Abstract
Background
Postoperative early recurrence (ER) is a major obstacle to long-term survival after curative liver resection (LR) in patients with hepatocellular carcinoma (HCC). This study aimed to establish preoperative and postoperative nomograms to predict ER in HCC without macrovascular invasion.
Methods
Patients who underwent curative LR for HCC between January 2012 and December 2016 were divided into training and internal prospective validation cohorts. Nomograms were constructed based on independent risk factors derived from the multivariate logistic regression analyses in the training cohort. The predictive performances of the nomograms were validated using the internal prospective validation cohort.
Results
In total, 698 patients fulfilled the eligibility criteria. Among them, 265 of 482 patients (55.0%) in the training cohort and 120 of 216 (55.6%) patients in the validation cohort developed ER. The preoperative risk factors associated with ER were age, alpha-fetoprotein, tumor diameter, and tumor number, and the postoperative risk factors associated with ER were age, tumor diameter, tumor number, microvascular invasion, and differentiation. The pre- and postoperative nomograms based on these factors showed good accuracy, with concordance indices of 0.712 and 0.850 in the training cohort, respectively, and 0.754 and 0.857 in the validation cohort, respectively. The calibration curves showed optimal agreement between the predictions by the nomograms and actual observations. The area under the receiver operating characteristic curves of the pre- and postoperative nomograms were 0.721 and 0.848 in the training cohort, respectively, and 0.754 and 0.844 in the validation cohort, respectively.
Conclusions
The nomograms constructed in this study showed good performance in predicting ER for HCC without macrovascular invasion before and after surgery. These nomograms would be helpful for doctors when determining treatments and selecting patients for regular surveillance or administration of adjuvant therapies.
Similar content being viewed by others
Background
Hepatocellular carcinoma (HCC) is the sixth most common cancer and the third leading cause of cancer-related death worldwide [1, 2]. Chronic hepatitis virus infection still is the prominent cause of HCC [3]. Hepatitis B virus (HBV) infection is the leading cause of HCC in Eastern Asian countries and most African countries [4]. Hepatitis C virus (HCV) is the leading virus-related cause of HCC in North America, Europe, Japan, parts of central Asia including Mongolia, and northern Africa and the Middle East, particularly Egypt [5]. And co-infection of hepatitis D virus (HDV) with HBV significantly enhances the recurrence risk of HCC patients after live donor liver transplantation (LT) [6]. Nonalcoholic fatty liver disease (NAFLD) is now the most common liver disease and a major risk factor for HCC in most developed countries [7, 8]. Other risk factors of HCC include alcohol abuse, exposure to dietary toxins such as aflatoxins and aristolochic acid [9]. LT, liver resection (LR), and radiofrequency ablation (RFA) are the three main curative modalities for HCC [2, 10]. Because of a shortage of donor livers and tumor location or diameter limitations, LR is the most common therapy for early and partial-intermediate stage HCC [10]. Remarkable improvements in surgical techniques and perioperative management have allowed selected patients with advanced-stage HCC to also undergo LR [11,12,13,14]. Unfortunately, the dramatically high incidence of postoperative recurrence significantly decreases the survival expectancy of patients with HCC after curative LR [2, 15, 16].
There are two common patterns of postoperative recurrence of HCC: early recurrence (ER) (≤ 2 years), which is derived from occult metastasis from the initial tumor, and late recurrence or de novo HCC (> 2 years after surgery), which arises from underlying liver diseases [17,18,19,20]. Since ER accounts for up to 70% of all postoperative recurrences and indicates poor long-term survival, it has garnered more attention [18,19,20]. Multiple risk factors associated with ER have been identified, such as microvascular invasion (MVI), high preoperative alpha fetoprotein (AFP) level, chronic active hepatitis, the absence of a tumor capsule, and large tumor size [17,18,19,20,21]. However, various postoperative therapies such as transcatheter arterial chemoembolization (TACE) [22,23,24], adoptive immunotherapy [25], iodine-131-labeled lipiodol [26, 27], interferon therapy [28], and cancer vaccines [29] have been shown to delay the postoperative recurrence of HCC, although these results need to be further verified. Therefore, identifying patients at high risk for ER who should receive adjuvant therapies might be a promising avenue for prolonging overall survival after curative LR.
Nomograms for predicting the outcomes of various diseases have been accepted by many investigators [30,31,32,33,34]. A nomogram is constructed based on the independent risk factors of special endpoints and is more accurate than commonly used staging systems [35]. Recently, Zhang et al. [36] established a nomogram to predict the incidence of ER in HCC with portal vein tumor thrombus after R0 LR. However, most curative LRs are performed in patients without macrovascular invasion, and nomograms for predicting ER in this subgroup of patients are lacking. Additionally, to the best of our knowledge, no study has analyzed the relationship between preoperative clinical parameters and ER. We believe that effective models for the prediction of ER would be helpful for surgeons in selecting optimal therapies and designing personalized surveillance strategies for HCC patients, especially during COVID-19 worldwide pandemic [37].
In this study, independent preoperative and postoperative risk factors for ER were identified in a large cohort of patients with HCC without macrovascular invasion. Two nomograms were then generated to preoperatively and postoperatively predict ER based on these factors. The performances of these nomograms were validated using an internal prospective cohort and receiver operating characteristic (ROC) curves.
