Abstract
Background
Men diagnosed with localized prostate cancer (PCa) on active surveillance (AS) have shown to cope with anxiety caused by living with an ‘untreated cancer’ and different factors can influence the tolerance level for anxiety in these patients. The present study analyzes Italian (Milan) and Dutch (Rotterdam) men prospectively included in the Prostate cancer International Active Surveillance (PRIAS) trial, aiming to explore whether socio-demographic factors (i.e. age, relationship status, education, nationality) may be relevant factors in conditioning the level of anxiety at AS entry and over time.
Methods
Italian and Dutch men participating in the IRB-approved PRIAS study, after signing an informed consent, filled in the Memorial Anxiety Scale for PCa (MAX-PC) at multiple time points after diagnosis. A linear mixed model was used to assess the relationship between the level of patient’s anxiety and time spent on AS, country of origin, the interaction between country and time on AS, patients’ relationship status and education, on PCa anxiety during AS.
Results
823 MAX-PC questionnaires were available for Italian and 307 for Dutch men, respectively. Median age at diagnosis was 64 years (IQR 60–70 years) and did not differ between countries. On average, Dutch men had a higher total MAX-PC score than Italian men. However, the level of their anxiety decreased over time. Dutch men on average had a higher score on the PCa anxiety sub-domain, which did not decrease over time. Minimal differences were observed in the sub-domains PSA anxiety and fear of recurrence.
Conclusion
Significant differences in PCa anxiety between the Italian and Dutch cohorts were observed, the latter group of men showing higher overall levels of anxiety. These differences were not related to the socio-demographic factors we studied. Although both PRIAS-centers are dedicated AS-centers, differences in PCa-care organization (e.g. having a multidisciplinary team) may have contributed to the observed different level of anxiety at the start and during AS.
Trial registration This study is registered in the Dutch Trial Registry (www.trialregister.nl) under NL1622 (registration date 11-03-2009), ‘PRIAS: Prostate cancer Research International: Active Surveillance—guideline and study for the expectant management of localized prostate cancer with curative intent’.
Similar content being viewed by others
Background
According to the international guidelines, men diagnosed with low-risk prostate cancer (PCa) can opt for definitive treatment (such as radical prostatectomy (RP) or radiotherapy (RT)), or opt for active surveillance (AS). AS involves a monitoring strategy with regular follow-up testing through prostate-specific antigen (PSA) tests, digital rectal examination (DRE), repeat prostate biopsies, and, when indicated, the use of magnetic resonance imaging (MRI). Should the PCa be reclassified or progress, then switching to RP or RT is still possible. Because the treatment choice for localized PCa is a preference-sensitive one, discussing quality of life (QoL) as part of shared decision making between the clinician and the patient is of central importance [1]. During this decision making process patients are supported by physicians and their family, and the decision making process involving all the stakeholders represents a valid tool for dealing with uncertainty and “emotional waves” [1, 2]. By choosing AS men may be aware that this is the choice that will likely protect their QoL, as it is the strategy that is related to the least side effects, mainly urinary incontinence, sexual dysfunction, and bowel inflammation [2,3,4].
Men on AS have 10- and 15-year disease-specific survival rates of > 98% and > 94% in long-running AS cohorts [5, 6]. While the disease-specific survival rates are excellent and studies show that AS has the least impact on prostate-specific functioning [7, 8], patients may be harmed by the psychological burden of living with an untreated cancer. Such burden has been found to be low for the majority of men following an AS-strategy. A small proportion of men on AS reported significant levels of anxiety after diagnosis but their anxious feelings decreased over time [9,10,11,12,13]. Even though the majority of studies in the literature agree that AS has limited impact on mental health and QoL [14], some studies reported different results [15,16,17]. Because the research evidence regarding the psychological impact of living with AS is mixed in its conclusions, in this study the focus will not lie on identifying whether or not men experience anxiety while on an AS management strategy [18]. Instead the aim is to explore whether socio-demographic factors (i.e. age, relationship status, education, and nationality) may be relevant factors in conditioning the level of anxiety at AS entry and over time in two dedicated AS-centers that are part of the Prostate cancer Research International Active Surveillance (PRIAS) study.
