Abstract
Background
Right hepatic arterial injury (RHAI) is the most common vascular injury sustained during laparoscopic cholecystectomy, occurring in up to 7% of cholecystectomies. RHAI is also the most common vascular injury associated with a bile duct injury (BDI) and is reported to occur in up to 41 – 61% of cases when routine angiography is employed following a BDI.
We present an unusual case of erosion of vascular coils from a previously embolised right hepatic artery into bilio-enteric anastomoses causing biliary obstruction. This is on a background of biliary reconstruction following a major BDI.
Case presentation
A 37-year old man underwent a bile duct reconstruction following a major BDI (Strasberg-Bismuth E4 injury) sustained at laparoscopic cholecystectomy. He had two separate bilio-enteric anastomoses of the right and left hepatic ducts and had a modified Terblanche Roux-en-Y access limb formed.
Approximately three weeks later he was admitted for significant gastrointestinal bleeding and was hypotensive and anaemic. Selective computed tomography angiography revealed a 2 x 2 centimetre right hepatic artery pseudoaneurysm, which was urgently embolised with radiological coils.
Two months later he developed intermittent fevers, rigors, jaundice, and right upper quadrant pain with evidence of intrahepatic biliary dilatation on magnetic resonance cholangiopancreatography. The degree of intrahepatic biliary dilatation progressively increased on subsequent imaging over several months, suggesting stricturing of the bilio-enteric anastomoses. Several attempts to traverse these strictures with a percutaneous transhepatic approach had failed. Then, approximately ten months after the initial BDI repair, choledochoscopy through the Terblanche access limb revealed multiple radiological coils within the bilio-enteric anastomoses, which had eroded from the previously embolised right hepatic artery. A laparotomy was performed to remove the coils, take down the existing obstructed bilio-enteric anastomoses and revise this. Following this the patient recovered uneventfully.
Conclusion
Obstructive jaundice and cholangitis secondary to erosion of angiographically placed embolisation coils is a rarely described complication. In view of the relative frequency of arterial injury and complications following major bile duct injury, we suggest that these patients be formally assessed for associated arterial injury following a major BDI.
Similar content being viewed by others
Background
Bile duct injury (BDI) associated with laparoscopic cholecystectomy (LC) occurs in 0.3 – 0.6% of cases [1]. Right hepatic arterial injury (RHAI) is the most common vascular injury during LC, occurring in up to 7% of cholecystectomies [2-4]. RHAI is also the commonest vascular injury associated with major BDI, with centers employing routine angiography following a BDI reporting RHAI rates of up to 41 – 61% [1,2,5], presumably secondary to the anatomical proximity of the right hepatic artery (RHA) to the bile duct (BD) [3,6]. Interestingly, where an associated biliary injury exists, arterial occlusions are far more common than pseudoaneurysms, however, where there is no biliary injury, reports of pseudoaneurysms are more common [3]. We present an unusual case of BDI repair complicated by RHA pseudoaneurysm requiring radiological coil embolisation, with a delayed complication of biliary obstruction secondary to erosion of coils into the hepato-enteric anastomosis.
Case presentation
A previously healthy 37-year old man was transferred to our service with high volume bilious drainage immediately following an elective LC for gallstone pancreatitis. An endoscopic retrograde cholangiopancreatography (ERCP) showed no flow above the mid common bile duct (CBD). Laparotomy found that the CBD was divided at the level of the cystic duct with segmental resection of the common hepatic duct involving the confluence of the hepatic ducts with separation of the right and left hepatic ducts (Strasberg-Bismuth E4 injury). A bile duct reconstruction was performed, bringing together the separated adjacent walls of the right and left hepatic ducts together and suturing them to form a common wall. The bilio-enteric anastomoses were then performed over separate externalised stents via a modified Terblanche Roux-en-Y limb [7]. The anastomoses on subsequent imaging gave the appearance of a preserved confluence, because of the sutured common adjoining walls of the right and left separated ducts. There was an uneventful recovery and he was discharged 10 days post-operatively with the biliary stents in situ.
One week after discharge, the patient experienced a gastrointestinal bleed and presented with melaena to a nearby hospital. He was found to have a haemoglobin level of 90 g/L (Reference range: 130 – 180 g/L) and was transfused with two units of packed red blood cells. He underwent a gastroscopy and colonoscopy to investigate this. No obvious cause for his bleeding was found, and one colonic pedunculated polyp was removed. His bleeding settled and he was discharged three days after admission. Our unit was not notified of this admission.
