Abstract
Background
Synchronous multiple early gastric cancer (SMEGC) refers to the simultaneous occurrence of two or more malignant cancer lesions in the stomach. For patients with multiple early gastric carcinomas, the choice of appropriate treatment remains controversial. This study is dedicated to comparing the clinical outcomes and prognosis of patients with SMEGC who underwent endoscopic submucosal dissection (ESD) or gastrectomy.
Methods
A total of 180 patients with more than one malignant cancer lesion in the stomach who had received gastrectomy or ESD between 2012 and 2021 were retrospectively evaluated to determine their clinical outcomes and prognosis. Univariate and multivariate logistic regression were utilized to identify risk factors for tumor recurrence.
Results
Over the 57.5 months median follow-up period for the 140 enrolled cases, tumor recurrence occurred in 8 (12%) in the ESD group but only 1 (1%) in the surgery group. Relapse-free survival (RFS) was higher in the surgery group (p = 0.023) in all cases; however, there was no significant difference in Overall survival (OS, p = 0.772). Complications were significantly higher in the surgery group than in the ESD group, but fewer in the radical distal gastrectomy group. Multivariate regression analysis revealed that ESD(p = 0.034), the main lesion size > 2 cm(p = 0.019), and undifferentiated tumor(p = 0.022) were independent risk factors for tumor recurrence.
Conclusions
For the treatment of simultaneous multifocal early gastric cancer, ESD has a good short-term effect and higher quality of life. However, ESD has a higher risk of recurrence than surgery. And we found that the partial gastrectomy appears to be considered as adequate treatment for some SMEGC patients.
Similar content being viewed by others
Introduction
Gastric cancer remains a leading malignant tumor in China. Its incidence rate ranks third among all tumors, and the mortality rate ranks third [1]. Currently, with advances in endoscopic techniques and the popularity of gastric cancer screening, the detection rates of early gastric cancer (the depth of tumor invasion was limited in mucosa and submucosal regardless of lymph node status [2]) and gastric dysplasia has increased in China. When more than one malignant lesion, including high grade dysplasia is found during endoscopy, the patient is diagnosed as having synchronous multiple early gastric cancer (SMEGC) [3]. According to previous literature reports, the incidence rate of multiple gastric early cancer ranges from 6 to 14% in gastric cancer [3,4,5,6]. Previous studies have shown that SMEGC has several characteristics, including occurring in older men, well-differentiated tumors, early-stage tumors, and does not increase the risk of lymph node metastasis [7]. The prognosis of SMEGC is similar to that of early gastric cancer of a single lesion.
Endoscopic submucosal dissection (ESD) as a minimally invasive method with less trauma, fewer complications, and similar therapeutic efficacy, has been widely accepted. According to the Guidelines for endoscopic diagnosis of early gastric cancer, the absolute indications for ESD are greater in number than before [8], and ESD become a major treatment for early gastric cancer without lymph node metastasis. But it is not clear whether multifocal early gastric cancer applies to this standard. Most current studies focus on the comparison of prognosis between multifocal gastric cancer and unifocal gastric cancer under ESD treatment [5, 9].In this research, we aimed to compare the clinical outcomes and prognosis of ESD and gastrectomy in patients with SMEGC in patients, and compare the advantages and disadvantages of the formal anatomic resection versus ESD.
Methods and materials
Patients
Between 2011 and 2021, all patients diagnosed with SMEGC in our hospital were collected. The inclusion criteria included:1) postoperative pathology confirmed 2 or more tumor or dysplasia lesions;2) each lesion must have distinct demarcation from adjacent areas of the microscopically normal gastric wall or transformation zone;3) each is not caused by local extension or metastasis of another lesion [10]; 4) postoperative pathology confirmed that the depth of tumor invasion was limited in mucosa and submucosal regardless of lymph node status; the exclusion criteria included:1) patients with other malignant tumor history; 2) with preoperative chemotherapy;3) pathological or clinical data was not complete.
Definitions
Curative resection was defined as complete resection with negative horizontal and vertical margins, with no nerve or lympho-vascular invasion [11].
