Abstract
Background
Nocturia is one of the most bothersome lower urinary tract symptoms and often impairs sleep quality in the elderly. Although previous studies on nocturia have indicated that the successful treatment of nocturia improves sleep quality, most used questionnaires and activity devices to analyze sleep/wake patterns. Therefore, there is little information about the treatment effects of desmopressin on objective sleep quality. The aim of the DISTINCT study is to investigate the change in subjective and objective sleep quality using electroencephalography (EEG) and the Pittsburgh Sleep Quality Index (PSQI) after the administration of desmopressin in patients with nocturia due to nocturnal polyuria.
Methods
A total of 20 male patients, ≥65 years old, with nocturnal polyuria, defined as a nocturnal polyuria index (NPi) (nocturnal urine volume / 24 h urine volume) value ≥0.33, will participate in this study. The participants must have a nocturnal frequency of ≥2 and the first uninterrupted sleep period (FUSP) must occur within < 2.5 h. Desmopressin 50 μg per day will be orally administered before going to bed for 4 weeks. Urinary frequency volume charts (FVC) and EEG will be recorded prior to treatment and at 1 week and 4 weeks after the initiation of treatment. The PSQI will be completed before and 4 weeks after treatment. The primary endpoint is the change from baseline in the mean time of slow-wave sleep (sleep stages N3 and N4) at 4 weeks. The secondary endpoints include the change in the mean value of each sleep variable, the mean delta power during the FUSP, the correlation between nocturnal urinary frequency and slow-wave sleep time, and the change in PSQI score before and after treatment.
Discussion
The DISTINCT study will provide valuable evidence to indicate that oral desmopressin treatment for nocturnal polyuria prolongs the FUSP, resulting in the extension of slow-wave sleep time associated with sleep quality.
Trial registration
The Japan Registry of Clinical Trials (jRCTs051190080). Registered 9 December, 2019.
Similar content being viewed by others
Background
Nocturia is a common disease in the elderly. One consequence of nocturia is the complaint of poor sleep quality due to polyuria and nocturnal voids [1]. Nocturia is defined by the International Continence Society as “The number of times urine is passed during the main sleep period. Having woken to pass urine for the first time, each urination must be followed by sleep or the intention to sleep” [2]. The prevalence of nocturnal urinary frequency ≥ 2 is 47% in Japanese residents ≥65 years old [3], 36% in European residents from 60 to 80 years old [4], and 14.2% in the United States (mean age of patients is 46 years) [5]. Nocturia correlates with age, race/ethnicity, medical problems (such as hypertension, diabetes, and stroke), psychological aspects, tasting habits, quality of life, and even mortality [6].
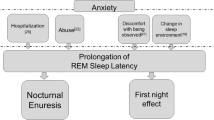
Nocturia causes poor sleep quality by prompting nocturnal voids during the first uninterrupted sleep period (FUSP) [7, 8]. Nocturia increases the number of nocturnal voids, and nocturnal voiding has been shown to be an independent predictor of both self-reported insomnia (75% increased risk) and reduced sleep quality (71% increased risk), along with female gender and other medical psychiatric conditions [7]. Nocturia decreases the FUSP, and the FUSP is a potentially valuable metric that correlates with changes in perceived sleep duration, depth, quality of sleep for the entire night, efficiency, and latency, as evaluated by Pittsburgh Sleep Quality Index (PSQI) [8]. The FUSP has a close relationship with slow-wave, or non-REM, sleep. Sleep stages are divided from 1 to 4, and slow-wave sleep occurs during stages N3 and N4. Stages N3 and N4 commonly occur during the first two sleep cycles (about 180 min after falling asleep) and are considered important for high-quality sleep [9].
We hypothesize that desmopressin treatment for nocturia will improve subjective and objective sleep quality. Desmopressin 25 and 50 μg orally disintegrating tablets are now available worldwide for nocturia and have been shown to decrease the number of nocturnal voids [10]. It is reported that subjective sleep quality, estimated by a quality of life questionnaire, was improved by desmopressin treatment [11]. Desmopressin prolonged the FUSP, suggesting that the slow-wave sleep time might also have been prolonged, although this has not been investigated.
