Abstract
Background
Patients with class I obesity may need metabolic and bariatric surgery (MBS) in the presence of obesity-associated medical problems, but MBS in this class of obesity is under debate. This study aimed to investigate the efficacy and safety of MBS in patients with class I obesity.
Methods and materials
This study was a historical cohort carried out on 112 patients with class I obesity with body mass index (BMI) of 30–35 kg/m2 with a 24-month follow-up underwent MBS at Rasoul-e-Akram Hospital. The required data were extracted through the Iran National Obesity Surgery Database. The data required for the study consisted of demographic information such as age, gender, and obesity-associated medical problems like type-2 diabetes mellitus (T2DM), hypertension, obstructive sleep apnea, and dyslipidemia before surgery, 6, 12, and 24 months after surgery.
Results
Mean age of the patients was 38.10 ± 10.04 years; mean BMI was 32.96 ± 1.35 kg/m2 and 83.9% (n = 94) of patients were female. Out of 18 patients with T2DM, 11 patients (61.11%) had complete remission and seven patients (38.88%) had partial remission. Obstructive sleep apnea, hypertension, dyslipidemia, and gastroesophageal reflux disease were observed in 18 (16.07%), 23 (20.53%), 43 (38.39%), and 13 patients (11.60%) before surgery and resolved at 24-month follow-up. Post-operative complications during the 24-month follow-up were checked to assess safety and there were no De novo gastroesophageal reflux disease, intolerance, leakage, pulmonary thromboembolism, deep vein thrombosis, incisional hernia, hypoalbuminemia (Albumin < 3.5 g/dl), excessive weight loss (BMI < 18.5 kg/m2) at any time during 24-months follow-ups and mortality. Early complications occurred as splenic injury in one case (0.89%), wound infection in one patient (0.89%), and extra-luminal bleeding in 10 (8.92%) after surgery, without any mortality.
Conclusion
MBS is safe and effective in class I obesity and can be considered in selected patients with obesity-associated medical problems.
Similar content being viewed by others
Introduction
It is estimated that more than 650 million people are obese worldwide [1]. Obesity as a global epidemic is associated with significant health, social, and economic consequences [2]. The association between obesity and psychological/psychiatric problems as well as many chronic diseases such as cardiovascular diseases, type 2 diabetes mellitus (T2DM), hypertension (HTN), physical disability and respiratory diseases has been confirmed [3]. Class I obesity, defined as having a body mass index (BMI) of 30 to 35 kg/m2, has been shown to be associated with a significant increased risk of developing diseases like type 2 diabetes, hypertension, dyslipidemia, obstructive sleep apnea (OSA), and mortality [4]. Extensive evidence supports the significant superiority of metabolic and bariatric surgery (MBS) over non-surgical treatment approaches in patients with a body mass index (BMI) of 27 or higher who are diagnosed with T2DM [5, 6]. Few studies have demonstrated the safety and efficacy of MBS in improving obesity-associated medical problems in class I obesity compared to higher BMI patients [7].
While BMI is a helpful tool for assessing obesity in patients, it is insufficient to classify obesity or determine whether metabolic and bariatric surgery (MBS) is necessary. Other scales, like the Edmonton Obesity Staging System (EOSS), take into account various aspects of obesity, including functional limitations and physical, psychologic, and psychiatric symptoms [8].
Despite new American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for MBS [9] that suggested MBS in suitable patients with class I obesity with obesity-associated medical problems that did not have a good respond to non-surgical treatments [10], and some studies confirmed the efficacy of MBS in weight loss and remission of obesity-associated medical problems such as hypertension (HTN), dyslipidemia (DLP) and type 2 diabetes mellitus (T2DM) in patients with Class I obesity [11,12,13], there are some concerns about MBS safety in this class of obesity.
This study aimed to evaluate the efficacy and safety of MBS in patients with class I obesity and obesity-associated medical problems in a two-year follow-up.
Methods and materials
Design and setting
This study was a historical cohort performed on 112 patients with class I obesity and at least one obesity-associated medical problem that did not have a good response to non-surgical therapies and underwent MBS at Rasoul-e-Akram hospital, an International Federation for the Surgery of Obesity and Metabolic Disorders center of excellence (IFSO-COE) for MBS. All patients underwent full evaluation by a multi-disciplinary team (MDT) before surgery. The patients were operated by one surgical team with the same techniques and had 24-month follow-up by MDT to evaluate weight loss and remission of obesity-associated medical problems and complications.