Methods
Study population
Men newly diagnosed with low-risk PCa, eligible for AS according to the PRIAS inclusion criteria—i.e. PSA ≤ 10 ng/mL; PSA-density < 0.2 ng/mL/mL; ≤ T2; 1–2 positive prostate needle-biopsy cores with Gleason score ≤ 3 + 3 = 6 between 2007–2017 and who signed a PRIAS-informed consent were invited to participate in the prospective QoL study. Men were eligible to participate in the QoL study if they spoke Italian or Dutch and were able to complete self-reported questionnaires. In the Italian center—since the introduction of the Memorial Anxiety scale for PCa (MAX-PC)—498 men have been enrolled in PRIAS. A total of 466 men were invited to participate in the QoL study; 32 men were not invited due to logistical reasons or an inability to complete the questionnaires. In the Netherlands the first 150 Dutch patients included in the PRIAS study were invited to participate in the QoL study. PRIAS (www.prias-project.org) and its associated prospective QoL study were approved by the Institutional Review Board of the Erasmus University Medical Center (PRIAS: MEC2004-339, PRIAS QoL: MEC2014-596) and of the Fondazione IRCCS Istituto dei Tumori in Milan (INT 46-07). Furthermore, all methods were carried out in accordance with relevant guidelines and regulations.
Patient reported outcomes (PRO) measures
Men were invited to complete QoL-questionnaires at various timepoints; for the Italian center timepoints are at enrollment on AS (T0), 10 months after diagnostic biopsy (T1), immediately after the first re-biopsy (only patients still suitable for continuing on AS; T2), and then once a year after the first re-biopsy (T3); for the Dutch center timepoints are 3–6 months after enrollment on AS, 9 and 18 months after start on AS. The QoL-questionnaires contained validated measures to evaluate, amongst others, PCa-related anxiety (Memorial Anxiety Scale for PCa—MAX-PC) [19,20,21,22]. The MAX-PC includes 18 items, with for each item four response options (single item score range 0–3). The total MAX-PC score ranges from 0–54, with 54 indicating maximum PCa-related anxiety. Patients with scores of ≥ 27 were considered to have clinically significant PCa anxiety [19, 20]. The MAX-PC consists of three subscales that measure (1) general anxiety related to PCa and treatment—i.e. PCa anxiety, (2) anxiety related to PSA levels—i.e. PSA anxiety, and (3) fear of recurrence (fear of disease progression). Validated Italian and Dutch translations of the MAX-PC were used [21, 22].
Statistical analyses
Linear mixed models were used to adjust for clustering at participant level using a random intercept for patients. Fixed effects included country (Italy or the Netherlands), education level (primary or secondary school; professional school or college; university and post-degree), relationship status (not married; married/living together), years on AS, and the interaction and its main effects between years on AS and country. The overall effect of a categorical variable was assessed by comparing the full imputed model with the model without the covariate of interest based on the likelihood ratio test.
All statistical analyses were performed with R version 3.5.1. Missing data were imputed using the Bayesian framework with R-package jointAI [23].
Results
A total of 525 (395/466 Italian (response rate 84.8%%), 130/150 Dutch (response rate 86,7%)) men—who completed at least one QoL-questionnaire—were included in the analyses (Table 1). Median age at diagnosis was 64 years (IQR 60–70 years) and did not differ between countries. The maximum number of MAX-PC measurements was 823 for Italian and 307 for Dutch men.
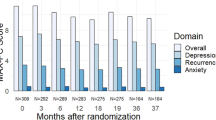
MAX-PC total score
The results of the analysis are presented in Table 2. The analysis shows that on average Dutch men score 13 points higher on the MAX-PC total score than Italian men (a higher score refers to a higher level of anxiety). In addition, the score decreases for Dutch men with on average one point for every year on AS compared to change over time for Italian men. These differences were not related to relationship status and education.
