Abstract
Background
One of the greatest challenges presented with RIRS is the potential for movement of the stone within the operative field associated with diaphragm and chest respiratory excursions due to mechanical ventilation. To overcome this challenge, we propose in this pilot study a new general anesthesia technique combining high frequency jet ventilation (HFJV) with small volume mechanical ventilation (SVMV). Data regarding safety, feasibility and surgeons’ impression was assessed.
Methods
Patients undergoing RIRS for kidney stones from November 2017 to May 2018 were prospectively recruited to participate in the study. In each case after the beginning of general anesthesia (GA) with mechanical ventilation (MV) surgeons were asked to assess the mobility of the operative field and conditions for laser lithotripsy according to the developed questionnaire scale. The questionnaire consisted of 5 degrees of assessment of kidney mobility and each question was scored from 1 to 5, 1 being very mobile (extremely poor conditions for dusting) and 5 completely immobile (Ideal conditions for dusting).
After the assessment GA was modified with combined respiratory support (CRS), reducing tidal volume and respiratory rate (small volume mechanical ventilation, SVMV) and applying in the same time transcatheter high frequency jet ventilation (HFJV) inside the closed circuit.
After beginning of CRS, surgeons were once again asked to assess the mobility of the operative field and the conditions for laser lithotripsy. Main ventilation parameters were recorded and compared in both regimens.
Results
A total of 38 patients were included in the study. The mean age was 49 (range 45–53) with a mean stone size of 10 mm (range 10–14) and Hounsfield unit of 1060 (range 930–1190). All patients underwent successful RIRS and no intraoperative complications occurred throughout the duration of the study. A statistically significant difference between ventilation parameters prior to and after CRS institution was detected in all cases, however their clinical impact was negligible. Despite this, assessment via the questionnaire scale point values varied significantly before and after the application of CRS and were 2.3 (2.1; 2.6) and 3.8 (3.7; 4.0) respectively (p < 0.001).
Conclusions
The novel combined respiratory approach consisting of HFJV and SVMV appears to provide better conditions for stone dusting through reduced respiratory kidney motion and is not associated with adverse health effects or complications.
Trial registration
NCT03999255, date of registration: 25th June 2019 (retrospectively registered).
Similar content being viewed by others
Background
According to the currently established guidelines released by the European Association of Urology, retrograde intrarenal surgery (RIRS) via flexible ureterorenoscopy, is considered a well-established and effective procedure for the treatment of urolithiasis [1]. RIRS is most typically performed under general anesthesia (GA) with mechanical ventilation (MV) assistance, though can also be conducted under spinal or epidural anesthesia [2].
Regardless of anesthesia method one of the greatest challenges presented with RIRS is the potential for movement of the stone within the operative field associated with diaphragm and chest respiratory excursions due to MV. To overcome this impediment, Emiliani and Traxer suggested a technique known as periodic apnea (PA) to allow for momentary respites in respirations to facilitate stone removal and to minimize stone movements during laser lithotripsy [3]. However, surgeons may hesitate to induce PA due to relevant concerns of inducing hypercapnea. To circumvent these concerns, high frequency jet ventilation (HFJV) during GA has been suggested [4]. However, this method makes it impossible to use inhalational anesthetics and does not monitor end-tidal CO2 levels nor the volume of exhaled air [5].
Thus, to provide stability of the operative field during RIRS, we propose a modified technique of GA, referred to as combined respiratory support (CRS). It implies HFJV with small volume mechanical ventilation (SVMV). The purpose of this study is to perform a pilot study to assess the safety and feasibility of this technique during RIRS.
Material and methods
After obtaining approval by the local ethics committee, we performed a prospective, single-center study in patients undergoing RIRS for renal stones from November of 2017 to May of 2018. Patients with kidneys stones with indications for RIRS, who were eligible to enroll in this study, were identified by the appropriate research personnel via diagnosis at an outpatient clinic visit. All patients provided written consent to participate in the study. Patients consented to publish the data obtained during the study. Thorough explanation of the study was provided to patients, after which all provided signed, informed consent. Patients with ASA class of greater than 3 and active urinary tract infection were excluded from the study. All procedures were performed by two experienced endourologists [6].
