Abstract
Background
Rheumatoid arthritis (RA) is often preceded by symptomatic phases during which classification criteria are not fulfilled. The health burden of these “at-risk” stages is not well described. This study assessed health-related quality of life (HRQoL), function, fatigue and depression in newly presenting patients with clinically suspect arthralgia (CSA), unclassified arthritis (UA) or RA.
Methods
Cross-sectional analysis of baseline Patient-Reported Outcome Measures (PROMs) was conducted in patients from the Birmingham Early Arthritis Cohort. HRQoL, function, depression and fatigue at presentation were assessed using EQ-5D, HAQ-DI, PHQ-9 and FACIT-F. PROMs were compared across CSA, UA and RA and with population averages from the HSE with descriptive statistics. Multivariate linear regression assessed associations between PROMs and clinical and sociodemographic variables.
Results
Of 838 patients included in the analysis, 484 had RA, 200 had CSA and 154 had UA. Patients with RA reported worse outcomes for all PROMs than those with CSA or UA. However, “mean EQ-5D utilities were 0.65 (95%CI: 0.61 to 0.69) in CSA, 0.61 (0.56 to 0.66) in UA and 0.47 (0.44 to 0.50) in RA, which was lower than in general and older (≥ 65 years) background populations.” In patients with CSA or UA, HRQoL was comparable to chronic conditions such as heart failure, severe COPD or mild angina. Higher BMI and older age (≥ 60 years) predicted worse depression (PHQ-9: -2.47 (-3.85 to -1.09), P < 0.001) and fatigue (FACIT-F: 5.05 (2.37 to 7.73), P < 0.001). Women were more likely to report worse function (HAQ-DI: 0.13 (0.03 to 0.21), P = 0.01) and fatigue (FACIT-F: -3.64 (-5.59 to -1.70), P < 0.001), and residents of more deprived areas experienced decreased function (HAQ-DI: 0.23 (0.10 to 0.36), P = 0.001), greater depression (PHQ-9: 1.89 (0.59 to 3.18), P = 0.004) and fatigue (FACIT-F: -2.60 (-5.11 to 0.09), P = 0.04). After adjustments for confounding factors, diagnostic category was not associated with PROMs, but disease activity and polypharmacy were associated with poorer performance across all PROMs.
Conclusions
Patient-reported outcomes were associated with disease activity and sociodemographic characteristics. Patients presenting with RA reported a higher health burden than those with CSA or UA, however HRQoL in the pre-RA groups was significantly lower than population averages.
Key messages
The development of RA is often preceded by symptomatic phases in which patients do not yet fulfil classification criteria for RA. This study confirms a significant negative impact of symptoms on patient functioning and health-related quality of life in those newly presenting with clinically suspect arthralgia, unclassified arthritis, and RA. Patient burden was associated with measures of disease activity and patient characteristics, and was comparable to serious conditions such as angina, chronic obstructive pulmonary disease and heart failure. Further studies are needed to establish if patients in symptomatic at risk of RA phases may benefit from pharmacological and non-pharmacological interventions to reduce symptom impact and improve quality of life.
Similar content being viewed by others
Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory joint disease characterised by synovitis, joint destruction, disability, comorbidity and reduced life expectancy [1]. It has a prevalence of 0.5-1% in the UK population and is 2–4 times more common in women than men [2].
RA can be preceded by phases in which patients have inflammatory joint symptoms (with or without clinically apparent synovial swelling) but during which they do not yet fulfil classification criteria for RA. These phases include clinically suspect arthralgia (CSA, symptoms associated with inflammatory arthritis but without clinically apparent synovitis) [3], and unclassified arthritis (UA, clinically apparent synovitis not yet fulfilling criteria for RA or other classifiable forms of arthritis).
Early treatment of RA improves clinical outcomes, including disease activity measures and joint damage [4] and is a key element of treatment guidelines [5]. The stages of disease preceding the development of classifiable RA (also referred to as ‘at-risk’ phases) [6] similarly present opportunities for therapeutic intervention [7, 8]. Most studies assessing the impact of interventions in these ‘at-risk’ phases have assessed impacts on progression to RA. However, interventions in at-risk phases may also benefit patients by modifying risk factors and/or improving symptoms [9].
In order to understand the scope for intervention in symptomatic at-risk phases, it is important to gain a comprehensive understanding of the impact of early symptoms on functioning and quality of life. Subjective perceptions of health status can be captured via patient-reported outcome measures (PROMs), which can quantify symptoms, functional ability and general health status. The impact of RA on PROMs is well understood, and PROMs are included in the core set of measures for RA clinical trials [10, 11]. However, the extent to which PROMs are impacted in pre-RA phases is less clear. Therefore, the aims of this study were (i) to compare PROM scores across patients newly presenting with CSA, UA or RA; (ii) to compare HRQoL reported by patients in these groups with population averages; and (iii) to identify demographic and clinical factors associated with function, HRQoL, fatigue and depression in these patients.