The aim of the DISTINCT study is to use electroencephalography (EEG) and PSQI to investigate the change in subjective and objective sleep quality after the administration of desmopressin to patients with nocturia due to nocturnal polyuria.
Methods/design
This is a single-arm, open-label, single-assignment study. It is an exploratory study to compare subjective and objective sleep qualities after 1 week and 4 weeks of desmopressin treatment for nocturnal polyuria (Fig. 1). Qualifying patients will be males, ≥65 years old, and suffering from insomnia due to nocturnal polyuria, defined as a nocturnal polyuria index (NPi) value (nocturnal urine volume / 24 h urine volume) of ≥0.33 [2].
Study design. A total of 20 patients with nocturnal polyuria will participate in this study. After the conformation of eligibility, the enrolled patients will be treated with oral desmopressin 50 μg per day. In the pre-screening period, 2-day frequency volume chart (FVC) and sleep encephalography (EEG) will be recorded and the Pittsburgh Sleep Questionnaire Index (PSQI) will be completed. Before visit Day 0, 2-day FVC and EEG will be recorded. Before visit Day 7 and Day 28, 2-day FVC and EEG will be recorded. On visit Day 28, the PSQI will be completed
This study will be conducted at Nara Medical University Hospital in compliance with both the articles of the Declaration of Helsinki (revised in October 2013) and the Ethical Guidelines for Medical and Health Research Involving Human Subjects established by the Ministry of Health, Labor, and Welfare in Japan.
Planned outcomes
Primary endpoint
The primary endpoint is the change in mean time of slow-wave sleep (stages N3 and N4) as evaluated by EEG at 28 days from baseline (Table 1).
Secondary endpoints
The secondary endpoints are listed in Table 1.
Safety endpoints
Data on the clinical trial results, vital sign measurements, and adverse events (AEs), especially signs of hyponatremia, will be collected at each visit. The severity, causal relationship to desmopressin, and outcomes of all AEs will be assessed.
Study population
A total of 20 male patients, ≥65 years old, with nocturnal polyuria, will participate in this study. The participants must have nocturnal frequency ≥ 2 and NPi ≥0.33, which will be recorded by 2-days FVC. Patients will be considered eligible for the study if they fulfill all of the inclusion criteria and none of the exclusion criteria, as defined in Table 2. The investigator will provide a sufficient explanation of the study to each patient and obtain written informed consent prior to the initiation of any study procedures.
Treatment
Patients will be provided with desmopressin 50 μg (as MINIRINMELT® OD Tablets 25 μg / 50 μg; Ferring Pharmaceuticals Co., Ltd., Tokyo, Japan) to be orally administered once daily prior to going to bed. The drug has been approved only for male patients with nocturnal polyuria in Japan.
Measurements
The schedule of data collection is detailed in Table 3. A window of ±2 days is acceptable.
Informed consent and registration
The principal investigator or co-investigator will explain the study to each eligible participant, using the informed consent documents. Participants who give written informed consent will be registered in this study. Registration will be closed when the planned total number of participants (20 participants) is reached.
Data collection
Patient characteristics will include age, height, weight, and medical history. Blood tests performed at pre-screening will evaluate the following clinical chemistry analytes: serum creatinine, estimated glomerular filtration rate, sodium (Na), potassium, chlorine (Cl), brain natriuretic peptide, fasting blood glucose, white blood cell count, red blood cell count, hemoglobin content, hematocrit, platelet count, total protein, albumin, blood urea nitrogen, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, and gamma-glutamyl transferase. Blood tests performed during the treatment period will evaluate Na and Cl.
A mobile EEG device, Sleep Graph® (Proassist, Ltd., Osaka, Japan), will be used for EEG recordings. The device is small, easy to carry, and well-validated by standard methods (polysomnography) [12]. The device records brain-waves during sleep, which indicate sleep stages.
The FVC will be recorded by the patients independently to assess the nocturnal frequency and nocturnal urine volume. The results of the visual analog scale (VAS) will be used as additional indicators of subjective sleep quality on days when FVC and EEG are recorded. The VAS is a measurement instrument that asks patients to rate their sleep from “I could sleep well” (left end of the scale) to “I could not sleep at all” (right end of the scale). Subjective sleep quality will be assessed by the length between the left end and the point at which a patient records their sleep rating.
