Abstract
Objective
To investigate the clinical significance of using 3D printing guides in modified unilateral puncture percutaneous vertebroplasty (PVP) for the treatment of osteoporotic vertebral compression fractures (OVCF), and to explore a new method for preventing paravertebral vein leakage during PVP in conjunction with a previous study of the optimal puncture-side bone cement/vertebral volume ratio(PSBCV/VV%).
Methods
This retrospective study analyzed 99 patients who underwent unilateral puncture PVP between January 2023 and December 2023. Patients were divided into a guide plate group (46 patients) and a conventional group (53 patients). The guide plate group underwent modified unilateral puncture PVP with the guidance of 3D printing guides, while the conventional group underwent unilateral puncture PVP using the conventional pedicle approach. The distribution of bone cement, surgical outcomes, and the occurrence of cement leakage into paravertebral veins were observed in both groups.
Results
The guide plate group had significantly shorter operating time and required fewer fluoroscopies compared to the conventional group. The amount of bone cement volume (BCV) used in the guide plate group was higher, but the amount of bone cement volume on the puncture side(PSBCV), the PSBCV/VV%, and the rate of paravertebral vein leakage were lower in the guide plate group compared to the conventional group (P < 0.05). Within each group, significant improvements in anterior vertebral margin height, Cobb angle, visual analog scale (VAS) score, and Oswestry Disability Index (ODI) were observed at 1 day and 1 month postoperatively compared to preoperative values (P < 0.05).
Conclusion
Using 3D printing guides in modified unilateral puncture PVP is a safe and effective method for treating OVCF. And it has the advantages of short operation time, less fluoroscopy, even distribution of bone cement, and a low rate of paravertebral vein leakage.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Osteoporosis is a common global endocrine disease, the incidence of which is increasing with the aging of the population [1,2,3,4]. According to a recent large-scale epidemiologic survey conducted in China, involving 20,416 participants, the prevalence of osteoporosis in individuals over the age of 40 was found to be 20.6% in women and 5% in men. Furthermore, the study highlighted that the prevalence of osteoporosis progressively increased with age [5]. Fractures are a common consequence of osteoporosis, with vertebral fractures being the most frequently observed [6,7,8]. Cui L [7] et al. reported that postmenopausal women had an incidence rate of vertebral fracture of 13.4% between the ages of 50 and 59, which further increased to 58.1% among those aged 80 years and above. The treatment options for osteoporotic vertebral compression fractures include conservative and surgical approaches [9]. PVP is a commonly performed surgical procedure for OVCF and is highly favored for its ability to provide rapid pain relief, stabilize the spine, and prevent complications associated with prolonged bed rest [9, 10]. There are two main approaches for PVP, namely unilateral puncture and bilateral puncture, and various studies have determined that there is no significant difference in therapeutic effectiveness between the two approaches [11, 12]. However, due to the shorter duration of the procedure and the reduced need for extensive fluoroscopies, an increasing number of medical professionals are now recommending the unilateral puncture approach [12,13,14]. The increasing recommendation of the unilateral approach by physicians is supported by several advantages, A meta-analysis by Yin P et al. [12]. showed that considering less operation time, less cement volume, lower mean radiation dose of patients, a lower rate of cement leakage and less surgery-related costs, we suggest that a unilateral PKP approach is advantageous. Another systematic review and meta-analysis by Sun H et al. [13]. also showed that we still encourage the use of the unipedicular approach as the preferred surgical technique for treatment of OVCFs due to less operation time, limited X-ray exposure, and minimal cement introduction and extravasat. A prospective randomized study by Zhang L et al. [14]. indicated that compared with bipedicular PVP, unipedicular PVP entails a shorter surgical time and lower X-ray irradiation. However, it is important to consider the potential disadvantages associated with unilateral puncture. One significant drawback is the poor distribution of cement, as it tends to be mainly concentrated on the puncture side [11]. This results in insufficient filling of the contralateral vertebral body with cement, which can compromise the effectiveness of the procedure. Our team’s previous study showed that when the PSBCV/VV% exceeded 13.68%, the risk of cement leakage from the paravertebral vein increased significantly [15]. Therefore, finding a solution to ensure better distribution of bone cement in unilateral puncture is an extremely crucial matter. As a part of this study, we incorporated the utilization of a guide plate created through 3D printing technology, which allowed us to determine the most optimal puncture path based on the specific computed tomography (CT) data of the patient before the surgical procedure. By choosing a puncture point that was positioned more laterally compared to the commonly used pedicle approach, and by increasing the internal inclination angle of the puncture, we aimed to create a puncture channel that could reach the vertebral body on the opposite side. We expect that using this method for PVP surgery will allow for a more even distribution of the cement, thereby prevent serious complications such as paravertebral vein leakage and pulmonary embolism.
