regardless of the defect length and side [4].
However, there are some intrinsic drawbacks of ileal substitutes, such as large tract lumen, mucous secretion, and metabolite absorption, which usually lead to pertinent complications like uroschesis, metabolic acidosis, electrolyte imbalance, and mucus obstruction [5]. Several modified techniques are proposed, including tapering the bowel graft, intestinal Onlay flap, and the Yong-Monti procedure, but only part of the issues is solved [6, 7].
To overcome the pitfalls completely, we modified the ileal conduit by tapering the antimesenteric part and stripping its mucosa to decrease ileal cross-sectional diameter and mucous secretion. In the short-term results of our preclinical animal research, which included 10 ureters of beagle dogs, no electrolyte disorders, severe obstruction, stricture, urine extravasation, or renal failure were observed, suggesting the feasibility and safety of the method. Intriguingly, H&E staining indicated no mucosal regeneration in 12 weeks [8]. Our current work aims to report this technique’s medium-term outcomes in 4 patients, including the patency of ileal ureter, renal function, electrolyte balance, and mucosa regeneration.
Materials and methods
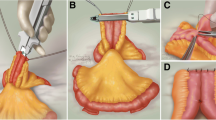
From September 2019 to October 2020, TDI was used for long-segment ureteral reconstruction in 4 patients on the right (2 male and 2 female). Two patients presented with panureteral avulsion (1 due to uterine evacuation; 1 ureteroscopy). Another 2 cases presented with high-risk UTUC in the distal ureter (1 patient with T1G1, tumor size > 2 cm, and 1 with T2G2; Table 1). Ureter replacement was performed using TDI in all 4 cases. An ileal segment was isolated and 1/2 to 2/3 of the antimesenteric part was longitudinally resected. Ileal mucosa was stripped with the blade of a blunt/blunt operating scissor. Obvious bleeding was stopped by cauterization. A 12Fr red rubber catheter was placed in the detubularized ileum to support, thus expediting ensuing closure with a running locking suture of 3–0 vicryl. Then, a double J ureteral stent (7Fr) was inserted into the reconstructed ileal tract. The proximal anastomosis was performed on the renal pelvis or mid ureter with a simple interrupted suture of 3–0 vicryl. The ileal nipple valve technique was used in ileo-vesical reimplantation (Fig. 1). Two drainage tubes were placed around the anastomoses through separate incisions. Follow-up modalities included serum creatinine, electrolytes, ultrasonography, CT urogram, renal scintigraphy, and ureteroscopy in carcinoma patients. This study was approved by the Ethics Committee of Affiliated Hospital of Zunyi Medical University (Protocol No. 20190113) and consent was obtained from all the patients.
Results
Mean operation time was 443 min (range 360–550) and blood loss was negligible. All patients’ postoperative urine was reddish in the early 3–5 days but without clotting and related ureteral or vesical obstruction. The mean follow-up was 29 months (range 23–36). According to the Clavien-Dindo classification, postoperative complication grade IIIb occurred in patient 1 who underwent uterine evacuation, repair, and ureter substitution [9]. The patient suffered recurrent high fevers 23 days after surgery. A percutaneous nephrostomy was performed to subside her pyrexia. Reflux pyelonephritis was diagnosed after retrograde urography. Reintervention was required to correct reflux by tapering the distal part of the ileal ureter. Thereafter, the patient recovered smoothly and complied with a regular follow-up (Fig. 2). The other 3 patients recovered uneventfully. The drainage tube was removed on day 5 post-operation and the double J stent removal was on month 3 post-operation. During follow-up, the serum creatinine of the 4 patients didn’t change noticeably. Lumina of neo-ureters remained patent, without stricture formation due to mucosal stripping or ileal wall tapering. No mucus obstruction, calcification, stone formation, or urinary tract tumor recurrence was observed in the period of up to 36-month follow-up (Figs. 3, 4A, B). All the renal units maintained adequate function. Mild hydronephrosis and split renal function impairment occurred in patient 1 as a result of vesicoureteral reflux but remained stable after the repair operation in a 2-year follow-up (Table 1). Intestinal mucosa regrowth was observed 18 months after the procedure. Dissimilar to the long dense finger-like projections of the origin, renewed mucosa presented in the form of short isolated islands (Fig. 4C,D).