Methods
Patient population
This is a cross-sectional analysis of baseline data from the Birmingham Early Arthritis Cohort (BEACON). BEACON recruits adult patients (≥ 18 years) who are naïve to conventional synthetic disease-modifying anti-rheumatic drug (DMARD) therapy and present with either clinically apparent synovitis of ≥ 1 joint or symptoms suggestive of inflammatory arthritis (e.g., morning stiffness, peripheral joint pain, a history of previous joint swelling) in the absence of clinically apparent joint swelling. Patients with symptoms solely due to degenerative joint disease are excluded. Participants are recruited from Sandwell and West Birmingham NHS Trust (SWB), University Hospitals Birmingham NHS Foundation Trust (UHB), and the Modality Partnership. Ethical approval was obtained from the West Midlands – Black Country Research Ethics Committee (Ref 12/WM/0258) and all participants gave written informed consent.
A diagnosis was assigned to each participant following their initial clinical assessment. The current analysis included participants with a diagnosis of CSA, UA or RA between 2013 and 2020. Diagnosis of RA required fulfilment of 1987 ACR criteria [12] or 2010 ACR/ EULAR criteria [13]; a diagnosis of CSA was applied where patients presented with symptoms which, in the opinion of a consultant rheumatologist, were suggestive of inflammatory arthralgia at risk of the development of RA (e.g., morning stiffness, peripheral joint pain, a history of previous joint swelling) in the absence of clinically apparent joint swelling [3]. Patients with UA had clinically apparent synovitis at initial assessment but did not fulfil classification criteria for another inflammatory condition (e.g. RA, psoriatic arthritis, spondyloarthritis, systemic lupus erythematosus, gout, pseudogout, reactive arthritis). Patients with other forms of arthritis or who provided no PROMs assessment were excluded from this analysis. The objectives of the analysis were determined in collaboration with three patient research partners with a diagnosis of RA who reviewed a description of the cohort, the items included in the PROMs, a summary of the data available and a list of potential analytic approaches.
Demographics and clinical assessment
Data collected at the initial assessment included clinical observations, laboratory findings, demographic data, current medication, and PROMs. Body mass index (BMI) was calculated from weight (kg) and height (m) and was categorised as: underweight and normal weight (< 25 kg/m2), overweight (25–30) and obese (≥ 30). Age was categorised into 18–39, 40–49, 50–59, and ≥ 60 years old. For this analysis, ethnicity data were classified as White, Asian, and other, reflecting the major ethnic groups in the area. Smoking status was categorised as current smoker, previous smoker and never smoker. Based on the patient’s residence address, a value of the quintile of the Index of Multiple Deprivation (IMD) [14] was assigned, with a larger number indicating a lower level of deprivation. The middle category (3rd quintile of IMD), reflecting average levels of deprivation, was used as a reference for the linear regression analysis.
Antibody status was recorded as positive if either rheumatoid factor (RF) or anti-cyclic citrullinated peptide (anti-CCP) antibodies were present at the time of first assessment. The Disease Activity Score 28 (DAS-28) was calculated using the C-reactive protein (CRP) formula [15] and categorised as remission (< 2.6), low (≥ 2.6 to < 3.2), moderate (> 3.2 to ≤ 5.1), and high (> 5.1) disease activity [16]. The number of medications used was stratified into < 5 and ≥ 5, based on the most commonly applied definition of polypharmacy [17]. Over-the-counter, topical, herbal, homoeopathic and non-prescribed supplements were excluded.
Patient reported outcome measures
Study participants completed a range of PROMs at the baseline visit:
HAQ-DI
The Stanford Health Assessment Questionnaire Disability Index (HAQ-DI) was specifically developed for the assessment of disability in patients with RA. Patients report the level of difficulty they have in performing certain activities in each of eight functional domains. A Likert scale is used, ranging from 0 (no difficulty) up to 3 (cannot be done at all). Additional scores reflect the use of aids and devices. The final score is the mean of scores of all categories with a range between 0 (best state) and 3 (worst state). HAQ-DI is not computed if the patient did not have scores for at least six categories. HAQ-DI has been shown to be reliable and valid in different languages and contexts [18, 19].