Materials and methods
General Information
This is a retrospective analytical study in which we aimed to analyze and compare the outcomes of patients with OVCF who underwent PVP between January 2023 and December 2023 at our institution. The patients were divided into two groups: the guide plate group and the conventional group. In the guide plate group, the optimal puncture path was designed based on the patient’s CT data before surgery, a personalized puncture guide plate was printed, and unilateral puncture PVP was performed under the guidance of the guide plate during surgery. In the conventional group, unilateral puncture PVP was performed using the conventional method. The study was approved by the Ethics Committee of our hospital.
Inclusion and exclusion criteria
The inclusion criteria were as follows: (1) age greater than 55 years; (2) bone density findings suggestive of osteoporosis; (3) clear history of trauma; (4) compression fracture of a single vertebra; (5) CT and magnetic resonance imaging (MRI) findings suggestive of a fresh fracture; and (6) absence of psychiatric disorders and coagulation disorders.
The exclusion criteria were as follows: (1) vertebral compression fracture not caused by trauma; (2) compression fracture of multiple vertebrae; (3) severe compression fracture causing difficulty in puncture; (4) infection at the puncture site or combined with other systemic infections; (5) patients with other diseases who could not tolerate the surgery.
Surgical approach All surgeries were performed by experienced surgeons.Unilateral puncture PVP was performed in both groups. Bone cement and surgical instruments were provided by the same company (Via Andrea Doria).
The guide plate group: underwent modified unilateral puncture PVP using 3D-printed guide plate guidance
Guiding plate production: The patient’s CT data were imported into Mimics 21.0 software before the operation, the corresponding sequence was selected, and 3D reconstruction of the vertebral body was performed. The puncture point was planned on the 3D reconstructed model. The puncture point was more lateral than that of the conventional pedicle approach, and the puncture path was shaped along the lateral side of the pedicle to the medial side and finally reached the opposite side of the vertebral body. The reconstructed vertebral body model with the planned puncture pathway was copied and imported into 3-Matic software. To create the guide plate on 3-Matic software, the corresponding skin position of the patient was selected as the base of the guide plate, and the planned puncture channel was converted into a solid nail rod for Boolean operation to generate the guide plate. The guide plate was then converted into an STL file and imported into Materialise Magics 22.0 software for slicing. The slices were imported into a black flame S600 light-curing printer for printing, and the processed guide plate was sterilized preoperatively and prepared for intraoperative use (Fig. 1).
Surgical steps for the guide plate group
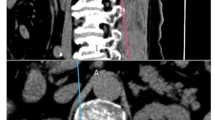
First, the patient was positioned in a prone position, with soft cushions placed under the chest and pubic symphysis to provide comfort and support. The abdomen was allowed to hang naturally, utilizing the force of gravity to restore the height of the vertebral body. Next, the operation area was prepared by sterilizing and laying a towel. C-arm fluoroscopy was then used to locate the punctured vertebral body. The side with clear visualization of the pedicle was chosen as the punctured side. Anesthesia was administered using 5 ml of lidocaine hydrochloride diluted 1:1 with 5 ml of saline. Align the marking line of the spinous process on the 3D printing guide with the top of the spinous process. To position the vertebral body for puncture, a positioning needle was inserted into the center of the guide plate puncture hole. The guide plate had been pre-designed to determine the distance of the puncture point from the midline and the internal inclination angle. These two parameters did not require adjustment during the operation. Since the change of body position causes the sagittal curvature of the vertebral body to change, the sagittal puncture angle only needs to be adjusted in the runway-shaped guide hole during the operation. In the lateral position, when the puncture needle is located at the posterior margin of the vertebral body, the orthogonal image of the puncture needle is precisely at the medial margin of the pedicle. The puncture is then continued into the anterior 1/3 of the vertebral body. Once the working channel is placed, the bone cement is prepared. The bone cement is injected while it is in the cement pulling phase. The injection of the bone cement is stopped when it approaches the posterior wall of the vertebral body(Fig. 2).