Methods
Patients
To eliminate the heterogeneity in the treatment of HCC from treatment concepts and surgical techniques, this study included only patients who underwent curative-intent resection for HCC between January 2012 and December 2016 at the West China Hospital, Sichuan University. The inclusion criteria were as follows: (1) pathologically diagnosed HCC without lymph node metastasis; (2) absence of tumor thrombus in the major branches of the portal and hepatic veins; (3) initial curative LR, which was defined as the removal of all recognizable tumors with a clear margin; (4) age not less than 18 years; and (5) Child–Pugh class A liver function. The exclusion criteria were as follows: (1) patients with other types of tumors; (2) loss of follow-up within 2 years; (3) poor function of other major organs (heart, lung, and kidney); and (4) incomplete data. Finally, 698 patients who fulfilled our eligibility criteria were included in this study. Among them, 482 patients who underwent curative LR between January 2012 and December 2014 were allocated to the training cohort, and the remaining 216 patients who underwent curative LR between January 2014 and December 2016 were allocated to the internal prospective validation cohort. Detailed information on the two cohorts is presented in Table 1. This study was approved by the ethics committee of West China Hospital, Sichuan University. Written informed consent was obtained from each patient for the data used in the analysis.
Surgery
To prepare for surgery, imaging examinations, including contrast-enhanced computed tomography (CT) and/or magnetic resonance imaging (MRI), were performed to evaluate the characteristics of the tumor. Routine blood tests included blood cell analysis, liver/renal/coagulation function tests, hepatitis B virus (HBV)/HCV screening tests, HBV deoxyribonucleic acid (HBV-DNA) measurement, and serum tumor markers, including AFP, carcinoembryonic antigen (CEA), carbohydrate antigen 19–9 (CA199), and CA125. The albumin-bilirubin (ALBI) score was used to evaluate liver function in each patient and was computed using the following formula: − 0.085 × (albumin, g/L) + 0.66 × log (bilirubin, μmol/L). Patients were stratified into three groups according to previously described cutoffs, resulting in three grades: ALBI grade 1 (≤ − 2.60), grade 2 (> − 2.60 to − 1.39), and grade 3 (> − 1.39). Heart and lung functions were primarily evaluated by electrocardiography and chest radiography, and echocardiography and pulmonary function tests were performed if necessary. Before surgery, a multidisciplinary team consultation was routinely performed to design individual treatments for all patients. Surgical decisions were made based on tumor characteristics, reserve liver function, American Society of Anesthesiologists score [38], and the technological feasibility of LR.
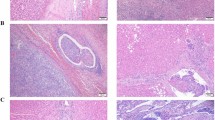
All the eligible patients underwent open surgery. A right subcostal incision with midline extension was performed. Intraoperative ultrasonography (US) was routinely performed to identify additional nodules that were not revealed preoperatively and determine a tumor-free margin of at least 1 cm. Anatomic resection was the first option for patients with an ideal tumor location and no obvious liver cirrhosis. To decrease surgical blood loss, intermittent Pringle maneuver was performed at a cycle of 15/5 min of clamp/unclamp time. After removal from the body, tumor specimens were fixed with 4% paraformaldehyde for 15 min and delivered to the histological department for histological examination. Finally, surgical information, including surgery duration, resection type, blood loss, and transfusion, was recorded carefully.
Follow-up
The postoperative follow-up program was described in our previous study [39]. In brief, all patients were regularly followed up in the first postoperative month, every 3 months for the next 3 years, and every 6 months thereafter. Abdominal US, serum AFP levels, HBV-DNA load, and liver function were routinely examined at each follow-up. Enhanced CT or MRI scans were performed when suspicious lesions were found or when AFP was persistently elevated. If necessary, bone scintigraphy or positron emission tomography was performed to confirm bone or distant metastases. Tumor recurrence was diagnosed based on the typical appearance of a new lesion on at least two radiological examinations with or without elevated AFP levels. Once HCC recurrence was diagnosed, the most appropriate treatments, such as rehepatectomy, RFA, salvage LT, TACE, sorafenib, and best supportive care, were recommended according to the characteristics of the recurrent tumors and liver function.
Recurrence time was defined as the interval between LR and the first diagnosis of recurrence. In line with previous studies, we classified tumors with a recurrence time of no more than 2 years as ER; otherwise, the recurrence pattern was classified as late recurrence [17,18,19,20]. Overall survival (OS) was defined as the interval between LR and death or last follow-up. The follow-up was conducted in March 2019.
Statistical analysis
All statistical analyses were performed using SPSS version 24.0 (IBM SPSS Inc,
Chicago, IL, USA) and R software version 3.5.0 with the rms package (http://www.r-project.org/). In order to make the prediction models easier to use, all quantitative variables in this study were categorized, including age, tumor size, and all blood test results. Categorical variables are expressed as numbers or percentages and were compared using Pearson’s chi-square or Fisher’s exact test. Univariate and stepwise multivariate analyses were performed using logistic regression to identify independent risk factors related to ER in the training cohort. Nomograms for preoperative and postoperative prediction of ER were generated based on the results of multivariate logistic regression analyses. The predictive performances of the nomograms were evaluated using the concordance index (C-index) and calibration curves. Model performance was validated using the internal prospective validation cohort. For the clinical use of the constructed nomograms, the total pre- and postoperative risk scores of each patient were calculated using the nomograms. ROC curve analysis was performed to calculate the optimal cutoff values that were determined by maximizing the Youden index (sensitivity + specificity − 1). The predictive ability of the optimal cutoff values was assessed based on the sensitivity, specificity, predictive values, and likelihood ratios. All analyses were two-tailed, and statistical significance was set at P < 0.05.