EQ-5D
Health-Related Quality of Life (HRQoL) data were collected using EQ-5D, a standardised instrument measuring generic health status. EQ-5D comprises two distinct self-report elements: (i) the health profile: a patient’s self-reported health status on five health dimensions (mobility, self-care, usual activities, pain and anxiety), and (ii) EQ-VAS: a patient’s rating of overall health on a scale from 0 (worst possible) to 100 (best possible health). It is accompanied by a ‘value set’ (also known as ‘utilities’) which reflects the preferences of the general public in a specific population [20]. Utilities can have values from 1 (best health) through 0 (state of health equivalent to death) to the worst state imaginable, which is represented by negative values as it is perceived as a state worse than death.
EQ-5D data were initially collected in the cohort using a 3-level instrument (EQ-5D-3L). This was subsequently replaced by a 5-level instrument (EQ-5D-5L), resulting in approximately a third of the cohort data being assessed with the later version. For the combined analysis, the 5-level data were mapped into the original 3-level utility values [21, 22].
PHQ-9
Depression was measured with Patient Health Questionnaire-9 (PHQ-9), a unidimensional depression scale derived from PHQ [23]. A review of the instrument in general, medical, diverse, and rheumatological populations revealed good reliability [24]. It consists of nine items, each of which is scored 0 to 3, indicating the degree of severity (0 - not at all, 1 - several days, 2 - more than half of the days, or 3 - nearly every day), providing a 0 to 27 severity score. To assess the prevalence of depression, PHQ-9 scores were grouped as 0–4 no depression, 5–9 mild depression, and ≥ 10 moderate to severe depression [23].
FACIT-F
Evaluation of fatigue in arthritis patients was endorsed by the Outcome Measures in Rheumatology consortium [25]. Fatigue was measured using a unidimensional scale, Functional Assessment of Chronic Illness Therapy – Fatigue (FACIT-F), originally developed for oncology patients with anaemia but subsequently used across a range of chronic illnesses [26]. The measurement covers physical, functional and emotional fatigue as well as social consequences of fatigue. FACIT-F consists of 13 questions rated on a scale of 0–4 (0 – Not at all, 1 – A little bit, 2 – Somewhat, 3 – Quite a bit, 4 – Very much). The final score ranges from 0 to 52, with scores for each of the answers calculated according to the FACIT-F-specific algorithm. When there are missing data, prorating formula ([Sum of item scores] x [N of items] / [N of items answered]) is used as long as more than 50% of the items are answered. Higher scores indicate a lower level of fatigue [27].
Statistical analysis
Descriptive statistical analyses were performed on complete case data, defined as data available to perform each individual analysis. Continuous data were presented as means and 95% confidence intervals (CI), and categorical data as counts and proportions. Univariate subgroup analyses were performed using t-tests when two groups were compared and ANOVA when there were three or more categories. Post-hoc analysis comparing multiple categories pairwise was conducted applying Bonferroni correction. The correlations between the PROMs of interest were explored by calculating Pearson product-moment correlation coefficient.
A comparison of the HRQoL of diagnostic subgroups with other populations was visualised with a forest plot. The comparison groups encompassed general population data from the Health Survey for England (2017) and subgroups of participants aged 65 years or older and with other common chronic diseases, namely chronic obstructive pulmonary disease (COPD: mild and severe) [28], angina (mild and severe) [29] and heart failure [30].
The univariate analysis was performed independently for each PROM for all factor variables of interest. Variables with P > 0.1 were removed from the multivariable model in a backward selection approach, except for diagnosis, which was the variable of interest. The selection of dependent variables was assessed with the likelihood ratio test. Next, the multivariate multiple linear regression model, simultaneously accounting for the correlations between the PROMs, was built using significant variables in at least one of the multivariable models. All analyses were performed using Stata 16.1 (StataCorp LLC, USA). Statistical significance was assumed where P < 0.05.
Results
898 patients in the BEACON cohort had a baseline diagnosis of CSA, UA or RA. Sixty of these patients were excluded as they did not have any PROM data recorded at baseline. The characteristics of excluded patients were largely similar than that of the remaining in the cohort, except for some differences in ethnicity, BMI and diagnosis (Supplementary File, Table 1). The final study group consisted of 838 DMARD-naïve patients diagnosed with either CSA, UA or RA, further reduced in individual analyses due to missing or incomplete outcome data – by 13 (1.5%) in HAQ-DI, 118 (14.1%) in EQ-5D, 26 (3.1%) in FACIT-F and 8 (1.0%) in PHQ-9. Missingness in HAQ-DI, FACIT-F and PHQ-9, ranging between 1 and 3.1%, was assumed unsubstantial. Comparison of patient characteristics with and without valid EQ-5D utilities showed no significant differences between the subgroups (Supplementary File, Table 2).