MAX-PC subscale ‘PCa anxiety’
The results of the analysis are presented in Table 3 and show that on average Dutch men score nine points higher on the MAX-PC subscale ‘PCa anxiety’ than Italian men. The score for Dutch men does not decrease over time compared to the change over time for Italian men. Relationship status and education are no predictors for the differences seen in the ‘PCa-anxiety’ subscale scores.
MAX-PC subscale ‘PSA Anxiety’
On average, Dutch men score 0.5 points lower on the MAX-PC subscale ‘PSA anxiety’ than Italian men. This subscale score for Dutch men does not decrease over time as compared to the change over time for Italian men, see Table 4. Relationship status and education are no predictors for the differences seen in the ‘PSA anxiety’ subscale scores.
MAX-PC subscale ‘Fear of Recurrence’
On average, Dutch men score three points higher on the MAX-PC subscale ‘Fear of Recurrence’ than Italian men. This subscale score decreases for Dutch men, with on average 0.7 points for every additional year on AS compared to the change over time for Italian men, see Table 5. Relationship status and education are no predictors for the differences seen in the ‘Fear of recurrence’ subscale scores.
Discussion
The present study aims to identify cultural-related factors associated with psychological well-being addressing anxiety as the main outcome in patients undergoing AS as a treatment for localized PCa in two dedicated AS-centers that are part of PRIAS.
Findings showed significant differences between the Italian and Dutch cohorts in self-reported disease-specific anxiety, the latter group of men showing a higher overall level of disease-specific anxiety of 13 points as measured by the MAX-PC questionnaire. Results of the analyses showed that the significant differences in disease-specific anxiety in our study could not be explained by sociodemographic factors such as education or relationship status, nor by the relation between center and years on AS, and the time on AS (in years). Country seems to be the variable that is associated with the observed levels of anxiety.
In a study by Ruane-McAteer and colleagues, AS patients showed higher anxiety levels compared to patients undergoing active treatment within nine months after diagnosis. Authors suggested that anxiety levels might be lower among patients undergoing AS at medical centres with a long experience in managing patients on AS. It is possible that focusing on studying and refining their AS protocols and procedures may lead to a greater acceptance and trust in AS by both patients and their clinicians [17]. That does not necessarily hold that collaborating specialists in the field of urology, like the oncologists and radiotherapists from the same centre, share such an attitude. In this study, the QoL-data from two dedicated AS-centers which follow the same AS-protocol have been analyzed. While we can expect differences in the psychological well-being of patients on AS between AS-dedicated vs. non-dedicated centers, here it is seen that even between two AS-dedicated centers the level of disease-specific anxiety can differ significantly. It can be hypothesized that cultural differences in cancer coping strategies between Northern and Southern European populations may play a role, but it might also be that this finding can be explained, in part, by the different clinical settings adopted in the two organizations. In the qualitative research conducted by Seaman et al., the importance of the clinician–patient relationship in navigating the experience of a PCa diagnosis and subsequent management with AS is shown [17, 24]. Before entering on AS, Italian patients meet with the different specialists involved in PCa care within a multidisciplinary team simultaneously (i.e. a urologist, a radiation oncologist and a psychologist), and they discuss the available treatment options together in one session (i.e. RP, external beam radiotherapy (EBRT), brachytherapy (BT) and AS). The multidisciplinary team shows men a unique agreement about “what he can do” and navigates with the patients and his family through the different options so that the patient is proactive in the final decision of the ‘best’ strategy for himself, in that particular moment of his life [1]. In this context, men may feel reassured that whatever treatment choice they make is supported by the multidisciplinary team of specialists and hence experience a feeling of hope about the possibility of protecting their QoL. Furthermore, men can ask for a psychological visit in case of need. On the other hand Dutch men eligible for AS will individually meet with one or several specialists in sequence, to talk about RP, RT and AS. Men do not necessarily have to talk to all specialists before deciding on which treatment they would like to start. So while both centers are dedicated AS-centers, the way PCa care is organized in Rotterdam and Milan may add to the different levels of anxiety experienced by AS patients. In the ProtecT trial which randomized PCa patients to either undergoing RP, RT, or active monitoring (an adapted form of AS) lessons have been learned on information provision, decision-making and the role specialists play in that process. It was found that surgeons and oncologists may inadvertently create an additional barrier to AS through their own personal preferences for treatments. On top of that barrier then also comes the difficulty of presenting AS as an equal option to the more traditional definitive treatment options (RP, RT) [18, 25,26,27,28,29]. Such a hesitation may subsequently profile into the patient-physician communication and leave potential marks in the patients’ line of thought.