Eligibility criteria
Inclusion criteria were all patients (by census sampling method) with a body mass index of 30 to 35 kg/m2, aged between 18 and 75 years who underwent MBS in our center.
Surgical methods
RYGB
Patients were positioned in a slightly reversed Trendelenburg position, under general anesthesia, following the French technique. CO2 insufflation was carried out using a Veress needle, and an optical trocar was inserted in the midline, approximately 10 to 15 cm below the xiphoid process. Two 12-mm trocars were placed as the right and left working hands, while two 5-mm trocars served as an assistant and for liver retraction. A gastric pouch measuring six centimeters in length was constructed, utilizing a 36-French bougie. The gastrojejunostomy was created 100 cm from the Treitz ligament, and a 75 cm Roux limb was formed. The jejunojejunostomy was performed using a 30 mm white endo-stapler, closing both the Petersen and jejunojejunal defects with prolene 2 − 0 sutures.
SG
Following the initial steps mentioned previously, which included releasing the angle of His and performing gastrolysis, a sleeve gastrectomy (SG) was performed. The SG was carried out with purple linear endo-staplers, starting 4 cm proximal to the pylorus, over a 36-French bougie. Additionally, an omentopexy was performed along the entire length of the staple line.
OAGB
Similar to the initial steps described earlier, a narrow pouch was created distal to the Crow’s foot, using a 36-French tube. A side-to-side gastrojejunostomy was then performed, utilizing a linear 30-mm stapler, approximately 150 cm after the Treitz ligament.
Gastric plication
Gastrolysis was initiated 4 cm proximal to the pylorus, employing hemostatic devices, and continued until reaching the His angle about 2 cm from the esophago-gastric junction. Plication was performed in two rows, following a 36-French bougie as a guide.
Data collection
The required data were extracted through the Iran National Obesity Surgery Database (INOSD) [14] provided by a minimally invasive surgery research center. The data required for the study consisted of demographic information such as age and gender, obesity-associated medical problems like T2DM, HTN, OSA, gastroesophageal reflux disease (GERD), dyslipidemia and hypoalbuminemia before surgery, 6, 12, and 24-month after surgery extracted from the database.
Outcome definitions
Efficacy was defined as a remission/improvement of obesity-associated medical problems and weight loss outcomes such as total weight loss percent (%TWL) and Excess weight loss percent (%EWL). Safety was checked by assessing early complications such as leak, bleeding, and mortality and late complications such as hypoalbuminemia (Alb < 3.5 g/dl), de novo GERD, and excessive weight loss (BMI < 18.5 kg/m2) at any time during 24 months follow-ups [15].
The outcomes of associated medical problems (resolution/improvement) were defined based on “Standardized Outcomes Reporting In Metabolic And Bariatric Surgery“ [16].
T2DM (complete remission: HbA1c < 6%, FBG < 100 mg/dl in the absence of anti-diabetic medications; improvement: reduction in HbA1c and FBG (not meeting the criteria for remission) or decrease in anti-diabetic medication requirement [16].
Ethical issues
The research adhered to the fundamentals of the Declaration of Helsinki. The Ethical Committee of the Iran University of Medical Sciences approved the protocol for this study (#IR.IUMS.REC.1400.361).
Statistical analysis
To analyze the data, number and percentage indices were employed for qualitative variables, and quantitative variables mean, standard deviation, mean, and minimum-maximum value indices were utilized. Due to the normal distribution of the data, parametric tests were used such as repeated measure ANOVA, one-way ANOVA, and McNemar test for checking the binary status of obesity-associated medical problems. To check the significance of changes between groups (One anastomosis gastric bypass, Roux-en Y gastric bypass, sleeve gastrectomy, and gastric plication), one-way ANOVA was used for %TWL and %EWL indices at 6, 12, and 24-month follow up in which these indices was significantly different for %EWL at 6-month follow up. Efficacy also was checked by assessing remission of OSA, HTN, dyslipidemia, and T2DM. All descriptive tables and statistical tests were prepared using SPSS software version 21 and the statistical significance level was considered 0.05.
