Abstract
Background
Hemangiopericytomas (HPCs) are uncommon soft tissue tumors. HPCs that grow in the cranial base are rare. Therefore, skull-base surgeons tend to overlook this disease. This study aimed to increase the awareness of HPCs by summarizing case data from our institution and related publications. We also aimed to contribute to the number of reported cases for future systematic reviews of HPCs.
Methods
This study included all patients who underwent surgery for HPC/solitary fibrous tumor (SFT) between August 2015 and August 2019. All surgeries were performed at Xiangya Hospital Central South University. We analyzed clinical characteristics, surgical highlights, treatment modalities, and outcomes.
Results
We included six patients, aged 32–64 years. Lesions were located in the parapharyngeal space in three patients, pterygopalatine fossa in two, and saddle area in one. All patients underwent nasal endoscopic endonasal surgery. In five patients, tumors involved the internal carotid artery (ICA). The exposure and protection of the ICA during surgery are challenging but critical to complete tumor removal. The 3-year overall survival(OS) rate was 66.7%.
Conclusions
HPC/SFTs are rare tumors of the cranial base that are prone to recurrence. Cranial base HPC/SFTs are often closely associated with the ICA. To our knowledge, this case series reports the largest number of cases of HPCs associated with the ICA. We believe that there is a strong relationship between patient prognosis and whether the tumor encircles the ICA and whether the tumor is completely resected. To confirm this suggestion, more cases are needed for further analysis.
Similar content being viewed by others
Introduction
Hemangiopericytoma (HPC), also known as solitary fibrous tumor(SFT), were first described by Stout and Murray. HPCs may be benign or malignant and originate from the pericytes of the capillary and venous walls [1]. Pathologically, HPCs are characterized by abundant spindle cells and “staghorn” vascular branches. HPCs can occur anywhere in the body, with the most common locations being the trunk, pelvis, and lower extremities. Of all reported cases, 15–25% occurred in the head and neck. Only 5% have been found in the nose or paranasal sinuses [2, 3]. HPCs are found in the cranial base region. Epidemiologically, there is no sex, age, or ethnic predilection for the occurrence of HPCs/SFTs. HPCs/SFTs are clinically characterized by malignancy-like aggressiveness, a tendency to recur, and metastasis risk [4, 5]. Surgery remains the mainstay of treatment. Of note, given the rarity of the diagnosis, it is difficult to assess the impact of radiotherapy or chemotherapy [6]. Due to the paucity of studies on this condition, the factors affecting its prognosis are not clear, but total intraoperative tumor resection is important. Existing publications on cranial base HPCs/SFTs are few and mostly case reports. Hence, only limited assumptions can be made about the tumor.
We collected data on patients with cranial base HPCs/SFTs who received surgical treatment at our institution in the last 4 years. We also summarized the findings from available publications including the clinical features and treatment. These details were combined to complement the small but growing literature on HPCs. We aimed to share our experiences and lessons learned in the treatment of HPCs, which are closely related to the internal carotid artery (ICA). Our insights may be useful to cranial base surgeons for the diagnosis and treatment of this type of tumor.
Materials and methods
We retrospectively reviewed the data of patients who underwent surgical treatment for cranial base tumors from August 2015 to August 2019 and summarized the details, including the results of the pathological examinations. Consent was obtained from the patient or the patient’s family. The study was approved by our institutional ethics department.
Imaging examinations, such as cranial base computed tomography (CT), cranial base enhanced magnetic resonance imaging (MRI), cranial base magnetic resonance angiography (MRA), or cranial base digital subtraction angiography, to show the tumor and its relationship with important anatomical structures were performed for all patients. All endoscopic endonasal surgeries (EES) were performed by Dr. Weihong Jiang at Xiangya Hospital Central South University. Additional clinical information was collected through medical case records and at follow-ups.
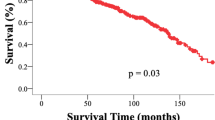
We summarized the key points relating to the exposure and protection of the ICA during tumor resection surgeries by analyzing the surgical videos. We also compared the patient’s preoperative and postoperative cranial base MRI findings to determine whether the tumor had been fully removed. We analyzed the overall survival (OS) rate of these patients using the Kaplan–Meier method in SPSS (version 21.0, SPSS Inc., Chicago, IL, USA).