In the statistical sequence of lesions in patients was also defined, the lesion with the largest depth of tumor invasion was identified as the main lesion; and if two or more tumor lesions have the same depth of invasion, the largest lesion is considered as the main lesion, the remaining tumor lesions regarded as the minor lesions [12]. The maximum diameter of tumor was measured by the postoperative specimen.
Synchronous recurrence was defined as a newly developed adenocarcinoma or high-grade dysplasia within 12 months after curative resection, while metachronous recurrence was defined as a newly developed adenocarcinoma or high-grade dysplasia which had developed more than 12 months after curative resection. Our hospital provides eradication therapy for all patients diagnosed with H. pylori infection upon discharge.
Data collection
All clinical data, including demographics, pathological results, gastrectomy types and postoperative complications, were collected from the clinical database.
Statistical analysis
SPSS version 26.0 statistical software was used for statistical analysis. All continuous variables were described as mean ± standard deviation (SD) or median (interquartile range, IQR), and compared by student’s test or Mann-Whitney U test. All categorical variables were described as frequency (percentage), and the chi-square test or Fisher’s exact test was used to analyze categorical variables when applicable. The prognostic overall survival (OS) and relapse-free survival (RFS) were conducted by the Kaplan-Meier method. P-value less than 0.05 was considered statistically significant.
Results
Clinical baseline characteristics
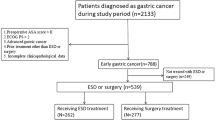
A total of 180 patients who underwent gastrectomy or ESD therapy were included in our research,101 patients were in the ESD group and 79 patients were in the surgery group. Among them, due to the exclusion of patients with neuroendocrine neoplasm, gastrointestinal stromal tumors, and hyperplastic polyp, we were left with 87 patients in ESD group and 73 patients in surgery group, as shown in Fig. 1. After excluding patients who underwent non-curative resection, we were left with 140 patients, including the gastrectomy groups (n = 73) and the ESD group (n = 67). There were 309 independent lesions, 17 patients had 3 independent lesions, 6 patients had 4 independent lesions in the stomach, and the remaining patients had 2 independent lesions. The size of the main and minor lesions had an important positive correlation (r = 0.5024, P < 0.0001), as the size of the minor lesion increased with the increase of the main lesion (Fig. 2).
The baseline characteristics of the 140 patients are listed in Table 1. The size of the minor lesion showed that lesion larger than 2 cm was more frequent in the surgery group than in the ESD (26%vs12% P = 0.035) group. There was no significant difference in the mean age and underlying diseases. In the pathologic findings of main and minor lesions, poorly differentiated adenocarcinoma was more common in the surgery group (25%vs6%, P < 0.001;21%vs6%, P < 0.001 respectfully). Ulcerated lesions were more frequent in the surgery group than in the ESD group (38%vs8%, P < 0.001) as was the invasion of the submucosa (13%vs33%, P = 0.007).
Clinical prognostic outcomes
According to the Guidelines for endoscopic diagnosis of early gastric cancer [8], patients undergoing endoscopic resection are divided into two groups: absolute indications and relative indications. There were 61 patients in the absolute indications group, 4 of whom had a non-curative resection; of these 4 patients, 1 patient received additional radical gastrectomy immediately after ESD, 1 patient was found to have differentiated adenocarcinoma 15 months after ESD and received surgical treatment, 1 patient received additional ESD during postoperative review, and no tumor recurrence occurred in the last patient during long-term endoscopic follow-up. In relative indications group, without a curative resection, 12 of whom underwent a later gastrectomy while the other 4 patients were managed by long-term endoscopic follow-up without tumor recurrence.