Results
The mean age of the patients was 38.10 ± 10.04 years; the mean BMI was 32.96 ± 1.35 kg/m2 and 83.9% (n = 94) of patients were female (Table 1). The most common type of surgery was Roux-en-Y gastric bypass (RYGB) that performed on 61 patients. The type of MBS is shown in Fig. 1.
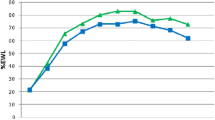
The type of MBS was not an effective factor for %TWL or %EWL changes (Table 2). %TWL trend is shown in Fig. 2. Out of 18 patients with T2DM, 11 patients (61.11%) had complete remission (HbA1C less than 6 and FBS less than 100) and seven patients (38.88%) had partial remission (HbA1C less than 6.5 and FBS less than 125). OSA was observed in 18 patients (16.07%) before surgery and reached zero at 24-month follow-up. HTN was observed in 23 patients (20.53%) before surgery and reached zero at 24-month follow-up. Dyslipidemia was observed in 43 patients (38.39%) before surgery and reached zero at 24-month follow-up. Also, GERD was observed in 13 patients (11.60%) before surgery and reached zero at 24-month follow-up (Table 3).
Post-operative complications during the 24-month follow-up were checked to assess the safety as reported based on the Clavien-Dindo classification in Table 4.
Discussion
The findings of this study provide compelling evidence supporting the effectiveness and safety of metabolic and bariatric surgery (MBS) in patients with Class I obesity, as demonstrated in two years of follow-up. Regardless of the specific type of MBS procedure performed, our patients experienced no instances of mortality and did not exhibit excessive weight loss.
According to the updated guidelines from the 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) [9], the indications for metabolic and bariatric surgery have changed from the previous NIH criteria [17]. According to the new guidelines, individuals with a BMI of 30-34.9 kg/m2, who have metabolic disease and have not achieved significant or long-lasting weight loss or improvement in co-morbidities through non-surgical methods, should be considered for MBS.
Class I obesity is associated with an increased risk of various conditions, including T2DM, HTN, DLP, metabolic syndrome, non-alcoholic fatty liver disease (NAFLD), and obesity-related cancers. However, relying solely on BMI as a criterion for MBS may not provide a complete picture, as BMI alone does not accurately reflect the individual’s underlying biological factors [18].
To address this limitation, alternative classification tools such as the Edmonton Obesity Staging System (EOSS) take into account multiple aspects of obesity, including physical symptoms, psychological/psychiatric symptoms, and functional limitations. These comprehensive tools offer a more accurate prediction of total obesity-related mortality and can effectively identify patients who are genuine candidates for MBS. Therefore, considering additional factors beyond BMI is crucial in determining the appropriate candidates for MBS [18].
On the other hand, the suggestion of MBS only according to BMI may not be completely true, because BMI alone cannot be a perfect predictor of patients’ body biological components [18].
So, other classification tools such as the Edmonton Obesity Staging System (EOSS) which includes all aspects of obesity such as physical, psychologic/psychiatric symptoms, and functional limitations are more accurate in predicting total obesity-related mortality and can be useful for determining which patients are true candidates for MBS [8]. According to a recently published global survey, there are different MBS approaches in the treatment of patients with low BMI around the world [19].
The most important issue is the safety of MBS in these patients which should be evaluated in different studies. In a study conducted by Jackson et al., the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP) database was evaluated to assess the safety of MBS in patients with class I obesity. The findings of the study confirmed the short-term safety of MBS in this specific patient population. The analysis provided evidence supporting the favorable safety profile of MBS procedures for individuals with class 1 obesity [7].
In this study, we did not find any significant morbidity after MBS. We did not have any hypoalbuminemia, but anemia occurred in 4 (3.57%) of the patients who were all treated with Iron supplement prescription. Maiz et al., reported anemia in 0.5% and 1.8% of patients with class I obesity who underwent sleeve gastrectomy (SG) and RYGB respectively at one-year follow-up [20]. They also reported 1.1% portomesenteric vein thrombosis in 1.1% of patients who underwent SG and 0.2 and 0.4% leak after SG and RYGB respectively [20].
In a study conducted by Verban et al., [11] the outcomes of patients who underwent primary SG were compared between those with a BMI below 35 kg/m2 and those with a BMI equal to or above 35 kg/m2. The results revealed that patients with lower BMI experienced higher resolution rates for T2DM, HTN, and DLP. Additionally, they were more likely to achieve a normal weight following SG.
