Abstract
Background
Active surveillance (AS) is the preferred treatment for patients with very low-and low-risk prostate cancer (PCa), but it is underperformed worldwide. This study aimed to report knowledge, attitudes, and practices (KAP) of AS for PCa among urologists in Brazil.
Methods
This cross-sectional study used a questionnaire with 50 questions divided into participant characteristics, knowledge regarding inclusion criteria for AS, follow-up, intervention triggers, acceptance, and practice for an index patient. Data analysis comprises absolute and relative frequencies of the variables. After that, a logistic regression was performed in order to verify possible patterns of answers provided by the respondents in the index patient questionnaire.
Results
Questionnaires were sent through the SurveyMonkey® platform to 5,015 urologists using email addresses and through social media. A total of 600 (12%) questionnaires returned and 413 (8.2%) were completed and included in the analysis. Only 53% of urologists adopt AS for low- and very-low-risk PCa. Inclusion criteria were patients with age > 50 years (32.2%), prostate specific antigen (PSA) < 10 ng/mL (87.2%), T1 clinical stage (80.4%), Biopsy Gleason score ≤ 6, positive cores ≤ 2 (44.3%), positive core involvement < 50% (45.3%), and magnetic resonance imaging findings (38.7%). The PSA doubling time was still used by 60.3%. Confirmatory biopsy (55.9%), PSA level (36.6%), and digital rectal examination (34.4%) were considered by most urologists for follow-ups. Patient preference (85.7%), upgrade of Gleason score (73.4%), and increased number of positive cores (66.8%) were associated with conversion to definitive treatment. In an index patient, non-acceptance and active treatment request were the most cited reasons for not performing AS.
Conclusion
There is significant variability in the KAP of AS in Brazil, which indicates the need to reinforce AS, its inclusion and follow-up criteria, and the benefits for physicians and the general population.
Trial registration: Not applicable.
Similar content being viewed by others
Background
There were approximately 65,000 New cases of prostate cancer (PCa) in Brazil in 2020. In 2017, mortality due to neoplasia was 15,576 [1]. In the last two decades, PCa diagnosis has increased, especially in the low-risk category, mainly because of more widespread prostate specific antigen (PSA) screening [2].
Active surveillance (AS) is a safe option for low- and very low-risk PCa [3, 4]. Current guidelines from the European Association of Urology (EAU) [5], American Urological Association (AUA) [6], and National Comprehensive Cancer Network (NCCN) [7] recommend AS as the preferred treatment option for these patients. Intermediate-risk PCa patients present with poor outcomes when managed through AS, but its use should be considered in selected cases. Nevertheless, AS remains underperformed worldwide [8].
This study aimed to report the knowledge, attitudes, and practices (KAP) of AS for PCa among urologists in Brazil.
Methods
This cross-sectional study followed a checklist for reporting the E-Survey results [9].
An anonymous survey was created to assess KAP of AS for PCa among urologists in Brazil. Questionnaires were sent through the SurveyMonkey® platform to 5015 urologists from the Brazilian urological community using email addresses obtained from the Brazilian Society of Urology membership directory and through social media.
The instrument for data collection was developed ad hoc for this study and comprised two parts consisting in the mapping of fundamental concepts in AS and the validation of the categories identified. The first part adopted a delphi approach through semi-structured interviews until saturation, that is, when little or no variation is observed in the answers [10]. Participants were specialists in Urologic oncology. The interview consisted of three questions: (1) List the topics or knowledge that a doctor should already know about AS; (2) What are the typical and exclusive contents of AS? (3) List the most common misconceptions about AS. The common points mentioned were aggregated by equality, similarity or thematic coherence in order to reduce the number of conceptual categories. This procedure was carried out independently by two researchers with ties dismissed by a third participant. The saturation point was reached after three interviews, as the answers were similar, equivalent or complementary [11].
The survey consisted of 50 questions, divided into participant characteristics (five items), acceptance and inclusion criteria to select patients for AS (11 items), practice characteristics (nine items), follow-up protocol (five items), intervention triggers (11 items), and knowledge about index patient (65-year-old male without comorbidities, potent and continent, diagnosed with very low or low-risk PCa) (nine items) (Additional file 1).