Results
Patient characteristics
The patient characteristics are shown in Table 1. Except for the neutrophil-to-lymphocyte ratio (NLR) (P = 0.007), platelet-to-lymphocyte ratio (PLR) (P = 0.011), ALBI grade (P = 0.025), and presence of cirrhosis (P = 0.016), the baseline and clinicopathological data were comparable between the training and validation cohorts. The median follow-up period for all included patients was 36 months (range, 1–78 months). ER was observed in 265 (55.0%) and 120 (55.6%) patients in the training and validation cohorts, respectively.
Independent predictors of early recurrence
As shown in Table 2, univariate logistic analyses revealed that multiple variables, including sex, age, hepatitis B surface antigen (HBsAg), HBV-DNA, hepatitis B e antigen, AFP, neutrophil count, platelet count, NLR, PLR, aspartate aminotransferase, gamma-glutamyl transpeptidase, tumor diameter, tumor number, Barcelona Clinic Liver Cancer stage, differentiation, MVI, satellite lesions, and resection type, were significantly associated with ER in the training cohort. Subsequent multivariate analyses further revealed that four preoperative risk factors, including age (P < 0.001), AFP level (< 20 vs 20–400 ng/mL, P = 0.001; < 20 vs > 400 ng/mL, P = 0.004), tumor diameter (≤ 5 vs 5–10 cm, P < 0.001; ≤ 5 vs > 10 cm, P = 0.008), and tumor number (1 vs 2, P = 0.019; 1 vs 3, P = 0.035). And five postoperative risk factors, including age (OR = 0.981, 95% CI 0.975–0.987, P < 0.001), tumor diameter (≤ 5 vs 5–10 cm, P < 0.001; ≤ 5 vs > 10 cm, P = 0.003), tumor number (1 vs 2, P = 0.003; 1 vs 3, P = 0.042), differentiation (P = 0.025), and MVI (P < 0.001), were significantly associated with ER in HCC patients without macrovascular invasion after curative LR (Table 3).
Construction of pre- and postoperative nomograms for predicting early recurrence
Two nomograms that integrated all significant independent factors for pre- and postoperative prediction of ER were generated using the rms package in R (Fig. 2). The C-indices of the pre- and postoperative nomograms in the training cohort were 0.712 (95% CI 0.666–0.758, P < 0.001) and 0.850 (95% CI 0.781–0.919, P < 0.001), respectively. The calibration plots showed ideal agreement on the incidence of ER between the predictions by the nomograms and the actual observations during follow-up (Fig. 1).
Pre- and postoperative nomograms and calibration curves for predicting early recurrence in training cohort. a The preoperative independent risk factors and nomogram for early recurrence. b The postoperative independent risk factors and nomogram for early recurrence. c The calibration curve of preoperative nomogram in training cohort. d The calibration curve of postoperative nomogram in raining cohort
For clinical use of the constructed nomograms, the projection of each variable on the point scale gave a unique score for each variable (Fig. 1). After adding the scores for all variables, the total points for each patient were calculated. Then, the projection of the total points on the probability scale represented the individual probability for ER.
Validation of the prediction models
The performances of the preoperative and postoperative nomograms were validated using the internal prospective validation cohort. The total preoperative and postoperative points for each patient in the validation cohort were calculated using the two nomograms. Then, the preoperative and postoperative total points were treated as a new risk factor to calculate the C-indices and produce calibration curves for ER. The C-indices for the pre- and postoperative prediction of ER in the validation cohort were 0.754 (95% CI 0.690–0.818, P < 0.001) and 0.857 (95% CI 0.750–0.949, P < 0.001), respectively. The calibration curves also showed ideal consistency between the predicted and observed probability of ER (Fig. 2).
In addition, the predictive performances of the nomograms were evaluated using ROC curve analysis (Fig. 3). In the training cohort, the areas under the ROC curves (AUCs) of the pre- and postoperative nomograms were 0.721 (95% CI 0.684–0.759, P < 0.001) and 0.848 (95% CI 0.814–0.883, P < 0.001) respectively; in the internal prospective validation cohort, the AUCs of the pre- and postoperative nomograms were 0.754 (95% CI 0.690–0.817, P < 0.001) and 0.844 (95% CI 0.790–0.897, P < 0.001), respectively. These were comparable with the C-indices of the nomograms. These results indicate that the constructed nomograms perform well in predicting ER for patients with HCC without macrovascular invasion after curative LR.
