Abstract
Purpose
To assess the test–retest and inter-rater reliability of goniometry and fleximetry in measuring cervical range of motion in individuals with chronic neck pain.
Methods
A reliability study. Thirty individuals with chronic neck pain were selected. Cervical range of motion was measured by goniometry and fleximetry at two time points 7 days apart. To characterize the sample, we used the numerical pain rating scale, Pain-Related Catastrophizing Thoughts Scale, and Neck Disability Index. Intraclass correlation coefficient (ICC), standard error of measurement (SEM) and minimum detectable change (MDC) were calculated. Correlations between goniometry and fleximetry measurements were performed using Spearman’s correlation coefficient (rho).
Results
For goniometry, we found excellent test–retest reliability (ICC ≥ 0.986, SEM ≤ 1.89%, MDC ≤ 5.23%) and inter-rater reliability (ICC ≥ 0.947, SEM ≤ 3.91%, MDC ≤ 10.84%). Similarly, we found excellent test–retest reliability (ICC ≥ 0.969, SEM ≤ 2.71%, MDC ≤ 7.52%) and inter-rater reliability (ICC ≥ 0.981, SEM ≤ 1.88%, MDC ≤ 5.20%) for fleximetry. Finally, we observed a strong correlation between the goniometry and the fleximetry for all cervical movements (rho ≥ 0.993).
Conclusion
Goniometry and fleximetry measurements are reliable for assessing cervical range of motion in individuals with chronic neck pain.
Similar content being viewed by others
Introduction
Chronic neck pain is a multifactorial condition with variable clinical features [1, 2]. Therefore, in addition to the use of scales or questionnaires to measure, for example, pain intensity and disability, cervical range of motion should be part of the physical examination performed in individuals with chronic neck pain to allow a better understanding of the clinical characteristics, in addition to being a measure moderately correlated with pain intensity, disability, and fear of movement [3].
Various instruments for measuring cervical range of motion have been reported in the scientific literature, such as a smartphone app [4], cervical range of motion tools [5], goniometry [6], and gravity inclinometry. In Brazil, fleximetry is gravity inclinometry with Velcro fastening system [7]. The goniometry is a low-cost instrument commonly used to measure range of motion of multiple joints. Regarding the evaluation of the reliability of the goniometry in measuring cervical range of motion, Farooq et al.[6] and Rondoni et al. [8] identified adequate reliability for measuring cervical range of motion in healthy individuals, with intraclass correlation coefficient (ICC) ranging from 0.79 to 0.98, and Chaves et al. [9] used a goniometry in healthy individuals, identifying moderate reliability for all cervical movements, with an ICC ranging from 0.44 to 0.54.
The fleximetry is an instrument specially used in Brazil [7], due to the robust commercialization of this equipment by several companies. It has evaluation characteristics similar to those of the goniometry; however, it uses Velcro to attach the device to the body. Among the few published studies on the cervical region, the most important one found test–retest and inter-rater reliability ranging from moderate to excellent for the use of a fleximetry in healthy individuals [7].
Previous research in healthy individuals cannot be extrapolated to individuals with chronic neck pain [6, 7]. Previous studies indicate that individuals with chronic neck pain have lower cervical range of motion compared to healthy individuals, and psychological aspects related to chronic pain imply lower cervical range of motion, such as kinesiophobia [10, 11]. Furthermore, there is a consensus in the literature regarding the influence of sample characteristics on the measurement properties of instruments, which justifies the need for research on cervical range of motion [12].
The cervical range of motion (CROM) device has good reliability and is widely used in clinical and research settings [13]. However, it is more expensive than the regular goniometry and fleximetry. Therefore, the greater the number of reliable instruments, the greater the clinical assessment repertoire. Therefore, the purpose of this study was to assess the test–retest and inter-rater reliability of goniometry and fleximetry in measuring cervical range of motion in individuals with chronic neck pain.
Methods
Design and ethics aspects
This is a reliability study whose report is based on the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) [14]. Individuals signed an informed consent form prior to participation. The study was approved by the institution’s human research ethics committee (opinion number 2.935.437).
Individuals and eligibility criteria
Individual recruitment occurred after the study’s disclosure by means of posters, pamphlets, social networks, and messaging apps from August 2020 to July 2021. The data collection was performed in a private, well-lit, temperature-controlled room, without external noises, located in a physiotherapy clinic in the city of São Luís (Maranhão, northeast of Brazil).
