Abstract
Background
Xanthine urinary stones are a rare entity that may occur in patients with Lesch–Nyhan syndrome receiving allopurinol. There is little literature describing imaging characteristics of these stones, and the most appropriate approach to imaging these stones is therefore unclear. We performed in-vitro and in-vivo analyses of xanthine stones using computed tomography (CT) at different energy levels, ultrasound (US), and magnetic resonance imaging (MRI).
Methods
Five pure xanthine stones from a child with Lesch-Nyhan were imaged in-vitro and in-vivo. CT of the stones was performed at 80 kVp, 100 kVp, 120 kVp and 140 kVp and CT numbers of the stones were recorded in Hounsfield units (HU). US of the stones was performed and echogenicity, acoustic shadowing and twinkle artifact were assessed. MRI of the stones was performed and included T2-weighted, ultrashort echo-time-weighted and T2/T1-weighted 3D bFFE sequences and signal was assessed.
Results
In-vitro analysis on CT demonstrated that xanthine stones were radiodense and the average attenuation coefficient did not differ with varying kVp, measuring 331.0 ± 51.7 HU at 80 kVp, 321.4 ± 63.4 HU at 100 kVp, 329.7 ± 54.2 HU at 120 kVp and 328.4 ± 61.1 HU at 140 kVp. In-vivo analysis on CT resulted in an average attenuation of 354 ± 35 HU. On US, xanthine stones where echogenic with acoustic shadowing and twinkle artifact. On MRI, stones lacked signal on all tested sequences.
Conclusion
Xanthine stone analyses, both in-vitro and in-vivo, demonstrate imaging characteristics typical of most urinary stones: dense on CT, echogenic on US, and lacking signal on MRI. Therefore, the approach to imaging xanthine stones should be comparable to that of other urinary stones.
Similar content being viewed by others
Background
Xanthine urolithiasis is a rare entity, occurring in patients with Lesch–Nyhan syndrome, who are receiving allopurinol treatment, and in patients with hereditary xanthinuria [1,2,3,4]. While a rare condition, xanthine urolithiasis may cause recurrent symptoms in this group of patients and require frequent medical attention. Children with Lesch–Nyhan syndrome are developmentally delayed, and often cannot appropriately verbalize their symptoms or localize their pain, making clinical assessment difficult. This often leads to multiple imaging studies over time. Understanding the imaging characteristics of these stones on different imaging modalities is imperative for effective clinical management.
Little is written in the medical literature about the imaging of xanthine stones, and no previous in-vitro studies have described the imaging characteristics of xanthine stones on CT, US or magnetic resonance imaging (MRI). A small number of in-vivo studies have described xanthine stones as radiolucent on radiographs and excretory urograms, as echogenic with posterior shadowing on ultrasound (US) and as having a computed tomography (CT) number ranging from 276–480 HU on conventional single energy CT [1,2,3,4].
Given the small number of previous studies on the topic, we sought to further characterize the imaging features of this rare urinary stone. Utilizing an in-vitro and in-vivo study design we characterized the imaging findings of xanthine stones on varying CT energy levels (80, 100, 120 and 140 kVp), US and MRI.
Methods
This is a retrospective study, and for this type of study formal consent and an ethics approval by an IRB are not required.
Stones that were previously passed by a child aged 3–10 years old with Lesch–Nyhan syndrome on allopurinol therapy were retained and analyzed. Stones’ diameters measured 4.2 mm, 3.0 mm, 3.9 mm, 2.2 mm and 2.6 mm. The stones were then characterized on the available imaging modalities performed on the patient prior to the stones being passed.
In-vitro CT images of the stones were obtained using a GE LightSpeed VCT CT scanner. Stones were placed within saline-containing syringes arranged concentrically in an acrylic PMMA phantom. A 16 cm diameter CTDI phantom was used. CT imaging was performed at 80 kVp, 100 kVp, 120 kVp and 140 kVp levels. Tube current was 250 mA for 80 kVp, 100 kVp, and 120 kVp, and tube current was 210 mA at 140 kVp. Other imaging parameters included: 1.00 s scan time, 0.625 mm section thickness, 40 mm collimation, helical mode with 0.984 pitch, display Field of View (FOV) = 36 cm; scan FOV = 50 cm (adult). The corresponding CT numbers of the stones were recorded in Hounsfield units (HU) using region-of-interest sampling.