The predictive ability of the nomograms
The optimal cutoff values of the total preoperative and postoperative nomogram scores for predicting ER were 88 (range: 4–284) and 110 (range: 5–356), respectively (Table 4). For the preoperative model, the sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio for distinguishing ER were 0.611, 0.716, 0.704, 0.587, 2.151, and 0.543, respectively, in the training cohort and 0.730, 0.677, 0.733, 0.674, 2.260, and 0.399, respectively, in the validation cohort. For the postoperative model, the sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio for distinguishing ER were 0.706, 0.802, 0.793, 0.724, 3.564, and 0.367, respectively, in the training cohort, and 0.679, 0.800, 0.764, 0.699, 3.394, and 0.401, respectively, in the validation cohort.
Discussion
With the development of surgical techniques and perioperative management, LR has become increasingly safe for early, intermediate, and selected advanced-stage HCCs [40]. Further, prognostic analysis indicates that LR is more effective than other therapies for HCC patients with an advanced tumor burden [41, 42]. However, postoperative recurrence, especially ER, significantly shortens the survival expectancy for patients who undergo curative LR [18, 20, 21]. In addition, repeated treatments after recurrence not only seriously impacted patients’ quality of life but also heavily increased the medical burden.
Predictors of ER have been investigated in numerous studies. Imamura et al. [17] found that non-anatomical resection, the presence of MVI, and serum AFP ≥ 32 ng/mL were significantly associated with ER of HCC after hepatectomy. Portolani et al. [18] reported that cirrhosis, chronic active hepatitis, HCV positivity, vascular infiltration, and transaminase levels were significantly associated with ER in patients with HCC after hepatectomy. Cheng et al. [21] observed that a tumor diameter > 5 cm, the absence of a tumor capsule, and the presence of MVI were correlated with ER of solitary HCC after curative resection. A recent study conducted by Zhang et al. [36] revealed that HBV positivity, advanced portal vein tumor thrombus (PVTT), high HBV-DNA load, the presence of satellite nodules, elevated AFP, and large tumor diameter were significantly associated with ER of HCC with PVTT after R0 LR. In the present study, using a large cohort of HCC patients without macrovascular invasion, four preoperative and five postoperative independent risk factors for ER were identified. The nomograms based on these factors showed good predictive ability for ER, with C-indices of 0.721 and 0.850 for the pre- and postoperative models in the training cohort, respectively, and 0.754 and 0.857 for the pre- and postoperative models in the validation cohort, respectively. Further, the calibration curves in the training and validation cohorts showed ideal agreement between prediction and actual observation.
All risk factors incorporated in the present nomograms are easily obtainable clinically and have been demonstrated to be associated with the prognosis of HCC after curative LR. In this study, age was negatively associated with the incidence of postoperative ER. Compared with younger patients, elderly patients with HCC normally have lower AFP levels, lower rates of HBsAg positivity, and a lower tumor burden [43,44,45]. Furthermore, the levels of some serum tumor markers are significantly lower in elderly patients than in younger patients [46]. Tumor size and number are commonly used in various HCC staging systems [47,48,49]. Larger tumor size and more tumors indicate a higher probability of intrahepatic metastasis and a poorer prognosis [50,51,52,53,54]. Serum AFP level is not only a significant prognostic predictor for HCC [54,55,56,57], but is also associated with many metastatic characteristics of HCC, such as MVI [58], an incomplete tumor capsule [59, 60], and satellite lesions [61]. MVI is a signal of intrahepatic vessel dissemination [62], and has been repeatedly been shown to be an independent risk factor for ER and poor OS in HCC patients who undergo curative LR [63,64,65]. Tumors with poor pathological differentiation indicate tumor cells with aggressive behavior, which have a greater ability to proliferate and metastasize than tumor cells with good differentiation [66, 67].
The ROC curves showed that the optimal cutoff values for the pre- and postoperative nomograms were 88 and 110, respectively. A score equal to or greater than the cutoff values indicated a high risk of ER. In clinical practice, the preoperative nomogram might be useful for surgeons when designing therapy for patients with HCC. The postoperative nomogram may serve as a tool for selecting patients for adjuvant therapy and more frequent surveillance.
This study has some limitations. First, the models were constructed based on retrospective data, and their performance needs to be validated prospectively. Second, this study only included patients from a single center, and future external validation is necessary. Third, the main etiology of HCC in the present study was HBV infection, and the performances of the present models for HCC with other etiologies need to be validated. Finally, examination of other recurrence-related factors is necessary to further improve the predictive accuracy of these nomograms.
Conclusion
The present study revealed that four preoperative and five postoperative clinical variables were significantly associated with ER in patients with HCC without macrovascular invasion after curative LR. Two nomograms based on these predictors showed ideal predictive performance. These prediction models are meaningful for doctors when designing treatments before surgery and selecting patients for regular surveillance and administration of adjuvant therapies after surgery.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available because of patient privacy but are available from the corresponding author upon reasonable request.