Our findings, furthermore, revealed that the initial increase of the total MAX-PC and the fear of recurrence scores in Dutch men decreases slowly over time (for the total MAX-PC score with, on average, 1 point for every year on AS) as compared to Italian men which can be explained by the higher overall value that Dutch men reported at the start of AS. The difference in PSA anxiety was however small, and seems to be in the opposite direction of the total MAX-PC and fear of recurrence scores. Eymech et al. studied the biopsychosocial and holistic impact of living with untreated PCa while following an AS strategy through qualitative interviews [30]. It was recognized that men may experience cyclical anxiety around monitoring appointments. So while men after the diagnosis and recognition of the potential impact of low-risk PCa return to a normal state of mind and they do not worry about their PCa on a day-to-day or month-to-month basis, monitoring appointments may still cause a peak-anxiety moment [30].
As mentioned above, country is most likely to represent the way PCa care is organized in the two dedicated AS-centers. It can be hypothesized that once a man enters a clinical organization in which decision making has been collegially implemented, he may feel reassured and “in control” over his health. Moreover, the presence of a psychologist both at the entrance on AS and during the AS monitoring path might be helpful in supporting men and in taking charge of those who feel anxious. Similarly, a previous study from Vasarainen et al. explored the “bridge” role of the nurse between men on AS and the urologist [31]. These findings revealed that receiving support may help in explaining patients the low impact of AS on QoL.
Even though in the Dutch cohort anxiety levels were higher as compared to the Italian cohort, our findings showed that their anxiety levels slowly decreased over time. This is supported by a number of studies which demonstrated that during AS there is a psychological adjustment process ongoing [13, 32], with anxiety decreasing over time [31, 33,34,35]. Men may feel confident on AS as time goes by, since after being exposed to multiple follow-up AS follow-up visits it may be observed an habituated response effect [36], which in turn may lead to a gradual reduction in anxiety.
There are strengths and limitations in the conduct of this study. A strength is that both the Milan and Rotterdam centre use the PRIAS inclusion criteria and the AS-monitoring scheme. A limitation, however, is the timing of the questionnaires, which were around the same time, but not identical. In the statistical analyses this has been accounted for by including ‘time on AS (in years)’ as a fixed effect. Furthermore, we have to acknowledge that no control group was involved, and that the results of our analyses could hardly be generalized to other countries and/centers. It can, however, be perceived as an invitation to explore this topic further by comparing different countries and different care organizations. Finally, we were not able to distinguish whether the effect of country could also, in part, be attributed to a potential difference in ‘mind set’ between Italian and Dutch men.
Conclusions
In conclusion, in aiming to identify socio-demographic factors associated with psychological outcome to AS in two dedicated AS-centers being part of the worldwide, multi-center PRIAS study, country seems to be the variable that is associated with the observed differences in levels of anxiety. Country is most likely to represent the way PCa care is organized in the two dedicated AS-centers. In the present study the relevance of a multidisciplinary setting in PCa care organizations is briefly touched upon. A multidisciplinary clinical team including a psychologist can make a difference in offering AS-eligible patients tailored treatment information and in helping them to better understand their choice for AS, which is likely to have an impact on their anxiety levels. In daily clinical practice, clinicians and experts should be aware that involving patients in the decision making phase may easily lead to a higher trust in clinicians, better adherence to treatment recommendations, and facilitate patients’ engagement in quality of healthcare services.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PCa:
-
Prostate cancer
- RP:
-
Radical prostatectomy
- RT:
-
Radiotherapy
- AS:
-
Active surveillance
- PSA:
-
Prostate-specific antigen
- DRE:
-
Digital rectal examination
- MRI:
-
Magnetic resonance imaging
- QoL:
-
Quality of life
- PRIAS:
-
Prostate cancer Research International Active Surveillance study
- MAX-PC:
-
Memorial Anxiety scale for Prostate Cancer
- IQR:
-
Interquartile range
- CI:
-
Confidence interval
- EBRT:
-
External beam radiotherapy
- BT:
-
Brachytherapy
References
Bellardita L, Dordoni P, De Luca L, Delor JPM, Valdagni R. Better-informed decision-making to optimize patient selection. In: Klotz L, editor. Active surveillance for localized prostate cancer. Cham: Humana Press; 2018. p. 149–67.