In-vivo CT images of the stones were obtained from two CT scans performed on the patient prior to stone passage. Both studies were performed at 100 kVp. The corresponding CT numbers of the stones were recorded in Hounsfield units (HU) using region-of-interest sampling.
US images of the stones were obtained using a General Electric (GE) Logiq E9 US machine. Stones were placed one by one in a 0.9% NaCl saline bath on a standoff pad in a round plastic container. Stones were imaged with 7 MHz and 15 MHz transducers. Imaging characteristics were recorded, including echogenicity of the stones, acoustic shadowing and twinkle artifact on color Doppler imaging.
In-vivo US images of the stones were obtained from three US scans performed on the patient prior to stone passage. Imaging characteristics were recorded, including echogenicity of the stones, acoustic shadowing and twinkle artifact on color Doppler imaging.
MR images of the stones were obtained on a 3 T Philips Achieva MRI scanner with a 32-channel head coil. Stones were first visualized in air-filled syringes and then in saline-filled syringes. T2-weighted (T2W) turbo spin echo (TSE) sequences, multi-slice balanced field echo (bFFE, or balanced steady-state free precession) sequences, and 3D stack-of-stars ultra-short-TE (UTE) sequences with radial k-space trajectory acquisition were tested on the phantoms [5]. TSE-based T2W sequences had repetition time (TR) = 1500 ms, echo time (TE) = 80 ms, flip angle = 90°, slice thickness = 4 mm, gap = 0.4 mm, matrix size = 156 × 126, and FOV = 200 × 174 mm; T2/T1-weighted bFFE sequences had TR = 2.7 ms, TE = 1.2, flip angle = 40°, thickness = 5 mm, gap = 1 mm, FOV = 256 × 260, matrix size = 144 × 163; and UTE sequence had TR = 4.27 ms, dual TE = 0.142/1.2 ms, Flip angle = 9°, FOV = 200 mm, matrix size = 184 × 184, number of excitations (NEX) = 1, slice thickness = 2.2 mm, and scan duration = 2 min 23 s. No in-vivo MRI images of the stones were performed on the patient prior to stone passage.
After imaging analysis of the stones was complete, chemical analysis of all stones was performed to confirm their composition.
Results
Chemical analysis confirmed that all five stones where composed of 100% xanthine.
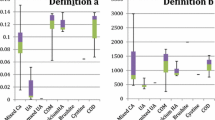
On in-vitro CT analysis, stones had an average CT number of 331.0 ± 51.7 HU at 80 kVp, 321.4 ± 63.4 HU at 100 kVp, 329.7 ± 54.2 HU at 120 kVp and 328.4 ± 61.1 HU at 140 kVp (Figs. 1, 2) (Table 1) (Additional file 1). On in-vivo CT analysis performed on the patient prior to stone passage on two separate imaging studies at 100kVp, a 6 mm stone had an average CT number of 304 ± 26 HU, a 9 mm stone measured 374 ± 8 HU, and a 10 mm stone measured 383 ± 12 HU (Fig. 3).
On US all stones were echogenic, demonstrated posterior acoustic shadowing, and twinkle artifact with color Doppler imaging on in-vitro analysis (Figs. 4, 5). In-vivo stone analysis performed prior to passage on US demonstrated stones that were echogenic, demonstrated posterior acoustic shadowing, and twinkle artifact (Figs. 6, 7).
On in-vitro MRI analysis, stones were only visualized as a signal void when imaged in saline-filled syringes, and were not visualized when imaged in air-filled syringes on all sequences, including TSE based T2W sequences, UTE sequences and T2/T1-weighted 3D bFFE sequences (Figs. 8, 9). In-vivo MRI imaging was not available.
Discussion
To the best of the authors’ knowledge, this is the first in-vitro study describing the imaging characteristics of xanthine stones on CT with multiple different energy levels, US and MRI. A previous in-vivo study of xanthine stones using conventional single energy CT showed CT numbers of stones ranging from 276–480 HU [2]. Previous in-vivo US studies have shown xanthine stones to be echogenic with posterior acoustic shadowing, with features identical to other urinary calculi [3]. No previous studies have described the imaging characteristics of xanthine stones on MRI.