Questionnaire
The secondary outcome of the study was to implement a subjective questionnaire in order to assess surgeon’s feedback on novel technique. The questionnaire consisted of 5 degrees of assessment of kidney mobility and each question was scored from 1 to 5, 1 being very mobile (extremely poor conditions for dusting), 2 being significantly mobile (unsatisfactory conditions for dusting), 3 being slightly mobile (satisfactory conditions for dusting), 4 almost immobile (good conditions for dusting) and 5 completely immobile (Ideal conditions for dusting) (Table 1). This was done in 2-step fashion in every patient and each patient served his own control: first, after the beginning of GA with MV in the mode of normal ventilation the questionnaire was implemented and surgeons were asked to assess the mobility of the operative field and the decency of conditions for laser lithotripsy. In addition to this assessment, anesthesia parameters including results of arterial blood gas analysis were recorded and evaluated in order to address safety concerns.
Second, novel CRS technique was then instituted and maintained throughout RIRS. Before lithotripsy itself surgeons were once again asked to assess the mobility of the operative field and conditions for laser lithotripsy according to the previously mentioned questionnaire. Monitoring of end-tidal carbon dioxide (EtCO2) level was carried out by intermittent capnography. Besides main anesthesia parameters with results of arterial blood gas analysis were recorded at the end of lithotripsy while on CRS for later comparison.
CRS technique
The concentration of Sevoflurane was increased from 1.4–2.6 vol% to 8 vol%. The following changes were then made to alter ventilation patterns: the tidal volume (Vt) (6–8 ml/kg IBW) and the respiratory rate (8–15 per minute) (RR) were decreased by 2–3 times, the ratio of inhalation to exhalation (I:E) was increased from 1:2 to 1:3, the fraction of inspired oxygen (FiO2) was decreased from 40 to 21% in the fresh gas flow (FGF) of 1.0 l/min. Transcatheter HFJV through tracheal tube was initiated with a ZisLINEJV-100 high frequency respirator (Triton-Electronics, Russia) with a respiratory cycle frequency (RCF) of 300 per minute, I:E = 1:3, FiO2 = 1.0 and working pressure (WP) 0.3–0.6 bar. Depth of anesthesia was measured by BIS Monitor (Covidien AG, Zurich, Switzerland).
Surgical technique
RIRS was performed with the patient in the lithotomy position with 7.5 Flex X2 ureteroscope (Karl Storz, Tuttlingen, Germany). Lithotripsy was performed with a holmium laser using 270 μm fibers at 0.3–0.5 J and 20–40 Hz (VersaPulse® PowerSuite™ 100 W) with patient under CRS. Dusting technique was utilized in all patients. A fragment was deliberately left to be extracted for stone analysis. Ureteral access sheath was used in 2 cases (stone size 14 mm).
Statistical analysis
Nonparametric resampling, permutation and randomization procedures (bootstrap and Monte Carlo) were applied for the statistical data analysis using software PAST [7]. Statistical significance of the observed effects was tested by p-values and confidence intervals (CIs). Threshold of 0.001 was considered as a critical significance level. For the expression of the clinical importance of findings, and their unification the so-called “standardized effect size” was used.
Results
A total of 38 patients were enrolled in the study with a mean age of 49 years (range 45–53). Mean body mass index was 27 kg/m2 (range 25–28). Mean ASA score was 2 (range 1–3). Mean stone size was 10 mm (range 10–14). Mean stone density was 1060 (range 930–1190). All cases were successful. Mean duration of RIRS was 26 min (range 20–32). Stone free rate in the study confirmed by ultrasound and KUB at 8 weeks was 86% (Table 2).
A statistically significant difference between ventilation parameters prior and after CRS institution was detected in all cases (Table 3). End-tidal CO2 with CRS implementation was 40 42 43 mmHg during RIRS which is in the range of normocapnia. No intraoperative complications occurred for any patients throughout the duration of the study. There was statistical significance in surgeons’ subjective questionnaire assessment points before and after the application of CRS 2.3 (2.1; 2.6) and 3.8 (3.7; 4.0) p < 0.0001, respectively (Table 2).