A priori sample size calculation was performed considering a confidence coefficient of 0.95 and an amplitude of the confidence interval for the ICC of 0.30. The calculation was performed to detect moderate reliability (ICC = 0.75) according to the study conducted by Fleiss [15]. Therefore, a minimum sample size of 24 individuals was estimated. The calculation of the sample size was performed based on the study by Bonett [16].
The inclusion criteria were: age between 18 and 59 years; either sexes; verbal reports of neck pain for more than ninety days; and a score in the numerical pain rating scale (NPRS) ≥ 3 points [17]. The exclusion criteria were: the presence of specific neck pain (neck pain attributable to a specific and identifiable cause, such as a history of spinal surgery and/or vertebral fractures; spondylosis and spondylolisthesis; the presence of radiculopathy and/or herniated disc confirmed by imaging and neurological impairment by physical examination with the presence of altered sensitivity, reflex and/or muscle strength); a history of physical therapy interventions for neck pain in the last ninety days or medication (anti-inflammatory, painkillers and/or muscle relaxants) in the last seven days; a medical diagnosis of cancer, rheumatological, neurological, psychiatric, cardiovascular or metabolic diseases; and pregnancy [18, 19].
Pain assessment
We used three instruments to characterize the chronic neck pain of the individuals within the biopsychosocial context. Thus, pain intensity, disability, and catastrophizing were assessed to allow an understanding of the main components related to the multidimensional pain assessment.
The NPRS is a scale used to quantify pain intensity by means of a sequence of eleven numbers (0 represents "no pain" and 10 indicates "the worst pain you can imagine"). For pain with movement, we asked the individual to perform flexion, extension, lateral flexion to the left and right, and rotation to the left and right. After that, we evaluated the highest pain intensity perceived by the individual, regardless of which movement evoked the pain. This scale was previously validated in Portuguese [17].
The Pain-Related Catastrophizing Thoughts Scale (PCTS) is composed of nine items arranged on a Likert scale that varies in a numerical measure from 0 to 5 associated with the words "almost never" and "almost always". The total score is obtained by the sum of the total score, divided by the number of items answered. The final scores range from 0 to 5 points, with higher scores indicating a higher occurrence of catastrophic thoughts according to the version adapted to the Brazilian population [20].
The Neck Disability Index (NDI) is a questionnaire that has been adapted and validated for the Brazilian population, which is capable of measuring disability in individuals with chronic neck pain. It consists of 10 items with 6 response possibilities, ranging from 0 to 5. The total score varies from 0 to 50 points; the higher the value, the greater the disability [21].
The Baecke Habitual Physical Activity Questionnaire (BHPAQ) was used to assess the individuals’ habitual physical activity.14 It is an instrument that has already been validated for the Brazilian population, which measures physical activity in the occupational, sports, and leisure dimensions. The score for each domain varies between 1 and 5 points, with no cutoff points. Lower scores correspond to less active individuals [22].
Data collection flow
After application of the eligibility criteria and evaluation of neck cervical by an independent researcher (not involved in the measurement of cervical range of motion), the first rater measured the cervical range of motion (flexion, extension, lateral flexion to the left, lateral flexion to the right, rotation to the left, and rotation to the right) using a goniometry or fleximetry (the choice of instrument order was defined by drawing lots, i.e., first goniometry followed by fleximetry or vice versa).
After 10 min of rest, the second rater performed the same measurement. After 10 min of rest, the first rater measured the movements using the instrument that was not previously used and, finally, after 10 min of rest, the second rater also carried out the evaluation with the second instrument (Fig. 1). For the reliability analysis, the raters repeated the procedure after a seven-day interval between the test sessions [23]. The order of movements to be measured was defined by drawing lots before starting the data collection.
The raters have at least three years of clinical experience in evaluating and treating individuals with chronic neck pain. Also, the two raters performed four weeks of training prior to the study: lectures were carried out informing the technical details of the equipment; the raters handled the instrument; there was standardization of the approach and verbal command during data collection; a safety protocol established to proceed in the face of adverse reactions (such as increased pain through repetitive movements, nausea and dizziness).