Sample size calculation
This study is designed to demonstrate a statistically significant difference in the change from baseline in slow-wave sleep time in patients treated with desmopressin 50 μg with overall power of 80% and an overall Type 1 error rate of 5% (two-sided). The R program was used for sample size calculation. Bliwise et al. reported that in 15 patients studied, 8 patients had one or two voids, and 7 patients had three or four voids, showing a trend for higher amounts of N3 sleep at 81.4 ± 28.8 min vs 48.2 ± 40.7 min, respectively, assuming a total sleep time of 6 h [13]. Based on these data, we assumed 33.2 min as the difference between both groups and 35.7 min as the standard deviation, and determined that data from 13 subjects will be needed to detect a significant difference from baseline. Considering subject withdrawal, missing data, and feasibility, we assume 20 subjects will be sufficient.
Statistical analysis
Primary endpoint
A Wilcoxon matched-pairs signed rank test would be used to compare the mean time of slow-wave sleep (N3 + N4) at Day 26 or 27 with that at baseline.
Secondary endpoints
A Wilcoxon matched-pairs signed rank test will be used to compare the mean score of the PSQI at Day 28 with that at baseline, and the mean time of slow-wave sleep (N3 + N4) at Day 5 or 6 with that at baseline. Friedman’s test and Dunn’s multiple comparisons test will be used to compare the change in mean total sleep time, mean sleep efficiency, mean sleep latency, mean VAS, mean time of sleep stages, and delta power during the FUSP from baseline to Day 26 or 27. The dependency between the mean time of slow-wave sleep (N3 + N4), the score of the PSQI, VAS, FUSP, number of voids, delta power during the FUSP, and other baseline characteristics will be analyzed using a linear regression model at Day 28. The significance level for statistical tests will be 0.05 on two sides.
Discussion
The aim of the DISTINCT study is to investigate the change in subjective (measured by PSQI) and objective (measured by EEG) sleep quality after the administration of desmopressin to patients with nocturia due to nocturnal polyuria. One of the treatment goals for nocturia is to prolong the FUSP because slow-wave sleep, which is important for brain rest, appears early in sleep. Desmopressin, which has world-wide marketing authorization, has been demonstrated as safe and efficacious in prolonging the FUSP. However, the prolongation of slow-wave sleep time following desmopressin use has not been studied. The DISTINCT study addresses this gap in the research.
Additionally, this study will rely on a novel approach for measuring objective sleep quality. The standard method for analyzing sleep stages is polysomnography, which requires placing many sensors on a patient’s head and body, and can be performed only in laboratories. Therefore, it is difficult for nocturia patients who go to the toilet for voiding to undergo polysomnography, which fixes patients to the bed during the sleep period. The portable EEG device used in this study does not restrain patients and was demonstrated as useful in our previous study, which demonstrated the linkage between sleep quality assessed by the PSQI and slow-wave sleep time [14].
This study has several limitations, including a small number of patients, and an open-label, single-arm modality. However, the results will provide valuable evidence by which to demonstrate the positive effects of desmopressin on objective sleep quality, which is associated with the occurrence of deeper sleep stages in patients with nocturnal polyuria.
Availability of data and materials
Not applicable.
Abbreviations
- FUSP:
-
First uninterrupted sleep period
- PSQI:
-
Pittsburgh Sleep Quality Index
- EEG:
-
Electroencephalography
- NPi:
-
Nocturnal polyuria index
- AE:
-
Adverse event
- Na:
-
Sodium
- Cl:
-
Chlorine
- VAS:
-
Visual analog scale
- FVC:
-
Frequency volume chart
References
Asplund R. Nocturia, nocturnal polyuria, and sleep quality in the elderly. J Psychosom Res. 2004;56:517–25.
Hashim H, Blanker MH, Drake MJ, Djurhuus JC, Meijlink J, Morris V, et al. International Continence Society (ICS) report on the terminology for nocturia and nocturnal lower urinary tract function. Neurourol Urodyn. 2019;38:179–83.