Surgical steps for the conventional group
Surgical steps for the conventional group were performed following the same positional repositioning, disinfection, and anesthesia procedures as in the guide group. The chosen puncture path involved the pedicle root approach. In the orthostatic image, the puncture entry point was located at the outer edge of the vertebral arch root, while the lateral image was positioned in the posterior aspect of the spinal canal. Adjustments were made to the puncture inclination angle and sagittal angle. In the lateral position, when the puncture needle was positioned at the posterior edge of the vertebral body, the orthostatic image showed it at the medial edge of the pedicle. The puncture was then continued into the anterior third of the vertebral body. The remaining steps of the procedure were identical to those in the guide plate group.
Outcome measurements
The clinical data of patients in the 2 groups were recorded, including age, sex, bone density, operation time, BCV, PSBCV, VV, PSBCV/VV%, bone cement distribution score, number of fluoroscopies, amount of anesthesia, as well as the height of anterior margin of the vertebral body, Cobb’s angle of the injured vertebrae, vas score, and ODI in the preoperative period, the first day of the postoperative period, and the first month of the postoperative period. Cement distribution score was recorded using an 8-point scale based on the postoperative frontal and lateral X-ray results (Fig. 3) [16].
The two surgeons imported the patient’s preoperative CT data into Mimics 21.0 software, used the threshold segmentation function to isolate the surgical vertebral body, and calculated the VV. The patient’s postoperative CT data were imported into the Mimics 21.0 software, and the bone cement was isolated using the threshold segmentation function, and the BCV and the PSBCV were calculated. As described in our previous study, the midpoints of the upper and lower vertebral endplates were marked on coronal CT scans to divide the vertebral body into left and right parts. PSBCV was defined as the volume of cement in half of the vertebral body on the side of the entry point (i.e., the puncture side) [15]. The two surgeons judged whether there was a leakage of cemented paravertebral veins based on postoperative CT and radiographic findings.
Statistical analysis
Data on continuous variables for the two groups of patients were expressed as \(\:\stackrel{-}{X}\)± s. The differences between the two groups were assessed by paired t- tests. the normality of the distribution of all the data were tested using the KS test. The differences between the two groups in terms of sex and paravertebral venous leakage were assessed using the X2- test. All of these were statistically analyzed using SPSS 24.0 software. The differences in the data between the preoperative and postoperative periods for the two groups were plotted using GraphPad Prism 9 software.
Results
From January 2023 to December 2023, a total of 99 patients with OVCF were enrolled, including 46 patients in the guide plate group and 53 patients in the conventional group, and all patients completed the surgery normally.
Characterization of baseline data
There was no statistically significant difference in sex, age, and bone mineral density of the patients in the two groups (Table 1).
Comparison of surgical operation data
The operating time in the guide plate group were significantly lower than thatin the conventional group (P = 0.000). The number of intraoperative fluoroscopies in the guide plate group were significantly lower than that in the conventional group (P = 0.000). The difference in the amount of surgical anesthetics used by the two groups of patients was not statistically significant (Table 2).
Comparison of bone cement and paravertebral vein leakage rates
The difference in VV between the two groups was not statistically significant. The BCV and cement distribution score were greater in the guide plate group than in the conventional group, but the PSBCV and the PSBCV/VV% were significantly lower in the guide plate group than in the conventional group. The rate of cemented paravertebral vein leakage was significantly greater in the conventional group than in the guide plate group (P = 0.045, Table 3).
Imaging analysis
The differences in the preoperative, 1-day postoperative, and 1-month postoperative heights of the anterior margin of the vertebral body and the Cobb angle of the injured vertebra were not statistically significant between the two groups of patients (Table 4). However, intragroup comparisons between the two groups of patients revealed statistically significant differences in the height of the anterior margin of the vertebral body and the Cobb angle of the injured vertebra at 1 day and 1 month postoperatively compared to the preoperative period (Fig. 4).