Discussion
The main concern with ileal ureter replacement is the possibility of postoperative complications such as mucous obstruction, metabolic disorder, and renal function deterioration caused by mucous secretion, metabolite absorption of ileal mucosa, and a large cross-sectional diameter of the ileal lumen. To circumvent these risks, we modified ileal segments by tapering the wall and stripping the mucosa and have already conducted an animal study to confirm its safety and efficacy [8]. The purpose of the present study is to further report its feasibility and outcomes in patients. All the patients tolerated the procedure. Medium-term follow-up results indicated that all 4 neo-ureters remained patent, devoid of fibrosis, stricture formation, metabolic disorders, and electrolyte imbalance (1 patient recovered after a repair operation). To the best of our knowledge, this is the first report to document ureteral substitution's safety and medium-term outcomes with TDI in patients with LSUD.
Because of its inherent function of secretion and absorption, ileal mucosa becomes troublesome when used to replace a part of the urinary tract. To overcome the complications it caused, intestine seromuscular grafts were proposed and used in canine enterocystoplasty, but severe shrinkage occurred [10,11,12]. Several years later, Lima used demucosalized colon or ileum combined with an inflatable silicone model to prevent graft contraction in bladder augmentation and improved the outcomes [13]. Herein, we first adopted demucosalized ileum for lengthy ureteral replacement. In terms of stripping depth, we preferred to use a surgical scissor to only strip the mucosa. According to Dewan’s research, removal of the muscularis mucosa with the inner portion of the submucosa is required to prevent enteric mucosal regeneration [14]; however, this also risks impairing microcirculation and the enteric nervous system of the ileal flap, which accounts for the substitute's shrinkage and contraction [15, 16]. In the ureteroscopic follow-up of our 2 cancer patients, ileal mucosal regrowth did occur in month 18 post-operation. The renewed mucosa, however, became acclimated to the urine environment and was characterized by diminished mucus secretion capacity.
Another vexing issue with ileal replacement is the large cross-sectional diameter. It will cause back-and-forth, retrograde peristalsis, progressive dilatation, and elongation, thereby resulting in urinary stasis, obstruction, and renal function deterioration [17]. The Yang-Monti technique reduces ileal diameter and associated complications. However, this approach necessitates more bowel segments for LSUD, particularly in the panureter defects, which means more anastomoses and a higher risk of postoperative urine leakage and infections. Shokeir first adopted tailored ileal segments for ureteral replacement and achieved better treatment results [18]. Their method mitigated but did not eliminate mucus secretion. We integrated the mucosa stripping technique and ileal tapering technique to restore the continuity of long ureteral defects. Only 1/3 of the ileal wall was tapered in patient 1, and this was still too large for ileal ureter replacement. Afterward, we increased the tapered portion to 1/2–2/3 of its original size, making it more suitable for replacement.
Some researchers set serum creatinine value at 2 mg/dL as a threshold to perform ileal ureter replacement [19]. One of our patients with renal dysfunction, serum creatinine 2.65 mg/ml, did not experience metabolic disorders post-operation, which might indicate the amelioration of absorptive ability. However, the preoperative renal function of the other 3 patients was normal, with the ability to compensate for metabolic disorders. Whether mucosa stripping could be beneficial to reduce absorption remains to be elucidated.
Conclusions
Ileal wall tapering and mucosa stripping confined to the muscularis mucosae level will not result in shrinkage, fibrosis, or stricture formation of the ileal ureter. Adequate ileal wall tapering, appropriate mucosal stripping, and nipple valve technique are required to reduce postoperative complications. The present work provides evidence for further application of TDI in the replacement of LSUD in patients.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- LSUD:
-
Long-segment ureteral defect
- TDI:
-
Tapered demucosalized ileum
- UTUC:
-
Upper tract urothelial carcinoma
- CT:
-
Computed tomography
References
Armatys SA, Mellon MJ, Beck SD, Koch MO, Foster RS, Bihrle R. Use of ileum as ureteral replacement in urological reconstruction. J Urol. 2009;181(1):177–81.
Ubrig B, Roth S. Reconfigured colon segments as a ureteral substitute. World J Urol. 2003;21(3):119–22.
Xiong S, Zhu W, Li X, Zhang P, Wang H, Li X. Intestinal interposition for complex ureteral reconstruction: a comprehensive review. Int J Urol. 2020;27(5):377–86.