Goniometry
We measured the cervical range of motion for flexion, extension, lateral flexion and rotation with the individual seated according to Marques [24]. Flexion and extension: the axis of the goniometer was positioned at the level of the seventh cervical vertebra, with the fixed arm kept perpendicular to the ground, and at the end of the movement, the mobile arm was aligned with the earlobe. Lateral flexion (right/left): the axis of the goniometer was positioned over the spinous process of C7, the fixed arm was perpendicular to the ground, and the mobile arm was on the midline of the cervical spine. Rotation (right/left): the goniometer axis was positioned at the center of the head, the fixed arm was positioned at the center of the head, and at the end of the movement, the mobile arm was aligned with the nose. Figure 2 shows the measurement of cervical range of motion using the goniometer.
Measurements with goniometer of range of motion for flexion (A), extension (B), rotation to the right (C), lateral flexion to the right (D), lateral flexion to the left (E), and rotation to the left (F). Before and during the movements, all individuals were instructed not to compensate the movement with the trunk (thoracolumbar region), thus isolating the movement specifically to the cervical region
Fleximetry
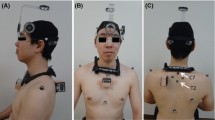
We measured the cervical range of motion for flexion, extension, lateral flexion and rotation according to Florêncio et al. [7]. Flexion/extension: the volunteer was placed in a seated position, with feet flat on the floor, and fleximeter in the right temporal region. Lateral lateral flexion (right/left): we used the same individual positioning and fleximeter in the central occipital region. Rotation (right/left): we place the individual supine, with their head off the stretcher, and the fleximeter in the upper central region of the skull. Figure 3 shows the measurement of cervical range of motion using fleximetry.
Measurements with fleximetry of range of motion for flexion (A), lateral flexion to the right (B), rotation to the left (C), extension (D), lateral flexion to the left (E), and rotation to the right (C). Before and during the movements, all individuals were instructed not to compensate the movement with the trunk (thoracolumbar region), thus isolating the movement specifically to the cervical region
Statistical analysis
The intraclass correlation coefficient (ICC) and 95% of confidence interval were used to determine the test–retest and inter-rater reliability in the measurement of cervical spine movements performed by means of goniometry and fleximetry, considering two-way mixed effects, absolute agreement, multiple raters/measurements [25]. We also used the standard error of measurement (SEM) and minimum detectable change (MDC) at 95% of confidence interval [26].
The classification to ICC was based on Fleiss [15]: values below 0.40 indicate low reliability; between 0.40 and 0.75, moderate reliability; between 0.75 and 0.90, substantial reliability; and greater than 0.90, excellent reliability. Interpretation of the SEM value was as follows: ≤ 5% = very good; > 5% and ≤ 10% = good; > 10% and ≤ 20% = doubtful; and > 20% = negative [27].
For the correlations between the goniometry and fleximetry, we initially applied the Shapiro–Wilk test, followed by the Spearman’s correlation coefficient (rho). We consider correlations adequate when above 0.7 [12]. Data processing was performed using the SPSS software, version 17.0 (Chicago, IL, USA), and a significance level of 5% was adopted in all analyses.
Results
Thirty-two individuals were recruited for the study, two of whom were excluded for not attending the retest session. Thus, the final sample consisted of thirty individuals. Table 1 describes the characteristics of the study individuals. The majority are female (70%, n = 21), with a body mass of 66.24 and a stature of 1.61 (± 0.07).
For goniometry (Tables 2 and 3), we found excellent test–retest reliability (ICC ≥ 0.986, SEM ≤ 1.89%, MDC ≤ 5.23%) and inter-rater reliability (ICC ≥ 0.947, SEM ≤ 3.91%, MDC ≤ 10.84%). Similarly, for fleximetry (Tables 4 and 5), we found excellent test–retest reliability (ICC ≥ 0.969, SEM ≤ 2.71%, MDC ≤ 7.52%) and inter-rater reliability (ICC ≥ 0.981, SEM ≤ 1.88%, MDC ≤ 5.20%).
We observed a strong correlation between the goniometry and the fleximetry for all cervical movements (rho ≥ 0.993), proving that the instruments are in agreement (Table 6).