The inclusion criteria included being a Brazilian urologist and signing an informed consent. Incomplete questionnaires were discarded.
The sample size for a population of unknown size, with non-random distribution, a 95% confidence level, and a 5% margin of error, required 385 respondents for a survey.
The data analysis pipeline comprised descriptive statistics steps in terms of the absolute and relative frequencies of the study variables. Categorical variables were compared using the chi-squared test. Pairwise comparisons were performed for all variables. Then, a chi-squared test of independence was used, where classes of respondents were the dependent variable and tested against items of the index patient knowledge part of the questionnaire. A logistic regression was performed in order to verify possible patterns of answers provided by the respondents in the “index patient knowledge questionnaire”. Considering that the variables of interest are categorical and that the analysis was based on the occurrence of responses instead of a yes/no response ratio, a binomial distribution was adopted for the logit (link function), with a non-robust covariance. The regression results were presented as non-adjusted regression coefficients (R). Statistical significance was set at p < 0.05. Statistical analyses were performed using the R Studio version 1.1.383.
Results
Participants characteristics
Questionnaires were sent to 5015 urologists. A total of 600 (600/5015, 12%) questionnaires returned and 413 (413/5015, 8.2%) were completed and included in the analysis. The characteristics of the respondents are listed in Table 1.
Acceptance and Inclusion criteria to select patients for AS protocol
AS is the preferred treatment option for patients with low-risk and very low-risk PCa for 53% of urologists, while 5.3% do not recommend AS and consider any form of active treatment instead. Thirty percent of urologists reported that they did not use a predefined protocol for selecting patients who were candidates for AS. When a protocol was used (70% of the time), the one that was most frequently adopted was the one from John Hopkins (43.3%). Table 2 summarises the criteria considered for the AS indications.
Concerning age, 22.5% of urologists considered AS only for patients aged above 60 years and 17.2% indicated it only for patients aged above 70 years. A PSA level of < 10.0 ng/mL was an inclusion criterion for 87.2% of the urologists. More than half (53%) of the urologists did not consider PSA density (PSA-D) to suggest AS. In contrast, 60.3% used PSA doubling time (PSAdt) as an inclusion criterion for AS. For clinical staging indications, AS is an option for 80.4% of urologists in T1 tumours, 11.6% in T2a tumours, 2.7% in T2b tumours, and 1.5% in T2c tumours. A Gleason score (GS) of 6 or less was an inclusion criterion for 93.2% of the urologists and 5.3% considered AS for some selected Gleason 7 (3 + 4) cases, while 0.5% considered it for Gleason 7 (4 + 3) cases. Two or fewer positive cores were used by 44.3% of urologists, 33.2% used ≤ 3 positive cores, 9.9% used < 34% of the cores involved, and 6.3% did not use this as a criterion to indicate AS. Approximately 30.8% of urologists use < 20% as the maximum involvement of each positive core as a criterion to indicate AS, while 45.3% used 50% as the threshold to indicate AS. Approximately 38.7% of urologists use magnetic resonance imaging (MRI) as an eligibility criterion to allocate a patient to an AS protocol (Table 2).
Practice characteristics
MRI is inaccessible to 15.7% of urologists, 9.2% have access to MRI of the pelvis, without a specific prostate protocol (multiparametric MRI (mpMR), and 1.5 and 3.0 Tesla mpMRI is available for 40.9% and 34.2% of urologists, respectively. Prostate biopsies are mostly performed at the same institution by the urologists (17.4%) who ordered it (17.4%), other urologists (19.6%), or radiologists (35.6%). The remaining 27.4% prostrate biopsies were performed elsewhere. The majority of biopsies were transrectal (99.3%). In terms of the number of cores retrieved, sextant biopsies (12 cores with two from each area) were the most common (41.6%). Fusion-guided biopsy was available for 52.3% of the urologists (23.7% with software, 28.6% cognitive), but 47.7% did not have access for their practice. The time interval between biopsy request and its execution was less than one month in most cases (67.1%). Biopsy histopathological reports provide GS in different ways. The vast majority provided Gleason for each specific fragment (87.9%). Occasionally, a unique GS is determined for fragments of the right lobe and another for fragments of the left lobe all together (5.6% of cases), and elsewhere only a single ‘general’ GS (6.5% of cases) is described. Histopathological reports do not indicate the number of positive cores and percentage of involvement of positive fragments in 1.7% and 3.6% of urologists’ practices, respectively (Table 3).
