Abstract
Background
The appropriate application of various treatment for upper tract urothelial carcinomas (UTUCs) is the key to prolong the survival of UTUC patients. Herein, we used data in our database to assess the oncological outcomes between partial ureterectomy (PU) and radical nephroureterectomy (RNU).
Methods
From 2007 to 2014, 255 patients with UTUC undergoing PU or RNU in our hospital database were investigated. Perioperative, postoperative data, and pathologic outcomes were obtained from our database. Cancer-specific survival (CSS) was assessed through the Kaplan-Meier method with Cox regression models to test the effect of these two surgery types.
Results
The mean length of follow-up was 35.8 months (interquartile range 10–47 months). Patients with high pT stage (pT2–4) suffered shorter survival span (HR: 9.370, 95% CI: 2.956–29.697, P < 0.001). There were no significant differences in CSS between PU and RNU (P = 0.964). In the sub-analysis, CSS for RNU and PU showed no significant difference for pTa–1 or pT2–4 tumor patients (P = 0.516, P = 0.475, respectively).
Conclusions
PU is not inferior to RNU in oncologic outcomes. Furthermore, PU is generally recognized with less invasive and better renal function preservation compared with RNU. Thus, PU would be rational for specific patients with UTUCs.
Similar content being viewed by others
Background
Upper tract urothelial carcinomas (UTUCs), as a kind of urothelial carcinomas (UCs), accounting for only 5–10% [1]. Generally, 60% of UTUCs are invasive [2]. Seventy to Ninety years old showed the highest morbid risk among all age groups and are three times more ordinary in men [2]. UTUC with pure nonurothelial histology is quite rare, but about 25% of cases have variants. Computed tomography (CT) is an available imaging technique with high diagnostic accuracy [3]. In about 90% of cases, the tumor grade can be determined with a low false negative rate [4]. Ureteroscopic biopsy combining with urinary cytology, and imaging findings such as hydronephrosis may contribute for the decision of surgical type like partial ureterectomy (PU) and radical nephroureterectomy (RNU) [5]. Tumor stage and grade, lymph node involvement, lymphovascular invasion, surgical margins, and pathological factors could be used to estimate prognosis [2]. Nowadays, the concept for preservation of renal function has been emphasized. For low-risk UTUC, kidney-sparing surgery (KSS) unlike radical surgery could preserve kidney function without compromising oncological outcomes. KSS such as PU are performed for the patients with solitary kidney, renal insufficiency, or low-risk tumors. RNU is still the standard treatment for high-risk UTUCs, no matter where the tumor location is [2, 6]. Herein, we used data in our database to assess the oncological outcomes between PU and RNU.
Methods
Study population and treatment
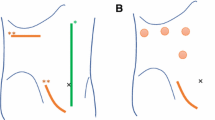
The research protocol was approved by the ethics committee of Jilin University’s Institutional Ethical Review Board, and written informed consent was obtained. Three hundred thirty two patients with UTUC from January 2007 to December 2014 in our database were included in First Hospital of Jilin University. Of them, 52 patients were excluded for suspected multifocal tumors in the upper urinary tract preoperatively. Another 25 patients were excluded for distant metastases (n = 14), no surgical treatment (n = 3), suffering previous or concurrent radical cystectomy (n = 8). Among the remaining 255 patients, 182 of them underwent RUN, 73 of them underwent PU. All Patients were evaluated disease progression by CT preoperatively. During the study period, ureteroscopy with biopsy was not routinely performed. The choice and surgical technique of RNU and PU could not be standardized. Surgeon preferences have a significant impact on the selection and surgical technique of RNU and PU. For RNU, the kidney and entire ureter with a bladder cuff were excised. PU was performed along with the excision of ureteral segment. There were no statistically differences between age at surgery, sex, tumor side, presence of hematuria, and presence of hydronephrosis. Clinical and pathological staging was in accordance with TNM classification 2002 [7, 8].