Demographic and clinical characteristics with respect to diagnosis
The demographic and clinical characteristics of the study group are presented in Table 1. Patients in at-risk of RA stages constituted nearly half of the study group (23.9% [n = 200] with CSA and 18.4% [n = 154] with UA); the remaining patients had RA (57.8%, n = 484). There were twice as many women as men, and 66.2% were White. 45.3% of patients were living in the areas of the first quintile of IMD (i.e. of highest deprivation). Nearly half never smoked (48.0%), and 22.9% were regularly taking five or more medications.
As expected, diagnostic subgroups differed in the level of disease activity. Over a third of patients with CSA were in DAS-28 remission, while this was the case only in 2.9% of patients with RA. Similarly, only three patients with CSA had a DAS-28 score of > 5.1, whilst nearly a half of those with RA did. There were also significant differences in the proportions of patients with positive antibodies, on polypharmacy and across the categories of duration of symptoms (Table 1).
Health state assessment by diagnosis
On average, patients with RA had lower functional status, HRQoL, and worse fatigue and depression than those with CSA or UA. Table 2 presents the mean values of all four PROM measures across the diagnostic groups. There were statistically significant differences between the means, with the RA group consistently having worse outcomes than both CSA and UA groups for all four PROMs (P < 0.001 for any pairwise comparison with the RA group), while there were no significant differences between CSA and UA. The prevalence of moderate-to-severe depression was 48% for patients with RA, 32% for those with CSA, and 27% for those with UA.
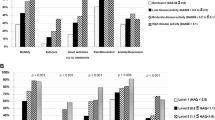
To give context to the HRQoL burden in patients at risk of, or with newly presenting RA, the mean EQ-5D scores in diagnostic groups were compared with the general population and other long-term conditions (Fig. 1). HRQoL across all diagnoses was significantly lower for this cohort than in the Health Survey for England (HSE) population as a total or in a subgroup of participants aged over 65 years. HRQoL in patients with CSA and UA was greater than in those with RA or severe angina and was comparable to patients diagnosed with severe COPD, mild angina or heart failure.
Comparison of Health-Related Quality of Life (HRQoL) expressed as EQ-5D score. Blue triangle: mean EQ-5D in the study diagnostic subgroups; blue circles: mean EQ-5D in the background general and condition-specific populations. Whiskers represent 95% confidence intervals. CSA: clinically suspect arthralgia, HSE: Health Survey for England, COPD: chronic obstructive pulmonary disease
Associations of the severity of outcomes with clinical and demographic factors
Multivariate analyses were conducted to assess the associations between PROMs (disability, HRQoL, depression and fatigue) with clinical and demographic characteristics; the final model is presented in Table 3. Increased functional disability was associated with female sex, older age, obesity, living in areas with lower quintiles of social deprivation, increased disease activity and polypharmacy. HRQoL was associated with increased disease activity and polypharmacy. The severity of depression (PHQ-9) increased with older age, increasing BMI, living in areas with the lowest quintile of social deprivation, increased disease activity and polypharmacy. Fatigue (FACIT-F) was associated with the female sex, increasing BMI, disease activity and polypharmacy. After adjusting for the demographic and clinical factors, the diagnosis assigned at baseline did not affect any of the studied PROMs. Antibody status, smoking, ethnicity, and duration of symptoms were removed from the model as redundant variables.
There were significant differences in the distribution of DAS-28 between the diagnostic groups (Table 1). Figure 2 illustrates the interplay between the diagnosis, disease activity and the studied PROMs. It presents the values of each PROM across all three diagnoses in the DAS-28 strata. In line with the regression model, physical functioning, HRQoL, depression and fatigue were not affected by the diagnosis but varied between DAS-28 states.
Discussion
This study explores functional impairment (HAQ-DI), health-related quality of life (EQ-5D), depression (PHQ-9), and fatigue (FACIT-F) in patients with CSA and UA, constituting “at-risk” phases of RA, and in patients with newly presenting RA [3]. All disease stages were associated with major negative impacts on patients’ function and well-being, with RA associated with worse scores for all studied PROMs. Comparison of HRQoL with national survey averages revealed significant impairment across all diagnostic subgroups. In CSA and UA, HRQoL was comparable to multiple serious chronic conditions, including severe COPD, mild angina, or heart failure. Patients with RA at initial presentation reported HRQoL comparable to severe angina.
