Abstract
Background
Suburethral sling with tension-free vaginal tape (TVT) has become a popular treatment for stress urinary incontinence (SUI). Erosion of the tape into the vaginal is rare. Very few patients present with vaginal tape erosion and recurrence of SUI.
Case presentation
A 49-year-old female patient with stress urinary incontinence was treated with a retropubic suburethral TVT sling. 2 months later, recurrent symptoms of SUI developed. 6 months later, the patient complained of repeated vaginal discharge and foreign body sensation. Body physical examination revealed a 1-cm-long tape extrusion at the left anterior vaginal wall beside the midline. Cystourethroscopy revealed no urethral mesh erosion. Surgical removal of the extrusion tape revealed that the left arm of the tape was in the vaginal mucosa layer rather than between the whole thickness of the vaginal mucosa and urethral. The tape around the urethral was dissected and removed. A new retropubic tape was placed simultaneously. At the 8-months follow-up after surgery, the patient was continent without tape vaginal exposure.
Conclusions
Vaginal mesh erosion should be considered in a patient who presents with sustained vaginal discharge after being treated with a suburethral sling. It is important to place the tape between the whole thickness of the vaginal mucosa and the urethral in SUI surgery. A shallow placement of the tape may lead to vaginal tape erosion and recurrence of SUI. These complications can be avoided by following the correct manipulation procedure and referring to the tissue layer anatomy.
Similar content being viewed by others
Background
Stress urinary incontinence (SUI) is a major urological problem as many as 25% of women older than 20 years have SUI [1].The retropubic tension-free vaginal tape (TVT) procedure has become the standard of care for SUI with demonstrated long-term efficacy and low complications since its introduction in 1996 by Ulmsten et al. [2]. Vaginal erosion after TVT or transobturator tape placement is a rare complication with an incidence ranging from 0.2 to 22% [3, 7].Tape vaginal erosion with SUI recurrence together is extremely rare [4, 5]. We recently experienced a case of rapid SUI recurrence and later vaginal tape exposure because of the shallow placement of the tension-free vaginal tape.
Case presentation
A 49-year-old woman was referred to our center because of vaginal tape exposure for 2 weeks and recurrent SUI symptoms for 4 months. The patient had a history of a retropubic TVT sling procedure performed at 6 months ago due to SUI at a local hospital. 2 month later after the TVT surgery, the patient had recurrent SUI symptoms, such as urine leakage when sneezing and coughing. After physical examination and symptoms estimation, no special treatment was recommended to the patient by the physician of the local hospital. 6 months after surgery, the patient had aggravating urine leakage symptoms and repeated vaginal discharge and foreign body sensation. Vaginal tape exposure was found by her male partner for dyspareunia 2 weeks before the patient came to our center. Her medical history was significant for hypertension history for 2 years. Her blood pressure was well controlled with candesartan. The patient had once natural delivery and was in menopausal status before TVT surgery.
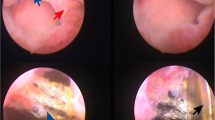
Urinalysis and vaginal secretions were negative. Body physical examination revealed a 1-cm-long tape extruding (yellow circle contour) from the left anterior vaginal wall beside the midline (Fig. 1, red arrow). Cystourethroscopy revealed no urethral tape erosion. Urodynamic examination confirmed the SUI diagnosis. A 2-cm-long longitude incision in the anterior vaginal wall was made. Transvaginal periurethral dissection was performed. Surgical removal of the extruded tape revealed that the left arm of the tape was wrongly put in the vaginal mucosa layer(Fig. 2, yellow arrow) rather than between the whole thickness of vaginal mucosa and urethral (Fig. 2, green arrow). A 5-cm-long tape around the urethral was dissected and removed (Fig. 3). A new retropubic tape was placed simultaneously. At the 8-months follow-up after surgery, the patient was continent without tape vaginal exposure.
Discussion and conclusions
Although the TVT sling procedure either by retropubic or transobturator way is been demonstrated to be a safe and effective surgery for SUI, there have been reports of complications. The most common complications are de novo urge incontinence and voiding dysfunction [3, 4, 6]. Vaginal tape erosion/exposure/extrusion is a rare complication with an incidence ranging from 0.2 to 22% [3, 7].Tape vaginal erosion with SUI recurrence together is extremely rare [4, 5]. The exact reasons for vaginal tape erosions remain uncertain, but possible explanations include wound infection, excessive sling tension, small mesh pore size, poor mesh incorporation, radiotherapy, postoperative vaginal atrophy, and premature sexual intercourse after operation [7,8,9]. Risk factors for erosion are the length of vaginal incision > 2 cm, recurrent vaginal incision for postoperative complications, and previous pelvic organ prolapse or incontinence surgery [7]. In our case, none of the above reasons can explain the mechanism of rapid SUI recurrence and later tape erosion. We verified in surgery that the right arm was in the proper layer of the vaginal wall and had no erosion. The left arm of the tape, however, was wrongly put in the vaginal mucosa layer rather than between the whole thickness of vaginal mucosa and urethral. Thus, shallow placement of the tape may cause rapid recurrence of SUI and vaginal tape erosion. In order to get the correct anatomy for the tape placement, we usually inject 10–20 ml saline into the vaginal mucosa. The incision should be deep enough to separate the whole thickness of the vaginal wall. Blunt dissection is recommended by using tissue scissor. It`s important to make sure that the bilateral tissue tunnels for the tape placement are in the same layer of the vaginal wall. After dissection of the vaginal mucosa, the urethral should be in integrity.