Statistical analysis
Outcomes were measured by survival time (from the time of surgery to cancer specific mortality). Continuous variables were described as the median (interquartile range). T tests or nonparametric tests were carried out to assess the differences in variables with a continuous distribution. Categorical variables were described as the frequency (percentage) and analyzed by the Chi-square or Fisher exact test. The Cox proportional hazard models were employed for univariate and multivariate analyses to determine whether surgery type (RNU vs PU) and other variables was associated with CSS. The survival curves of each stratified variablewere plotted by the Kaplan-Meier method and compared by log-rank test. SPSS version 18.0 (SPSS Inc., Chicago, IL) was used for statistical analyses. All P values were two-tailed, and P value < 0.05 indicated statistical significance.
Results
Clinicopathological characteristics
The mean length of follow-up was 35.8 months (interquartile range 10–47 months). The baseline characteristics of the patients are shown in Table 1. The mean age and percent of male in RNU group were 66.74 ± 8.41 and 49.5%, respectively; 67.62 ± 10.09 and 41.4% in PU group, respectively. Smokers in RNU group were much more than in PU group (38.2% vs 15.6%, P = 0.021). In RNU group, half of the patients had tumor in the left kidney (54.1%). PU group is contrary to it (39.7%). The proportion of patients with hydronephrosis, hematuria or abnormal renal function in RNU group were close to PU group (P > 0.05). Compared with PU group,operation time of patients in RNU group was much longer (157.50 (116.25–180.00) vs 95.00 (76.25–126.25), P < 0.001). In RNU group, nearly half (42.0%) were diagnosed at pT stage1, 5.2% at pT stage a, 27.6% at pT stage 2, 23.6% at pT stage 3, and only 1.7% at pT stage4. In PU group, the proportion is 49.3, 3, 37.3, 9, and 1.5%, respectively.
Oncological outcome
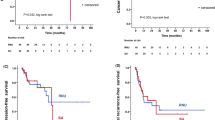
Univariable and multivariable analyses for CSS after surgery were shown in Table 2. On multivariable analysis, pT stage was significantly associated with CSS. The results showed that patients with high pT stage (pT2–4) suffered shorter survival span (HR: 9.370, 95% CI: 2.956–29.697, P < 0.001). The independent predictors of CSS were higher pT (P < 0.001; Table 2). The specific results are exhibited in Table 2. Furthermore, there were no significant differences in CSS between PU and RNU (P = 0.964) (Fig. 1). In the sub-analysis, there was no significant difference in 3-year CSS probability between pTa–1 tumor patients treated with RNU (87.7%) and PU (82.9%) (P = 0.516). Similarly, for patients with pT2–4 tumors, 3-year CSS for RNU and PU showed no significant difference (38.0% vs 31.3%, P = 0.475, respectively) (Fig. 2).
Discussion
UTUC is a kind of rare malignancy. The main treatments for URUC are RNU and KSS like PU. Recent data indicated that patients with low grade UTUC could be treated by PU effectively. The guidelines of the European Association of Urology suggested that PU is a legitimate therapy for small, unifocal, low grade UTUC with no signs of infiltration [2, 7, 9], and indicated that RNU is still the standard treatment for high-risk UTUCs [2, 10]. However, Bagrodia et al. compared the prognosis of UTUC patients who suffered either RNU or PU. They suggested that PU seemed to possess oncologic efficacy equal to RNU. Meanwhile, PU could preserve the renal function to the maximum extent [9]. Similar results were also demonstrated in the investigation from Fukushima et al. [11]. Colin et al. conducted a multicenter cohort study of UTUC which suggested that surgical interventions was not the independent prognostic factor for recurrence-free survival (RFS) and CSS [6]. The investigation from Hung et al. indicated that the local recurrences, bladder recurrences, distant metastasis, and CSS showed no significant differences between RNU and PU [12]. These findings mentioned above would show the ability of PU to maximize the preservation of renal function in carefully selected patients.