Despite reports of a range of symptoms in the phases preceding RA development [31, 32], there are limited examples of assessments using PROMs in these groups. The extent of functional disability identified in the present study aligns with that found in a longitudinal study of patients with CSA [33]. Interestingly, in those CSA patients who progressed to develop clinical arthritis within a year of follow-up, HAQ scores did not increase between presentation with CSA and arthritis development [34]. A previous study in the Netherlands also reported similar levels of patient burden for CSA as for RA [35].
The relationship between RA status and depression has been shown to be bidirectional: patients with RA are at increased risk of depression, and the incidence of RA is higher in depressed than non-depressed individuals [36]. In patients with early RA, persistent depression and anxiety were also linked with poorer health outcomes over time and reduced treatment response [37]. However, the prevalence of depression has not been well studied in the phases preceding clinically apparent RA. Our findings indicate a significant burden of depression in both CSA and UA patients reflecting an unmet need.
Fatigue is an important feature of inflammatory arthritis and is often described by those affected as one of their most troublesome symptoms [38]. While fatigue is well recognised in RA, it has not been well studied in CSA and UA. The levels of fatigue reported by patients diagnosed with CSA, UA and RA in this study were higher than normative values for the general population [39], indicating increased fatigue in all three diagnostic groups. CSA and UA scores corresponded to the 10–13 percentile of normative data, and RA scores corresponded to the 7–8 percentile, demonstrating that fatigue in pre-RA stages is only slightly less burdensome than in clinically established RA.
Our analysis shows that, on an individual level, patient function and well-being were not associated with baseline diagnosis per se but were strongly affected by disease activity, polypharmacy, obesity and demographic characteristics, including sex, older age, and social status. BMI and, to a lesser degree, social status are modifiable factors affecting patients’ function and well-being. The findings confirm the results of previous studies reporting that unhealthy weight may further exacerbate mental and physical impairments associated with arthralgia or arthritis [40, 41]. Moreover, obesity has also been linked to worse disease activity over follow-up [42,43,44]. Our data raise the possibility that management of obesity and increased social support in the preclinical stages of the condition may be associated with improved health and well-being.
Our analysis of this large representative sample provides rich insight into important health inequalities. Living in the most deprived areas was associated with a worse functional state and severity of depression but not with overall HRQoL or fatigue. This complements the recent findings of the association of sociodemographic factors with worse disease activity in RA, independently of clinical measures [45]. Research from other countries [46, 47] also links low socioeconomic status with worse PROMs at baseline in patients with early inflammatory arthritis. The inter-relationships between the variables studies in this analysis are consistent with biopsychosocial models of health and disease.
Our study shows that decreased functional status and compromised health outcomes are reported in individuals at risk of RA. Studies of pharmacological intervention in the at-risk stages should therefore assess the impact of the intervention on these important patient-reported outcomes. Furthermore, non-pharmacological approaches, including self-management strategies, are widely recognised in treating patients with RA [48], improving a range of PROMs. The impact of such approaches on patients with CSA and UA also needs to be investigated.
Strengths and limitations
The main strength of this study is the broad range of validated PROMs, all endorsed by the American College of Rheumatology for use in patients with rheumatic diseases [24, 26, 49, 50], looking at different aspects of patients’ health. The large sample size allowed for complex analysis with high external validity; the sample is socially and demographically diverse and from a cohort with broad inclusion criteria recruited from a diverse catchment area of over 1 million people. Our study includes three major groups often seen in new patient clinics and has important clinical implications, providing insight into often overlooked hidden disabilities, especially in those with CSA where there is no joint swelling and the results of laboratory investigations and imaging may be normal.
Limitations include the recruitment of CSA patients based on clinical opinion. The more recently published set of observations formalising the diagnosis of CSA [3] could not be formally applied as many patients were recruited before these criteria were published and not all relevant variables were collected prior to the point at which the criteria were published. Furthermore, in this cross-sectional analysis, we are unable to relate patient-reported burden at baseline to disease status at follow-up. It should also be noted that causal relationships cannot be inferred from the observed associations.
Conclusions
Across clinically apparent at-risk stages of RA and in newly presenting RA, patients experience a considerable health burden. Patient-reported function, HRQoL, depression and fatigue were associated with disease activity, polypharmacy, obesity, and demographic factors such as sex, older age and deprivation.
Data availability
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
References
Myasoedova E, Davis JM, Crowson CS, Gabriel SE. Epidemiology of rheumatoid arthritis: rheumatoid arthritis and mortality. Curr Rheumatol Rep. 2010;12(5):379–85.