Menichetti J, De Luca L, Dordoni P, Donegani S, Marenghi C, Valdagni R, Bellardita L. Making Active Surveillance a path towards health promotion: a qualitative study on prostate cancer patients’ perceptions of health promotion during Active Surveillance. Eur J Cancer Care. 2019;28(3):e13014.
Marenghi C, Alvisi MF, Palorini F, Avuzzi B, Badenchini F, Bedini N, Bellardita L, Biasoni D, Bosetti D, Casale A, Catanzaro M, Colecchia M, De Luca L, Donegani S, Dordoni P, Lanocita R, Maffezzini M, Magnani T, Menichetti J, Messina A, Morlino S, Paolini B, Rancati T, Stagni S, Tesone A, Torelli T, Tulli Baldoin E, Vaiani M, Villa S, Villa S, Zaffaroni N, Nicolai N, Salvioni R, Valdagni R. Eleven-year management of prostate cancer patients on active surveillance: what have we learned? Tumori J. 2017;103(5):464–74.
Reyna VF, Nelson WL, Han PK, Pignone MP. Decision making and cancer. Am Psychol. 2015;70(2):105.
Klotz L, Vesprini D, Sethukavalan P, Jethava V, Zhang L, Jain S, Yamamoto T, Mamedov A, Loblaw A. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol. 2015;33:272–7.
Tosoian JJ, Mamawala M, Epstein JI, Landis P, Wolf S, Trock BJ, Carter HB. Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. J Clin Oncol. 2015;33(30):3379–85.
Donovan JL, Hamdy FC, Lane JA, Mason M, Metcalfe C, Walsh E, Blazeby JM, Peters TJ, Holding P, Bonnington S, Lennon T, Bradshaw L, Cooper D, Herbert P, Howson J, Jones A, Lyons N, Salter E, Thompson P, Tidball S, Blaikie J, Gray C, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Davis M, Turner EL, Martin RM, Neal DE, ProtecT Study Group. Patient-reported outcomes after monitoring, surgery, or radiotherapy for prostate cancer. N Engl J Med. 2016;375(15):1425–37.
Venderbos LDF, Deschamps A, Dowling J, Carl E-G, Remmers S, van Poppel H, Roobol MJ. Europa Uomo Patient Reported Outcome Study (EUPROMS): descriptive statistics of a prostate cancer survey from patients to patients. Eur Urol Focus. 2021;7(5):987–94.
Anderson J, Burney S, Brooker JE, Ricciardelli LA, Fletcher JM, Satasivam P, Frydenberg M. Anxiety in the management of localised prostate cancer by active surveillance. BJU Int. 2014;114(1):55–61.
Venderbos LDF, van den Bergh RC, Roobol MJ, Schröder FH, Essink-Bot M-L, Bangma CH, Steyerberg EW, Korfage IJ. A longitudinal study on the impact of active surveillance for prostate cancer on anxiety and distress levels. Psychooncology. 2015;24:348–54.
Parker PA, Davis JW, Latini DM, Baum G, Wang X, Ward JF, Kuban D, Frank SJ, Lee AK, Logothetis CJ, Kim J. Relationship between illness uncertainty, anxiety, fear of progression and quality of life in men with favourable-risk prostate cancer undergoing active surveillance. BJU Int. 2016;117:469–77.