On the four different energy levels on CT, in-vitro xanthine stones had an average CT number of 321.4–331.0 HU. There was no significant difference in the measured HU when imaging at different energies (80, 100, 120 and 140 kVp). On the two in-vivo imaging studies performed prior to stone passage xanthine stones had an average CT number of 304–383 HU. These in-vitro and in-vivo numbers are similar to CT numbers reported in the aforementioned in-vivo study of xanthine stones that used conventional single energy CT.
Interestingly, xanthine stones have relatively lower CT numbers than most urinary calculi. For example, reported mean CT numbers for struvite stones are 401–871 HU, cystine stones are 248–1088 HU, calcium oxalate stones are 865–1039 HU, and calcium phosphate stones are 1417 HU [6,7,8]. Xanthine stones have similar mean CT numbers to uric acid stones, which have reported CT numbers ranging from 270–519 [6, 8]. This may not be surprising given that xanthine and uric acid are part of the same metabolic pathway. The lower density of xanthine stones likely explains the previous literature describing them as radiolucent on radiographs. The lower density makes them more difficult to appreciate on radiographs than other more dense calculi, and stones were likely radiographically occult rather than truly radiolucent.
On in-vitro and in-vivo US, all xanthine stones were echogenic, showed posterior acoustic shadowing, and demonstrated twinkle artifact with color Doppler imaging. These features are identical to other types of urinary stones. Previous in-vivo analyses of xanthine stones have also showed them to be indistinguishable from other urinary stones on US [1,2,3]. Based on these findings, ultrasound is equally suitable to evaluate xanthine stones as any other type of urinary stone.
Xanthine stones showed no signal on all in-vitro MRI sequences tested, including UTE MRI sequences. Stones are expected to result in signal voids on conventional MRI sequences, but recent studies of UTE imaging have shown signal within other types of urinary calculi on UTE sequences [9, 10]. This has led some to suggest that these sequences might be utilized to evaluate urolithiasis. Our analysis suggests that xanthine stones are unlikely to be well visualized when utilizing the described MRI techniques in a clinical setting, including UTE sequences.
Although xanthine urolithiasis is a rare condition, it may cause recurrent symptoms in patients with Lesch–Nyhan syndrome on allopurinol therapy and in patients with hereditary xanthinuria. Children with Lesch–Nyhan syndrome are developmentally delayed and are often unable to appropriately verbalize their symptoms, making imaging particularly important in the clinical assessment of these patients. Given the recurrent nature of this condition, multiple imaging studies may be needed over the course of a lifetime. While our study examined rare xanthine stones from a single patient, thus perhaps limiting generalizability, we believe that based on the results of this study, xanthine stones are easily detectable on US. Therefore, US may be the first line imaging test in the evaluation of xanthine stones given its lack of ionizing radiation and ability to visualize these stones. Recent developments in UTE MRI sequences have suggested that MRI may provide an additional imaging modality to assess urinary calculi without ionizing radiation. However, our in-vitro analysis suggests that xanthine stones are not easily detectable on MRI, including UTE sequences, and MRI is unlikely to be helpful in the evaluation of xanthine urolithiasis. Unfortunately, no in-vivo MRI imaging of the stones was performed on this patient prior to stone passage. Our analysis suggests that xanthine stones are well visualized on CT. Therefore, judicious use of conventional non-contrast CT may be appropriate in patients with xanthine urolithiasis when ultrasound is inconclusive or insufficient. The risks of radiation exposure should always be considered, especially given the recurrent nature of this condition and the potential need for multiple imaging studies over a lifetime.
A limitation of our study stems from the small size of xanthine stones on in-vitro analysis. Stones smaller than 5 mm in diameter tend to demonstrate lower CT numbers regardless of composition secondary to partial-volume effects. CT numbers in our in-vitro analysis may be lower given the smaller size of the stones studied. However, on in-vivo analysis, prior to stone passage, the stones were as large as 10 mm and had comparable CT numbers to that of our in-vitro analysis. This may perhaps partially negate the effect of volume averaging on our in-vitro findings. Previous MRI studies that were able to demonstrate signal within urinary stones used stones larger than 1 cm, which is larger than the stones evaluated in this study [7, 10, 11]. This small size may have contributed to the lack of signal seen on all MRI sequences tested in our study. Future studies could benefit from analyzing larger stones, if available.