Discussion
The instruments tested in this study (goniometry and fleximetry) have excellent reliability in individuals with chronic neck pain when using different times and raters to assess cervical range of motion.
In addition to the goniometry’s reliability for cervical range of motion in healthy individuals [6], the literature presents the following results for other joints: shoulder [28, 29], hip [30], knee [31], ankle [32], finger [33], wrist [34], and lower back [35]. For the fleximetry, in addition to the reliability study in healthy individuals [7, 36], only one reliability study was conducted with chronic shoulder pain [28, 29]. In our study, we observed higher ICC values (greater than 0.90), which can be explained by 2 reasons: 1) the clinical experience of the raters and their prior training prior to data collection, which leads to standardization in the scoring and consequently to similar values in the measurement of cervical range of motion; and 2) the use of the mean of 3 repetitions in the statistical analysis, which leads to less scatter.
In addition to the ICC, we found adequate SEM (< 5%) and MDC values. According to a previous study, SEM values less than 5% are very good, but for MDC, no interpretative values have been established in the literature [27]. From previously published reliability studies of cervical range of motion in healthy subjects, Farooq et al. [6] found SEM values ≤ 3.35º, while Florêncio et al. [7] did not calculate SEM. MDC was not calculated in either study.
Regarding clinical interpretation, Gajdosik and Bohannon [38] state that range of motion is just range of motion, although the relationship between cervical range of motion and disability has been described previously [37]. Therefore, measurement of this joint aspect needs to be complemented by other clinical measures such as pain intensity, disability, and kinesiophobia in individuals with chronic neck pain.
The high magnitude correlations between the goniometry and fleximetry found in the present study, in addition to the excellent reliability of the two instruments, support clinical professionals in choosing which instrument to use in their routine assessment of individuals with chronic neck pain.
Our study has some limitations that need to be described. Our study used analog devices, so it is not possible to extrapolate these results to digital devices for measuring cervical range of motion [38, 39]. Furthermore, our results do not support the reliability of goniometry and fleximetry to assess range of motion of other spinal regions. Our study did not assess the clinical stability of individuals’ symptoms at retest, and this should be considered when analyzing the results found here. We suggest that future studies use self-report instruments specifically adapted to the sample of interest, investigate whether the quantity of joint movements affects the quality of the measure under investigation, and whether other methods of measurement are reliable.
Conclusion
Goniometry and fleximetry measurements are reliable for assessing cervical range of motion in individuals with chronic neck pain.
Availbility of data and materials
The data and materials in this paper are available from the corresponding author on request.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- ICC:
-
Intraclass correlation coefficient
- SEM:
-
Standard error of measurement
- MDC:
-
Minimum detectable change
- Rho:
-
Spearman’s correlation coefficient
References
Rampazo ÉP, da Silva VR, de Andrade ALM, Back CGN, Madeleine PM, Arendt-Nielsen LLR. Sensory, motor, and psychosocial characteristics of individuals with chronic neck pain: a case-control study. Phys Ther. 2021;101:1–10.
Girasol CE, Dibai-Filho AV, de Oliveira AK, de Jesus Guirro RR. Correlation between skin temperature over myofascial trigger points in the upper trapezius muscle and range of motion, electromyographic activity, and pain in chronic neck pain patients. J Manipulative Physiol Ther. 2018;41:350–7.
Sarig Bahat H, Weiss PL, Sprecher E, Krasovsky A, Laufer Y. Do neck kinematics correlate with pain intensity, neck disability or with fear of motion? Man Ther. 2014;19:252–8.
Stenneberg MS, Busstra H, Eskes M, van Trijffel E, Cattrysse E, Scholten-Peeters GGM, et al. Concurrent validity and interrater reliability of a new smartphone application to assess 3D active cervical range of motion in patients with neck pain. Musculoskelet Sci Pract. 2018;34:59–65.
Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008;38:640–5.
Farooq MN, Mohseni Bandpei MA, Ali M, Khan GA. Reliability of the universal goniometer for assessing active cervical range of motion in asymptomatic healthy persons. Pakistan J Med Sci. 2016;32:457–61.
Florêncio LL, Pereira PA, Silva ERT, Pegoretti KS, Gonçalves MC, Bevilaqua-Grossi D. Agreement and reliability of two non-invasive methods for assessing cervical range of motion among young adults. Rev Bras Fisioter. 2010;14:175–81.