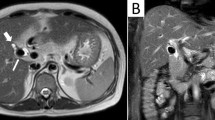
Two days following this discharge, the patient had an episode of haematochezia associated with collapse at home. He was taken to the emergency department of our hospital where he was hypotensive (blood pressure 92/63 mmHg) and tachycardic (heart rate 115 beats/min). His abdomen was soft and non-tender, and digital rectal examination revealed dark red blood. His haemoglobin level was 111 g/L. He was initially resuscitated with crystalloids, but had further episodes of fresh rectal bleeding. Repeat haemoglobin was 58 g/L, and packed red blood cell transfusion was commenced. Urgent selective computed tomography angiography was performed revealing a 2 × 2 centimetre aneurysm arising from the RHA/cystic artery adjacent to surgical clips. The aneurysm was embolised with platinum and stainless steel radiological coils (Figure 1, Figure 2). A tubogram through the biliary stents after the procedure showed no evidence of leakage or stricture of the biliary anastomoses. He had no further bleeding and was discharged three days later. Four weeks later, the stents were removed in the outpatient rooms.
Two months later the patient developed intermittent fevers, rigors, jaundice and right upper quadrant pain. His liver function tests revealed a cholestatic picture with an elevated bilirubin of 59 μmol/L (Reference range: 0 – 17 μmol/L), ALP 473 U/L (Reference range: 30 – 115 U/L) and GGT 721 U/L (Reference range: < 66 U/L).
A magnetic resonance cholangiopancreatography (MRCP) was performed, showing slight prominence of the intrahepatic biliary radicles above the level of the right and left main hepatic ducts, with preservation of the contour of the biliary ducts without evidence of irregularity or stenosis. A hepatobiliary iminodiacetic acid (HIDA) scan to assess biliary excretion showed mild retention of tracer in left hepatic lobe inferiorly in pre- and post-cholecystokinin images but no evidence to suggest biliary stenosis. It also suggested poor emptying from the Roux loop and it was felt that associated bacterial overgrowth within the Roux loop may have been responsible for his symptoms and he was kept on low dose oral antibiotics with improvement of his liver function tests at six weeks (bilirubin 9 U/L, ALP 361 U/L and GGT 504). Progress MRCP two months later revealed increasing intrahepatic biliary dilatation with the left main hepatic duct increasing in diameter from 6.6 mm on the previous MRCP to 9.8 mm, suggesting a significant bilio-enteric anastomotic stricture.
Thus, approximately 10 months after his BD reconstruction, he was admitted electively for percutaneous transhepatic cholangiography (PTC) and balloon dilatation of this bilio-enteric anastomosis. After confirmation of the stricture by PTC, a 4 French catheter was inserted into his left ductal system and an 8.5 French pigtail catheter was placed into his right ductal system but neither could be advanced into the enteric limb (Figure 3). Two further attempts were made at PTC balloon dilatation, but both failed. It was decided to attempt to visualise the anastomosis through the Terblanche access limb. Choledochoscopy through the modified Terblanche access limb showed multiple radiological coils from the previous embolisation of the RHA pseudoaneurysm at the site of the anastomoses, causing a mechanical obstruction (Figure 4, Figure 5). Laparotomy was performed and the bilio-enteric anastomoses were taken down to remove the coils. The right and left ductal systems were evaluated with intraoperative cholangiogram and the bilio-enteric anastomoses were revised using the existing Roux limb around 10 French infant feeding catheters, which were externalised again through the modified Terblanche limb.
Post-operative recovery was uneventful. A cholangiography through the catheters showed good drainage of contrast through the bilio-enteric anastomoses. The patient was discharged 10 days after his operation, with total resolution of his jaundice and improvement in eating, drinking and general daily function. The stents were removed at six weeks and six years later the patient remained well with normal liver function tests and no further episodes of cholangitis.
Discussion
From cadaveric studies, RHAI occurs in up to 7% of cholecystectomies. RHAI without concomitant BDI or portal vein injury rarely causes clinically significant liver or biliary ischaemia [2-4]. This may be due to the ability of the hilar marginal arteries to shunt blood from the left hepatic arterial system across to the remaining distal divided RHA system. It has been suggested that RHAI combined with biliary injuries can lead to ischaemic stricturing which may not become stable for several months following the injury and may be responsible for anastomotic stricturing after early repair [3]. Review of the vascularity of the BD has suggested that high anastomoses are to be preferred to low anastomoses [8]. Interestingly, there is disagreement as to whether a RHAI actually worsens biliary injury, which may relate to referral patterns and timing of repair [1]. Schmidt et al. found on univariate and mutivariate analyses that associated arterial injury and repair in the presence of active peritonitis were associated with increased complications after BDI [9]. However the delayed repair view is not universal, with many authors supporting early repairs [1,10,11]. A recent paper has emphasised that early repair by a specialist Hepatobiliary surgeon is associated with equivalent stricture rates to delayed repair but improved quality of life, return to normal activities and lower cost [12].