We also summarized the available publications on cranial base HPCs/SFTs and combined the details with our patient data. Furthermore, we discussed the key points of diagnosis and treatment and analyze the factors affecting prognosis.
Results
Clinical characteristics of included patients
Our study included six patients (three men and three women), aged 32–64 years. Lesions were located in the parapharyngeal space in three patients, pterygopalatine fossa in two, and saddle area in one. The investigated tumor characteristics included the tumor topographical site, pathological type, differentiation status, and pathological stage. Patient characteristics are shown in Table 1.
Treatment and prognosis of included patients
Three patients underwent their first surgery in other hospitals. Patients #1 and #5 underwent multiple surgical procedures. Only one patient received radiotherapy after the last surgery. The specific consultation processes and outcomes are shown in Fig. 1. Patient #3 was found to have a pseudoaneurysm on postoperative MRA. As a result, a balloon embolization of the ICA was performed (Fig. 2).
The average follow-up time was 36 months (range, 16–70 months). At the time of writing, four patients were still alive. The main cause of death was cachexia. The 3-year OS rate was 66.7%. Figure 3 shows patients with preoperative to postoperative imaging comparisons. Patients #3 and #5 had mismatched pre- and postoperative imaging because they were primarily reviewed at other hospitals postoperatively. The images of patients #3 and #5 are shown in Additional file 1: Fig. S1. None of the patients had new neurological deficits after the final surgery.
Visualization and protection of ICA during EES
In five of the six patients in this group, the tumor was closely related to the ICA of the cranial base segment. Patient #2 is used as an example to illustrate the importance of revealing and protecting the ICA in the EES of cranial base HPCs. Figure 4 shows the process of resecting the lesion around the ICA. The resection of the cranial base HPCs was performed in two parts: resection of the lesion and reconstruction of the cranial base structures. Patient #2 had a lesion that encircled the ICA from the paraclival to the parapharyngeal space, so safe resection of the tumor surrounding the ICA was critical to the success of the surgery. Using the pterygoid process(PS) as a landmark to reveal the eustachian tube(ET) and the foramen lacerum(FL). Then resection of the ET while preserving the evator veli palatine can guide the search for an ICA. After removal of the lesion surrounding the ICA (Figure d–f), the adventitia of the ICA is removed, as in Figure g. After the ICA was released from the paraclival to the parapharyngeal space, autologous fat was filled to prevent ICA suspension, and the skull base was repaired with an artificial dura and a pre-prepared lateral nasal wall flap.
Exposure and protection of ICA in endoscopic endonasal surgery. a Reveal the contents of the PF. b, c Removal of the ET and preservation of the EVP. d–g Removal of lesions around ICA, free ICA. h Fill in autologous fat. i Reconstruction of cranial base with LNF. SS, sphenoid sinus; PS: pterygoid process; IA: infraorbital artery; MA: maxillary artery; PF: pterygopalatine fossa; ET: eustachian tube; EVP: evator veli palatine; IPS: inferior petrosal sinus; ICA: internal carotid artery; PD: petrous drum; LNF: lateral nasal flap
Pathology of included patients
The pathology results of the cases in this group all showed hemangiopericytomas (Grade II), and immunohistochemical tests were performed in all cases (Table 2). Among the six included patients, only patient #4 (a young female patient) was treated in the oncology department for postoperative intensity-modulated radiotherapy supplemented with radiotherapy for sensitization, while the rest of the patients did not receive radiotherapy or other combination therapy after surgery.
The pathology results showed hemangiopericytomas (grade II) for all patients. Immunohistochemical tests were performed (Table 2). Only patient #4 (a young female patient) was treated in the oncology department for postoperative intensity-modulated radiotherapy, supplemented with radiotherapy for sensitization. The other patients did not receive radiotherapy or other combination therapy after surgery.
Discussion
HPCs/SFTs account for less than 1% of all vascular tumors [7]. Fewer than 5% occur in the nose or sinuses. HPCs of the skull base are extremely rare. HPCs/SFTs exhibit malignant features and are prone to recurrence and metastasis [4,5,6]. Despite the low incidence of this tumor, the specific nature of the condition makes the diagnosis and treatment of HPCs/SFTs of the cranial base difficult. Previous publications on HPCs were mostly case reports. Our efficacy results were not better than those of previous studies. Therefore, we have summarized our cases and findings from the literature.