Symptoms of vaginal tape erosion include sustained vaginal discharge, vaginal bleeding, dyspareunia of the patient or her partner [8,9,10]. Some patients may have no symptoms, so a careful vaginal examination is needed after surgery for follow-up. Vaginal tape erosion without other problems can be treated in a conservative way, such as prointravaginal estrogen administration [5, 11]. When conservative treatments fail, partial or complete tape removal is recommended [5, 11, 12]. For the correction of recurrent SUI, retropubic TVT tape is recommended for high priority with encouraging success [13]. Therefore, after partial removal of periurethral tape, we put another retropubic vaginal tape. At the 8-months follow-up after surgery, the patient was continent without tape vaginal exposure.
For the technique of TVT either by retropubic or transobturator pathway, it is important to place the tape between the whole thickness of the vaginal mucosa and the urethral in SUI. A shallow tape placement may cause rapid SUI recurrence and the vaginal tape erosion. These complications can be avoided by following the correct manipulation procedure and referring to tissue layer anatomy.
Availability of data and materials
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- SUI:
-
Stress urinary incontinence
- TVT:
-
Tension-free vaginal tape
References
Holroyd-Leduc JM, Straus SE. Management of urinary incontinence in women: scientific review. JAMA. 2004;291:986–95.
Schierlitz L, Dwyer P, Rosamilia A, et al. Effectiveness of tension-free vaginal tape compared with transobturator tape in women with stress urinary incontinence and intrinsic sphincter deficiency. Obstet Gynecol. 2008;112:1253–61.
Karram MM, Segal JL, Vassallo BJ, Kleeman SD. Complications and untoward effects of the tension-free vaginal tape procedure. Obstet Gynecol. 2003;101:929–32.
Kuuva N, Nilsson CG. A nationwide analysis of complications associated with the tension-free vaginal tape (TVT) procedure. Acta Obstet Gynecol Scand. 2002;81(1):72–7.
Domingo S, Alamá P, Ruiz N, Perales A, Pellicer A. Diagnosis, management and prognosis of vaginal erosion after transobturator suburethral tape procedure using a nonwoven thermally bonded polypropylene mesh. J Urol. 2005;173(5):1627–30.
Gomes CM, Carvalho FL, Bellucci CHS, et al. Update on complications of synthetic suburethral slings. Int Braz J Urol. 2017;43(5):822–34.
Kokanali MK, Doğanay M, Aksakal O, Cavkaytar S, Topçu HO, Özer İ. Risk factors for mesh erosion after vaginal sling procedures for urinary incontinence. Eur J Obstet Gynecol Reprod Biol. 2014;177:146–50.
Bhargava S, Chapple CR. Rising awareness of the complications of synthetic slings. Curr Opin Urol. 2004;14(6):317–21.
Kobashi KC, Govier FE. Management of vaginal erosion of polypropylene mesh slings. J Urol. 2003;169:2242–3.
Deval B, Haab F. Management of the complications of the synthetic slings. Curr Opin Urol. 2006;16:240–3.
Ismail S, Chartier-Kastler E, Reus C, Cohen J, Seisen T, Phé V. Functional outcomes of synthetic tape and mesh revision surgeries: a monocentric experience. Int Urogynecol J. 2019;30(5):805–13.
Forzini T, Viart L, Alezra E, Saint F. Erosive complications of mid urethral slings (MUS): 10 years of surgical experience. Prog Urol. 2015;25(5):240–8.
Ashok K, Wang A. Recurrent urinary stress incontinence: an overview. J Obstet Gynaecol Res. 2010;36(3):467–73.
Acknowledgements
Not applicable.
Funding
Natural Science Foundation of Zhejiang Province granted Dr. Xiao Huang for the projector named “Treatment of chemokine CXCL 12 combined with muscle precursor stem cell autografting on rat stress urinary incontinence” (number: LY19H050008) for female stress urinary incontinence basic and clinical research.
Author information
Authors and Affiliations
Contributions
XH: Data collection, manuscript writing; The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The manuscript entitled “Case report of vaginal erosion and recurrence of stress urinary incontinence due to shallow placement of tension-free vaginal tape” is under the permission and consent to participate from The ethics committee of the Zhejiang University First affiliated Hospital.
Consent for publication
I declare that the written consent was obtained from the participant. We received the consent to publish from the patient herself. We keep the “Consent form” for request anytime.
Competing interests
The author declare that he has no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Huang, X. Case report of vaginal erosion and recurrence of stress urinary incontinence due to shallow placement of tension-free vaginal tape. BMC Urol 22, 67 (2022). https://doi.org/10.1186/s12894-022-01016-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-022-01016-5