Abbreviations
- HCC:
-
Hepatocellular carcinoma
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HDV:
-
Hepatitis D virus
- LT:
-
Liver transplantation
- LR:
-
Liver resection
- RFA:
-
Radiofrequency ablation
- ER:
-
Early recurrence
- MVI:
-
Microvascular invasion
- AFP:
-
Alpha-fetoprotein
- CEA:
-
Carcinoembryonic antigen
- CA199:
-
Carbohydrate antigen 19–9
- CA125:
-
Carbohydrate antigen 125
- TACE:
-
Transcatheter arterial chemoembolization
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the ROC curve
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- HBV-DNA:
-
Hepatitis B virus deoxyribonucleic acid
- ALBI:
-
Albumin-bilirubin
- US:
-
Ultrasonography
- OS:
-
Overall survival
- C-index:
-
Concordance index
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- HBsAg:
-
Hepatitis B surface antigen
- OR:
-
Odds ratio
- CI:
-
Confidence interval
- PVTT:
-
Portal vein tumor thrombus
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. https://doi.org/10.3322/caac.21262.
Llovet JM, Zucman-Rossi J, Pikarsky E, Sangro B, Schwartz M, Sherman M, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2016;2:16018. https://doi.org/10.1038/nrdp.2016.18.
El-Serag HB. Epidemiology of viral hepatitis and hepatocellular carcinoma. Gastroenterology. 2012;142(6):1264-73.e1. https://doi.org/10.1053/j.gastro.2011.12.061.
Park JW, Chen M, Colombo M, Roberts LR, Schwartz M, Chen PJ, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015;35(9):2155–66. https://doi.org/10.1111/liv.12818.
Yang JD, Mohamed EA, Aziz AO, Shousha HI, Hashem MB, Nabeel MM, et al. Characteristics, management, and outcomes of patients with hepatocellular carcinoma in Africa: a multicountry observational study from the Africa Liver Cancer Consortium. Lancet Gastroenterol Hepatol. 2017;2(2):103–11. https://doi.org/10.1016/s2468-1253(16)30161-3.
Baskiran A, Akbulut S, Sahin TT, Koc C, Karakas S, Ince V, et al. Effect of HBV-HDV co-infection on HBV-HCC co-recurrence in patients undergoing living donor liver transplantation. Hepatol Int. 2020;14(5):869–80. https://doi.org/10.1007/s12072-020-10085-3.
Younossi ZM, Blissett D, Blissett R, Henry L, Stepanova M, Younossi Y, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577–86. https://doi.org/10.1002/hep.28785.
Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73–84. https://doi.org/10.1002/hep.28431.
Yang JD, Hainaut P, Gores GJ, Amadou A, Plymoth A, Roberts LR. A global view of hepatocellular carcinoma: trends, risk, prevention and management. Nat Rev Gastroenterol Hepatol. 2019;16(10):589–604. https://doi.org/10.1038/s41575-019-0186-y.
Hartke J, Johnson M, Ghabril M. The diagnosis and treatment of hepatocellular carcinoma. Semin Diagn Pathol. 2017;34(2):153–9. https://doi.org/10.1053/j.semdp.2016.12.011.
Chok KS, Cheung TT, Chan SC, Poon RT, Fan ST, Lo CM. Surgical outcomes in hepatocellular carcinoma patients with portal vein tumor thrombosis. World J Surg. 2014;38(2):490–6. https://doi.org/10.1007/s00268-013-2290-4.
Ye JZ, Zhang YQ, Ye HH, Bai T, Ma L, Xiang BD, et al. Appropriate treatment strategies improve survival of hepatocellular carcinoma patients with portal vein tumor thrombus. World J Gastroenterol. 2014;20(45):17141–7. https://doi.org/10.3748/wjg.v20.i45.17141.
Kokudo T, Hasegawa K, Matsuyama Y, Takayama T, Izumi N, Kadoya M, et al. Survival benefit of liver resection for hepatocellular carcinoma associated with portal vein invasion. J Hepatol. 2016;65(5):938–43. https://doi.org/10.1016/j.jhep.2016.05.044.
Sakamoto K, Nagano H. Surgical treatment for advanced hepatocellular carcinoma with portal vein tumor thrombus. Hepatol Res. 2017;47(10):957–62. https://doi.org/10.1111/hepr.12923.
European Association for the Study of the Liver, European Organisation for Research and Treatment of Cancer. EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56(4):908–43. https://doi.org/10.1016/j.jhep.2011.12.001.
Belghiti J, Panis Y, Farges O, Benhamou JP, Fekete F. Intrahepatic recurrence after resection of hepatocellular carcinoma complicating cirrhosis. Ann Surg. 1991;214(2):114–7. https://doi.org/10.1097/00000658-199108000-00004.
Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J Hepatol. 2003;38(2):200–7.
Portolani N, Coniglio A, Ghidoni S, Giovanelli M, Benetti A, Tiberio GA, et al. Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg. 2006;243(2):229–35. https://doi.org/10.1097/01.sla.0000197706.21803.a1.
Cucchetti A, Piscaglia F, Caturelli E, Benvegnu L, Vivarelli M, Ercolani G, et al. Comparison of recurrence of hepatocellular carcinoma after resection in patients with cirrhosis to its occurrence in a surveilled cirrhotic population. Ann Surg Oncol. 2009;16(2):413–22. https://doi.org/10.1245/s10434-008-0232-4.
Poon RT. Differentiating early and late recurrences after resection of HCC in cirrhotic patients: implications on surveillance, prevention, and treatment strategies. Ann Surg Oncol. 2009;16(4):792–4. https://doi.org/10.1245/s10434-009-0330-y.