All the patients in the surgery group underwent curative resections, and only 1 case had tumor recurrence after surgery and died. But there were 11 cases of complications, including 2 bowel obstructions,1 anastomotic leak, and 8 developed malnutrition after gastrectomy. All 8 malnourished patients had undergone total gastrectomy, including 1 death. In the group of 67 cases undergoing an ESD for curative resection, additional radical gastrectomy and ESD were performed in 4 and 8 of these cases, respectively. Among them, tumor recurrence was confirmed in 8 cases by postoperative pathology. According to the time of recurrence, synchronous recurrences arose in 4 patients, and metachronous recurrences were detected in 4 other patients. Only 1 patient had a complication, serious intraoperative haemorrhage, which required a blood transfusion. The median follow-up time among 8 patients with recurrences was 43 months (ranging from 9 to 70 months). Relapse-free survival (RFS) was higher in the surgery group (p = 0.023, Fig. 3) in all patients, but there was no important difference in Overall survival (OS)(p = 0.772). Subsequently, we discovered that there was no statistical significance in overall survival (OS) between the partial gastrectomy group and the total gastrectomy group in the surgical cohort (p = 0.218, Fig. 4).
Univariate and multivariate analysis
First, we performed a logistic regression to reveal risk factors for tumor recurrence between patients in surgery and ESD for curative resection groups. Univariate analysis identified the ESD group(p = 0.034), and the main lesion size > 2 cm(p = 0.019) with statistically significant for the risk of tumor recurrence. Then we included factors with P < 0.1 from univariate analysis into multivariate analysis, similarly, ESD group(p = 0.017), and the main lesion size > 2 cm(p = 0.011) were statistical significance (Table 2). Since only 1 patient in the surgery group had metastasis and died, we further explored the risk factors of tumor recurrence in the ESD for curative resection group by performing a logistic regression. In univariate analysis, main lesion size > 2 cm(p = 0.016), and minor undifferentiated lesion(p = 0.027) were statistically significant (Table 3). Multivariate analysis suggests that the important risk factor for tumor recurrence was the main undifferentiated lesion(p = 0.022).
Discussion
In recent years, the diagnostic rate of early gastric cancer and gastric dysplasia has increased in China [1], due to the advances in endoscopic techniques and the popularity of gastric cancer screening. With these improvements in diagnosis, endoscopic treatment of early gastric neoplastic lesions without lymphovascular invasion has become more widespread. It is precisely because ESD preserves most of the stomach that the incidence of metachronous tumors after ESD is higher than that after gastrectomy [13], because of the propensity of the mucosa to develop multiple areas of potential dysplasia in selected patients. This is especially true for patients with multiple early gastric carcinomas in whom the appropriate treatment remains controversial. In our study, we compared the clinical prognostic outcomes between the surgery group and ESD for curative resection group. Our results revealed that the surgery group had a better RFS outcome than ESD for curative resection group. As expected, the complications in the surgery group were much higher than in the ESD for curative resection group(Table 4). We also found that the complications in partial gastrectomy group were decreased compared to those who underwent total gastrectomy. Notably, our univariate and multivariate analysis demonstrated that the main lesion size > 2 cm, and undifferentiated tumor were independent risk factors for tumor recurrence. Special attention should be given to this group of patients, such as regular endoscopy. After careful consideration, either radical distal gastrectomy or function-preserving gastrectomy may be considered as appropriate treatments.
According to previous studies, older age, male sex, well-differentiated tumors, a family history of gastric cancer, smoking, and drinking were important risk factors for multifocal gastric cancer [14, 15]. Nitta et al. reported that age ≥ 65 years and severe intestinal metaplasia of surrounding mucosa were important independent risk factors for multifocal gastric cancer by multivariate analysis [3]. Our findings are similar to prior research, most (79%,111/140) of patients in groups were male, and 62% (87/140) of the patients were with age ≥ 65 years. The main lesion in 81(58%) patients were diagnosed with well-differentiated gastric cancer, and 28(20%) patients were diagnosed with dysplasia. One of the possible reasons is that most of the patients were early gastric carcinoma in this study. Hereditary diffuse gastric cancer (HDGC) is a dominantly inherited cancer syndrome characterized by a high incidence of diffuse gastric cancer [16]. Several studies have shown that HDGC is closely related to the germline pathogenic variation of E-cadherin gene (CDH1) [17, 18]. At present, CDH1 variant carriers diagnosed with HDGC should be advised to undergo prophylactic total gastrectomy [19, 20]. However, data on whether our patients had a CDH1 mutation are not available because we were not able to evaluate them for this mutation; we understand that this is a limitation of our retrospective study lacking data in the CDH1 mutation. More recently we have become more aware of this possibility and are evaluating certain patients for this mutation, especially those with family members who have had gastric cancer.