Studer et al. reported the 5-year outcomes of RYGB and SG in a group of 37 patients with class I obesity. They found that remission of HTN was achieved in 42% of the patients, and remission of DLP was observed in 64% of the cases. They also noted a 12% incidence of de novo reflux after SG, with no excessive weight loss or mortality observed [12].
Kular et al. reported anemia (3.9%), hypoalbuminemia (0.8%), excessive weight loss (2.3%), and bile reflux (0.8%) in patients with class I obesity who underwent one anastomosis gastric bypass (OAGB) in a 7-year follow-up which all treated by conservative management [21]. Hong et al. and Cevallos et al. also confirmed the safety of SG in this class of obesity [22, 23].
According to a study conducted by Gamme et al., there was no statistically significant difference in the risk of postoperative complications between individuals with class I obesity and those with Class II and higher obesity after SG and RYGB. The study’s findings indicate that patients in Class I obesity do not face a higher risk of postoperative complications compared to individuals with higher levels of obesity [24].
This study similar to previous studies confirms the safety of MBS in patients with class I obesity.
Although BMI alone cannot predict the T2DM outcomes after medical or surgical treatment modalities [25], it has been demonstrated that MBS has a more significant and durable effect on remission and improvement of T2DM compared to non-surgical treatments such as GLP-1 analog, SGLT-2 inhibitors in patients with BMI < 35 Kg/m2 [26, 27].
According to our study, 11 out of 18 patients (61.1%) achieved complete remission and seven (38.9%) achieved partial remission after undergoing MBS, with a two-year follow-up.
In a study by Cevallos et al., 73.8%, 52.2%, and 50% of patients saw complete remission of T2DM after 24, 36, and 60 months, respectively [23]. Berry et al. reported complete and partial remission in 60% and 40% of patients, respectively, after a three-year follow-up after SG [28]. Baldwin et al. reported 100% remission in T2DM at 12 months after SG and RYGB in Patients with class I obesity [29].
The current study showed complete remission of OSA, GERD, DLP, and HTN in 100% of patients in our 2-year follow which confirms the efficacy of MBS in remission of obesity-associated medical problems in patients with class I obesity. These excellent results are reported in similar previous studies with different metabolic/bariatric surgical procedures [20, 28,29,30,31].
Our study also found that the weight loss outcomes after OAGB, RYGB, gastric plication, and SG were 33.58%, 31.59%, 22.29%, 26.50% in terms of total weight loss percentage, and 87.46%, 74.83%, 62.53%, and 75.41% in terms of excess weight loss percentage (EWL%), respectively. These results are consistent with previous studies and further support the efficacy of MBS in weight loss for patients with class I obesity. It is important to note that MBS should only be considered after non-surgical treatments have failed for patients with class I obesity and related diseases [20, 22, 23, 28,29,30, 32] that confirm the efficacy of different types of MBS in weight loss outcomes in patients with class I obesity.
In patients with class I obesity, MBS should be considered after the failure of non-surgical treatments such as medical therapies and lifestyle modification in the treatment of obesity and weight-related diseases [10].
Limitations of the study
Our study represents an acceptable sample size with a year’s follow to evaluate class I obesity patients who have undergone MBS. Also, we assessed the effects of different types of MBS on obesity-related diseases. However, we acknowledge several limitations. The study was retrospective with the limitations of this design. Because of this, we had to deal with a lack of information and insufficient follow-up resulting in low cases. Additionally, MBS was performed by different surgeons, and surgical technique details for example biliopancreatic limb length were not included in this study.
Hopefully, further larger trials with longer follow-ups would generate the necessary evidence to allow a better patient selection for MBS based on their associated conditions and individual considerations in low BMI patients.
Conclusion
Class I obesity is accompanied by many obesity-associated medical problems that treated in the early stages could avoid becoming more severe. Our study showed that MBS is a safe and effective option that allows patients to reach a successful weight loss with considerable obesity-associated medical problems remission and a low rate of complications. Further studies are needed to investigate the results of MBS in patients with low BMI in the long run.
Data availability
The datasets used during the current study are available from the the corresponding author on reasonable request.
References
Smith KB, Smith MS. Obesity statistics. Prim Care. 2016;43(1):121–35. ix.
Puhl RM, Heuer CA. Obesity stigma: important considerations for public health. Am J Public Health. 2010;100(6):1019–28.
