Abstract
Purpose
The treatment strategies for acute appendicitis differ depending on the facility, and various studies have investigated the usefulness of conservative treatment with antibiotics, laparoscopic surgery, and interval appendectomy (IA). However, although laparoscopic surgery is widely used, the clinical strategy for acute appendicitis, especially complicated cases, remains controversial. We assessed a laparoscopic surgery-based treatment strategy for all patients diagnosed with appendicitis, including those with complicated appendicitis (CA).
Methods
We retrospectively analysed patients with acute appendicitis treated in our institution between January 2013 and December 2021. Patients were classified into uncomplicated appendicitis (UA) and CA groups based on computed tomography (CT) findings on the first visit, and the treatment course was subsequently compared.
Results
Of 305 participants, 218 were diagnosed with UA and 87 with CA, with surgery performed in 159 cases. Laparoscopic surgery was attempted in 153 cases and had a completion rate of 94.8% (145/153). All open laparotomy transition cases (n = 8) were emergency CA surgery cases. No significant differences were found in the incidence of postoperative complications in successful emergency laparoscopic surgeries. In univariate and multivariate analyses for the conversion to open laparotomy in CA, only the number of days from onset to surgery ≥ 6 days was an independent risk factor (odds ratio: 11.80; P < 0.01).
Conclusion
Laparoscopic surgery is preferred in all appendicitis cases, including CA. Since laparoscopic surgery is difficult for CA when several days from the onset have passed, it is necessary that surgeons make an early decision on whether to operate.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Acute appendicitis is one of the most common surgical conditions. However, the clinical presentation of appendicitis varies depending on the degree of inflammation and the patient’s background [1,2,3]. Recently, many reports have classified acute appendicitis as uncomplicated appendicitis (UA) and complicated appendicitis (CA). (1) CA is often defined as a gangrenous appendix, perforated appendix, or peri-appendiceal abscess [2, 3]. Traditionally, emergency surgery has been the gold standard for the treatment of acute appendicitis. However, because of the widespread use of laparoscopic surgery or conservative treatment options with antibiotics, treatment strategies have been diversifying and differ depending on the institution. Several studies have reported that conservative treatment with antibiotics may successfully treat most UA cases [4,5,6]. Furthermore, recent research has demonstrated that CA could also be treated with antibiotics [7, 8]. The efficacy of laparoscopic surgery or interval appendectomy (IA) after conservative treatment has also been proved in the past decades [8, 9]. Although consensus has not been reached, several reports have verified the usefulness of laparoscopic surgery for CA cases. Therefore, we assessed a laparoscopic surgery-based treatment strategy for all patients diagnosed with appendicitis, including those with CA.
Material and methods
Study population
We retrospectively evaluated medical records of all patients diagnosed with acute appendicitis in our institution between January 2013 and December 2021. We excluded patients who did not have sufficient data.
Diagnosis
Diagnosis of appendicitis is comprehensively determined by clinical findings, blood sampling data, and imaging (computed tomography or ultrasonography). Further, several experienced surgeons re-evaluated the diagnosis.
Therapeutic strategy
Patients with suspected having with appendicitis initially underwent blood test and computed tomography (CT) (and ultrasonography). Antibiotics was administered as soon as the diagnosis was made. Emergency surgery was indicated for patients with peritoneal irritation sign, severe tenderness or sepsis at the first visit. We comprehensively consider not only patients’ imaging but also the symptoms and general conditions to determine whether or not emergency surgery is needed. Further, we performed emergency surgery for patients who deteriorated on study within 24 h after admission. Patients with mild symptoms were treated conservatively with fasting and antibiotics. Furthermore, they were recommended to undergo appendectomy on standby as an IA after more than a month.