Hirayama A, Torimoto K, Mastusita C, Okamoto N, Morikawa M, Tanaka N, et al. Evaluation of factors influencing the natural history of nocturia in elderly subjects: results of the Fujiwara-kyo study. J Urol. 2013;189:980–6.
Bing MH, Moller LA, Jennum P, Mortensen S, Skovgaard LT, Lose G. Prevalence and bother of nocturia, and causes of sleep interruption in a Danish population of men and women aged 60-80 years. BJU Int. 2006;98:599–604.
Coyne KS, Zhou Z, Bhattacharyya SK, Thompson CL, Dhawan R, Versi E. The prevalence of nocturia and its effect on health-related quality of life and sleep in a community sample in the USA. BJU Int. 2003;92:948–54.
Yoshimura K. Correlates for nocturia: a review of epidemiological studies. Int J Urol. 2012;19:317–29.
Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med. 2009;10:540–8.
Bliwise DL, Holm-Larsen T, Goble S. Increases in duration of first uninterrupted sleep period are associated with improvements in PSQI-measured sleep quality. Sleep Med. 2014;15:1276–8.
Stanley N. The underestimated impact of nocturia on quality of life. Eur Urol. 2005;Suppl 4:17–9.
Weiss JP, Herschorn S, Albei CD, van der Meulen EA. Efficacy and safety of low dose desmopressin orally disintegrating tablet in men with nocturia: results of a multicenter, randomized, double-blind, placebo controlled, parallel group study. J Urol. 2013;190:965–72.
Kerrebroeck P, Rezapour M, Cortesse A, Thüroff J, Riis A, Nørgaard JP. Desmopressin in the treatment of nocturia: a double-blind, placebo-controlled study. Eur Urol. 2007;52:221–9.
Nonoue S, Mashita M, Haraki S, Mikami A, Adachi H, Yatani H, et al. Inter-scorer reliability of sleep assessment using EEG and EOG recording system in comparison to polysomnography. Sleep Biol Rhythms. 2017;15:39–48.
Bliwise D, Dijk DJ, Juul KV. Nocturia is associated with loss of deep sleep independently from sleep apnea. Neurourol Urodyn. 2015;34:392.
Matsushita C, Torimoto K, Goto D, Morizawa Y, Kiba K, Shinohara M, et al. Linkage of lower urinary tract symptoms to sleep quality in elderly men with nocturia: a community based study using home measured electroencephalogram data. J Urol. 2017;197:204–9.
Acknowledgements
We would like to thank Dr. Nagaaki Marugami, who belongs to Department of Radiology and Nuclear Medicines, Nara Medical University and has agreed to monitor this study.
Funding
Ferring Pharmaceuticals Co., Ltd. funded this study and supported the protocol preparation.
Author information
Authors and Affiliations
Contributions
All authors were involved in the planning and execution of the DISTINCT study. TK was a major contributor in writing the manuscript with help of NY. MM was responsible for statistical design and analysis. AK and TN interpreted the existing patient data regarding nocturnal polyuria and sleep disorder. FK critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In accordance with the law for clinical research in Japan, the protocol of this study was approved by the Nara Medical University Certified Review Board (Approval Number; nara0012). This study is conducted in compliance with the articles of the Declaration of Helsinki (revised in October 2013) and in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects established by the Ministry of Health, Labor, and Welfare in Japan. This study is also conducted in accordance with the law for clinical research in Japan (the Clinical Trials Act). In accordance with the Japanese Clinical Trials Act, this study is also registered in the Japan Registry of Clinical Trials (jRCTs051190080). The principal investigator or co-investigator will provide an explanation regarding the study to each eligible participant, using informed consent documents approved by the review board. Participants who give written informed consent will be registered in this study.
Consent for publication
All named authors take responsibility for the integrity of the work as a whole and have given their approval for this paper to be published.
Competing interests
The funding of this protocol by the manufacturer of desmopressin is a competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Torimoto, K., Miyake, M., Nakai, Y. et al. Rationale, design, and methods of electroencephalography-based investigation of the effects of oral desmopressin on improving slow-wave sleep time in nocturnal polyuria patients (the DISTINCT study): protocol for a single-arm, open-label, single-assignment trial. BMC Urol 20, 96 (2020). https://doi.org/10.1186/s12894-020-00668-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-020-00668-5