Diagnosis of cranial base HPCs/SFTs
The clinical presentation of patients with HPCs/SFTs of the cranial base may vary depending on the specific site of growth. If the main body of the tumor is located in the nasal cavity and grows toward the cranial base, nasal symptoms, such as nasal congestion and epistaxis, tend to be the main clinical manifestations, and the patient may not report any headaches and earaches. If the main body of the tumor is in the anterior skull base, infratemporal fossa, pterygopalatine fossa, or parapharyngeal space, headaches are most common. Corresponding regional neurological dysfunction, such as distorted mouth, hearing loss, and vision loss, and other symptoms may also be evident. From the literature, headache symptoms were predominant (24/41), followed by ocular symptoms (4/41), auditory symptoms (2/41), facial palsy symptoms (2/41), nasal symptoms (8/41), and pituitary abnormalities (1/41) (Fig. 5A) [8,9,10,11,12,13,14,15,16,17,18,19,20]. Patients often undergo ENT-head and neck surgery or neurosurgery for these clinical complaints. HPCs/SFTs rare, and the lesions have nonspecific clinical features. Hence, it is often difficult to define the pathology preoperatively. Imaging is a valuable tool in the diagnosis of HPCs. Moreover, enhanced cranial base CT and MRI are the preferred imaging techniques [11]. Features of HPCs/SFTs include an isolated mass with relatively well-defined irregular or dumbbell-shaped borders, which may have internal signal voids. On CT, the tumor often shows a heterogeneous enhancing signal shadow, with or without bone destruction.
The gold standard for the diagnosis of HPCs/SFTs of the cranial base remains pathological diagnosis [10], and preoperative biopsy is still necessary for those whose lesion main location in the nasal cavity or whose cranial base lesion invade the nasal cavity. The pathological findings of our cases were synthesized, and some pathological features of perivascular cell tumors were summarized in conjunction with literature reports. Under light microscopy, oval and spindle-shaped cells can be seen, with vessels ranging in size from tiny capillary-like slits to larger open channels, and a typical antler-like pattern of vessels is usually seen [11]. In contrast, immunohistochemical findings are helpful in the differential diagnosis of this disease and other tumors such as meningioma; we synthesized the immunohistochemical findings of previous literature on HPCs/SFTs of the cranial base and combined them with our cases and found that the immunohistochemical findings of HPCs/SFTs are usually CD34 (n = 35/45, 77.8%), Vimentin (n = 10/11,90.9%), Bal-2 ( n = 8/9,88.9%), STAT6 (n = 28/29,96.6%), and Ki67 index ranging from 8 to 40%. In contrast, S100 (n = 3/7,42.9%), CD31 (n = 2/9,22.2%), and EMA (n = 0/15) were largely unexpressed [8, 9, 12, 15, 18, 21,22,23,24,25,26,27]. CD34 (+) and EMA (−) can better distinguish HPCs/SFTs from meningiomas that are more similar in histomorphology [15, 28], Fig. 5B shows a typical HE staining picture of HPC.
Treatment of cranial base HPCs/SFTs
HPCs/SFTs have pro-vascular characteristics [29]. The ICA often encircles or becomes invaded by the tumor. Hence, the protection of the ICA during surgical treatment of cranial base lesions is particularly important. For surgical treatment of HPCs/SFTs, it is crucial to achieve total dissection of the ICA as much as possible. However, owing to the specificity of the location of the lesion, surgical excision of the lesion without damaging important vascular and neurological functions requires a high level of anatomical knowledge of the cranial base and technique sensitivity. During the resection of giant HPCs/SFTs at the cranial base, if it is not possible to remove the tumor completely, staged surgery to protect nerve function and avoid damage to important blood vessels should be considered.
HPCs/SFTs are usually aggressive, and the probability of recurrence and distant metastasis is not low. Therefore, postoperative radiotherapy is necessary to prevent tumor recurrence [30]. Although only one patient in the present study received postoperative radiotherapy, the other patients, who did not receive radiotherapy, did not experience recurrence. Based on only a few cases, it is not possible to determine the necessity of postoperative radiotherapy and other comprehensive treatments. Whether postoperative radiotherapy has any effect on improving survival requires further studies with larger cohort analyses.