Marzouk K, Assel M, Ehdaie B, Vickers A. Long-term cancer specific anxiety in men undergoing active surveillance of prostate cancer: findings from a large prospective cohort. J Urol. 2018;200(6):1250–5.
Dordoni P, Badenchini F, Alvisi MF, Menichetti J, De Luca L, Di Florio T, Magnani T, Marenghi C, Rancati T, Valdagni R, Bellardita L. How do prostate cancer patients navigate the active surveillance journay? A 3-year longitudinal study. Support Care Cancer. 2021;29(2):645–51.
Bellardita L, Valdagni R, Van den Bergh R, Randsdorp H, Repetto C, Venderbos LDF, Lane JA, Korfage IJ. How does active surveillance for prostate cancer affect quality of life? A systematic review. Eur Urol. 2015;67:637–45.
Watts S, Leydon G, Eyles C, Moore CM, Richardson A, Birch B, Prescott P, Powell C, Lewith G. A quantitative analysis of the prevalence of clinical depression and anxiety in patients with prostate cancer undergoing active surveillance. BMJ Open. 2015;5(5):e006674.
Sharpley CF, Christie DR, Bitsika V. Variability in anxiety and depression over time following diagnosis in patients with prostate cancer. J Psychosoc Oncol. 2010;28(6):644–65.
Ruane-McAteer E, Porter S, O’Sullivan J, Dempster M, Prue G. Investigating the psychological impact of active surveillance or active treatment in newly diagnosed favorable-risk prostate cancer patients: a 9-month longitudinal study. Psychooncology. 2019;28(8):1743–52.
Ruane-McAteer E, Prue G. Psychological aspects of active surveillance. World J Urol. 2021. https://doi.org/10.1007/s00345-020-03553-w.
Roth AJ, Rosenfeld B, Kornblith AB, Gibson C, Scher HI, Curley-Smart T, Holland JC, Breitbart W. The Memorial Anxiety Scale for Prostate Cancer: validation of a new scale to measure anxiety in men with prostate cancer. Cancer. 2003;97(11):2910–8.
Roth A, Nelson CJ, Rosenfeld B, Warshowski A, O’Shea N, Scher H, Holland JC, Slovin S, Curley-Smart T, Reynolds T, Breitbart W. Assessing anxiety in men with prostate cancer: further data on the reliability and validity of the Memorial Anxiety Scale for Prostate Cancer (MAX-PC). Psychosomatics. 2006;47(4):340–7.
Alvisi MF, Repetto C, Rancati T, Badenchini F, Magnani T, Marenghi C, Villa S, Nicolai N, Salvioni R, Avuzzi B, Valdagni R, Bellardita L, Prostate Cancer Multidisciplinary Clinic Working Group. Italian cultural adaptation of the memorial anxiety for prostate Cancer scale for the population of men on active surveillance. Tumori. 2018;104(3):172–8.
Van den Bergh RCN, Korfage IJ, Borsboom GJ, Steyerberg EW, Essink-Bot ML. Prostate cancer-specific anxiety in Dutch patients on active surveillance: validation of the memorial anxiety scale for prostate cancer. Qual Life Res. 2009;18(8):1061–6.
Erler NS, Rizopoulos D, Jaddoe VW, Franco OH, Lesaffre EM. Bayesian imputation of time-varying covariates in linear mixed models. Stat Methods Med Res. 2019;28(2):555–68.
Seaman AT, Taylor KL, Davis K, Nepple KG, Lynch JH, Oberle AD, Hall IJ, Volk RJ, Schacht Reisinger H, Hoffman RM. Why men with a low-risk prostate cancer select and stay on active surveillance: a qualitative study. PLoS ONE. 2019;14(11):e0225134.
Donovan JL. Presenting treatment options to men with clinically localized prostate cancer: the acceptability of active surveillance/monitoring. J Natl Inst Monogr. 2012;45:191–6.