Hepatic artery pseudoaneurysm following LC has a reported incidence of 0.5 – 0.8% and can present four weeks post-operatively but may occur up to 13 months post-operatively [13-16]. Radiographic embolisation has been used successfully in the management of post-cholecystectomy pseudoaneurysms [13,15-18]. A variety of embolic agents have been described, including coils, Gelfoam, tissue adhesives, thrombin, detachable balloons and autologous clot [15]. Tulsyan et al. reported technical success in endovascular treatment of 11 hepatic artery pseudoaneurysms using coils, N-butylcyanoacrylate (N-BCA) glue or a combination of both depending on the desired rate of polymerisation [19]. The ideal placement of coils is a point of contention, with some authors advocating packing of the pseudoaneurysm itself and others suggesting “sandwich packing” (i.e. distal and proximal coil packing) to avoid rupturing the pseudoaneurysm [17], as well as to avoid coil migration [20,21]. In the elective setting, combination of stenting with a covered stent to maintain arterial flow and the packing and exclusion technique have been proposed, but no large series of this technique have yet been described and it may be problematic in the emergency setting [22-24].
Aneurysm coil migration from all sites into the gastrointestinal tract has been reported in at least twelve cases [25,26]. Coil migration into the CBD from the RHA has been reported in five cases (Table 1) [27,28]. Coil erosion into the BD or bilio-enteric anastomoses causing biliary obstruction is exceedingly rare, and we were only able to find three other reports of this in the literature [14,27,28].
Conclusion
Obstructive jaundice and cholangitis secondary to erosion of angiographically placed embolisation coils is a rarely described complication following treatment of arterial injury subsequent to iatrogenic BDI. In view of the relative frequency of arterial injury and complications following major BDI, we would suggest that these patients be formally assessed for associated arterial injury.
Consent
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
References
Pekolj J, Alvarez F, Palavecino M, Clariá R, Mazza O, De Santibañes E. Intraoperative management and repair of bile duct injuries sustained during 10,123 laparoscopic cholecystectomies in a high-volume referral center. J Am Coll Surg. 2013;216(5):894–901.
Alves A, Farges O, Nicolet J, Watrin T, Sauvanet A, Belghiti J. Incidence and consequence of an hepatic artery injury in patients with postcholecystectomy bile duct strictures. Ann Surg. 2003;238(1):93–6.
Strasberg S, Helton W. An analytical review of vasculobiliary injury in laparoscopic and open cholecystectomy. HPB (Oxford). 2011;13(1):1–14.
Halasz N. Cholecystectomy and hepatic artery injuries. Arch Surg. 1991;126(2):137–8.
Koffron A, Ferrario M, Parsons W, Nemcek A, Saker M, Abecassis M. Failed primary management of iatrogenic biliary injury: incidence and significance of concomitant hepatic arterial disruption. Surgery. 2001;130(4):722–8.
Stewart L, Robinson T, Lee C, Liu K, Whang K, Way L. Right hepatic artery injury associated with laparoscopic bile duct injury: incidence, mechanism, and consequences. J Gastrointest Surg. 2004;8(5):523–30.
Krige J, Bornman P, Harries-Jones E, Terblanche J. Modified hepaticojejunostomy for permanent biliary access. Br J Surg. 1987;74(7):612–3.
Terblanche J, Worthley C, Spence R, Krige J. High or low hepaticojejunostomy for bile duct strictures? Surgery. 1990;108(5):828–34.
Schmidt S, Settmacher U, Langrehr J, Neuhaus P. Management and outcome of patients with combined bile duct and hepatic arterial injuries after laparoscopic cholecystectomy. Surgery. 2004;135(6):613–8.
Stewart L. Iatrogenic biliary injuries: identification, classification, and management. Surg Clin North Am. 2014;94(2):297–310.
Perera M, Silva M, Hegab B, Muralidharan V, Bramhall S, Mayer A, et al. Specialist early and immediate repair of post-laparoscopic cholecystectomy bile duct injuries is associated with an improved long-term outcome. Ann Surg. 2011;253(3):553–60.