Comparison of prognosis
The differences in the preoperative, 1-day postoperative, and 1-month postoperative VAS scores and ODI dysfunction indices of the two groups of patients were not statistically significant (Table 5). However, intragroup comparisons between the two groups of patients revealed statistically significant differences in the VAS score and ODI at 1 day and 1 month postoperatively compared to the preoperative period (Fig. 5).
Discussion
Analysis of the therapeutic effect of unilateral puncture PVP guided by 3D- printed guide plate
This study showed no difference in the treatment of OVCF between the guide plate group and the conventional group. There was no significant difference in postoperative vertebral body height, postoperative Cobb angle, postoperative VAS score, and ODI between the two groups. However, all these parameters showed significant improvement compared to the preoperative period, indicating that both the guide plate group and the conventional group achieved good results in the treatment of OVCF.
The role of 3D-printed guide-guided unilateral puncture PVP in the prevention of cemented paravertebral vein leakage
Leakage of bone cement into the paravertebral veins is a common complication of PVP [15, 17]. This leakage can easily transfer cement to other locations, eventually entering the pulmonary vasculature and potentially causing life-threatening pulmonary embolism [18, 19]. Therefore, it is crucial to prevent leakage of bone cement into the paravertebral veins. Our research team showed that the PSBCV/VV% is an important risk factor for paravertebral vein leakage. We suggested that the risk of cement paravertebral vein leakage increases when the PSBCV/VV% exceeds 13.68% [15]. In this study, the incidence of paravertebral vein leakage in the guide plate group was significantly lower than that in the conventional group. The total amount of BCV injected in the guide plate group was greater, but the PSBCV and the PSBCV/VV% were lower compared to the conventional group. This is because the cement in the guide plate group was better distributed contralaterally, while the cement in the conventional group was mainly distributed on the puncture side. As a result, the PSBCV/VV% was higher in the conventional group, making it more prone to paravertebral vein leakage.
Advantages and disadvantages of conventional unilateral puncture PVP
PVP is a procedure in which bone cement is injected into the vertebral body through a special puncture tool and channel. This procedure provides quick pain relief, stabilizes the spine, and avoids complications associated with bed rest [9, 10]. In the past, PVP required bilateral puncture, which increased the operation time and fluoroscopic radiation dose. Some patients were unable to tolerate the prolonged prone position, preventing the surgery from being performed. In recent years, unilateral puncture PVP has been increasingly used in clinics. Numerous reports have shown that unilateral puncture PVP has the advantages of shorter operation time, fewer fluoroscopies, and lower operation risk, while achieving the same therapeutic effect as bilateral puncture [11, 14, 20, 21]. However, unilateral puncture PVP also has some disadvantages, with the most common being the distribution of bone cement. Due to the limited width of the pedicle root, it is difficult to reach the contralateral vertebral body during unilateral puncture, resulting in poor dispersion of cement in the contralateral vertebral body [20, 22]. Increasing the internal inclination angle of the puncture may lead to nerve injury and cemented spinal canal leakage. Therefore, improving the distribution of bone cement to the contralateral side in unilateral puncture PVP has become a recent research focus. Shi X et al. [20]. performed unilateral PVP using a puncture device with a bendable tip, which resulted in cement diffusion to the contralateral side, but the cement distribution was not controlled. Zhu D et al. [23]. used the extracorporeal puncture route for unilateral puncture, which allowed the puncture channel to reach the contralateral vertebrae. The study showed no difference in the distribution of bone cement compared to bilateral puncture, but it also pointed out that extracorporeal puncture may cause bone cement leakage through the puncture point of the vertebral body. Previous studies have shown that thoracic lateral pedicle puncture may cause pneumothorax, [24] and lateral lumbar pedicle puncture may cause arterial injury [25,26,27]. Therefore, the application of these methods is limited.