Surgeon’s impression assessed with the proposed questionnaire scale demonstrated that CRS leads to extremely high improvement in the stability of operative field (Fig. 1).
Discussion
Retrograde Intrarenal surgery is being increasingly used in renal stones. This is partly due to advancements in surgical and endoscopic technology. Although RIRS is less technically challenging then PCNL, laser lithotripsy can be challenging. Respiratory renal movement and proper laser settings are the two main contributing components of successful lithotripsy [8]. In order to minimize kidney displacement due to respiratory motion, several methods have been previously suggested including high frequency ventilation [9], PA [3], abdominal compression [10], and general anesthesia with low ventilation [11]. There have been many modifications suggested, but each technique has its own advantages and limitations.
Öberg and Sjöstrand were first to describe the HFJV in 1967 [9]. Initially it was utilized in otolaryngology, bronchial and lung surgery [12]. In the past decade, an increasing interest in HFJV’s advantages in keeping target organs relatively motionless during surgery to optimize surgical precision has grown. In regards to stone treatment, in 1988 Warner and colleagues were the first to demonstrate the potential benefits of HFJV for shock wave lithotripsy (SWL) and since then several studies have confirmed the benefits of HFJV in SWL [4, 13, 14]. Popiolek et al. was the first to present high frequency positive pressure ventilation in RIRS during the 2017 World Congress of Endourology, demonstrating the true necessity of stabilization of the operative field [15]. However, while high frequency ventilation may facilitate quicker stone removal via the occurrence of less adverse stone movements, this method also makes it impossible to use inhalational anesthetics and does not monitor end-tidal CO2 levels nor the volume of exhaled air [5]. Therefore in our opinion, high frequency ventilation remains a suboptimal approach toward anesthesiological support during RIRS.
The periodic apnea technique has been presented as useful during RIRS to minimize adverse motion of target organs [3]. This method uses preoxygenation with FiO2 of 1.0, followed by a MV pause. The criterion for starting over the ventilation was the SpO2 drop below 93%. However, there is a possible delay between the true SpO2 drop and the pulse oximeter readings [16, 17]. Prolonged apnea leads to an inevitable hypercapnea which, in turn, results in adverse effects in patients with compromised cardiovascular status, increased intracranial pressure, metabolic acidosis or hyperkalemia [18]. The hypoxemia tolerance varies highly depending on the patient’s individual condition. SpO2 decrease is usually accompanied by a compensatory circulatory system response, which requires shorter ventilation pauses in aged patients, while younger patients can tolerate up to 6 min apnea [19].
Abdominal compression in the form of belts or plates was previously described in SWL. Belt compression in a group of 50 patients provided reduction of the kidney motion amplitude by an average of 32% detected by fluoroscopy control [20]. Plate compression in a group of 10 volunteers and 10 patients reduced kidney motion by 4 mm on average and increased SWL efficacy by 23% detected by ultrasound control [10]. Currently, no information regarding the applicability of abdominal compression in RIRS exists. The technique of general anesthesia with low ventilation (LV) was previously described by Kourmpetis et al. who suggested the following settings of GA during RIRS: respiratory rate ≤ 8/min and tidal volume < 500 ml [11]. According to the results of their study, LV was associated with better fragmentation, removal, and processing rates but not operating rate. Although end-tidal CO2 in the LV group was 50 mmHg this finding was not associated with clinical side effects. However, this level of end-tidal CO2 is defined as mild hypercapnia and may cause possible negative health consequences [21].
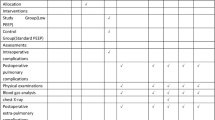
Our technique of combined two respiratory approaches, consisting of HFJV and SVMV, which thereby provided significantly better conditions for stone dusting assessed by expert urologists, all while precluding the development of hypercapnea. No CRS associated complications developed during or after the operation. In order to avoid any the following preventive measures were undertaken: the insufflation catheter was inserted through a sealed adapter into the tracheal tube thus, direct contact of the catheter with the trachea was excluded; development of tracheitis described in the literature is more attributed to the use of machines without gas conditioning option and the use of high pressure. We used “ZisLINEJV-100” machine with the air conditioning option and low working pressure of 0.3–0.6 bar; the heat and moisture exchanger filter was used in a closed respiratory circuit (Fig. 2).