Next, we compared the clinical outcomes and prognosis between ESD and gastrectomy in patients with multifocal gastric neoplasms and found that there existed no significant difference in OS. Additionally, the postoperative adverse events were significantly less in the ESD group than in the gastrectomy group. However, during the follow-up period, we found that the recurrence rates were higher in the ESD group, which is similar to the latest study by Xu et al. [9]. One probable explanation is that recurrence was detected during the patients’ postoperative gastroscopy, and timely surgical resection after diagnosis was performed [21].As shown in Fig. 1, additional radical gastrectomy and ESD was performed in 4 and 8 of the patients with curative resection, respectively. For patients with multifocal early gastric cancer, identifying important risk factors is urgently needed to reduce tumor recurrence rate.
Herein, our research investigated the risk factor for carcinoma recurrence between patients in gastrectomy and ESD for curative resection groups and we found that ESD and the size of main lesion > 2 cm are closely associated with higher risk of carcinoma recurrence. To further elucidate the causes of recurrence in patients undergoing ESD for curative resection, our study subsequently compared recurrent and non-recurrent patients in ESD for curative resection group. We found that the undifferentiated type of the main lesion will significantly increase the risk of carcinoma recurrence, which is consistent with our traditional views [22].
In regard to the location of main lesions, Chen et al. and Kim et al. reported that the location of the main lesion is mostly in the lower third [23,24,25]. Our data show that the location of the main lesion is mostly in the lower third, while the middle third has the least, which is consistent with previous study. In contrast, Nitta and colleagues reported that the middle third had 50 cases(54%), but their study still proved that more than half of the patients’ tumor location were located in the lower two-thirds of the stomach [3].
At present, the treatment of multifocal gastric cancer is similar to that of single gastric lesions, and still remains controversial. Kasuga et al. and Joh et al. reported that ESD is a feasible and effective option for the treatment of synchronous early gastric carcinoma [5, 26]. However, previous studies have shown that with ESD in the treatment of multifocal gastric cancer, there will be a high recurrence rate of tumors, as well as minor lesions missed with endoscopy [9, 27]. Therefore, Morgagni et al. found that subtotal gastrectomy could be considered a sufficient treatment when gastroscopy determines that the lesions of multifocal gastric cancer are limited to the lower third [25]. Within our study, there were 43 patients with total gastrectomy in the surgery group, and 10 patients had serious complications after surgery, while only 1 patient (1/30) had serious complications when underwent distal partial gastrectomy. In recent years, a number of studies have shown that distal gastrectomy has fewer complications compared to total gastrectomy [28, 29]. Notably, there was no significant difference in the survival rates of patients between the two groups, which is consistent with a previous study by Mocan et al. [29]. Therefore, we found that patients with distal partial gastrectomy have a better prognosis and no recurrence of the tumor. For multifocal gastric cancer patients with high risk factors for tumor recurrence, distal partial gastrectomy can be considered as adequate treatment.
We acknowledge that our study has certain limitations. First, this research was a retrospective study, which means that selection bias cannot be completely avoided. Second, we lack of genetic evaluation for e-cadherin positivity due to the limitation of the retrospective study. Thirdly, it is a single-center study with a limited sample size. Therefore, multicenter studies with larger sample sizes are required to confirm our findings.
Conclusion
In conclusion, while the OS of ESD is comparable to surgery for curative treatment of SMEGC, ESD has a higher incidence of tumor recurrence compared to gastrectomy. Patients with SMEGC who have a main tumor size ≥ 2 cm and undifferentiated type are at higher risk of recurrence and require more attention. Regular endoscopic monitoring of patients with these characteristics is necessary. Additionally, we found no significant difference in OS between partial and total gastrectomy in the surgical cohort. Therefore, for SMEGC patients with high risk factors for tumor recurrence and limited lesions in the lower third, partial gastrectomy may be considered as adequate treatment.