Rondoni A, Rossettini G, Ristori D, Gallo F, Strobe M, Giaretta F, et al. Intrarater and inter-rater reliability of active cervical range of motion in patients with nonspecific neck pain measured with technological and common use devices: a systematic review with meta-regression. J Manipulative Physiol Ther. 2017;40:597–608.
Chaves TC, Nagamine HM, Belli JFC, de Hannai MCT, Bevilaqua-Grossi D, de Oliveira AS. Reliability of fleximetry and goniometry for assessing cervical range of motion among children. Rev Bras Fisioter. 2008;12:283–9.
Rampazo ÉP, da Silva VR, de Andrade ALM, Back CGN, Madeleine P, Arendt-Nielsen L, et al. Sensory, Motor, and Psychosocial Characteristics of Individuals With Chronic Neck Pain: A Case Control Study. Phys Ther. 2021;101:33774667.
Asiri F, Reddy RS, Tedla JS, Al Mohiza MA, Alshahrani MS, Govindappa SC, et al. Kinesiophobia and its correlations with pain, proprioception, and functional performance among individuals with chronic neck pain. PLoS ONE. 2021;16: e0254262.
Prinsen CAC, Mokkink LB, Bouter LM, Alonso J, Patrick DL, de Vet HCW, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res. 2018;27:1147–57.
Williams MA, Williamson E, Gates S, Cooke MW. Reproducibility of the cervical range of motion (CROM) device for individuals with sub-acute whiplash associated disorders. Eur Spine J. 2012;21:872–8.
Kottner J, Audigé L, Brorson S, Donner A, Gajewski BJ, Hróbjartsson A, et al. Guidelines for reporting reliability and agreement studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64:96–106.
Fleiss JL. The design and analysis of clinical experiments. New York: Wiley; 1986.
Bonett DG. Sample size requirements for estimating intraclass correlations with desired precision. Stat Med. 2002;21:1331–5.
Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152:2399–404.
Dibai-Filho AV, De Oliveira AK, Girasol CE, Dias FRC, De Jesus Guirro RR. Additional effect of static ultrasound and diadynamic currents on myofascial trigger points in a manual therapy program for patients with chronic neck pain: a randomized clinical trial. Am J Phys Med Rehabil. 2017;96:243–52.
Pontes-Silva A, Avila MA, Fidelis-de-Paula-Gomes CA, Dibai-Filho AV. The Short-Form Neck Disability index has adequate measurement properties in chronic neck pain patients. Eur Spine J. 2021;30:3593–9.>
Sardá-Junior J, Nicholas MK, Pereira IA, Pimenta CA de M, Asghari A, Cruz RMC. Validation of the pain-related catastrophizing thoughts scale. Bangladesh J Med Sci. 2008;34:1–17.
Cook C, Richardson JK, Braga L, Menezes A, Soler X, Kume P, et al. Cross-cultural adaptation and validation of the Brazilian Portuguese version of the Neck Disability Index and Neck Pain and Disability Scale. Spine (Phila Pa 1976). 2006;31:1621–7.
Florindo AA, Dias de Oliveira Latorre M do R, Constante Jaime P, Tanaka T, de Freitas Zerbini CA. Methodology to evaluation the habitual physical activity in men aged 50 years of more. Rev Saude Publica. 2004;38:307–14.
Pinheiro JS, Monteiro OLS, Pinheiro CAB, Penha LMB, Almeida MQG, Bassi-Dibai D, et al. Seated single-arm shot-put test to measure the functional performance of the upper limbs in exercise practitioners with chronic shoulder pain: a reliability study. J Chiropr Med. 2020;19:153–8.
Marques AP. Manual de Goniometria. 2nd edition. São Paulo: Manole; 2003.
Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15:155–63.
Tucci HT, Martins J, Sposito GDC, Maria P, Camarini F. Closed kinetic chain Upper Extremity Stability test (CKCUES test): a reliability study in persons with and without shoulder impingement syndrome. Musculoskelet Disord. 2014;15:1–9.
Ostelo RWJG, De Vet HCW, Knol DL, Van Den Brandt PA. 24-Item Roland-Morris Disability Questionnaire was preferred out of six functional status questionnaires for post-lumbar disc surgery. J Clin Epidemiol. 2004;57:268–76.
