Abstract
Background
Since the advent of immunohistochemistry for the diagnosis of stromal tumours, the incidence of leiomyosarcomas has significantly decreased. Nowadays, gastric leiomyosarcoma is an exceptionally rare tumour. We report the second case in the English literature of gastric leiomyosarcoma revealed with massive bleeding and hemodynamic instability and diagnostic pitfalls that we encountered.
Case presentation
A 63-year-old woman, with 2 years’ history of dizziness and weakness probably related to an anaemic syndrome, presented to the emergency room with hematemesis, melena and hemodynamic instability.
On examination, she had conjunctival pallor with reduced general condition, blood pressure of 90/45 mmHg and a pulse between 110 and 120 beats per minute. On digital rectal examination, she had melena. Laboratory blood tests revealed a haemoglobin level at 38 g/L.
The patient was admitted to the intensive care department. After initial resuscitation, transfusion and intravenous Omeprazole continuous infusion, her condition was stabilized. She underwent upper gastrointestinal endoscopy showing a tumour of the cardia, protruding in the lumen with mucosal ulceration and clots in the stomach. Biopsies were taken. Histological examination showed interlacing bundles of spindle cells, ill-defined cell borders, elongated hyperchromatic nuclei with marked pleomorphism and paranuclear vacuolization. Immunohistochemistry showed positivity for Vimentine, a strong and diffuse immunoreactivity for smooth muscle actin (SMA). Immunoreactivities for KIT and DOG1 were doubtful.
Computed tomography scan revealed a seven-cm tumour of the cardia, without adenopathy or liver metastasis.
The patient underwent laparotomy. A total gastrectomy was performed without lymphadenectomy. Post-operative course was uneventful.
Histological examination of the tumour specimen found the same features as preoperative biopsies with negative margins. We solicited a second opinion of an expert in a reference centre for sarcomas in France, who confirmed the diagnosis of a high grade gastric leiomyosarcoma.
Conclusion
Gastric leiomyosarcoma is a rare tumour. Diagnosis is based on histological examination with immunohistochemistry, which could be sometimes confusing like in our case. The validation of a pathological expert is recommended.
Similar content being viewed by others
Background
Gastrointestinal stromal tumours (GISTs) were considered to be of smooth muscle origin. They were misdiagnosed as leiomyomas and leiomyosarcomas. Since the advent of immunohistochemistry for the diagnosis of stromal tumours, the incidence of leiomyosarcomas has significantly decreased. Nowadays, gastric leiomyosarcoma is an exceptionally rare tumour [1]. Discovery of this tumour is generally made at a late stage as its growth is often insidious. Diagnosis relies on accurate histological examination with immunohistochemistry, as treatment and prognosis differ widely between different types of mesenchymal tumours.
We present the case of a gastric leiomyosarcoma revealed by a massive upper gastrointestinal bleeding and diagnostic pitfalls that we encountered.
Case presentation
A 63-year-old woman, with 2 years’ history of dizziness and weakness probably related to an anaemic syndrome, presented to the emergency room with hematemesis, melena and hemodynamic instability. There was no history of chronic liver disease, dyspepsia, ulcer disease, nonsteroidal anti-inflammatory drugs or aspirin use.
On examination, she had conjunctival pallor with reduced general condition, blood pressure of 90/45 mmHg and a pulse between 110 and 120 beats per minute. On digital rectal examination, she had melena. There were no abdominal wall varices, no hepatomegaly, and no palpable mass or adenopathy.
Laboratory blood tests revealed a haemoglobin level at 38 g/l with haematocrit at 13.4%. The mean corpuscular volume was in the normal range.
The patient was admitted to the intensive care department. After initial resuscitation, transfusion and intravenous Omeprazole continuous infusion, her condition was stabilized. She underwent upper gastrointestinal endoscopy showing a tumour of the cardia, protruding in the lumen with mucosal ulceration and clots in the stomach (Fig. 1). Biopsies were taken. Histological examination showed interlacing bundles of spindle cells, ill-defined cell borders, elongated hyperchromatic nuclei with marked pleomorphism and numerous mitoses. Immunohistochemistry showed positivity for Vimentine, a strong and diffuse immunoreactivity for SMA. Immunoreactivities for KIT and DOG1 were doubtful.
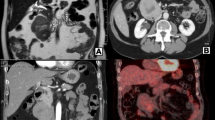
Computed tomography (CT) scan revealed a seven-cm tumour of the cardia, without adenopathy or liver metastasis (Fig. 2).
After multidisciplinary meeting, we suspected the diagnosis of stromal tumour of the cardia with high risk of re-bleeding and we decided to perform a total gastrectomy.