Surgical procedures
Laparoscopic appendectomy was typically performed in patients who were eligible for surgery, while open laparotomy was carried out in cases with possible tumours or extensive abscesses. We performed laparoscopic surgery with three ports, with an additional port added depending on intraoperative findings. Furthermore, we occasionally performed single-incision laparoscopic surgery as a part of the IA procedure. Appendiceal mesentery was resected using ultrasonic coagulating sears, and appendix was ligated by Endloop (Ethicon, Johnson and Johnson, Arlington, TX, USA). For cases in which the amount of intraoperative bleeding was very small or uncountable, the amount of bleeding was set to 5 ml for the convenience of analysis.
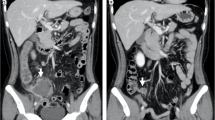
Computed tomography assessment
Abdominal computed tomography (CT) was performed at the time of appendicitis diagnosis, and the images were evaluated by three or more experienced gastrointestinal surgeons. In this study, the images were reassessed retrospectively and classified into two categories (uncomplicated and complicated appendicitis) according to the previous literature. The CA group included gangrenous and perforated appendicitis. CT findings suggestive of CA included extraluminal appendicoliths, abscesses, appendiceal wall enhancement defects, and extraluminal defects [2, 3, 10].
Histopathological findings
Pathological findings were evaluated by a board-certified pathologist and classified into four types based on the degree of inflammation: catarrhalis, phlegmonous, gangrenous, and chronic appendicitis.
Statistical analysis
Continuous values are presented as medians. Between-group differences in qualitative and quantitative variables were analysed using two-tailed Fisher’s exact test, Pearson's chi-squared test, and Wilcoxon rank-sum test. Multiple logistic regression analysis of the factors contributing to the conversion of laparoscopic surgery to open laparotomy was performed. A P value of < 0.05 was considered statistically significant. Variables with a P value of < 0.05 according to a univariate analysis were included in the multivariate analysis. Each cut-off value was calculated using the Receiving Operating Characteristic curve. Propensity score matching was performed to adjust for patients’ background: age, sex, underlying diseases, and body mass index (BMI). All analyses were performed using JMP statistical software version 14.1.0 (SAS Institute Inc., Cary, NC, USA).
Results
We assessed 308 patients who were diagnosed with acute appendicitis. Of these, 305 were analysed and three were ineligible because they had a final diagnosis of appendiceal mucinous adenoma or adenocarcinoma in the postoperative pathological findings. The median age of the patients was 37.4 years, and the number of male and female patients was 167 and 138, respectively. Surgery was performed in 159 patients, with laparoscopic surgery attempted on 153 patients, and an open laparotomy transition was required in eight of those cases. Thus, the completion rate of the laparoscopic surgery was 94.8% (145/153). Six of the 159 surgical cases indicated for open surgery because of extensive abscess formations, some were also suspected of tumours preoperatively. The baseline characteristics of the patients are presented in Supplementary Table 1 (Online Resource 1).
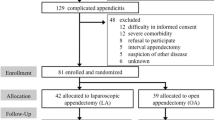
A total of 305 cases were classified into 218 UA and 87 CA cases based on CT findings at the time of the diagnosis (Table 1). Patients with CA were significantly older (P < 0.001) and had an increased likelihood of associated comorbidities (P = 0.01). In the preoperative laboratory data, the white blood cell count, neutrophil rate and count, and C-reactive protein level were significantly higher in the CA group. The UA cases included 38.5% (84/218) of patients who underwent surgery, and half of these (42/84) had an IA. All patients with UA (84/ 84) successfully underwent laparoscopic surgery. In the CA patients, surgery was performed in 86.2% (75/87) of cases. Of these, 16 cases were transitions after unsuccessful conservative treatment and three cases underwent IA. All patients who underwent IA (45/45) were successfully treated with laparoscopic surgery (Fig. 1).