In the current study, we noticed that pathological stage remained the most important predictor for the CSS of patients with UTUCs. The results also revealed that CSS showed no significant differences between RNU and PU in both low pT stage (pTa–1) and high pT stage (pT2–4) UTUCs. The probable reason is that the number of patients involved in our study is not large enough, thus this study may not be powerful enough to show significance [6]. Furthermore, there were some selection biases that RNU group seemed to have more aggressive pathological features compared with PU group, because there was not the standardized indication for PU and surgeon preferred PU for lower stage UTUCs [13, 14]. Selection biases can lead to better survival in PU group compared with RNU group, though the difference was not significant in our analysis. Our findings, and similar findings from other researchers, indicated that PU could act as a selectable treatment for selected UTUC patients [15]. In addition, pathologists with expertise rechecked all the pathologic specimens, and all pathologic results were collected standardly.
This study is retrospective study, and the number of involved patients is relatively small. These two characteristics are the main limitations of this study. Because a prospective randomized controlled study of PU compared with RNU is difficult due to the rarity of UTUC. Secondly, we could not ascertain whether PU was done imperatively or electively. Furthermore, surgeon preferences have a great impact on the surgical technique and indication for RNU and PU, which could not be determined standardly. Nor can we assess which cases are suitable for endoscopic treatment when receiving RNU therapy [16, 17].. Multiple surgeons were employed to operate on the investigated patients. This situation might lead to a selection bias and variable surgical techniques. Finally, another limitation of our research is that we could not provide the information about tumor grade and metastases due to the sample problem.
Conclusion
In conclusion, PU and RNU might possess equivalent long-term oncologic outcomes. Furthermore, PU could reduce the adverse outcomes of nephron loss caused by RNU. PU could be rational selection for selected patients with UTUCs. Further randomized researches compared with PU and RNU are still necessary to support the results. Prospective trials with large sample sizes are essential to more accurately assess the role of PU in UTUC.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author on reasonable request.
Abbreviations
- CSS:
-
Cancer-specific survival
- CT:
-
Computed tomography
- KSS:
-
Kidney-sparing surgery
- PU:
-
Partial ureterectomy
- RFS:
-
Recurrence-free survival
- RNU:
-
Radical nephroureterectomy
- UC:
-
Urothelial carcinomas
- UTUC:
-
Upper tract urothelial carcinoma
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018;68(1):7–30.
Roupret M, Babjuk M, Comperat E, Zigeuner R, Sylvester RJ, Burger M, et al. European Association of Urology guidelines on upper urinary tract urothelial carcinoma: 2017 update. Eur Urol. 2018;73(1):111–22.
Zigeuner R, Shariat SF, Margulis V, Karakiewicz PI, Roscigno M, Weizer A, et al. Tumour necrosis is an indicator of aggressive biology in patients with urothelial carcinoma of the upper urinary tract. Eur Urol. 2010;57(4):575–81.
Rojas CP, Castle SM, Llanos CA, Cortes JAS, Bird V, Rodriguez S, et al. Low biopsy volume in ureteroscopy does not affect tumor biopsy grading in upper tract urothelial carcinoma. Urol Oncol: Semin Orig Invest. 2013:1696–700. https://doi.org/10.1016/j.urolonc.2012.05.010.
Clements T, Messer JC, Terrell JD, Herman MP, Ng CK, Scherr DS, et al. High-grade ureteroscopic biopsy is associated with advanced pathology of upper-tract urothelial carcinoma tumors at definitive surgical resection. J Endourol. 2012;26(4):398–402.
Colin P, Ouzzane A, Pignot G, Ravier E, Crouzet S, Ariane MM, et al. Comparison of oncological outcomes after segmental ureterectomy or radical nephroureterectomy in urothelial carcinomas of the upper urinary tract: results from a large French multicentre study. BJU Int. 2012;110(8):1134–41.