Burgmer R, Legenbauer T, Müller A, de Zwaan M, Fischer C, Herpertz S. Psychological outcome 4 years after restrictive bariatric Surgery. Obes Surg. 2014;24(10):1670–8.
Cerci M, Bellini MI, Russo F, Benavoli D, Capperucci M, Gaspari AL, et al. Bariatric Surgery in moderately obese patients: a prospective study. Gastroenterol Res Pract. 2013;2013:276183.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, et al. Bariatric Surgery versus Intensive Medical Therapy for Diabetes – 5-Year outcomes. N Engl J Med. 2017;376(7):641–51.
Rao WS, Shan CX, Zhang W, Jiang DZ, Qiu M. A meta-analysis of short-term outcomes of patients with type 2 Diabetes Mellitus and BMI ≤ 35 kg/m2 undergoing Roux-en-Y gastric bypass. World J Surg. 2015;39(1):223–30.
Jackson TN, Cox BP, Grinberg GG, Yenumula PR, Lim RB, Chow GS, et al. National usage of bariatric Surgery for class I obesity: an analysis of the metabolic and bariatric Surgery Accreditation and Quality Improvement Program. Surg Obes Relat Diseases: Official J Am Soc Bariatr Surg. 2023;19(11):1255–62.
De Luca M, Angrisani L, Himpens J, Busetto L, Scopinaro N, Weiner R, et al. Indications for Surgery for obesity and weight-related Diseases: position statements from the International Federation for the Surgery of Obesity and metabolic disorders (IFSO). Obes Surg. 2016;26(8):1659–96.
Eisenberg D, Shikora SA, Aarts E, Aminian A, Angrisani L, Cohen RV et al. 2022 American Society of Metabolic and Bariatric Surgery (ASMBS) and International Federation for the Surgery of Obesity and Metabolic Disorders (IFSO) Indications for Metabolic and Bariatric Surgery. Obesity surgery. 2022.
Aminian A, Chang J, Brethauer SA, Kim JJ. ASMBS updated position statement on bariatric Surgery in class I obesity (BMI 30–35 kg/m(2)). Surgery for obesity and related Diseases: official journal of the American Society for Bariatric Surgery. 2018;14(8):1071–87.
Varban OA, Bonham AJ, Finks JF, Telem DA, Obeid NR, Ghaferi AA. Is it worth it? Determining the health benefits of sleeve gastrectomy in patients with a body mass index < 35 kg/m(2). Surg Obes Relat Diseases: Official J Am Soc Bariatr Surg. 2020;16(2):248–53.
Studer AS, Magdy M, Bacon SL, Denis R, Pescarus R, Garneau PY, et al. Five-year outcomes after Surgery for class 1 obesity: a retrospective analysis of a Canadian bariatric centre’s experience. Can J Surg J canadien de chirurgie. 2022;65(6):E763–e9.
Zhou X, Ke Z, Sun F, Li F, You Z, Zhang J, et al. Effect of bariatric Surgery on metabolic syndrome in Chinese patients with low body Mass Index: a propensity score matching study. Obes Surg. 2023;33(10):3051–61.
Kermansaravi M, Shahmiri SS, Khalaj A, Jalali SM, Amini M, Alamdari NM, et al. The First web-based Iranian national obesity and metabolic Surgery database (INOSD). Obes Surg. 2022;32(6):2083–6.
Hatami M, Pazouki A, Kabir A. Excessive weight loss after bariatric Surgery: a prediction model retrospective cohort study. Updates Surg. 2022;74(4):1399–411.
Brethauer SA, Kim J, El Chaar M, Papasavas P, Eisenberg D, Rogers A, et al. Standardized outcomes reporting in metabolic and bariatric Surgery. Obes Surg. 2015;25(4):587–606.
Gastrointestinal surgery for severe obesity. Consensus statement National Institutes of Health Consensus Development Conference. 1991;9(1):1–20.
Busetto L, Dixon J, De Luca M, Shikora S, Pories W, Angrisani L. Bariatric Surgery in class I obesity: a position Statement from the International Federation for the Surgery of obesity and metabolic disorders (IFSO). Obes Surg. 2014;24(4):487–519.
Shahmiri SS, Parmar C, Yang W, Lainas P, Pouwels S, DavarpanahJazi AH, et al. Bariatric and metabolic Surgery in patients with low body mass index: an online survey of 543 bariatric and metabolic surgeons. BMC Surg. 2023;23(1):272.