Follow-up
During follow-up, 26.6% of urologists did not perform a confirmatory biopsy. The remaining patients underwent a confirmatory biopsy, mainly between 6 and 12 months after diagnosis (55.9%). Approximately 63% of urologists perform additional biopsies after a confirmatory biopsy, every one to two years (37.3% and 25.7%, respectively). The remaining only perform it if a trigger point is reached, such as a PSA rise (29.5%) or an MRI modification (7.5%) (Table 4).
Intervention triggers
Triggers for active treatment during follow-up are presented in Table 5. More than one answer was permitted.
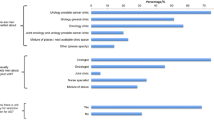
Knowledge about index patient
The reasons for not performing AS in an index patient (65-year-old male without comorbidities, potent and continent, diagnosed with very low or low-risk PCa) are listed in Table 6. More than one answer was provided.
Response patterns
The logistic regression among ‘Indication of AS’ versus ‘Index Patient Knowledge’ was statistically significant for the following items: Considering those who did not indicate AS, there was a direct relation to ‘I don't know enough about this type of treatment to properly follow-up the patients’ (p = 0.030, R = 2.19) and ‘I believe that AS is an inappropriate approach for patients with prostate cancer, even at low or very-low risk’ (p = 0.004, R = 2.14), while an inverse relation was observed with ‘Patient does not accept AS and requests active treatment’ (p = 0.018, R = − 1.21). Considering those who indicate AS occasionally, there is a direct relation to ‘I would like to indicate, but I cannot schedule laboratory tests and/or biopsy and/or outpatient return with the appropriate interval’ (p = 0.026, R = 0.83), while an inverse relation was observed with ‘Morbidity associated with multiple biopsies’ (p = 0.001, R = -1.01) and ‘I would like to indicate, but the histopathological report does not provide the necessary data’ (p = 0.012, R = − 2.72). Finally, considering those who indicated AS, there was an inverse relation to ‘I believe that AS is an inappropriate approach for patients with PCa, even at low or very-low risk’ (p = 0.024, R = − 2.42), ‘Morbidity associated with multiple biopsies’ (p = 0.001, R = − 1.06), and ‘I would like to indicate, but I cannot schedule laboratory tests and/or biopsy and/or outpatient return with the appropriate interval’ (p = 0.048, R = − 0.74).
Regarding the region of Brazil and the indication of AS, multiple logistic regression showed a significant difference in the southern region (p = 0.028, R = 1.87).
Discussion
AS has been proposed as the preferred treatment option for low- and very low-risk PCa; however, the inclusion criteria and follow-up schedules present great variability [3, 5, 12,13,14,15,16,17]. The features that vary most are the number of positive cores, proportion of cancer in each positive core, PSA cut-off, and use of PSA-D and PSAdt. The absence of homogeneous recommendations affects urological practice.
Total PSA up to 10 ng/dL is an inclusion criterion used by Klotz et al. [4], Tosoian et al. [3], Godtman et al. [12], and Bokhorst et al. [15]. Selvadurai et al. [13] accepted patients with PSA levels up to 15 ng/dL. Findings showed that the vast majority of urologists in Brazil use PSA < 10 ng/dL (87.2%) as the cut-off limit to propose AS.
Tosoian et al. [3] and Bokhorst et al. [15] considered PSA-D as an inclusion criterion. During follow-up, PSA-D is an important risk factor for progression of PCa [18]. In this study, up to 53.3% of urologists did not use it as an inclusion criterion. For those who adopt it, PSA-D < 15%, as in Johns Hopkins [3], is the cut-off for 31.5% and < 20%, as in PRIAS [15], is the cut-off for 6.8%.