Cheng Z, Yang P, Qu S, Zhou J, Yang J, Yang X, et al. Risk factors and management for early and late intrahepatic recurrence of solitary hepatocellular carcinoma after curative resection. HPB (Oxford). 2015;17(5):422–7. https://doi.org/10.1111/hpb.12367.
Sun JJ, Wang K, Zhang CZ, Guo WX, Shi J, Cong WM, et al. Postoperative adjuvant transcatheter arterial chemoembolization after R0 hepatectomy improves outcomes of patients who have hepatocellular carcinoma with microvascular invasion. Ann Surg Oncol. 2016;23(4):1344–51. https://doi.org/10.1245/s10434-015-5008-z.
Liu S, Guo L, Li H, Zhang B, Sun J, Zhou C, et al. Postoperative adjuvant trans-arterial chemoembolization for patients with hepatocellular carcinoma and portal vein tumor thrombus. Ann Surg Oncol. 2018;25(7):2098–104. https://doi.org/10.1245/s10434-018-6438-1.
Zhang XP, Liu YC, Chen ZH, Sun JX, Wang K, Chai ZT, et al. Postoperative adjuvant transarterial chemoembolization improves outcomes of hepatocellular carcinoma associated with hepatic vein invasion: a propensity score matching analysis. Ann Surg Oncol. 2019;26(5):1465–73. https://doi.org/10.1245/s10434-019-07223-z.
Takayama T, Sekine T, Makuuchi M, Yamasaki S, Kosuge T, Yamamoto J, et al. Adoptive immunotherapy to lower postsurgical recurrence rates of hepatocellular carcinoma: a randomised trial. Lancet. 2000;356(9232):802–7. https://doi.org/10.1016/s0140-6736(00)02654-4.
Lau WY, Lai EC, Leung TW, Yu SC. Adjuvant intra-arterial iodine-131-labeled lipiodol for resectable hepatocellular carcinoma: a prospective randomized trial-update on 5-year and 10-year survival. Ann Surg. 2008;247(1):43–8. https://doi.org/10.1097/SLA.0b013e3181571047.
Boucher E, Corbinais S, Rolland Y, Bourguet P, Guyader D, Boudjema K, et al. Adjuvant intra-arterial injection of iodine-131-labeled lipiodol after resection of hepatocellular carcinoma. Hepatology. 2003;38(5):1237–41. https://doi.org/10.1053/jhep.2003.50473.
Sun HC, Tang ZY, Wang L, Qin LX, Ma ZC, Ye QH, et al. Postoperative interferon alpha treatment postponed recurrence and improved overall survival in patients after curative resection of HBV-related hepatocellular carcinoma: a randomized clinical trial. J Cancer Res Clin Oncol. 2006;132(7):458–65. https://doi.org/10.1007/s00432-006-0091-y.
Peng BG, Liang LJ, He Q, Kuang M, Lia JM, Lu MD, et al. Tumor vaccine against recurrence of hepatocellular carcinoma. World J Gastroenterol. 2005;11(5):700–4. https://doi.org/10.3748/wjg.v11.i5.700.
He Y, Zhu Z, Chen Y, Chen F, Wang Y, Ouyang C, et al. Development and validation of a novel diagnostic nomogram to differentiate between intestinal tuberculosis and Crohn’s disease: a 6-year prospective multicenter study. Am J Gastroenterol. 2019;114(3):490–9. https://doi.org/10.14309/ajg.0000000000000064.
Wang Y, Li J, Xia Y, Gong R, Wang K, Yan Z, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol. 2013;31(9):1188–95. https://doi.org/10.1200/jco.2012.41.5984.
Gross JP, Whelan TJ, Parulekar WR, Chen BE, Rademaker AW, Helenowski IB, et al. Development and validation of a nomogram to predict lymphedema following axillary surgery and radiotherapy in women with breast cancer from the NCIC CTG MA.20 randomized trial. Int J Radiat Oncol Biol Phys. 2019. https://doi.org/10.1016/j.ijrobp.2019.05.002.
Chon YE, Park H, Hyun HK, Ha Y, Kim MN, Kim BK, et al. Development of a new nomogram including neutrophil-to-lymphocyte ratio to predict survival in patients with hepatocellular carcinoma undergoing. Cancers. 2019. https://doi.org/10.3390/cancers11040509.
Nassiri F, Mamatjan Y, Suppiah S, Badhiwala JH, Mansouri S, Karimi S, et al. DNA methylation profiling to predict recurrence risk in meningioma: development and validation of a nomogram to optimize clinical management. Neuro Oncol. 2019. https://doi.org/10.1093/neuonc/noz061.
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–80. https://doi.org/10.1016/s1470-2045(14)71116-7.
Zhang XP, Chen ZH, Zhou TF, Li LQ, Chen MS, Wen TF, et al. A nomogram to predict early postoperative recurrence of hepatocellular carcinoma with portal vein tumour thrombus after R0 liver resection: a large-scale, multicenter study. Eur J Surg Oncol. 2019. https://doi.org/10.1016/j.ejso.2019.03.043.
Akbulut S, Garzali IU, Hargura AS, Aloun A, Yilmaz S. Screening, surveillance, and management of hepatocellular carcinoma during the COVID-19 pandemic: a narrative review. J Gastrointest Cancer. 2022. https://doi.org/10.1007/s12029-022-00830-2.