Maiz C, Alvarado J, Quezada N, Salinas J, Funke R, Boza C. Bariatric Surgery in 1119 patients with preoperative body mass index < 35 (kg/m(2)): results at 1 year. Surg Obes Relat Diseases: Official J Am Soc Bariatr Surg. 2015;11(5):1127–32.
Kular KS, Manchanda N, Cheema GK. Seven years of mini-gastric bypass in type II Diabetes patients with a body Mass Index < 35 kg/m(2). Obes Surg. 2016;26(7):1457–62.
Hong JS, Kim WW, Han SM. Five-year results of laparoscopic sleeve gastrectomy in Korean patients with lower body mass index (30–35 kg/m²). Obes Surg. 2015;25(5):824–9.
Cevallos L, Rodríguez FM, Herrera A, Sepúlveda EM, Donatini G, Guilbert L, et al. Metabolic Surgery and class 1 obesity (< 35 kg/m(2)): a prospective study with Short-, Mid-, and long-term results among latinos. Obes Surg. 2021;31(6):2401–9.
Gamme G, Dang JT, Switzer N, Gill R, Birch DW, Karmali S. Evaluating the safety of bariatric Surgery for weight loss in class I obesity: a propensity-matched analysis of north American data. Surg Obes Relat Diseases: Official J Am Soc Bariatr Surg. 2019;15(4):629–35.
Cohen R, Caravatto PP, Petry T. Metabolic Surgery for type 2 Diabetes in patients with a BMI of < 35 kg/m(2): a surgeon’s perspective. Obes Surg. 2013;23(6):809–18.
Bhandari M, Mathur W, Kumar R, Mishra A, Bhandari M. Surgical and Advanced Medical Therapy for the treatment of type 2 Diabetes in Class I obese patients: a short-term outcome. Obes Surg. 2017;27(12):3267–72.
Hsu CC, Almulaifi A, Chen JC, Ser KH, Chen SC, Hsu KC, et al. Effect of bariatric Surgery vs Medical Treatment on type 2 Diabetes in patients with body Mass Index Lower Than 35: five-year outcomes. JAMA Surg. 2015;150(12):1117–24.
Berry MA, Urrutia L, Lamoza P, Molina A, Luna E, Parra F, et al. Sleeve gastrectomy outcomes in patients with BMI between 30 and 35 – 3 years of Follow-Up. Obes Surg. 2018;28(3):649–55.
Baldwin D, Sanchez-Johnsen L, Bustos R, Mangano A, Masrur M. Metabolic Surgery outcomes in U.S. patients with Class I obesity. Bariatr Surg Pract Patient care. 2021;16(2):85–91.
Ahluwalia JS, Chang PC, Tai CM, Tsai CC, Sun PL, Huang CK. Comparative study between laparoscopic adjustable gastric banded plication and sleeve gastrectomy in moderate Obesity–2 year results. Obes Surg. 2016;26(3):552–7.
Angrisani L, Favretti F, Furbetta F, Iuppa A, Doldi SB, Paganelli M, et al. Italian Group for Lap-Band System: results of multicenter study on patients with BMI < or = 35 kg/m2. Obes Surg. 2004;14(3):415–8.
Ismail M, Nagaraj D, Rajagopal M, Ansari H, Nair M, Hegde A, et al. Seven-year outcomes of laproscopic sleeve gastectomy in Indian patients with different classes of obesity. Obes Surg. 2019;29(1):191–6.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
M.K. and R.V., M.S. and Sh.Sh. wrote the manuscript and analyzed the data. M.S. and R.V. performed statistical analysis. M.K., Sh.Sh., M.S., A.M., F.E., and A.P. collected and described the data and figures. M.K., A.P.F.E., and Sh. Sh. performed the surgeries. M.K., Sh. Sh. and F.E. followed up with the patients. M.K. and A.M. designed the study. All authors reviewed and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of the Iran University of Medical Sciences approved the protocol for this study (#IR.IUMS.REC.1400.361). Written informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kermansaravi, M., Valizadeh, R., Shahsavan, M. et al. Metabolic and bariatric surgery in patients with class I obesity; a two-year follow-up. BMC Surg 24, 6 (2024). https://doi.org/10.1186/s12893-023-02295-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-02295-x