Conclusions
Xanthine urinary stones are a rare type of urinary calculus that may cause recurrent symptoms requiring numerous imaging tests over a lifetime. In-vitro and in-vivo analyses showed that xanthine stones are easily detectable on US and CT, but failed to demonstrate signal on all MRI sequences tested. CT numbers of xanthine stones did not vary when imaging with different energies. We believe that US should be considered the first line imaging test in the evaluation of xanthine urinary calculi and judicious use of CT is warranted when ultrasound is inconclusive or insufficient and risks of radiation have been considered.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CT:
-
Computed tomography
- US:
-
Ultrasound
- MRI:
-
Magnetic resonance imaging
- FOV:
-
Field of view
- HU:
-
Hounsfield units
- T2W:
-
T2-weighted
- TSE sequences:
-
Turbo spin echo
- bFFE:
-
Multi-slice balanced field echo or balanced steady-state free precession
- UTE:
-
3D stack-of-stars ultra-short-TE
- TR:
-
Repetition time
- TE:
-
Echo time
References
Gargah T, et al. Xanthine urolithiasis. Saudi J Kidney Dis Transpl. 2010;21(2):328–31.
Pais VM Jr, et al. Xanthine urolithiasis. Urology. 2006;67(5):1084.e9–11.
Mestrinho LA, et al. Xanthine urolithiasis causing bilateral ureteral obstruction in a 10-month-old cat. J Feline Med Surg. 2013;15(10):911–6.
Ogawa A, Watanabe K, Minejima N. Renal xanthine stone in Lesch–Nyhan syndrome treated with allopurinol. Urology. 1985;26(1):56–8.
Rahmer J, et al. Three-dimensional radial ultrashort echo-time imaging with T2 adapted sampling. Magn Reson Med. 2006;55(5):1075–82.
Newhouse JH, et al. Computed tomographic analysis of urinary calculi. AJR Am J Roentgenol. 1984;142(3):545–8.
Motley G, et al. Hounsfield unit density in the determination of urinary stone composition. Urology. 2001;58(2):170–3.
Deveci S, et al. Spiral computed tomography: role in determination of chemical compositions of pure and mixed urinary stones—an in vitro study. Urology. 2004;64(2):237–40.
el Ibrahim SH, et al. Detection of different kidney stone types: an ex vivo comparison of ultrashort echo time MRI to reference standard CT. Clin Imaging. 2016;40(1):90–5.
Yassin A, et al. In vitro MR imaging of renal stones with an ultra-short echo time magnetic resonance imaging sequence. Acad Radiol. 2012;19(12):1566–72.
Saw KC, et al. Helical CT of urinary calculi: effect of stone composition, stone size, and scan collimation. AJR Am J Roentgenol. 2000;175(2):329–32.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
SS assisted with attaining the imaging of xanthine stones using various modalities, and drafted the manuscript. QP obtained MRI imaging of the stones and provided technical parameters that were used, and assisted in editing the manuscript. AHS obtained CT imaging of the stones and provided technical parameters that were used, and assisted in editing the manuscript. BAD developed the concept for the study along with MCL, cultivated the stones, provided urological insight, and assisted in editing the manuscript. MCL developed the concept for the study along with BAD, oversaw preparation of the imaging of the stones and in editing the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Although the need for consent to participate was waived, informed consent for publication was obtained from the patient’s parent. The patient data was obtained from a patient at our institution. No administrative permissions and/or licenses were acquired by our team to access the data used in our research.
Consent for publication
Written informed consent was obtained from the patient’s parent.
Competing interests
B.A.D. is a consultant for Astellas Pharma Europe for a separate, unrelated study. M.C.L. received an industry grant from Carestream Health for a separate, unrelated study, Study # 17-10-77.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
In-vitro CT mean and SD values at four different KVP.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shamir, S.B., Peng, Q., Schoenfeld, A.H. et al. CT, US and MRI of xanthine urinary stones: in-vitro and in-vivo analyses. BMC Urol 20, 157 (2020). https://doi.org/10.1186/s12894-020-00736-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-020-00736-w