In contrast, PSAdt has not been used by most of the AS protocols because this feature is a weak stage upgrading predictor in the specimen analysis after surgery [19]. Conversely, more than 60% of the responders still used PSAdt to indicate AS where 13.1% will offer AS if PSAdt is more than six months, and 24% will consider AS only if PSAdt is more than 12 months.
The number of positive cores and maximum tumour involvement in each core were both considered as inclusion criteria by Tosoian et al. [3], Welty et al. [20], Thomsen et al. [6], and Soloway et al. [7]. These characteristics are also linked to unfavourable evolution during follow-up and a higher chance of tumour reclassification [21]. The EAU [5] and NCCN guidelines [7] define very low-risk PCa when up to two cores are involved, as described by Epstein et al. [22]. However, AUA guidelines [6] classify very-low risk when there are < 34% positive cores, as the number of cores retrieved in a prostate biopsy has risen from the original six to a much greater sampling. In this study, 44.3% of urologists considered ≤ 2 positive cores, and 9.9% considered < 34% of the total cores as an inclusion criterion. A considerable number of urologists (33.2%) adopted a criterion of ≤ 3 positive cores, which was used by Thomsen [16].
Less than 50% maximum involvement of a positive core to include patients in an AS protocol was considered by 45.3% of the urologists, as used by Tosoian et al. [3], Welty et al. [20], and Thomsen et al. [16]. Notably, 43.4% of urologists used other cut-off limits as part of the inclusion criteria. Less than 20% of tumours in each core, as in Soloway et al. [17], was adopted by 30.8% urologists and less than 30% of tumours in each core, as in Thompson et al. [14], was used by 12.6%.
The follow-up management is also different in terms of the interval of digital rectal exam and PSA evaluation, and the role of confirmatory and re-biopsy indications varies among studies [3, 4, 13,14,15,16,17, 20]. This study also revealed similar differences in responses in terms of follow-up management preferences.
Although Brazil is a country with limited resources and a lack of MRI availability, a significant number of urologists order it to manage AS, even though its use during follow-up is still under investigation and has conflicting results [23, 24]. Also, it is has been demonstrated that MRI targeted biopsies can cause a “grade inflation” and this should be considered during the risk assessment [25]. The availability of MRI in Brazil varies according to the working environment (private versus public). In the public environment, mpMRI is accessible to 56.7% of urologists, and in almost two-thirds of these cases, only 1.5 Tesla equipment is available. In contrast, mpMRI can be easily ordered by 80% of urologists in private institutions, and half of them are 3 Tesla. The use of MRIs also varies according to geography, being less available in the northern and north-eastern regions, considered as economically disadvantaged areas compared to the rest of the country.
Since there is not a validated Brazilian guideline regarding the management of patients under AS, Brazilian urologists adapt their practice according to their own convenience, mixing criteria from diverse international guidelines, as demonstrated by our survey.
There was a direct relationship between the response of the urologists who did not indicate AS and the lack of knowledge about AS because they considered this type of treatment inappropriate for the index patient. While analysing those that indicated AS occasionally, we found that they did not consider the biopsy to be harmful and they have good pathology reports; however, they do not indicate AS regularly because of lack of access to scheduled laboratory tests and/or biopsy and/or outpatient return with the appropriate interval. As expected, urologists who indicated AS agreed to the harmfulness of biopsy were able to follow-up patients and had access to good pathology reports.
This study demonstrated that AS remains underused in Brazil. Only 53% of respondents considered it the preferred option for low- and very low-risk PCa in most cases. In developed countries, AS has gained traction in recent years. In the United States, up to 75% of very low-risk cases are initially treated with AS [26]. In Sweden, use of AS is even greater, reaching 91% for very-low-risk and 74% for low-risk cases [27].