Poujade L, Branchereau J, Rigaud J, Perrouin-Verbe MA. Ileal ureter replacement: early morbidity and long-term results. Prog Urol. 2021;31(6):357–67.
Verduyckt FJ, Heesakkers JP, Debruyne FM. Long-term results of ileum interposition for ureteral obstruction. Eur Urol. 2002;42(2):181–7.
Patil N, Javali T. Application of the “Yang-Monti principle” in children with iatrogenic ureteral injuries. J Pediatr Urol. 2021;17(4):543.e1-43.e7.
Bao JS, He Q, Li Y, Shi W, Wu G, Yue Z. Yang-Monti principle in bridging long ureteral defects: cases report and a systemic review. Urol J. 2017;14(4):4055–61.
Gu H, Chen S, Wu Y, Shen L, Luo Y, Li X, Huang H, Zhao Z. Improved long ureteral reconstruction with ileum by longitudinal clipping and mucosal stripping: an animal study. Urol J. 2020;17(2):198–203.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–13.
Shoemaker WC, Marucci HD. The experimental use of seromuscular grafts in bladder reconstruction; preliminary report. J Urol. 1955;73(2):314–21.
Van Helsdingen PJ. Ureter replacement by collagen and seromuscular parts of the large bowel in dogs. Eur Urol. 1984;10(4):276–81.
Salle JL, Fraga JC, Lucib A, Lampertz M, Jobim G, Jobim G, Putten A. Seromuscular enterocystoplasty in dogs. J Urol. 1990;144(2 Pt 2):454–6; discussion 60.
Lima SV, Araujo LA, Vilar Fde O, Lima RS, Lima RF. Nonsecretory intestinocystoplasty: a 15-year prospective study of 183 patients. J Urol. 2008;179(3):1113–6.
Dewan PA. Autoaugmentation demucosalized enterocystoplasty. World J Urol. 1998;16(4):255–61.
Cervellione RM, Hajnal D, Varga G, Rakoczy G, Kaszaki J, Keene D, Goyal A, Dickson A, Cserni T. Mucosectomy impairs ileal microcirculation and results in flap contraction after experimental ileocystoplasty. J Pediatr Urol. 2017;13(1):81.e1-81.e5.
Urbán D, Marei MM, Hajnal D, Varga G, Érces D, Poles M, Imre D, Szabó A, Cervellione RM, Cserni T. Mucosectomy disrupting the enteric nervous system causes contraction and shrinkage of gastrointestinal flaps: potential implications for augmentation cystoplasty. J Pediatr Urol. 2020;16(1):20–6.
Bazeed MA, El-Rakhawy M, Ashamallah A, El-Kappany H, El-Hammady S. Ileal replacement of the bilharzial ureter: is it worthwhile? J Urol. 1983;130(2):245–8.
Shokeir AA, Gaballah MA, Ashamallah AA, Ghoneim MA. Optimization of replacement of the ureter by ileum. J Urol. 1991;146:306–10.
Pamecha Y, Shelke U, Patil B, Patwardhan S, Kini S. Use of ileum for complex ureteric reconstruction: assessment of long-term outcome, complications, and impact on renal function. Urol Ann. 2018;10(4):369–74.
Acknowledgements
Not applicable.
Funding
This report was supported by the National Natural Science Foundation of China (Grant No. 81960148), the Scientific Foundation of Zunyi City (Grant No. HZ2020229), Guizhou Science and Technology Department (Grant No. ZK2021380) and the Doctoral Foundation of the Affiliated Hospital of Zunyi Medical University (Grant No. 201801).
Author information
Authors and Affiliations
Contributions
SC prepared the manuscript. YJ drew Fig. 1. WT, HG, and HX collected the medical records and made Table 1. DY and KL provided Figs. 2, 3 and 4. GL reviewed the manuscript. ZZ performed the surgery and provided constructive suggestions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods were carried out in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or with comparable ethical standards. The Ethics Committee of Affiliated Hospital of Zunyi Medical University (Zunyi, China) approved this study (Protocol No. 20190113). Informed consent was obtained from all subjects and/or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, S., Jian, Y., Tang, W. et al. Replacement of long-segment ureteral defect with tapered demucosalized ileum: medium-term outcomes of 4 patients. BMC Urol 23, 7 (2023). https://doi.org/10.1186/s12894-023-01173-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-023-01173-1