The patient underwent laparotomy. There was a nine-cm tumour of the cardia and the fundus, and no sign of peritoneal seeding or liver metastasis. A total gastrectomy was performed without lymphadenectomy (Fig. 3). Post-operative course was uneventful.
Histological examination of the tumour specimen found the same features as preoperative biopsies with negative margins (Fig. 4). We solicited a second opinion of an expert in a reference centre for sarcomas in France. Immunohistochemistry showed the following: DOG1 staining was focally positive for some normal cells of Cajal. Otherwise, neoplastic cells were DOG1 -, c Kit - (Fig. 5), CD34 -, smooth muscle actin + and h-caldesmon + (Fig. 6). In conclusion, it was in favour of a high grade gastric leiomyosarcoma.
Discussion and conclusion
Before the late 90’s, GISTs were misdiagnosed as leiomyomas and leiomyosarcomas [2]. Advances in immunohistochemistry led to the decrease of the incidence of gastric leiomyosarcomas to 1% of all malignant gastric tumours [1, 3, 4]. We report a case of this rare sarcoma with some particularities.
First, gastric leiomyosarcomas are generally insidious since they have a predominant extraluminal component [5]. It may be revealed by gastric outlet obstruction, perforation [6] or bleeding like in our case. Bleeding generally occurs when the tumour erodes the mucosa causing a chronic anaemia. Massive bleeding is not very common. To our knowledge, this is the second case in the literature of gastric leiomyosarcoma with massive bleeding and hemodynamic instability [4].
Second, arising between the muscularis propria and muscularis mucosa layers, diagnosis of leiomyosarcomas relies on histological examination of deep biopsies. Conventional endoscopy usually yields superficial and normal mucosa. Endoscopic ultrasonography, on the other hand, has been proved to be of great sensitivity, up to 97% [1], in the diagnosis of these tumours. It may be required to obtain deep biopsies. In our establishment, this technique was not available. Nevertheless, we succeeded to obtain an adequate sampling with conventional endoscopy. This is may be due to the endoluminal growth of the tumour and mucosal ulceration.
Third, histological examination was not evident. In the first and second pathology reports, based respectively on endoscopic biopsies and resection specimen, we had doubts about the positivity of KIT and DOG1 immunoreactivities. These two markers present the basis for the diagnosis of GISTs. Miettinen et al. declared that sensitivities of DOG1 and KIT were nearly identical: 94.4% and 94.7% [7]. DOG1 is considered the best marker for GISTs with better specificity [8, 9]. More recent studies showed that DOG1 positivity could be detected in neoplastic tissues other than GISTs [10,11,12]. But, there were no cases of gastric leiomyosarcoma with positive DOG1 staining like ours. In our case, positivity of DOG1 markers resulted in diagnostic confusion, especially that postoperative therapeutic approach will differ depending on whether it is a stromal tumour or not. In such cases, based on Ray-Coquard et al. study [13], the European Society for Medical Oncology (ESMO) recommends the validation of a pathological expert “when the original diagnosis was made outside a reference centre/network” [14]. So, we requested another opinion from an expert in France to confirm the diagnosis.
Finally, the localization of the tumour in the cardia is exceptional and presents a challenge for the surgeon especially if adjacent structures, such as the aorta, are invaded. In fact, surgery is the only curative option for leiomyosarcomas. The type of surgery depends on the size and localization of the tumour [15]. It ranges from a wedge resection to a total gastrectomy with en bloc resection if adjacent organs are invaded. In March 2018, Sato et al. first published a case of a small gastric leiomyosarcoma treated with endoscopic submucosal dissection [16]. Resection margins affect directly the prognosis. Systematic lymphadenectomy is not recommended as leiomyosarcoma have predilection for hematogenous spread and lymph node involvement is rare [6]. In our case, a total gastrectomy was performed rather than partial resection due to the size and localization of the tumour.
In conclusion, gastric leiomyosarcoma is a rare tumour. Diagnosis is based on histological examination with immunohistochemistry, which could be sometimes confusing like in our case. The validation of a pathological expert is recommended. Treatment depends on surgery with a very little place reserved for chemotherapy and radiotherapy in advanced cases [17, 18]. Prognosis is still very poor [1, 4, 19].
Abbreviations
- CT:
-
Computed tomography
- ESMO:
-
European Society for Medical Oncology
- GIST:
-
Gastrointestinal stromal tumours
- SMA:
-
Smooth muscle actin
References
Karila-Cohen P, Petit T, Kotobi H, Merran S. Léiomyosarcome gastrique. J Radiol. 2004;85:1993–7.