Findings showed that economically less-favoured regions presented worse AS indications and acceptance rates when compared to more developed areas (South Region). This has also been observed in other studies. A survey demonstrated that AS is underused in Lebanon due to patient non-compliance and discrete acceptance among physicians [28]. Although the use of AS varies based on geographic location, county-level socioeconomic factors in the United States did not influence its indication [29].
Continuous medical education programmes and patient awareness campaigns are essential to reinforce AS and reduce the overtreatment of PCa and its potential complications. It is important to address the advantages of AS as a treatment option for the public, since the main reason for not performing AS was patient non-acceptance (88%).
This is the largest worldwide survey to evaluate AS and the first large-scale survey in low- to middle-income countries. Despite this, the response rate was 12% in the lower tier of what can be expected in voluntary e-mail-based surveys [30,31,32]. Another aspect that may represent a selection bias is that responders average age was 46.8 years old, maybe being more web/IT oriented, and prone to follow international guidelines and be updated to current practices.
We believe that this study described in detail Brazilian urologists’ knowledge, attitude, and practice regarding AS. Based on this data, public authorities and medical societies may have an instrument to guide the construction of a national guideline.
Conclusions
PCa management through AS in a low-middle-income country presents many challenges. Many urologists do not adopt AS for a number of reasons. Continuous medical education and population awareness programmes are the most important methods to disseminate evidence-based knowledge in medical and general populations and to reduce overtreatment of PCa.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AS:
-
Active surveillance
- AUA:
-
American Urological Association
- EUA:
-
European Association of Urology (EAU)
- GS:
-
Gleason score
- KAP:
-
Knowledge, attitudes, and practices (KAP)
- mpMRI:
-
Multiparametric magnetic resonance imaging
- MRI:
-
Magnetic resonance imaging
- NCCN:
-
National Comprehensive Cancer Network (NCCN)
- PCa:
-
Prostate cancer PC
- PSA:
-
Prostate specific antigen
- PSA-D:
-
PSA density
- PSAdt:
-
PSA doubling time
References
Instituto Nacional do Câncer. https://www.inca.gov.br/campanhas/cancer-de-prostata/2020/saude-do-homem. Accessed 24 June 2020.
Ploussard G, Epstein JI, Montironi R, Carroll PR, Wirth M, Grimm MO, et al. The contemporary concept of significant versus insignificant prostate cancer. Eur Urol. 2011;60:291–303.
Tosoian JJ, Mamawala M, Epstein JI, Landis P, Wolf S, Trock BJ, Carter HB. Intermediate and longer-term outcomes from a prospective active-surveillance program for favorable-risk prostate cancer. J Clin Oncol. 2015;33:3379–85.
Klotz L, Vesprini D, Sethukavalan P, Jethava V, Zhang L, Jain S, Yamamoto T, Mamedov A, Loblaw A. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol. 2015;33:272–7.
Mottet N, van den Bergh R, Briers CN, et al.: EAU—ESTRO—ESUR—SIOG guidelines on prostate cancer 2020. In: European Association of urology guidelines. 2020 Edition. Arnhem, The Netherlands: European Association of Urology Guidelines Office, vol presented at the EAU Annual Congress Amsterdam 2020.
Sanda MG, Cadeddu JA, Kirkby E, Chen RC, Crispino T, Fontanarosa J, Freedland SJ, Greene K, Klotz LH, Makarov DV, Nelson JB, Rodrigues G, Sandler HM, Taplin ME, Treadwell JR. Clinically localized prostate cancer: AUA/ASTRO/SUO guideline. Part II: recommended approaches and details of specific care options. J Urol. 2018;199:990–7.
NCCN Prostate Cancer Guidelines, 2020. https://www.nccn.org/professionals/physician_gls/default.aspx. Accessed 24 June 2020.
Musunuru HB, Yamamoto T, Klotz L, Ghanem G, Mamedov A, Sethukavalan P, Jethava V, Jain S, Zhang L, Vesprini D, Loblaw A. Active surveillance for intermediate risk prostate cancer: survival outcomes in the Sunnybrook experience. J Urol. 2016;196:1651–8.
Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6:e34.
McMillan SS, King M, Tully MP. How to use the nominal group and Delphi techniques. Int J Clin Pharm. 2016;38:655–62.