Safiri S, Kolahi AA, Hoy D, Smith E, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of rheumatoid arthritis 1990–2017: a systematic analysis of the Global Burden of Disease study 2017. Ann Rheum Dis. 2019;78(11):1463–71.
van Steenbergen HW, Aletaha D, Beaart-van de Voorde LJJ, Brouwer E, Codreanu C, Combe B, et al. EULAR definition of arthralgia suspicious for progression to rheumatoid arthritis. Ann Rheum Dis. 2017;76(3):491–6.
van Nies JA, Krabben A, Schoones JW, Huizinga TW, Kloppenburg M, van der Helm-van Mil AH. What is the evidence for the presence of a therapeutic window of opportunity in rheumatoid arthritis? A systematic literature review. Ann Rheum Dis. 2014;73(5):861–70.
Smolen JS, Landewé RBM, Bijlsma JWJ, Burmester GR, Dougados M, Kerschbaumer A, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79(6):685–99.
Gerlag DM, Raza K, van Baarsen LGM, Brouwer E, Buckley CD, Burmester GR, et al. EULAR recommendations for terminology and research in individuals at risk of rheumatoid arthritis: report from the Study Group for Risk factors for rheumatoid arthritis. Ann Rheum Dis. 2012;71(5):638–41.
Stanway JA, Isaacs JD. Tolerance-inducing medicines in autoimmunity: rheumatology and beyond. Lancet Rheumatol. 2020;2(9):e565–75.
Raza K, Klareskog L, Holers VM. Predicting and preventing the development of rheumatoid arthritis. Rheumatology. 2015;55(1):1–3.
Mankia K, Siddle HJ, Kerschbaumer A, Alpizar Rodriguez D, Catrina AI, Cañete JD, et al. EULAR points to consider for conducting clinical trials and observational studies in individuals at risk of rheumatoid arthritis. Ann Rheum Dis. 2021;80(10):1286–98.
Felson DT, Anderson JJ, Boers M, Bombardier C, Chernoff M, Fried B, et al. The American College of Rheumatology preliminary core set of disease activity measures for rheumatoid arthritis clinical trials. The Committee on Outcome measures in Rheumatoid Arthritis clinical trials. Arthritis Rheum. 1993;36(6):729–40.
Kirwan JR, Minnock P, Adebajo A, Bresnhan B, Choy E, de Wit M, et al. Patient perspective: fatigue as a recommended patient centered outcome measure in rheumatoid arthritis. J Rheumatol. 2007;34(5):1174–7.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. 1988;31(3):315–24.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3, et al. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League against Rheumatism collaborative initiative. Arthritis Rheum. 2010;62(9):2569–81.
Ministry of Housing Communities & Local Government. English indices of deprivation 2019. [13/12/2022]. https://assets.publishing.service.gov.uk/.
Wells G, Becker JC, Teng J, Dougados M, Schiff M, Smolen J, et al. Validation of the 28-joint disease activity score (DAS28) and European League against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann Rheum Dis. 2009;68(6):954–60.
Singh JA, Furst DE, Bharat A, Curtis JR, Kavanaugh AF, Kremer JM, et al. 2012 update of the 2008 American College of Rheumatology Recommendations for the Use of Disease-modifying antirheumatic drugs and Biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res. 2012;64(5):625–39.
Bechman K, Clarke BD, Rutherford AI, Yates M, Nikiphorou E, Molokhia M, et al. Polypharmacy is associated with treatment response and serious adverse events: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatol (United Kingdom). 2019;58(10):1767–76.
Bruce B, Fries JF. The Stanford Health Assessment Questionnaire: dimensions and practical applications. Health Qual Life Outcomes. 2003;1:20.
Stanford University School of Medicine. The Health Assessment Questionnaire. 13/05/2020]. http://www.chcr.brown.edu/pcoc/ehaqdescrscoringhaq372.pdf.
Maheswaran H, Petrou S, Rees K, Stranges S. Estimating EQ-5D utility values for major health behavioural risk factors in England. J Epidemiol Commun Health. 2013;67(2):172–80.
National Institute for Health and Care Excellence. Position statement on use of the EQ-5D-5L value set for England (updated October 2019) [Accessed: 27/12/2020]. https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/technology-appraisal-guidance/eq-5d-5l.
van Hout B, Janssen MF, Feng Y-S, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–15.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13.
Smarr KL, Keefer AL. Measures of Depression and depressive symptoms. Arthritis Care Res. 2020;72(S10):608–29.
Kirwan JR, Hewlett SE, Heiberg T, Hughes RA, Carr M, Hehir M, et al. Incorporating the patient perspective into outcome assessment in rheumatoid arthritis–progress at OMERACT 7. J Rheumatol. 2005;32(11):2250–6.