MacDermid JC, Chesworth BM, Patterson S, Roth JH. Intratester and intertester reliability of goniometric measurement of passive lateral shoulder rotation. J Hand Ther. 1999;12:187–92.
Cools AM, De Wilde L, van Tongel A, Ceyssens C, Ryckewaert R, Cambier DC. Measuring shoulder external and internal rotation strength and range of motion: Comprehensive intra-rater and inter-rater reliability study of several testing protocols. J Shoulder Elb Surg. 2014;23:1454–61.
Pandya S, Florence JM, King WM, Robison JD, Oxman M, Province MA. Reliability of goniometric measurements in patients with Duchenne muscular dystrophy. Phys Ther. 1985;65:1339–42.
Hancock GE, Hepworth T, Wembridge K. Accuracy and reliability of knee goniometry methods. J Exp Orthop. 2018;5.
Youdas JW, Bogard CL, Suman VJ. Reliability of goniometric measurements and visual estimates of ankle joint active range of motion obtained in a clinical setting. Arch Phys Med Rehabil. 1993;74:1113–8.
van Kooij YE, Fink A, Nijhuis-van der Sanden MW, Speksnijder CM. The reliability and measurement error of protractor-based goniometry of the fingers: A systematic review. J Hand Ther. 2017;30:457–67.
Reissner L, Fischer G, List R, Taylor WR, Giovanoli P, Calcagni M. Minimal detectable difference of the finger and wrist range of motion: Comparison of goniometry and 3D motion analysis. J Orthop Surg Res. 2019;14:1–10.
Mieritz RM, Bronfort G, Kawchuk G, Breen A, Hartvigsen J. Reliability and measurement error of 3-dimensional regional lumbar motion measures: A systematic review. J Manipulative Physiol Ther. 2012;35:645–56.
Kubas C, Chen YW, Echeverri S, McCann SL, Denhoed MJ, Walker CJ, et al. Reliability and validity of cervical range of motion and muscle strength testing. J Strength Cond Res. 2017;31:1087–96.
Kim S, Kang K, Lee K. A correlation study on pain, range of motion of neck, Neck Disability Index and grip strength after thoracic manipulation and cervical stabilization training in chronic neck pain. J Korean Phys Ther. 2017;29:158–63.
Fraeulin L, Holzgreve F, Brinkbäumer M, Dziuba A, Friebe D, Klemz S, et al. Intra- and inter-rater reliability of joint range of motion tests using tape measure, digital inclinometer and inertial motion capturing. PLoS ONE. 2020;15: e0243646.
Torres R, Silva F, Pedrosa V, Ferreira J, Lopes A. The Acute Effect of Cryotherapy on Muscle Strength and Shoulder Proprioception. J Sport Rehabil. 2017;26:497–506.
Acknowledgements
We extend our gratitude to all the patients who so kindly volunteered to participate in this research, thereby forming our study sample.
Funding
This study was partially supported by the Coordination for the Improvement of Higher Education Personnel (CAPES, code 001) and by the Fundação de Amparo à Pesquisa e ao Desenvolvimento Científico e Tecnológico do Maranhão (FAPEMA, grant BM-01622/21). The funding source had no role in the study design, collection, analysis, interpretation of data, writing of the report, or in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
GGCA, AP-S, PCL, BSG, MLR, SKMPL, CAFPG, AVDF – Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Validation, Visualization, Writing (original draft, review, and editing).
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Universidade Federal do Maranhão – Brazil (report number: 2.935.437). Informed consent was obtained from all the individuals. All respondents participated in this study freely and with consent. All experiments were performed in accordance with relevant guidelines and regulations
Consent for publication
Informed consent was obtained from all subjects and/or their legal guardian(s).
Competing interests
AVDF, AP-S, and CAFPG are associate editors and peer reviewers of the BMC Musculoskeletal Disorders. The other authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Araujo, G.G.C., Pontes-Silva, A., Leal, P. et al. Goniometry and fleximetry measurements to assess cervical range of motion in individuals with chronic neck pain: a validity and reliability study. BMC Musculoskelet Disord 25, 651 (2024). https://doi.org/10.1186/s12891-024-07775-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07775-6