Worth to mention disadvantages of CRS: expenditures associated with the cost of one insufflation catheter per patient; the necessity of purchasing HFJV machine; the inability to control the concentration of oxygen (FiO2) in some HFJV machines.
Our study has several limitations. First, our sample size was restricted to 38 patients. Despite this, we were able to demonstrate a statistically significant difference using the developed surgeon questionnaire scale; indicating that the use of CRS was beneficial. Secondly, our study lacks objective criteria for evaluation such as operating or fragmentation and dusting rates. However, we have deliberately simplified our study protocol due to the fact that variables such as fragmentation and dusting rates are inherently dependent on factors such as stone size, stone density, renal anatomy, the surgeon’s expertise, where the main factor being assessed in this study was operative field stability. Lastly, we didn’t corroborate our findings with the stone free rates of patients since we sought only to assess the feasibility and safety of reducing respiratory kidney motion and thus providing better conditions for intracorporeal lithotripsy. Due to the limitations of this pilot study, additional investigation will be needed to address the aforementioned concerns.
Conclusions
Our impression is that according to the urologist assessment the novel combined respiratory approach consisting of HFJV and SVMV provides better conditions for stone dusting through reduced respiratory kidney motion and is not associated with adverse health effects or complications. Further larger sample studies are needed to confirm these findings and elucidate its effect on stone free rates.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CRS:
-
Combined respiratory support
- GA:
-
General anesthesia
- HFJV:
-
High frequency jet ventilation
- MV:
-
Mechanical ventilation
- PA:
-
Periodic apnea
- RIRS:
-
Retrograde intrarenal surgery
- SVMV:
-
Small volume mechanical ventilation
- SWL:
-
Shockwave lithotripsy
References
Turk C, Petrik A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T, Türk C, Knoll T, Petrik A. EAU Guidelines on Urolithiasis. Eur Assoc Urol. 2018;69(3):475–82.
Zeng G, Zhao Z, Yang F, Zhong W, Wu W, Chen W. Retrograde intrarenal surgery with combined spinal-epidural vs general anesthesia: a prospective randomized controlled trial. J Endourol. 2015;29(4):401–5.
Emiliani E, Talso M, Baghdadi M, Ghanem S, Golmard J, Pinheiro H, Gkentzis A, Butticè S, Traxer O. The use of apnea during Ureteroscopy. Urology. 2016;97:266–8.
Mucksavage P, Mayer WA, Mandel JE, Van Arsdalen KN. High-frequency jet ventilation is beneficial during shock wave lithotripsy utilizing a newer unit with a narrower focal zone. Can Urol Assoc J. 2010;4(5):333–5.
Galm En K, Harbut P, Freedman J, Jakobsson JG. High frequency jet ventilation for motion management during ablation procedures, a narrative review. Acta Anaesthesiol Scand. 2017;61(9):1066–74.
Skolarikos A, Gravas S, Laguna MP, Traxer O, Preminger GM, De La Rosette J. Training in ureteroscopy: a critical appraisal of the literature. BJU Int. 2011;108(6):798–805.
Hammer Ø, Harper DAT, Ryan PD. Paleontological statistics software package for education and data analysis. Palaeontol Electron. 2001;4:9–18.
Matlaga B, Chew B, Eisner B, Humphreys M, Knudsen B, Krambeck A, ... Shah O. Ureteroscopic Laser Lithotripsy: A Review of Dusting vs Fragmentation with Extraction. Journal of Endourology. 2018;32(1):1-6. https://doi.org/10.1089/end.2017.0641.
Sjöstrand U. Review of the physiological rationale for and development of high-frequency positive-pressure ventilation--HFPPV. Acta Anaesthesiol Scand Suppl. 1977;64:7–27.