In the comparison of emergency surgery groups between UA and CA, all patients in the UA group were treated completely with laparoscopic surgery, whereas in the CA group, 12.5% (8/64) required open laparotomy (P = 0.021). In all eight cases, the cause of the transition to open laparotomy was the presence of severe adhesions. Table 2 shows the comparison of emergency surgery cases successfully treated laparoscopically between UA and CA groups. Significant differences were found in analysis of the operation duration (58.5 vs 86 min, P < 0.001), drain placement rate (33.3 vs 83.9%, P < 0.001), and postoperative days (5 vs 7 days, P = 0.04). There was no significant difference in the incidence of postoperative complications between the groups (P = 1.0). Similar results were obtained when propensity score matching was performed to adjust the patients’ background in Table 2 (Supplementary Table 2; Online Resource 1).
In the comparison of the status between laparoscopically treated and open laparotomy converted cases in the CA group (Supplementary Table 3; Online Resource 1), the number of days from onset to surgery was significantly higher in the open transition group than in the laparoscopy completion group (2 vs 9 days, P < 0.001). CRP level at the first visit also tended to be higher in the open laparotomy transition group than in the laparoscopy completion group (7.0 vs 10.8, P = 0.054). Furthermore, the operative time, blood loss, postoperative complications, and postoperative hospital stay were all significantly higher in the open laparotomy converted group than in the laparoscopy completion group (Supplementary Table 2; Online Resource 1). In the univariate and multivariate analyses of the risk factors for the conversion to open laparotomy in CA, ≥ 6 days from onset to surgery was an independent risk factor (odds ratio 11.80; 95% confidence interval, 1.25–111.33; P < 0.01) (Table 3).
Discussion
In this study, we validated the usefulness of laparoscopic surgery for the treatment of appendicitis and attempted to evaluate the risk factors associated with converting to open laparotomy in CA. Because laparoscopic surgery could reduce postoperative complications and hospital stay, even in patients with CA, it is important to recognise these risk factors.
Treatment strategies for acute appendicitis vary depending on the facility and no definitive consensus exists, especially for CA cases. Some reports suggest that IA after conservative treatment is reasonable for CA, as IA reportedly has fewer postoperative complications and shorter postoperative hospital stays than emergency appendectomy [7]. However, for IA cases, the disadvantages are longer hospital stays and higher medical expenses [8]. Some studies have suggested that IA is unnecessary after the initial antibiotic treatment for CA [11, 12]. This is supported by the relatively low rates (approximately 10%) of appendicitis recurrence after conservative management, as well as high complication rates of the IA procedure [11, 12].
In recent decades, the use of laparoscopic surgery for appendicitis has become widespread. Advantages of laparoscopic surgery include a reduction in overall post-operative morbidity and surgical site infection, shorter postoperative hospital stay, less postoperative pain, and earlier postoperative recovery [13, 14]. Laparoscopic appendectomy has proven to be a safe alternative to open appendectomy in UA [15, 16]. However, the feasibility of laparoscopic surgery for CA has remained controversial. As a result of a meta-analysis, some studies concluded that laparoscopic surgery for CA has reduced surgical site infection rates compared to open surgery, with no difference with regard to intra-abdominal abscess complication rates [14, 17, 18]. The overall conversion rate from laparoscopic appendectomy to open appendectomy was reported to be approximately 10% [19]. To the best of our knowledge, there are no studies that verify the nature of cases that would convert to open laparotomy. In our study, all cases of UA were resolved by laparoscopic surgery, but it was revealed that cases of CA that were treated a few days after the onset of symptoms were more likely to convert to open laparotomy. The number of days from onset to surgery of ≥ 6 days was an independent risk factor for the conversion. The cause of this transition was the existence of strong adhesions in all the cases. It is important for surgeons to confirm the onset time during the patient’s first visit. For patients with CA with good general condition for whom some days from the onset have passed, IA could be a feasible alternative to emergency surgery. Resent multicenter study suggested that in-hospital delay of surgery in patients with CA was associated with a higher risk of a postoperative complication [20]. It is important that surgeons recognize and decide to operate patients with CA early as we suggested.