Elera-Fitzcarrald C, Rocha J, Burgos PI, Ugarte-Gil MF, Petri M, Alarcón GS. Measures of fatigue in patients with rheumatic diseases: a critical review. Arthritis Care Res. 2020;72(S10):369–409.
FACIT [14/05/2020]. https://www.facit.org/.
Pickard AS, Wilke C, Jung E, Patel S, Stavem K, Lee TA. Use of a preference-based measure of health (EQ-5D) in COPD and asthma. Respir Med. 2008;102(4):519–36.
Dyer MTD, Goldsmith KA, Sharples LS, Buxton MJ. A review of health utilities using the EQ-5D in studies of cardiovascular disease. Health Qual Life Outcomes. 2010;8(1):13.
Calvert MJ, Freemantle N, Cleland JGF. The impact of chronic heart failure on health-related quality of life data acquired in the baseline phase of the CARE-HF study. Eur J Heart Fail. 2005;7(2):243–51.
Stack RJ, van Tuyl LH, Sloots M, van de Stadt LA, Hoogland W, Maat B, et al. Symptom complexes in patients with seropositive arthralgia and in patients newly diagnosed with rheumatoid arthritis: a qualitative exploration of symptom development. Rheumatology (Oxford). 2014;53(9):1646–53.
van Tuyl LH, Stack RJ, Sloots M, van de Stadt LA, Hoogland W, Maat B, et al. Impact of symptoms on Daily Life in people at risk of rheumatoid arthritis. Musculoskelet Care. 2016;14(3):169–73.
ten Brinck RM, van Steenbergen HW, Mangnus L, Burgers LE, Reijnierse M, Huizinga TW, et al. Functional limitations in the phase of clinically suspect arthralgia are as serious as in early clinical arthritis; a longitudinal study. RMD Open. 2017;3(1):e000419.
ten Brinck RM, van Steenbergen HW, Mangnus L, Burgers LE, Reijnierse M, Huizinga TWJ, et al. Functional limitations in the phase of clinically suspect arthralgia are as serious as in early clinical arthritis; a longitudinal study. RMD Open. 2017;3(1):7.
Kuijper TM, Luime JJ, Alves C, Barendregt PJ, van Zeben J, Bindels PJ, et al. Quality of life and health care use in patients with arthralgias without synovitis compared with patients diagnosed with early rheumatoid arthritis: data from an early arthritis cohort. Arthritis Care Res (Hoboken). 2014;66(3):379–86.
Lu MC, Guo HR, Lin MC, Livneh H, Lai NS, Tsai TY. Bidirectional associations between rheumatoid arthritis and depression: a nationwide longitudinal study. Sci Rep. 2016;6:20647.
Matcham F, Norton S, Scott DL, Steer S, Hotopf M. Symptoms of depression and anxiety predict treatment response and long-term physical health outcomes in rheumatoid arthritis: secondary analysis of a randomized controlled trial. Rheumatology (Oxford). 2016;55(2):268–78.
Dures E, Cramp F, Hackett K, Primdahl J. Fatigue in inflammatory arthritis. Best Pract Res Clin Rheumatol. 2020;34(2):101526.
Montan I, Löwe B, Cella D, Mehnert A, Hinz A. General Population norms for the Functional Assessment of Chronic Illness Therapy (FACIT)-Fatigue scale. Value Health. 2018;21(11):1313–21.
Schoffman DE, Wilcox S, Baruth M. Association of Body Mass Index with physical function and Health-Related Quality of Life in adults with arthritis. Arthritis. 2013;2013:190868.
García-Poma A, Segami MI, Mora CS, Ugarte MF, Terrazas HN, Rhor EA, et al. Obesity is independently associated with impaired quality of life in patients with rheumatoid arthritis. Clin Rheumatol. 2007;26(11):1831–5.
Nikiphorou E, Norton S, Young A, Dixey J, Walsh D, Helliwell H, et al. The association of obesity with disease activity, functional ability and quality of life in early rheumatoid arthritis: data from the Early Rheumatoid Arthritis Study/Early Rheumatoid Arthritis Network UK prospective cohorts. Rheumatology. 2018;57(7):1194–202.
Thomas K, Lazarini A, Kaltsonoudis E, Drosos A, Papalopoulos I, Sidiropoulos P et al. Treatment patterns and achievement of the treat-to-target goals in a real-life rheumatoid arthritis patient cohort: data from 1317 patients. Therapeutic Adv Musculoskelet Disease. 2020;12.
Brown Z, Metcalf R, Bednarz J, Spargo L, Lee A, Hill C, et al. Modifiable lifestyle factors Associated with response to treatment in early rheumatoid arthritis. Acr Open Rheumatol. 2020;2(6):371–7.