Owens WD, Felts JA, Spitznagel EL Jr. ASA physical status classifications: a study of consistency of ratings. Anesthesiology. 1978;49(4):239–43.
Xu L, Li L, Wang P, Zhang M, Zhang Y, Hao X, et al. Novel prognostic nomograms for hepatocellular carcinoma patients with microvascular invasion: experience from a single center. Gut Liver. 2019. https://doi.org/10.5009/gnl18489.
Vitale A, Burra P, Frigo AC, Trevisani F, Farinati F, Spolverato G, et al. Survival benefit of liver resection for patients with hepatocellular carcinoma across different Barcelona Clinic Liver Cancer stages: a multicentre study. J Hepatol. 2015;62(3):617–24. https://doi.org/10.1016/j.jhep.2014.10.037.
Zhong JH, Ke Y, Gong WF, Xiang BD, Ma L, Ye XP, et al. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma. Ann Surg. 2014;260(2):329–40. https://doi.org/10.1097/sla.0000000000000236.
Hsu CY, Liu PH, Hsia CY, Lee YH, Nagaria TS, Lee RC, et al. Surgical resection is better than transarterial chemoembolization for patients with hepatocellular carcinoma beyond the Milan Criteria: a prognostic nomogram study. Ann Surg Oncol. 2016;23(3):994–1002. https://doi.org/10.1245/s10434-015-4929-x.
Faber W, Stockmann M, Schirmer C, Mollerarnd A, Denecke T, Bahra M, et al. Significant impact of patient age on outcome after liver resection for HCC in cirrhosis. Eur J Surg Oncol. 2014;40(2):208–13. https://doi.org/10.1016/j.ejso.2013.10.018.
Huang J, Li BK, Chen GH, Li JQ, Zhang YQ, Li GH, et al. Long-term outcomes and prognostic factors of elderly patients with hepatocellular carcinoma undergoing hepatectomy. J Gastrointest Surg. 2009;13(9):1627–35. https://doi.org/10.1007/s11605-009-0933-4.
Motoyama H, Kobayashi A, Yokoyama T, Shimizu A, Sakai H, Furusawa N, et al. Impact of advanced age on the short- and long-term outcomes in patients undergoing hepatectomy for hepatocellular carcinoma: a single-center analysis over a 20-year period. Am J Surg. 2015;209(4):733–41. https://doi.org/10.1016/j.amjsurg.2014.05.026.
Yan H, Yang Y, Zhang L, Tang G, Wang Y, Xue G, et al. Characterization of the genotype and integration patterns of hepatitis B virus in early- and late-onset hepatocellular carcinoma. Hepatology. 2015;61(6):1821–31. https://doi.org/10.1002/hep.27722.
Llovet JM, Bru C, Bruix J. Prognosis of hepatocellular carcinoma: the BCLC staging classification. Semin Liver Dis. 1999;19(3):329–38. https://doi.org/10.1055/s-2007-1007122.
Minagawa M, Ikai I, Matsuyama Y, Yamaoka Y, Makuuchi M. Staging of hepatocellular carcinoma: assessment of the Japanese TNM and AJCC/UICC TNM systems in a cohort of 13,772 patients in Japan. Ann Surg. 2007;245(6):909–22. https://doi.org/10.1097/01.sla.0000254368.65878.da.
Yau T, Tang VY, Yao TJ, Fan ST, Lo CM, Poon RT. Development of Hong Kong Liver Cancer staging system with treatment stratification for patients with hepatocellular carcinoma. Gastroenterology. 2014;146(7):1691-700.e3. https://doi.org/10.1053/j.gastro.2014.02.032.
Chiappa A, Zbar AP, Audisio RA, Leone BE, Biella F, Staudacher C. Factors affecting survival and long-term outcome in the cirrhotic patient undergoing hepatic resection for hepatocellular carcinoma. Eur J Surg Oncol. 2000;26(4):387–92. https://doi.org/10.1053/ejso.1999.0904.
Fu YP, Yi Y, Huang JL, Jing CY, Sun J, Ni XC, et al. Prognostic nomograms stratify survival of patients with hepatocellular carcinoma without portal vein tumor thrombosis after curative resection. Oncologist. 2017;22(5):561–9. https://doi.org/10.1634/theoncologist.2016-0231.
Izumi R, Shimizu K, Ii T, Yagi M, Matsui O, Nonomura A, et al. Prognostic factors of hepatocellular carcinoma in patients undergoing hepatic resection. Gastroenterology. 1994;106(3):720–7.
Nathan H, Schulick RD, Choti MA, Pawlik TM. Predictors of survival after resection of early hepatocellular carcinoma. Ann Surg. 2009;249(5):799–805. https://doi.org/10.1097/SLA.0b013e3181a38eb5.
Ince V, Akbulut S, Otan E, Ersan V, Karakas S, Sahin TT, et al. Liver transplantation for hepatocellular carcinoma: Malatya experience and proposals for expanded criteria. J Gastrointest Cancer. 2020;51(3):998–1005. https://doi.org/10.1007/s12029-020-00424-w.