Data Availability
The raw data in this study can be obtained from the corresponding author on reasonable request by email(mastctl@163.com).
Abbreviations
- SMEGC:
-
Synchronous multiple early gastric cancer
- ESD:
-
Endoscopic submucosal dissection
- RFS:
-
Relapse-free survival
- OS:
-
Overall survival
- HDGC:
-
Hereditary diffuse gastric cancer
References
Cao W, Chen HD, Yu YW, Li N, Chen WQ. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020. Chin Med J (Engl). 2021;134(7):783–91.
Saragoni L, Morgagni P, Gardini A, Marfisi C, Vittimberga G, Garcea D, et al. Early gastric cancer: diagnosis, staging, and clinical impact. Evaluation of 530 patients. New elements for an updated definition and classification. Gastric Cancer. 2013;16(4):549–54.
Nitta T, Egashira Y, Akutagawa H, Edagawa G, Kurisu Y, Nomura E, et al. Study of clinicopathological factors associated with the occurrence of synchronous multiple gastric carcinomas. Gastric Cancer. 2009;12(1):23–30.
Shi Q, Sun D, Cai SL, Xu MD, Qi ZP, Li B, et al. Clinical analysis of endoscopic submucosal dissection for the synchronous multiple primary early cancers in Esophagus and stomach: 12 cases Report. J Laparoendosc Adv Surg Tech A. 2018;28(9):1068–73.
Joh DH, Park CH, Jung S, Choi SH, Kim HK, Lee H, et al. Safety and feasibility of simultaneous endoscopic submucosal dissection for multiple gastric neoplasias. Surg Endosc. 2015;29(12):3690–7.
Lim JH, Kim SG, Choi J, Im JP, Kim JS, Jung HC. Risk factors for synchronous or metachronous tumor development after endoscopic resection of gastric neoplasms. Gastric Cancer. 2015;18(4):817–23.
Kim HM, Kim HK, Lee SK, Cho JH, Pak KH, Hyung WJ, et al. Multifocality in early gastric cancer does not increase the risk of lymph node metastasis in a single-center study. Ann Surg Oncol. 2012;19(4):1251–6.
Yao K, Uedo N, Kamada T, Hirasawa T, Nagahama T, Yoshinaga S, et al. Guidelines for endoscopic diagnosis of early gastric cancer. Dig Endosc. 2020;32(5):663–98.
Xu S, Chai N, Tang X, Linghu E, Lu Z, Wang S, et al. Outcomes of simultaneous endoscopic submucosal dissection for synchronous multiple gastric neoplastic lesions: a retrospective comparative study. Surg Endosc. 2022;36(6):4014–24.
Moertel CG, Bargen JA, Soule EH. Multiple gastric cancers; review of the literature and study of 42 cases. Gastroenterology. 1957;32(6):1095–103.
Japanese Gastric Cancer Treatment Guidelines. 2021 (6th edition). Gastric Cancer. 2023;26(1):1–25.
Japanese classification of gastric carcinoma. 3rd English edition. Gastric Cancer. 2011;14(2):101–12.
Kinami S, Aizawa M, Yamashita H, Kumagai K, Kamiya S, Toda M, et al. The incidences of metachronous multiple gastric cancer after various types of gastrectomy: analysis of data from a nationwide japanese survey. Gastric Cancer. 2021;24(1):22–30.
Eom BW, Lee JH, Choi IJ, Kook MC, Nam BH, Ryu KW, et al. Pretreatment risk factors for multiple gastric cancer and missed lesions. J Surg Oncol. 2012;105(8):813–7.
Isobe T, Hashimoto K, Kizaki J, Murakami N, Aoyagi K, Koufuji K, et al. Characteristics and prognosis of synchronous multiple early gastric cancer. World J Gastroenterol. 2013;19(41):7154–9.
Blair VR, McLeod M, Carneiro F, Coit DG, D’Addario JL, van Dieren JM, et al. Hereditary diffuse gastric cancer: updated clinical practice guidelines. Lancet Oncol. 2020;21(8):e386–e97.