Lynn MR. Determination and quantification of content validity. Nurs Res. 1986;35(382):385.
Godtman RA, Holmberg E, Khatami A, Pihl CG, Stranne J, Hugosson J. Long-term results of active surveillance in the Göteborg randomized, population-based prostate cancer screening trial. Eur Urol. 2016;70:760–6.
Selvadurai ED, Singhera M, Thomas K, Mohammed K, Woode-Amissah R, Horwich A, Huddart RA, Dearnaley DP, Parker CC. Medium-term outcomes of active surveillance for localised prostate cancer. Eur Urol. 2013;64:981–7.
Thompson JE, Hayen A, Landau A, Haynes AM, Kalapara A, Ischia J, Matthews J, Frydenberg M, Stricker PD. Medium-term oncological outcomes for extended vs saturation biopsy and transrectal vs transperineal biopsy in active surveillance for prostate cancer. BJU Int. 2015;115:884–91.
Bokhorst LP, Valdagni R, Rannikko A, Kakehi Y, Pickles T, Bangma CH, Roobol MJ, PRIAS study group. A decade of active surveillance in the PRIAS study: an update and evaluation of the criteria used to recommend a switch to active treatment. Eur Urol. 2016;70:954–60.
Thomsen FB, Berg KD, Røder MA, Iversen P, Brasso K. Active surveillance for localized prostate cancer: an analysis of patient contacts and utilization of healthcare resources. Scand J Urol. 2015;49:43–50.
Soloway MS, Soloway CT, Eldefrawy A, Acosta K, Kava B, Manoharan M. Careful selection and close monitoring of low-risk prostate cancer patients on active surveillance minimizes the need for treatment. Eur Urol. 2010;58:831–5.
Soeterik TFW, van Melick HHE, Dijksman LM, Biesma DH, Witjes JA, van Basten JA. Active surveillance for prostate cancer in a real-life cohort: comparing outcomes for PRIAS-eligible and PRIAS-ineligible patients. Eur Urol Oncol. 2018;1:231–7.
Ross AE, Loeb S, Landis P, Partin AW, Epstein JI, Kettermann A, Feng Z, Carter HB, Walsh PC. Prostate-specific antigen kinetics during follow-up are an unreliable trigger for intervention in a prostate cancer surveillance program. J Clin Oncol. 2010;28:2810–6.
Welty CJ, Cowan JE, Nguyen H, Shinohara K, Perez N, Greene KL, Chan JM, Meng MV, Simko JP, Cooperberg MR, Carroll PR. Extended followup and risk factors for disease reclassification in a large active surveillance cohort for localized prostate cancer. J Urol. 2015;193:807–11.
Petrelli F, Vavassori I, Cabiddu M, Coinu A, Ghilardi M, Borgonovo K, Lonati V, Barni S. Predictive factors for reclassification and relapse in prostate cancer eligible for active surveillance: a systematic review and meta-analysis. Urology. 2016;91:136–42.
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, Grading Committee. The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol. 2016;40:244–52.
Klotz L, Loblaw A, Sugar L, Moussa M, Berman DM, Van der Kwast T, Vesprini D, Milot L, Kebabdjian M, Fleshner N, Ghai S, Chin J, Pond GR, Haider M. Active surveillance magnetic resonance imaging study (ASIST): results of a randomized multicenter prospective trial. Eur Urol. 2019;75:300–9.
Jayadevan R, Felker ER, Kwan L, Barsa DE, Zhang H, Sisk AE, Delfin M, Marks LS. Magnetic resonance imaging-guided confirmatory biopsy for initiating active surveillance of prostate cancer. JAMA Netw Open. 2019;2:e1911019.
Mesko S, Marks L, Ragab O, Patel S, Margolis DA, Demanes DJ, Kamrava M. Targeted prostate biopsy gleason score heterogeneity and implications for risk stratification. Am J Clin Oncol. 2018;41(5):497–501.