Ma WJ, Wang HY, Teng LS. Correlation analysis of preoperative serum alpha-fetoprotein (AFP) level and prognosis of hepatocellular carcinoma (HCC) after hepatectomy. World J Surg Oncol. 2013;11:212. https://doi.org/10.1186/1477-7819-11-212.
Allard MA, Sa Cunha A, Ruiz A, Vibert E, Sebagh M, Castaing D, et al. The postresection alpha-fetoprotein in cirrhotic patients with hepatocellular carcinoma. An independent predictor of outcome. J Gastrointest Surg. 2014;18(4):701–8. https://doi.org/10.1007/s11605-013-2433-9.
Zhang XF, Yin ZF, Wang K, Zhang ZQ, Qian HH, Shi LH. Changes of serum alpha-fetoprotein and alpha-fetoprotein-L3 after hepatectomy for hepatocellular carcinoma: prognostic significance. Hepatobiliary Pancreat Dis Int. 2012;11(6):618–23.
Lei Z, Li J, Wu D, Xia Y, Wang Q, Si A, et al. Nomogram for preoperative estimation of microvascular invasion risk in hepatitis B virus-related hepatocellular carcinoma within the Milan criteria. JAMA Surg. 2016;151(4):356–63. https://doi.org/10.1001/jamasurg.2015.4257.
Xu J, Liu C, Zhou L, Tian F, Tai MH, Wei JC, et al. Distinctions between clinicopathological factors and prognosis of alpha-fetoprotein negative and positive hepatocelluar carcinoma patients. Asian Pac J Cancer Prev. 2012;13(2):559–62. https://doi.org/10.7314/apjcp.2012.13.2.559.
Tada T, Kumada T, Toyoda H, Kiriyama S, Sone Y, Tanikawa M, et al. Relationship between Lens culinaris agglutinin-reactive alpha-fetoprotein and pathologic features of hepatocellular carcinoma. Liver Int. 2005;25(4):848–53. https://doi.org/10.1111/j.1478-3231.2005.01111.x.
Maeda T, Takenaka K, Taguchi K, Kajiyama K, Shirabe K, Shimada M, et al. Small hepatocellular carcinoma with minute satellite nodules. Hepatogastroenterology. 2000;47(34):1063–6.
Rodriguez-Peralvarez M, Luong TV, Andreana L, Meyer T, Dhillon AP, Burroughs AK. A systematic review of microvascular invasion in hepatocellular carcinoma: diagnostic and prognostic variability. Ann Surg Oncol. 2013;20(1):325–39. https://doi.org/10.1245/s10434-012-2513-1.
Fan ST, Poon RT, Yeung C, Lam CM, Lo CM, Yuen WK, et al. Outcome after partial hepatectomy for hepatocellular cancer within the Milan criteria. Br J Surg. 2011;98(9):1292–300. https://doi.org/10.1002/bjs.7583.
Kaibori M, Ishizaki M, Matsui K, Kwon AH. Predictors of microvascular invasion before hepatectomy for hepatocellular carcinoma. J Surg Oncol. 2010;102(5):462–8. https://doi.org/10.1002/jso.21631.
Wang CC, Iyer SG, Low JK, Lin CY, Wang SH, Lu SN, et al. Perioperative factors affecting long-term outcomes of 473 consecutive patients undergoing hepatectomy for hepatocellular carcinoma. Ann Surg Oncol. 2009;16(7):1832–42. https://doi.org/10.1245/s10434-009-0448-y.
Han DH, Choi GH, Kim KS, Choi JS, Park YN, Kim SU, et al. Prognostic significance of the worst grade in hepatocellular carcinoma with heterogeneous histologic grades of differentiation. J Gastroenterol Hepatol. 2013;28(8):1384–90. https://doi.org/10.1111/jgh.12200.
Sasaki K, Matsuda M, Ohkura Y, Kawamura Y, Inoue M, Hashimoto M, et al. In hepatocellular carcinomas, any proportion of poorly differentiated components is associated with poor prognosis after hepatectomy. World J Surg. 2014;38(5):1147–53. https://doi.org/10.1007/s00268-013-2374-1.
Acknowledgements
None.
Funding
This work was supported by the National Natural Science Foundation of China (Nos. 81802468 and 81772193), the 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (Nos. ZYGD20009 and ZYJC18008), the Sichuan Province Key Technologies R&D Program (No. 19ZDYF), the Key Technology Research and Development Program of the Sichuan Province (No. 2021YFSY0009), and the Post-Doctor Research Project, West China Hospital, Sichuan University (No. 2020HXBH076).
Author information
Authors and Affiliations
Contributions
TH and XMQ conceived and designed the study; ZYF, XLL, and LXZ performed the experiments; and XLL was responsible for the analysis and interpretation of data. ZYF wrote the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Clinical Medical Research Ethics Committee of West China Hospital of Sichuan University (IRB number: FWA00009482IRBIORG0004190) and performed in accordance with the Declaration of Helsinki. All patients signed a preoperative informed consent form and agreed to participate in accompanying scientific research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, Y., Lei, X., Xu, L. et al. Preoperative and postoperative nomograms for predicting early recurrence of hepatocellular carcinoma without macrovascular invasion after curative resection. BMC Surg 22, 233 (2022). https://doi.org/10.1186/s12893-022-01682-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-022-01682-0