Dageforde L, Landman M, Feurer I, Poulose B, Pinson C, Moore D. A cost-effectiveness analysis of early vs late reconstruction of iatrogenic bile duct injuries. J Am Coll Surg. 2012;214(6):919–27.
Ozkan OS, Walser EM, Akinci D, Nealon W, Goodacre B. Guglielmi detachable coil erosion into the common bile duct after embolization of iatrogenic hepatic artery pseudoaneurysm. J Vasc Interv Radiol. 2002;13(9 Pt 1):935–8.
Rivitz S, Waltman A, Kelsey P. Embolization of an hepatic artery pseudoaneurysm following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 1996;19(1):43–6.
Sansonna F, Boati S, Sguinzi R, Migliorisi C, Pugliese F, Pugliese R. Severe hemobilia from hepatic artery pseudoaneurysm. Case Rep Gastrointest Med. 2011;2011:1–5.
Milburn J, Hussey J, Bachoo P, Gunn I. Right hepatic artery pseudoaneurysm thirteen months following laparoscopic cholecystectomy. EJVES Extra. 2007;13(1):1–3.
Nicholson T, Travis S, Ettles D, Dyet J, Sedman P, Wedgewood K, et al. Hepatic artery angiography and embolization for hemobilia following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol. 1999;22(1):20–4.
Johnson SR, Koehler A, PL K, Hanto DW. Long-term results of surgical repair of bile duct injuries following laparoscopic cholecystectomy. Surgery. 2000;128(4):668–77.
Tulsyan N, Kashyap VS, Greenberg RK, Sarac TP, Clair DG, Pierce G, et al. The endovascular management of visceral artery aneurysms and pseudoaneurysms. J Vasc Surg. 2007;45(2):276–83.
Takahashi T, Shimada K, Kobayashi N, Kakita A. Migration of steel-wire coils into the stomach after transcatheter arterial embolization for a bleeding splenic artery pseudoaneurysm: report of a case. Surg Today. 2001;31(5):458–62.
Shah NA, Akingboye A, Haldipur N, Mackinlay JY, Jacob G. Embolization coils migrating and being passed per rectum after embolization of a splenic artery pseudoaneurysm, “The Migrating Coil”: a case report. Cardiovasc Intervent Radiol. 2007;30(6):1259–62.
Van Steenbergen W, Lecluyse K, Maleux G, Pirenne J. Successful percutaneous cholangioscopic extraction of vascular coils that had eroded into the bile duct after liver transplantation. Endoscopy. 2007;39 Suppl 1:E210–1.
AlGhamdi HS, Saeed MA, AlTamimi AR, O’Hali WA, Khankan AA, AlTraif IH. Endoscopic extraction of vascular embolization coils that have migrated into the biliary tract in a liver transplant recipient. Dig Endoscopy. 2012;24(6):462–5.
DeFreitas D, Phade S, Stoner M, Bogey W, Powell C, Parker F. Endovascular stent exclusion of a hepatic artery pseudoaneurysm. Vasc Endovascular Surg. 2007;41(2):161–4.
Tekola BD, Arner DM, Behm BW. Coil migration after transarterial coil embolization of a splenic artery pseudoaneurysm. Case Rep Gastroenterol. 2013;7(3):487–91.
Han YM, Lee JY, Choi IJ, Kim CG, Cho S-J, Lee JH, et al. Endoscopic removal of a migrated coil after embolization of a splenic pseudoaneurysm: a case report. Clin Endosc. 2014;47(2):183–7.
Turaga KK, Amirlak B, Davis RE, Yousef K, Richards A, Fitzgibbons RJJ. Cholangitis after coil embolization of an iatrogenic hepatic artery pseudoaneurysm: an unusual case report. Surg Laparosc Endosc Percutan Tech. 2006;16(1):36–8.
Kao W, Chiou Y, Chen T. Coil migration into the common bile duct after embolization of a hepatic artery pseudoaneurysm. Endoscopy. 2011;43:E364–5.
Acknowledgement
We have no sources of funding to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SR, MC, KA, GS and NM were involved in the conception and design of the case report and ongoing critical revisions of the manuscript. All authors gave final approval of the version to be published.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Raashed, S., Chandrasegaram, M.D., Alsaleh, K. et al. Vascular coil erosion into hepaticojejunostomy following hepatic arterial embolisation. BMC Surg 15, 51 (2015). https://doi.org/10.1186/s12893-015-0039-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12893-015-0039-8