Visualization and protection of the ICA during EES
In cranial-based HPCs, ICA disclosure and protection are critical to the success of total tumor resection in EES. Many cranial base HPCs are closely related to the ICA of the skull base segment, and the tumor is often adjacent to or encircling the ICA. Patrona et al. reported a case of HPC involving the cavernous carotid artery (CCA) and discussed several skull base tumors involving the cavernous sinus region [17]. Five of our patients had HPCs involving the skull base segment of the ICA, CCA, ruptured segment of the ICA, and horizontal and vertical segments of the ICA. The parapharyngeal space segment was predominant. The need for ICA embolization on the side of the lesion before EES was considered according to the involvement of different ICA segments and the BOT test results.
Postoperative management of cranial base HPCs/SFTs
Due to the specificity of the site and growth pattern of cranial base HPCs/SFTs, the these lesions often grow around important blood vessels or nerves. In five of six patients in this study, the ICA was encircled by the tumor, which greatly increased the difficulty of the surgery and the risk of postoperative intracranial hemorrhage and other accidents. In patient #3, a pseudoaneurysm of the ophthalmic segment of the ICA appeared after surgery. For patients whose imaging shows a close relationship between the tumor and the blood vessels, CTA or MRA should be routinely performed before surgery. Moreover, the above tests should be reviewed after surgery to prevent and exclude the occurrence of aneurysms and other conditions [31]. For patients with lesions located in specific functional areas of the skull base, such as tumors in the saddle area that are closely related to the pituitary gland, preoperative and postoperative pituitary function tests should be performed to monitor pituitary function, so that postoperative symptoms can be detected and treated promptly.
Our goal was to share our experience in the diagnosis and treatment of HPCs, especially the importance of intraoperative visualization and protection of the ICA. We also aimed to contribute to the knowledge of this disease for cranial base surgeons.
Conclusions
HPC/SFTs are rare tumors of the cranial base that are prone to recurrence. Cranial base HPC/SFTs are often closely associated with the ICA. To our knowledge, case series reports the largest number of cases of HPCs associated with the ICA. We believe that there is a strong relationship between patient prognosis and whether t the tumor encircles the ICA and whether the tumor is completely resected. To confirm this suggestion, more cases are needed for further analysis.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- HPCs:
-
Hemangiopericytomas
- SFT:
-
Solitary fibrous tumor
- PS:
-
Pterygoid process
- PF:
-
Pterygopalatine fossa
- SA:
-
Saddle area
- EES:
-
Endoscopic endonasal surgeries
- ICA:
-
Internal carotid artery
- CCA:
-
Cavernous carotid artery
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- MRA:
-
Magnetic resonance angiography
- DSA:
-
Digital subtraction angiography
- PA:
-
Petrous apex
- FL:
-
Foramen lacerum
- CS:
-
Cavernous sinus
- CF:
-
Cranial fossa
- NC:
-
Nasal cavity
- FP:
-
Facial paralysis
- HL:
-
Hearing loss
- ET:
-
Eustachian tube
- MA:
-
Maxillary artery
- IA:
-
Infraorbital artery
- SS:
-
Sphenoid sinus
- EVP:
-
Evator veli palatine
- PD:
-
Petrous drum
- LNF:
-
Lateral nasal flap
- IPS:
-
Inferior petrosal sinus
References
Stout AP, Murray MR. Hemangiopericytoma: a vascular tumor featuring zimmermann’s pericytes. Ann Surg. 1942;116(1):26–33. doi:https://doi.org/10.1097/00000658-194207000-00004
Kuo FY, Lin HC, Eng HL, Huang CC. Sinonasal hemangiopericytoma-like tumor with true pericytic myoid differentiation: a clinicopathologic and immunohistochemical study of five cases. Head Neck. 2005;27(2):124–129. doi:https://doi.org/10.1002/hed.20122
Carew JF, Singh B, Kraus DH. Hemangiopericytoma of the head and neck. Laryngoscope. 1999;109(9):1409–1411. doi:https://doi.org/10.1097/00005537-199909000-00009
Guthrie BL, Ebersold MJ, Scheithauer BW, Shaw EG. Meningeal hemangiopericytoma: histopathological features, treatment, and long-term follow-up of 44 cases. Neurosurgery. 1989;25(4):514–522.