Unilateral puncture PVP guided by 3D- printed guide plates
In recent years, 3D printing technology has rapidly developed and is increasingly used in orthopedic surgery [28,29,30]. Among the applications, the use of 3D printing guide plates to assist surgery has become a research hotspot. Currently, 3D printing guide plates are mainly used to assist spinal pedicle screw implantation. Research has shown that 3D printing guide plate-assisted nail placement has the advantages of high accuracy and shorter operation time [31,32,33]. However, there is limited research on the application of 3D guides to assist puncture in PVP. The 3D guide plate designed in this study is personalized, based on the CT examination results of the patient before the operation. It is designed to have a more lateral puncture entry point compared to the conventional pedicle approach. The puncture path is shaped along the lateral side of the pedicle to the medial side, ultimately reaching the opposite side of the vertebral body. This design avoids the complications caused by lateral puncture of the pedicle root and the problem of poor cement dispersion in the interpedicular puncture of the pedicle root. Due to the greater internal inclination angle of the 3D guide plate group, the cement can be better dispersed to the contralateral side of the vertebral body. In this study, the cement distribution score in the guide plate group was significantly higher than that in the conventional group. The design of the guide plate in this study was based on preoperative CT planning of the internal inclination angle and sagittal angle of the puncture. As the sagittal angle of the vertebral body may change during the surgery, the guide plate was designed with a 1-cm-long runway shape for the sagittal angle, allowing for intraoperative adjustment. Because the guide plate group did not require intraoperative adjustment of the internal inclination angle and only required slight adjustment of the sagittal angle, the operative time was significantly shortened. The results of this study also showed that the operative time and the number of fluoroscopies were significantly lower in the guide plate group than in the conventional group.
Research shortcomings
One shortcoming of this study is that some intraoperative cemented venous leaks travelled distally with the blood flow and were therefore not detected on postoperative vertebral CT, which led to the speculation that the incidence of postoperative paravertebral venous leaks might be higher. Another shortcoming is that 3D-printed guides require a certain cost, and this study, because of research funding, can reduce some of the patients’ medical costs, which need to be evaluated for use in patients with poor financial ability. A final shortcoming of this study is that the study only included 1-month postoperative imaging data and lacked longer-term follow-up results, so it is not known whether there were differences in long-term complications between the 2 groups.
Conclusion
Both 3D printing guide plate-guided modified unilateral puncture PVP and conventional unilateral puncture PVP have good results in the treatment of OVCF. Compared to conventional unilateral puncture PVP, the 3D printing guide-guided modified unilateral puncture PVP has the advantages of shorter operation time, fewer fluoroscopies, and better distribution of bone cement. Due to the better cement distribution and lower PSBCV/VV% in the 3D printing guide plate-guided modified unilateral puncture PVP, it plays an important role in preventing cement leakage into the paravertebral veins.
Data availability
The datasets generated and/or analysed during the current study are not publicly available for data protection reasons. Data is available from the corresponding author on reasonable request.
Abbreviations
- PVP:
-
Percutaneous vertebroplasty
- OVCF:
-
Osteoporotic vertebral compression fractures
- PSBCV/VV%:
-
Puncture-side bone cement/vertebral volume ratio
- PSBCV:
-
Puncture-side bone cement volume
- VV:
-
Vertebral volume
- BCV:
-
Bone cement volume
- VAS:
-
Visual analogue scale
- ODI:
-
Oswestry dysfunction index
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
References
Park EJ, Joo IW, Jang MJ, Kim YT, Oh K, Oh HJ. Prevalence of osteoporosis in the Korean population based on Korea National Health and Nutrition Examination Survey (KNHANES), 2008–2011. Yonsei Med J. 2014;55(4):1049–57.
Yoshimura N, Muraki S, Oka H, Mabuchi A, En-Yo Y, Yoshida M, Saika A, Yoshida H, Suzuki T, Yamamoto S, et al. Prevalence of knee osteoarthritis, lumbar spondylosis, and osteoporosis in Japanese men and women: the research on osteoarthritis/osteoporosis against disability study. J Bone Min Metab. 2009;27(5):620–8.
Looker AC, Sarafrazi IN, Fan B, Shepherd JA. Trends in osteoporosis and low bone mass in older US adults, 2005–2006 through 2013–2014. Osteoporos Int. 2017;28(6):1979–88.