Busby AD, Wason J, Pratt AG, Young A, Isaacs JD, Nikiphorou E. The role of comorbidities alongside patient and disease characteristics in long-term disease activity in RA using UK inception cohort data. Rheumatology. 2022;61(11):4297–304.
Yang G, Bykerk VP, Boire G, Hitchon CA, Thorne JC, Tin D, et al. Does Socioeconomic Status affect outcomes in early inflammatory arthritis? Data from a Canadian Multisite suspected Rheumatoid Arthritis Inception Cohort. J Rheumatol. 2015;42(1):46–54.
Putrik P, Ramiro S, Chorus AM, Keszei AP, Boonen A. Socioeconomic inequities in perceived health among patients with musculoskeletal disorders compared with other chronic disorders: results from a cross-sectional Dutch study. RMD Open. 2015;1(1).
Marques A, Santos E, Nikiphorou E, Bosworth A, Carmona L. Effectiveness of self-management interventions in inflammatory arthritis: a systematic review informing the 2021 EULAR recommendations for the implementation of self-management strategies in patients with inflammatory arthritis. RMD Open. 2021;7(2).
Busija L, Ackerman IN, Haas R, Wallis J, Nolte S, Bentley S, et al. Adult Measures of General Health and Health-Related Quality of Life. Arthritis Care Res. 2020;72(S10):522–64.
Lane CY, Givens DL, Thoma LM. General Functional Status: common outcome measures for adults with Rheumatic Disease. Arthritis Care Res. 2020;72(S10):431–51.
Acknowledgements
We would like to thank patient research partners from the Rheumatology Research Patient Partnership (R2P2) at the University of Birmingham for their contribution to the study and continuous support.
Funding
No specific funding was received for this work, which was supported by the Research into Inflammatory Arthritis Centre Versus Arthritis (RACE) [grant number 22072]. KR, AF and MC are supported by the NIHR Birmingham Biomedical Research Centre.
Author information
Authors and Affiliations
Contributions
BT, KR, AF, MC, MF designed the study, contributed to, reviewed, and accepted the manuscript. BT analysed the data. KR, AF, BR, CMG, EJ, ER, GJ, IS, JT, NA, PP, RS, SB contributed to the design and or delivery of the BEACON cohort and recruited and followed up patients in the cohort including in relation to the collection of the data reported in this manuscript, reviewed, and accepted the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the West Midlands – Black Country Research Ethics Committee (Ref 12/WM/0258) and all participants gave written informed consent.
Consent for publication
Not Applicable.
Competing interests
Yes, the authors have competing interests as defined by BMC, or other interests that might be perceived to influence the results and/or discussion reported in this paper. “BR, EJ, ER, GJ, IS, JT, MF, NA, PP, RS, SB have no conflicts of interest to declare. BT receives funding from the National Institute for Health Research (NIHR). BT is also employed by Visible Analytics Ltd. KR declares personal fees from Abbvie and Sanofi and grant/research support from Bristol Myers Squibb, all outside the submitted work. AF declares personal fees from Abbvie, Roche and Janssen and grant/research support from Roche, UCB, Nascient, Mestag, GSK and Janssen, all outside the submitted work. CMG declares support for conference attendance from Eli Lilly. MC is Director of the Birmingham Health Partners Centre for Regulatory Science and Innovation, Director of the Centre for the Centre for Patient Reported Outcomes Research and is a National Institute for Health Research (NIHR) Senior Investigator. MC receives funding from NIHR, UK Research and Innovation (UKRI), NIHR Birmingham Biomedical Research Centre, the NIHR Surgical Reconstruction and Microbiology Research Centre and NIHR ARC West Midlands UK SPINE and Health Data Research UK at the at the University of Birmingham and University Hospitals Birmingham NHS Foundation Trust, NIHR/UKRI, Health Data Research UK, Innovate UK (part of UK Research and Innovation), Macmillan Cancer Support, UCB Pharma, Janssen, GSK and Gilead. MC has received personal fees from Astellas, Aparito Ltd, CIS Oncology, Takeda, Merck, Daiichi Sankyo, Glaukos, GSK and the Patient-Centered Outcomes Research Institute (PCORI) outside the submitted work. The views expressed in this article are those of the authors and not necessarily those of the NIHR, or the Department of Health and Social Care.”
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Torlinska, B., Raza, K., Filer, A. et al. Predictors of quality of life, functional status, depression and fatigue in early arthritis: comparison between clinically suspect arthralgia, unclassified arthritis and rheumatoid arthritis. BMC Musculoskelet Disord 25, 307 (2024). https://doi.org/10.1186/s12891-024-07446-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07446-6