Bazin P, Cabanne F, Feroldi J, Martin JF. Tumeurs myoides intra-murales de l'estomac: considérations microscopiques à propos de 6 cas. Ann Anat Path. 1960;5:484–97.
Miettinen M, Fetsch JF. Evaluation of biological potential of smooth muscle tumours. Histopathology. 2006;48(1):97–105.
Soufi M, Errougani A, Chekkof RM. Primary gastric leiomyosarcoma in young revealed by a massive hematemesis. J Gastrointest Cancer. 2009;40(1–2):69–72.
Beyrouti MI, Beyrouti R, Ben Amar M, Frikha F, et al. Sarcomes gastriques. Presse Med. 2008;37:60–6.
Weledji EP, Enoworock G, Ngowe MN. Gastric leiomyosarcoma as a rare cause of gastric outlet obstruction and perforation: a case report. BMC Res Notes. 2014;7:479.
Miettinen M, Wang ZF, Lasota J. DOG1 antibody in the differential diagnosis of gastrointestinal stromal tumors: a study of 1840 cases. Am J Surg Pathol. 2009;33(9):1401–8.
Robert BW, Christopher LC, Xin C, Brian PR, Subbaya S, Kelli M, et al. The novel marker, DOG1, is expressed ubiquitously in gastrointestinal stromal tumors irrespective of KIT or PDGFRA mutation status. Am J Pathol. 2004;165(1):107–13.
González-Cámpora R, Delgado MD, Amate AH, Gallardo SP, León MS, Beltrán AL. Old and new immunohistochemical markers for the diagnosis of gastrointestinal stromal tumors. Anal Quant Cytol Histol. 2011;33(1):1–11.
Swalchick W, Shamekh R, Bui MM. Is DOG1 Immunoreactivity specific to gastrointestinal stromal tumor? Cancer Control. 2015;22(4):498–504.
Sah SP, McCluggage WG. DOG1 immunoreactivity in uterine leiomyosarcomas. J Clin Pathol. 2013;66(1):40–3.
So Jung L, Chung SH, Ahrong K, Kyungbin K, Kyung UC. Gastrointestinal tract spindle cell tumors with interstitial cells of Cajal: prevalence excluding gastrointestinal stromal tumors. Oncol Lett. 2016;12(2):1287–92.
Ray-Coquard I, Montesco MC, Coindre JM, et al. Sarcoma: concordance between initial diagnosis and centralized expert review in a population-based study within three European regions. Ann Oncol. 2012;23:2442–9.
The ESMO/European Sarcoma Network Working Group. Soft tissue and visceral sarcomas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2014;25(3):102–12.
Piso P, Schlitt HJ, Klempnauer J. Stromal sarcoma of the stomach: therapeutic considerations. Eur J Surg. 2000;166(12):954–8.
Sato T, Akahoshi K, Tomoeda N, Kinoshita N, Kubokawa M, Yodoe K, et al. Leiomyosarcoma of the stomach treated by endoscopic submucosal dissection. Clin J Gastroenterol. 2018;11:1–6.
Grant CS, Kim CH, Farrugia G, Zinsmeister A, Goellner JR. Gastric Leiomyosarcoma. Prognostic factors and surgical management. Arch Surg. 1991;126:985–90.
O’Hanlon DM, Griffin SM. Management of other oesophageal and gastric neoplasms. In upper gastrointestinal surgery. A companion to specialist surgical practice. Edited by Michael griffin S, Raimes SA. London, NW1 7DX. WB Saunders Company Ltd: England; 2000.
Hsieh CC, Shih CS, Wu YC, et al. Leiomyosarcoma of the gastric cardia and fundus. Zhonghua Yi Xue Za Zhi. 1999;62:418–24.
Acknowledgements
The authors are pleased to acknowledge professor Jean-François Emile (Department of Histopathology in Ambroise Paré Hospital, France), who contributed to the diagnostic study.
Availability of data and materials
Available at the request of the readers.
Author information
Authors and Affiliations
Contributions
Conception and design of study: HA, ZH, BMA, BA. Acquisition of data: HA, JR, HD. Data analysis and interpretation: JR, BBE, HD, HA. Drafting of manuscript: HA, ZH. Critical analysis and approval of final version of manuscript: BMA, BA. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient has given us a written permission to use her medical data in this manuscript.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Hasnaoui, A., Jouini, R., Haddad, D. et al. Gastric leiomyosarcoma and diagnostic pitfalls: a case report. BMC Surg 18, 62 (2018). https://doi.org/10.1186/s12893-018-0393-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-018-0393-4