Bohris C, Stief CG, Strittmatter F. Improvement of SWL efficacy: reduction of the respiration-induced kidney motion by using an abdominal compression plate. J Endourol. 2016;30(4):411–6.
Kourmpetis V, Dekalo S, Levy N, Nir T, Bar-Yosef Y, Beri A, Yossepowitch O, Sofer M. Toward respiratory-gated retrograde intrarenal surgery: a prospective controlled randomized study. J Endourol. 2018;32(9):1–19.
Galmén K, Harbut P, Freedman J, Jakobsson JG. The use of high-frequency ventilation during general anaesthesia: an update. F1000Research. 2017;6:756.
Warner MA, Warner ME, Buck CF, Segura JW. Clinical efficacy of high frequency jet ventilation during extracorporeal shock wave lithotripsy of renal and ureteral calculi: a comparison with conventional mechanical ventilation. J Urol. 1988;139(3):486–7.
Cormack JR, Hui R, Olive D, Said S. Comparison of two ventilation techniques during general anesthesia for extracorporeal shock wave lithotripsy: high-frequency jet ventilation versus spontaneous ventilation with a laryngeal mask airway. Urology. 2007;70(1):7–10.
Popiolek M, Al-Rammahi D, Swartz R. The impact of high frequency positive-pressure ventilation on operation time in retrograde intrarenal surgery for stones <1 cm. J Endourol 2017;31:MP3-17.
Smith RA, Fu ES, Downs JB, Schweiger JW, Miguel RV. Hypoventilation by Pulse Oximetry; 2008.
Cacho G, Pérez-Calle JL, Barbado A, Lledó JL, Ojea R, Fernández-Rodríguez CM. Capnography is superior to pulse oximetry for the detection of respiratory depression during colonoscopy. Rev Esp Enferm Dig. 2010;102(2):86–9.
Wong DT, Yee AJ, Leong SM, Chung F. The effectiveness of apneic oxygenation during tracheal intubation in various clinical settings: a narrative review. Can J Anesth Can d’anesthésie. 2017;64(4):416–27.
Ramkumar V, Umesh G, Philip FA. Preoxygenation with 20o head-up tilt provides longer duration of non-hypoxic apnea than conventional preoxygenation in non-obese healthy adults. J Anesth. 2011;25(2):189–94.
Honey RJD, Healy M, Yeung M, Psihramis KE, Jewett MAS. The use of an abdominal Compression Belt to reduce stone movement during extracorporeal shock wave lithotripsy. J Urol. 1992;148(3):1034–5.
Pantazopoulos C, Xanthos T, Pantazopoulos I, Papalois A, Kouskouni E, Iacovidou N. A review of carbon dioxide monitoring during adult cardiopulmonary resuscitation. Hear Lung Circ. 2015;24(11):1053–61.
Acknowledgements
Not applicable.
Funding
None. There was no funding to support this study or publication.
Author information
Authors and Affiliations
Contributions
NG - Study conception & design and manuscript writing. UO - Study conception & design and manuscript writing. LK - Data collection and analysis. SPa - Study conception & design and manuscript writing. GA - Data collection and analysis. SPe - Study conception & design and manuscript writing. CMC - Manuscript writing and editing. ZO - Study conception & design, and manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Local ethics committee (Pavlov First Saint Petersburg State Medical University, Russia) approval was obtained to conduct this study. All patients provided written consent to participate in the study.
Consent for publication
The patient depicted in Fig. 2 gave written informed consent for publication of their photograph.
Competing interests
ZO is a member of the BMC Nephrology Editorial Board (Section Editor) and had no role in handling of this manuscript through peer review. All other authors declare that they have no financial or non-financial competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Gadzhiev, N., Oibolatov, U., Kolotilov, L. et al. Reducing kidney motion: optimizing anesthesia and combining respiratory support for retrograde intrarenal surgery: a pilot study. BMC Urol 19, 61 (2019). https://doi.org/10.1186/s12894-019-0491-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12894-019-0491-3