Several reports have discussed methods of appendectomy in laparoscopic surgery [21,22,23]. Zorzetti N et al. suggested the routine use of endloop for appendectomy even in case with complicated appendicitis because of cost effectivity and lower complications [21, 22]. Bao W et al. reported that purse-string sutures effectively reduced the incidence of postoperative complications after a laparoscopic appendectomy for CA [23]. We usually use endloop, but sometimes use endstapler for cases with necrotic appendicitis. Since there are still few reports on the method of excision, this is a topic for future research.
A recent topic on CA is the necessity of intraoperative peritoneal lavage. Whether intraoperative peritoneal lavage is effective for preventing postoperative intraabdominal abscesses for patients with CA remains controversial. Some study resulted that irrigation of peritoneal cavity during laparoscopic appendectomy could decrease the incidence of postoperative intraabdominal abscesses in patients with CA [24, 25]. Further, these patients also had faster postoperative recovery and lower hospital charges [24]. However, other studies denied the superiority of peritoneal lavage [26, 27]. One of the major problems is that the methods of peritoneal lavage are not standardized. A larg-scale multicenter study is needed.
This study has several limitations. First, it was a retrospective analysis with a small total number of CA cases, and its statistical power was too low for meaningful conclusions to be drawn for the broader application of the findings. Second, over the study period of 8 years, changes in the surgical indications, equipment, techniques, and perioperative management may have caused variations in the results.
Conclusion
In conclusion, laparoscopic surgery is useful in all appendicitis cases, including CA. It is important to promptly decide whether emergency surgery is required in complicated cases. Surgeons should consider open laparotomy or conservative treatment for CA that is evaluated some days from the first onset of symptoms.
Availability of data and materials
All publicly available data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Change history
07 August 2023
A Correction to this paper has been published: https://doi.org/10.1186/s12893-023-02120-5
Abbreviations
- CA:
-
Complicated appendicitis
- CT:
-
Computed tomography
- IA:
-
Interval appendectomy
- UA:
-
uncomplicated appendicitis
References
Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278–87.
Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg. 2015;102:979–90.
Fujiwara K, Abe A, Masatsugu T, Hirano T, Hiraka K, Sada M. Usefulness of several factors and clinical scoring models in preoperative diagnosis of complicated appendicitis. PLoS One. 2021;16(7):e0255253.
Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, et al. Antibiotic Therapy vs Appendectomy for Treatment of Uncomplicated Acute Appendicitis: The APPAC Randomized Clinical Trial. JAMA. 2015;313:2340–8.
Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156.
Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B, et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet. 2011;377:1573–9.
Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246:741–8.
Darwazeh G, Cunningham SC, Kowdley GC. A Systematic Review of Perforated Appendicitis and Phlegmon: Interval Appendectomy or Wait-and-See? Am Surg. 2016;82:11–5.
Kim JY, Kim JW, Park JH, Kim BC, Yoon SN. Early versus late surgical management for complicated appendicitis in adults: a multicenter propensity score matching study. Ann Surg Treat Res. 2019;97:103–11.
Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH. Systematic Review and Meta-Analysis of CT Features for Differentiating Complicated and Uncomplicated Appendicitis. Radiology. 2018;287:104–15.
Willemsen PJ, Hoorntje LE, Eddes EH, Ploeg RJ. The need for interval appendectomy after resolution of an appendiceal mass questioned. Dig Surg. 2002;19:216–20.
Tekin A, Kurtoğlu HC, Can I, Oztan S. Routine interval appendectomy is unnecessary after conservative treatment of appendiceal mass. Colorectal Dis. 2008;10:465–8.
Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16:1929–39.
Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg. 2010;34:2026–40.
Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg. 1998;186:545–53.
Sauerland S, Lefering R, Holthausen U, Neugebauer EA. Laparoscopic vs conventional appendectomy–a meta-analysis of randomised controlled trials. Langenbecks Arch Surg. 1998;383:289–95.