Amin MB, Greene FL, Edge SB, Compton CC, Gershenwald JE, Brookland RK, et al. The eighth edition AJCC cancer staging manual: continuing to build a bridge from a population-based to a more “personalized” approach to cancer staging. CA Cancer J Clin. 2017;67(2):93–9.
Mostofi FK, Sobin LH, Torloni H, Organization WH. Histological typing of urinary bladder tumours; 1973.
Bagrodia A, Kuehhas FE, Gayed BA, Wood CG, Raman JD, Kapur P, et al. Comparative analysis of oncologic outcomes of partial ureterectomy vs radical nephroureterectomy in upper tract urothelial carcinoma. Urology. 2013;81(5):972–7.
Seisen T, Peyronnet B, Dominguez-Escrig JL, Bruins HM, Yuan CY, Babjuk M, et al. Oncologic outcomes of kidney-sparing surgery versus radical Nephroureterectomy for upper tract urothelial carcinoma: a systematic review by the EAU non-muscle invasive bladder cancer guidelines panel. Eur Urol. 2016;70(6):1052–68.
Fukushima H, Saito K, Ishioka J, Matsuoka Y, Numao N, Koga F, et al. Equivalent survival and improved preservation of renal function after distal ureterectomy compared with nephroureterectomy in patients with urothelial carcinoma of the distal ureter: a propensity score-matched multicenter study. Int J Urol. 2014;21(11):1098–104.
Hung SY, Yang WC, Luo HL, Hsu CC, Chen YT, Chuang YC. Segmental ureterectomy does not compromise the oncologic outcome compared with nephroureterectomy for pure ureter cancer. Int Urol Nephrol. 2014;46(5):921–6.
Pedrosa JA, Masterson TA, Rice KR, Kaimakliotis HZ, Monn MF, Bihrle R, et al. Oncologic outcomes and prognostic impact of urothelial recurrences in patients undergoing segmental and total ureterectomy for upper tract urothelial carcinoma. Can Urol Assoc J. 2015;9(3–4):E187–92.
Simhan J, Smaldone MC, Egleston BL, Canter D, Sterious SN, Corcoran AT, et al. Nephron-sparing management vs radical nephroureterectomy for low- or moderate-grade, low-stage upper tract urothelial carcinoma. BJU Int. 2014;114(2):216–20.
Dalpiaz O, Ehrlich G, Quehenberger F, Pummer K, Zigeuner R. Distal ureterectomy is a safe surgical option in patients with urothelial carcinoma of the distal ureter. Urol Oncol. 2014;32(1):34 e31–8.
Fajkovic H, Klatte T, Nagele U, Dunzinger M, Zigeuner R, Hubner W, et al. Results and outcomes after endoscopic treatment of upper urinary tract carcinoma: the Austrian experience. World J Urol. 2013;31(1):37–44.
Cutress ML, Stewart GD, Tudor EC, Egong EA, Wells-Cole S, Phipps S, et al. Endoscopic versus laparoscopic management of noninvasive upper tract urothelial carcinoma: 20-year single center experience. J Urol. 2013;189(6):2054–60.
Acknowledgments
Not applicable.
Funding
We receive no funding support.
Author information
Authors and Affiliations
Contributions
SL: conception and design, data collection, statistical analysis, manuscript writing. YP: data analysis. JH: manuscript editing, supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures were approved by the Ethics Committee of First Hospital of Jilin University. Permission was obtained to access the data of First Hospital of Jilin University.
Consent for publication
The data do not contain any information that could identify the patient. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Li, S., Pan, Y. & Hu, J. Oncologic outcomes comparison of partial ureterectomy and radical nephroureterectomy for urothelial carcinoma. BMC Urol 19, 120 (2019). https://doi.org/10.1186/s12894-019-0557-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-019-0557-2