Hansford S, Kaurah P, Li-Chang H, Woo M, Senz J, Pinheiro H, et al. Hereditary diffuse gastric Cancer syndrome: CDH1 mutations and Beyond. JAMA Oncol. 2015;1(1):23–32.
Liu ZX, Zhang XL, Zhao Q, Chen Y, Sheng H, He CY, et al. Whole-exome sequencing among chinese patients with Hereditary diffuse gastric Cancer. JAMA Netw Open. 2022;5(12):e2245836.
Fitzgerald RC, Hardwick R, Huntsman D, Carneiro F, Guilford P, Blair V, et al. Hereditary diffuse gastric cancer: updated consensus guidelines for clinical management and directions for future research. J Med Genet. 2010;47(7):436–44.
Decourtye-Espiard L, Guilford P. Hereditary diffuse gastric Cancer. Gastroenterology. 2023;164(5):719–35.
Nakajima T, Oda I, Gotoda T, Hamanaka H, Eguchi T, Yokoi C, et al. Metachronous gastric cancers after endoscopic resection: how effective is annual endoscopic surveillance? Gastric Cancer. 2006;9(2):93–8.
Seo JH, Park JC, Kim YJ, Shin SK, Lee YC, Lee SK. Undifferentiated histology after endoscopic resection may predict synchronous and metachronous occurrence of early gastric cancer. Digestion. 2010;81(1):35–42.
Chen L, Yue C, Li G, Ming X, Gu R, Wen X, et al. Clinicopathological features and risk factors analysis of lymph node metastasis and long-term prognosis in patients with synchronous multiple gastric cancer. World J Surg Oncol. 2021;19(1):20.
Kim JH, Jeong SH, Yeo J, Lee WK, Chung DH, Kim KO, et al. Clinicopathologic similarities of the main and minor lesions of synchronous multiple early gastric Cancer. J Korean Med Sci. 2016;31(6):873–8.
Morgagni P, Marfisi C, Gardini A, Marrelli D, Saragoni L, Roviello F, et al. Subtotal gastrectomy as treatment for distal multifocal early gastric cancer. J Gastrointest Surg. 2009;13(12):2239–44.
Kasuga A, Yamamoto Y, Fujisaki J, Okada K, Omae M, Ishiyama A, et al. Simultaneous endoscopic submucosal dissection for synchronous double early gastric cancer. Gastric Cancer. 2013;16(4):555–62.
Lee HL, Eun CS, Lee OY, Han DS, Yoon BC, Choi HS, et al. When do we miss synchronous gastric neoplasms with endoscopy? Gastrointest Endosc. 2010;71(7):1159–65.
Kim DJ, Lee JH, Kim W. Comparison of the major postoperative complications between laparoscopic distal and total gastrectomies for gastric cancer using clavien-dindo classification. Surg Endosc. 2015;29(11):3196–204.
Mocan L, Tomus C, Bartos D, Zaharie F, Ioana I, Bartos A, et al. Long term outcome following surgical treatment for distal gastric cancer. J Gastrointestin Liver Dis. 2013;22(1):53–8.
Acknowledgements
The authors gratefully acknowledge all the investigators for their contributions to the trial.
Funding
None.
Author information
Authors and Affiliations
Contributions
LB, LT, MF, and MW contributed to the study design. LB, LP, CS, KJ, and HG, contributed to the data collection. LT analyzed data and LB wrote the manuscript. All authors read and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Nanjing Drum Tower Hospital, the Affiliated Hospital of Nanjing University Medical School(N0.2022-742-01), Nanjing, China. The entire process of this study followed the ethical standards of Declaration of Helsinki and its later amendments. The requirement for written informed consent was waived by Ethics Committee of Nanjing Drum Tower Hospital because of the retrospective nature of the study.
Consent for publication
None.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bao, L., Gao, H., Pu, L. et al. Comparison of clinical outcomes and prognosis between surgery and endoscopic submucosal dissection in patients with synchronous multifocal early gastric cancer. BMC Surg 23, 292 (2023). https://doi.org/10.1186/s12893-023-02194-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-02194-1