Yu MC, Feng YJ, Wang W, Fan W, Cheng HT, Xu J. Is laparoscopic appendectomy feasible for complicated appendicitis ?A systematic review and meta-analysis. Int J Surg. 2017;40:187–97.
Quah GS, Eslick GD, Cox MR. Laparoscopic appendicectomy is superior to open surgery for complicated appendicitis. Surg Endosc. 2019;33:2072–82.
Li X, Zhang J, Sang L, Zhang W, Chu Z, Li X, et al. Laparoscopic versus conventional appendectomy–a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2019;10:129.
Bolmers MDM, de Jonge J, Bom WJ, van Rossem CC, van Geloven AAW, et al. Snapshot Appendicitis Collaborative Study group. In-hospital Delay of Appendectomy in Acute, Complicated Appendicitis. J Gastrointest Surg. 2022;26:1063–1069.
Zorzetti N, Lauro A, Vaccari S, Ussia A, Brighi M, et al. A systematic review on the cost evaluation of two different laparoscopic surgical techniques among 996 appendectomies from a single center. Updates Surg. 2020;72:1167–74.
Zorzetti N, Lauro A, Bellini MI, Vaccari S, Via BD, et al. Laparoscopic appendectomy, stump closure and endoloops: A meta-analysis. World J Gastrointest Surg. 2022;14:1060–71.
Bao W, Wang J, Tang D, Li L, Meng X. Application and curative effect of laparoscopic purse-string sutures in the treatment of adult acute complicated appendicitis. BMC Surg. 2023;23:1.
Sun F, Wang H, Zhang F, Zhang X, Xing Z, et al. Copious Irrigation Versus Suction Alone During Laparoscopic Appendectomy for Complicated Appendicitis in Adults. J Invest Surg. 2018;31:342–6.
Escolino M, Becmeur F, Saxena A, Till H, Masieri L, et al. Infectious Complications After Laparoscopic Appendectomy in Pediatric Patients with Perforated Appendicitis: Is There a Difference in the Outcome Using Irrigation and Suction Versus Suction Only? Results of a Multicentric International Retrospective Study. J Laparoendosc Adv Surg Tech A. 2018;28:1266–70.
Siotos C, Stergios K, Prasath V, Seal SM, Duncan MD, et al. Irrigation Versus Suction in Laparoscopic Appendectomy for Complicated Appendicitis: A Meta-analysis. J Surg Res. 2019;235:237–43.
Burini G, Cianci MC, Coccetta M, Spizzirri A, Di Saverio S, et al. Aspiration versus peritoneal lavage in appendicitis: a meta-analysis. World J Emerg Surg. 2021;16:44.
Acknowledgements
The authors thank Editage (www.editage.jp) for English language editing.
Code availability
Not applicable.
Funding
No fundings.
Author information
Authors and Affiliations
Contributions
MS designed the study conception, acquired the data and prepared the manuscript. MS also analyzed and interpretated the data. MS YS NM drafted the manuscript. MS, YS, NM, TK, YH, HO, TI reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the research Ethics Committee of Kamifukuoka General Hospital, approval number [20220329]. All procedures involving human participants in this study were in accordance with the ethical standards of the institutional research committee and the 1964 Helsinki Declaration.
The requirement for written informed consent from each patient was waived owing to the retrospective design of the study by the research Ethics Committee of Kamifukuoka General Hospital approval number [20220329].
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplementary Table 1. Patients characteristics. Supplementary Table 2. Comparison of emergent surgery cases successfully treated by laparoscopy between UA and CA after propensity score matching. Supplementary Table 3. Comparison of laparoscopic surgery completion cases and open laparotomy transition cases in emergency CA surgery.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shiihara, M., Sudo, Y., Matsushita, N. et al. Therapeutic strategy for acute appendicitis based on laparoscopic surgery. BMC Surg 23, 161 (2023). https://doi.org/10.1186/s12893-023-02070-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-023-02070-y