Häussler B, Gothe H, Göl D, Glaeske G, Pientka L, Felsenberg D. Epidemiology, treatment and costs of osteoporosis in Germany–the BoneEVA Study. Osteoporos Int. 2007;18(1):77–84.
Wang L, Yu W, Yin X, Cui L, Tang S, Jiang N, Cui L, Zhao N, Lin Q, Chen L, et al. Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. Jama Netw Open. 2021;4(8):e2121106.
Yu F, Xia W. The epidemiology of osteoporosis, associated fragility fractures, and management gap in China. Arch Osteoporos. 2019;14(1):32.
Cui L, Chen L, Xia W, Jiang Y, Cui L, Huang W, Wang W, Wang X, Pei Y, Zheng X, et al. Vertebral fracture in postmenopausal Chinese women: a population-based study. Osteoporos Int. 2017;28(9):2583–90.
Ballane G, Cauley JA, Luckey MM, El-Hajj FG. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28(5):1531–42.
Wang R, Xu Y, Ma X. Risk factors and strategies for recovery quality, postoperative pain, and recurrent fractures between percutaneous kyphoplasty and percutaneous vertebroplasty in elderly patients with thoracolumbar compression fractures: a retrospective comparative cohort study. Ann Transl Med. 2023;11(2):122.
Clark W, Bird P, Gonski P, Diamond TH, Smerdely P, Mcneil HP, Schlaphoff G, Bryant C, Barnes E, Gebski V. Safety and efficacy of vertebroplasty for acute painful osteoporotic fractures (VAPOUR): a multicentre, randomised, double-blind, placebo-controlled trial. Lancet. 2016;388(10052):1408–16.
Cheng X, Long HQ, Xu JH, Huang YL, Li FB. Comparison of unilateral versus bilateral percutaneous kyphoplasty for the treatment of patients with osteoporosis vertebral compression fracture (OVCF): a systematic review and meta-analysis. Eur Spine J. 2016;25(11):3439–49.
Yin P, Ji Q, Wang Y, Liu Y, Wu Y, Yu Y, Hai Y, Su Q. Percutaneous kyphoplasty for osteoporotic vertebral compression fractures via unilateral versus bilateral approach: a meta-analysis. J Clin Neurosci. 2019;59:146–54.
Sun H, Li C. Comparison of unilateral and bilateral percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2016;11(1):156.
Zhang L, Liu Z, Wang J, Feng X, Yang J, Tao Y, Zhang S. Unipedicular versus bipedicular percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a prospective randomized study. Bmc Musculoskel Dis. 2015;16:145.
Gao T, Chen ZY, Li T, Lin X, Hu HG, Wang XY, Zeng J, Wu C. The significance of the best puncture side bone cement/vertebral volume ratio to prevent paravertebral vein leakage of bone cement during vertebroplasty: a retrospective study. Bmc Musculoskel Dis. 2023;24(1):470.
Liu J, Tang J, Zhang Y, Gu ZC, Yu SH. Percutaneous vertebral augmentation for osteoporotic vertebral Compression fracture in the midthoracic vertebrae (T5-8): a retrospective study of 101 patients with 111 fractured segments. World Neurosurg. 2019;122:e1381–7.
Saad A, Botchu R, James S. The Rates of Cement Leakage following Vertebroplasty in Osteoporotic versus Metastatic Disease. Indian J Radiol Imag. 2022;32(1):46–50.
Zhao Z, Qin D, Zhao W. Asymptomatic cement leakage into inferior vena cava. Qjm-Int J Med. 2022;115(1):49–50.
Franco E, Frea S, Solaro C, Conti V, Pinneri F. Fatal pulmonary embolism: when the cause is not a thrombus. Spine. 2012;37(6):E411–3.
Shi X, Li P, Li J, Bao C, Xiang J, Lu Y. Comparative evaluation of an innovative deflectable percutaneous kyphoplasty versus conventional bilateral percutaneous kyphoplasty for osteoporotic vertebral compression fractures: a prospective, randomized and controlled trial. Spine J. 2023;23(4):585–98.
Liu Y, Liu J, Suvithayasiri S, Han I, Kim JS. Comparative efficacy of Surgical interventions for Osteoporotic Vertebral Compression fractures: a systematic review and network Meta-analysis. Neurospine. 2023;20(4):1142–58.