Shelton JB, Buffington P, Augspurger R, Gaylis F, Cohen T, Mehlhaff B, Suh R, Bradford TJ, Kwan L, Koo AS, Shore N. Contemporary management of incident prostate cancer in large community urology practices in the United States. Urology. 2019;129:79–86.
Loeb S, Folkvaljon Y, Curnyn C, Robinson D, Bratt O, Stattin P. Uptake of active surveillance for very-low-risk prostate cancer in Sweden. JAMA Oncol. 2017;3:1393–8.
El Sebaaly R, Mansour M, Labban M, Jaafar RF, Armache A, Mukherji D, El Hajj A. Survey on the practice of active surveillance for prostate cancer from the Middle East. Prostate Int. 2020;8:41–8.
Washington SL 3rd, Jeong CW, Lonergan PE, Herlemann A, Gomez SL, Carroll PR, Cooperberg MR. Regional variation in active surveillance for low-risk prostate cancer in the US. JAMA Netw Open. 2020;3:e2031349.
Gudaru K, Gonzalez Padilla DA, Castellani D, Tortolero Blanco L, Tanidir Y, Ka Lun L, Wroclawski ML, Maheshwari PN, Figueiredo FCA, Yuen-Chun TJ. A global knowledge, attitudes and practices survey on anatomical endoscopic enucleation of prostate for benign prostatic hyperplasia among urologists. Andrologia. 2020;52:e13717.
Teoh JY, Ong WLK, Gonzalez-Padilla D, Castellani D, Dubin JM, Esperto F, Campi R, Gudaru K, Talwar R, Okhunov Z, Ng CF, Jain N, Gauhar V, Wong MC, Wroclawski ML, Tanidir Y, Rivas JG, Tiong HY, Loeb S, UroSoMe Working Group. A global survey on the impact of COVID-19 on urological services. Eur Urol. 2020;78:265–75.
Gomes CM, Favorito LA, Henriques JVT, Canalini AF, Anzolch KMJ, de Carvalho Fernandes R, Bellucci CHS, Silva CS, Wroclawski ML, Pompeo ACL, de Bessa J. Impact of COVID-19 on clinical practice, income, health and lifestyle behavior of Brazilian urologists. Int Braz J Urol. 2020;46:1042–71.
Acknowledgements
We would like to thank the assistance provided by Ms. Maria Beatriz Lemos (Research Nurse, HIAE), and Mr. Ricardo de Morais (Technical editor, SBU).
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization, M.L.W., B.S.A. and A.C.; Methodology, M.L.W., B.S.A., P.P.K., W.B., S.W., A.S., F.C.M., G.C.L., and A.C.; Software, M.L.W. and B.S.A.; Validation, M.L.W., B.S.A. and E.M.; Formal Analysis, M.L.W., B.S.A., and E.M.; Investigation, M.L.W., B.S.A., P.P.K., W.B., S.W., A.S., F.C.M., G.C.L., and A.C.; Resources, M.L.W.; Data Curation, M.L.W., B.S.A. and E.M.; Writing—Original Draft Preparation, M.L.W., B.S.A. and B.B.; Writing—Review & Editing, M.L.W., B.S.A., P.P.K., B.B. and A.C.; Supervision, A.C.; Visualization, M.L.W., P.P.K. and B.B; Project Administration, M.L.W., B.S.A. and A.C. All authors critical review of the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Commit-tee of the “Hospital Israelita Albert Einstein” (Approve Code CAAE: 15032919.1.0000.0071and date of approval 01/08/2019) and was performed in accordance with relevant guidelines and regulations. Each participant enrolled in this study signed an informed consent for the survey and to allow analysis for research purposes.
Consent for publication
Informed consent was obtained from all subjects involved in the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Survey about knowledge, acceptance, and practice of urologists concerning active surveillance for prostate cancer in Brazil.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wroclawski, M.L., Amaral, B.S., Kayano, P.P. et al. Knowledge, attitudes, and practices of active surveillance in prostate cancer among urologists: a real-life survey from Brazil. BMC Urol 22, 86 (2022). https://doi.org/10.1186/s12894-022-01036-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-022-01036-1