Fowler FJ Jr, Collins MM, Albertsen PC, Zietman A, Elliott DB, Barry MJ. Comparison of recommendations by urologists and radiation oncologists for treatment of clinically localized prostate cancer. JAMA. 2000;283(24):3217–22.
Hanna C, Mason M, Donovan J, Barber J. Clinical oncologists favour radical radiotherapy for localized prostate cancer: a questionnaire survey. BJU Int. 2002;90(6):558–60.
Mills N, Donovan JL, Wade J, Hamdy FC, Neal DE, Lane JA. Exploring treatment preferences facilitated recruitment to randomized controlled trials. J Clin Epidemiol. 2011;64(10):1127–36.
Wade J, Donovan JL, Lane JA, Neal DE, Hamdy FC. It’s not just what you say, it’s also how you say it: opening the ‘black box’ of informed consent appointments in randomized controlled trials. Soc Sci Med. 2009;68(11):2018–28.
Eymech O, Brunckhorst O, Fox L, Jawaid A, Van Hemelrijck M, Stewart R, Dasgupta P, Ahmed K. An exploration of wellbeing in men diagnosed with prostate cancer undergoing active surveillance: a qualitative study. Support Care Cancer. 2022;30(6):5459–68.
Vasarainen H, Lokman U, Ruutu M, Taari K, Rannikko A. Prostate cancer active surveillance and health-related quality of life: results of the Finnish arm of the prospective trial. BJU Int. 2012;109(11):1614–9.
Villa S, Kendel F, Venderbos LDF, Rancati T, Bangma CH, Carroll P, Denis L, Klotz L, Korfage IJ, Lane AJ, Magnani T, Mastris K, Rannikko A, Roobol MJ, Trock B, van den Bergh RCN, van Poppel H, Valdagni R, Bellardita L. Setting an agenda for assessment of health-related quality of life among men with prostate cancer on active surveillance: a consensus paper from a European School of Oncology Task Force. Eur Urol. 2017;71(2):274–80.
Van den Bergh RCN, Essink-Bot ML, Roobol MJ, Schröder FH, Bangma CH, Steyerberg EW. Do anxiety and distress increase during active surveillance for low risk prostate cancer? J Urol. 2010;183(5):1786–91.
Lokman U, Vasarainen H, Lahdensuo K, et al. Prostate cancer active surveillance: health-related quality of life in the Finnish arm of the prospective PRIAS-study. Three year update. Eur Urol Suppl. 2013;12(1):e274–5.
Kato T, Sugimoto M. Quality of life in active surveillance for early prostate cancer. Int J Urol. 2020;27(4):296–306.
Abramowitz JS, Deacon BJ, Whiteside SP. Exposure therapy for anxiety: principles and practice. New York: Guilford Publications; 2019.
Acknowledgements
The authors thank Fondazione Italo Monzino for its support for the project “Per un sentire condiviso: l’uomo e il tumore alla prostrate.”
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conception or design of the work: PD, SR, LV. Acquisition of data: FB (IT), PD (IT), CM (IT), study group of PRIAS Rotterdam. Analysis or interpretation of data: PD, SR, LV. Creation of new software used in the work: not applicable. Drafted the work or substantively revised it: PD, SR, RV, LB, LL, FB, CM, MR, LV. Approval of the submitted version of the manuscript: PD, SR, RV, LB, LL, FB, CM, MR, LV. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the Institutional Review Board of the Erasmus University Medical Center (PRIAS: MEC2004-339, PRIAS QoL: MEC2014-596) and of the Fondazione IRCCS Istituto dei Tumori in Milan (PRIAS: 4607). All participants received written information about the study, gave written consent and were informed about their ability to withdraw from the study at any time before publication of results.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Dordoni, P., Remmers, S., Valdagni, R. et al. Cross-cultural differences in men on active surveillance’ anxiety: a longitudinal comparison between Italian and Dutch patients from the Prostate cancer Research International Active Surveillance study. BMC Urol 22, 110 (2022). https://doi.org/10.1186/s12894-022-01062-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-022-01062-z