Zhang Y, Chen X, Ji J, Xu Z, Sun H, Dong L, Hao D. Comparison of unilateral and bilateral percutaneous kyphoplasty for bone cement distribution and clinical efficacy: an analysis using three-Dimensional computed tomography images. Pain Physician. 2022;25(6):E805–13.
Zhu D, Hu J, Wang L, Zhu J, Ma S, Liu B. A comparison between modified unilateral extrapedicular and bilateral Transpedicular Percutaneous Kyphoplasty in the treatment of lumbar osteoporotic vertebral Compression fracture. World Neurosurg. 2022;166:e99–108.
Wang YF, Shen J, Li SY, Yu X, Zou TM. Kambin triangle approach in percutaneous vertebroplasty for the treatment of osteoporotic vertebral compression fractures. Medicine. 2019;98(44):e17857.
Hong H, Li J, Ding H, Deng Y, Deng Z, Jiang Q. Unilaterally extrapedicular versus transpedicular kyphoplasty in treating osteoporotic lumbar fractures: a randomized controlled study. J Orthop Surg Res. 2023;18(1):801.
Heo DH, Cho YJ. Segmental artery injury following percutaneous vertebroplasty using extrapedicular approach. J Korean Neurosurg S. 2011;49(2):131–3.
Biafora SJ, Mardjetko SM, Butler JP, Mccarthy PL, Gleason TF. Arterial injury following percutaneous vertebral augmentation: a case report. Spine. 2006;31(3):E84–7.
Wang Z, Yang Y. Application of 3D Printing in Implantable Medical devices. Biomed Res Int. 2021;2021:6653967.
Wang D, Han L, Xu G, Zhang W, Li H, Xu C, Li H, Li J, Zhang H, Li J. 3D Printing and computer-aided design for Precision Osteotomy-aided modules in bone biomechanical study. Int J Bioprinting. 2022;8(4):607.
Kang HW, Lee SJ, Ko IK, Kengla C, Yoo JJ, Atala A. A 3D bioprinting system to produce human-scale tissue constructs with structural integrity. Nat Biotechnol. 2016;34(3):312–9.
Zhou W, Xia T, Liu Y, Cao F, Liu M, Liu J, Mi B, Hu L, Xiong Y, Liu G. Comparative study of sacroiliac screw placement guided by 3D-printed template technology and X-ray fluoroscopy. Arch Orthop Traum Su. 2020;140(1):11–7.
Guo F, Dai J, Zhang J, Ma Y, Zhu G, Shen J, Niu G. Individualized 3D printing navigation template for pedicle screw fixation in upper cervical spine. PLoS ONE. 2017;12(2):e171509.
Pijpker P, Kraeima J, Witjes M, Oterdoom D, Vergeer RA, Coppes MH, Groen R, Kuijlen J. Accuracy of patient-specific 3D-Printed Drill guides for pedicle and lateral Mass Screw insertion: an analysis of 76 cervical and thoracic screw trajectories. Spine. 2021;46(3):160–8.
Acknowledgements
Not applicable.
Funding
This study was supported by Zigong Key Science and Technology Program, Zigong Institute of Medical Big Data and Artificial Intelligence Collaborative Innovation Projects (2022zcygy18).
Author information
Authors and Affiliations
Contributions
Xu Lin and Zhi-Yu Chen analyzed and interpreted the patient data regarding the OVCF. Tao Gao were major contributors in writing the manuscript. Hai-Gang Hu and Chao Wu complete the operation. Tao Li, Sheng-Yu Wan and Jian-Dong Tang assisted with data collection. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The experimental protocol was established, according to the ethical guidelines of the Helsinki Declaration and was approved by the Human Ethics Committee of Zigong Fourth People’s Hospital. Written informed consent was obtained from individual or guardian participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it.The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Gao, T., Wan, SY., Chen, ZY. et al. Clinical significance of modified unilateral puncture percutaneous vertebroplasty guided by 3D- printed guides in the treatment of osteoporotic vertebral compression fractures: a retrospective study. BMC Musculoskelet Disord 25, 656 (2024). https://doi.org/10.1186/s12891-024-07750-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07750-1