Jääskeläinen J, Servo A, Haltia M, Wahlström T, Valtonen S. Intracranial hemangiopericytoma: radiology, surgery, radiotherapy, and outcome in 21 patients. Surg Neurol. 1985;23(3):227–236. doi:https://doi.org/10.1016/0090-3019(85)90087-4
Spitz FR, Bouvet M, Pisters PW, Pollock RE, Feig BW. Hemangiopericytoma: a 20-year single-institution experience. Ann Surg Oncol. 1998;5(4):350–355. doi:https://doi.org/10.1007/BF02303499
Palacios E, Restrepo S, Mastrogiovanni L, Lorusso GD, Rojas R. Sinonasal hemangiopericytomas: clinicopathologic and imaging findings. Ear Nose Throat J. 2005;84(2):99–102.
Simmonds JC, Rebeiz EE. Surgical resection of sinonasal hemangiopericytoma involving anterior skull base: Case reports and literature review. Am J Otolaryngol. 2017;38(1):87–91. doi:https://doi.org/10.1016/j.amjoto.2016.09.003
Vilendecic M, Grahovac G, Lambasa S, Jelec V, Topic I. Unrecognized hemangiopericytoma of posterior cervical region with intracranial extension. J Craniomaxillofac Surg. 2012;40(2):e51-e53. doi:https://doi.org/10.1016/j.jcms.2011.01.019
Heiser MA, Waldron JS, Tihan T, Parsa AT, Cheung SW. Temporal fossa hemangiopericytoma: a case series. Otol Neurotol. 2009;30(7):985–989. doi:https://doi.org/10.1097/MAO.0b013e3181b76b58
Diensthuber M, Götz F, Länger F, Lenarz T, Lenarz M. Extra- and intracranial dumbbell-shaped hemangiopericytoma. Eur Arch Otorhinolaryngol. 2008;265(4):481–484. doi:https://doi.org/10.1007/s00405-007-0466-y
Tan I, Soo MY, Ng T. Haemangiopericytoma of the trigeminal nerve. Australas Radiol. 2001;45(3):350–353. doi:https://doi.org/10.1046/j.1440-1673.2001.00935.x
Shaia WT, Bojrab DI, Babu S, Pieper DR. Lipomatous hemangiopericytoma of the skull base and parapharyngeal space. Otol Neurotol. 2006;27(4):560–563. doi:https://doi.org/10.1097/01.mao.0000185152.46833.ab
Thiringer JK, Costantino PD, Houston G. Sinonasal hemangiopericytoma: case report and literature review. Skull Base Surg. 1995;5(3):185–190. doi:https://doi.org/10.1055/s-2008-1058934
Sadahira Y, Sugihara K, Manabe T. Iatrogenic implantation of malignant meningioma to the abdominal wall. Virchows Arch. 2001;438(3):316–318. doi:https://doi.org/10.1007/s004280000347
Abdel-Fattah HM, Adams GL, Wick MR. Hemangiopericytoma of the maxillary sinus and skull base. Head Neck. 1990;12(1):77–83. doi:https://doi.org/10.1002/hed.2880120112
Patrona A, Patel KS, Bander ED, et al. Endoscopic endonasal surgery for nonadenomatous, nonmeningeal pathology involving the cavernous sinus. J Neurosurg. 2017;126(3):880–888. doi:https://doi.org/10.3171/2015.8.JNS15275
Sun Q, Zhang C, Chen W, He Y. The molecular mechanisms on glomangiopericytoma invasion. Orphanet J Rare Dis. 2013;8:152. Published 2013 Sep 29. doi:https://doi.org/10.1186/1750-1172-8-152
Leung GK, Lee WC, Nicholls JM. Radiation-induced rhabdomyosarcomatous transformation of a recurrent meningeal haemangiopericytoma. Acta Neurochir (Wien). 2007;149(11):1163–1167. doi:https://doi.org/10.1007/s00701-007-1289-8
Oosthuizen JC, Kennedy S, Timon C. Glomangiopericytoma (sinonasal-type haemangiopericytoma). J Laryngol Otol. 2012;126(10):1069–1072. doi:https://doi.org/10.1017/S0022215112001569
Patel AR, Flores BC, Ban VS, Hatanpaa KJ, Mickey BE, Barnett SL. Intracranial hemangiopericytomas: recurrence, metastasis, and radiotherapy. J Neurol Surg B Skull Base. 2017;78(4):324–30. https://doi.org/10.1055/s-0037-1599073.
Zhang Z, Han Y, Zhang K, Teng L. Investigation of vasculogenic mimicry in intracranial hemangiopericytoma. Mol Med Rep. 2011;4(6):1295–1298. doi:https://doi.org/10.3892/mmr.2011.567
Kiberd MB, Macaulay RJ, Christie SD. Skull base hemangiopericytoma: treatment options. Can J Neurol Sci. 2010;37(1):131–134. doi:https://doi.org/10.1017/s031716710000980x
Heyduck A, Wemmert S, Leuschner I, Schick B. Infantiles Hämangioperizytom der Nasenhaupthöhle [Infantile hemangiopericytoma of the nasal cavity]. HNO. 2018;66(5):396–398. https://doi.org/10.1007/s00106-017-0421-1
Morales Valencia E, Tavares de la Paz LA, Santos Vázquez G, Serrano Padilla AE, Moreno Pizarro E. Combined surgical approach to intracranial and extracranial hemangiopericytoma: case report and literature review. Cureus. 2020;12(3):e7447. https://doi.org/10.7759/cureus.7447 Published 2020 Mar 28.
Laviv Y, Michowitz S, Schwartz M. Neonatal intracranial hemangiopericytoma: a 7-year follow-up. Acta Neurochir (Wien). 2012;154(4):637–638. doi:https://doi.org/10.1007/s00701-011-1272-2
Ito S, Yokoyama J, Yoshimoto H, et al. Usefulness of Choline-PET for the detection of residual hemangiopericytoma in the skull base: comparison with FDG-PET. Head Face Med. 2012;8:3. Published 2012 Feb 7. doi:https://doi.org/10.1186/1746-160X-8-3
Son BC, Lee SW, Kim S, Hong JT, Sung JH, Yang SH. Transzygomatic approach with intraoperative neuromonitoring for resection of middle cranial fossa tumors. J Neurol Surg B Skull Base. 2012;73(1):28–35. doi:https://doi.org/10.1055/s-0032-1304561
Dufour H, Métellus P, Fuentes S, et al. Meningeal hemangiopericytoma: a retrospective study of 21 patients with special review of postoperative external radiotherapy. Neurosurgery. 2001;48(4):756–763. doi:https://doi.org/10.1097/00006123-200104000-00011
Combs SE, Thilmann C, Debus J, Schulz-Ertner D. Precision radiotherapy for hemangiopericytomas of the central nervous system. Cancer. 2005;104(11):2457–2465. doi:https://doi.org/10.1002/cncr.21448
Lampreechakul P, Tirakotai W, Lertbutsayanukul P, Siriwimonmas S, Liengudom A. Pre-operative embolization of intracranial and extracranial tumors: a review of 37 cases. J Med Assoc Thai. 2016;99(Suppl 3):S91–119.
Acknowledgements
Not applicable.
Funding
This Research was funded by the National Natural Science Foundation of China (81770985); Hunan Postdoctoral Program for Innovative Talent (2021RC2017) Natural Science Foundation of Hunan Province (2021JJ41027); The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
WJ, HZ conceived and designed the study. ZP, Ya W, RF, YF, QL and YuW acquired data, search the publications, performed the analysis, prepared the figures and table. ZP wrote the main manuscript. WJ supervised the study. All of the authors reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Xiangya Hospital Research Ethics Committee of Central South University. Informed consents were obtained from all the study participants, which was conducted according to the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Preoperative and postoperative MRI images of thecranial base. (a) Patient #3 (b) Patient #5.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Peng, Z., Wang, Y., Wang, Y. et al. Hemangiopericytoma/solitary fibrous tumor of the cranial base: a case series and literature review. BMC Surg 22, 289 (2022). https://doi.org/10.1186/s12893-022-01718-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-022-01718-5