Abstract
Purpose
To assess the clinical safety, accuracy, and efficacy of percutaneous kyphoplasty (PKP) surgery using an enhanced method of unilateral puncture on the convex side for the treatment of painful osteoporotic vertebral compression fractures (P-OVCF) with scoliosis.
Methods
Clinical and radiographic data of P-OVCF patients with scoliosis who underwent PKP via unilateral puncture on the convex side from January 2018 to December 2021 were retrospectively analyzed. This technique’s detailed surgical steps and tips were described. The local kyphosis angle (LKA), scoliosis Cobb angle (SCA), and local scoliosis Cobb angle (LSCA) were measured using X-ray and compared at pre-operation, post-operation, and the last follow-up. The width of pedicle (POW), inner inclination angle (IIA), lateral distance (LD), and puncture course length (PCL) were measured on the axial computed tomography image and compared between two sides. Postoperative computed tomography was employed to evaluate the condition of cement distribution and puncture. Clinical outcomes were evaluated using the Oswestry Disability Index (ODI) and Visual Analog Scale (VAS) for back pain (BP).
Results
Thirty-six patients, 23 women and 13 men, with an average age of 76.31 ± 6.28 years were monitored for 17.69 ± 4.70 months. The median surgical duration of single vertebrae was 35 min. The volume of bone cement for single vertebrae was 3.81 ± 0.87 ml and the proportion of sufficient cement distribution of the patients was 97.22. LKA was considerably improved from pre-operation to post-operation and sustained at the last follow-up. SCA and LSCA were not significantly modified between these three-time points. IIA, PCL, and LD were lower on the convex side than on the concave side. POW was considerably wider on the convex side. The ODI and VAS-BP scores were significantly improved after surgery and sustained during the follow-up.
Conclusions
Combining with the proper assessment of the pre-injured life status of patients, PKP surgery using unilateral puncture on the convex side for the treatment of P-OVCF with scoliosis can achieve safe, excellent clinical, and radiographic outcomes.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Percutaneous kyphoplasty (PKP), a minimally invasive operation, has been extensively used to treat painful osteoporotic vertebral compression fractures (P-OVCF) [1, 2] with lesser complications than percutaneous vertebroplasty [3, 4]. The key to a successful PKP surgery is a satisfactory puncture, which not only allows for symmetrical bone cement distribution but also helps to avoid complications [5, 6]. As technology has advanced, various intraoperative guiding methods for PKP puncture have been introduced, but PKP under C-arm fluoroscopy is still the most commonly used [7,8,9,10].
The unilateral puncture approach with less surgical time, cement consumption, a lower cement leakage ratio, and better short-term general health compared to bilateral puncture is recommended for PKP [10, 11]. The ideal target puncture point for a unilateral approach is thought to be in the vertebral body’s anterior one-third middle point [12, 13]. To make needles successfully reach the target point through the unilateral puncture, the proper inner inclination angle (IIA) and the distance from the puncture point to the midline in several puncture techniques were suggested in previous studies [13,14,15,16,17].
P-OVCF with scoliosis may have asymmetric vertebrae and pedicles in severely deformed and rotated spines, furthermore, the degeneration of facet joints, costotransverse joint, calcification shadow of costal cartilage and osteoporosis decrease the quality of intra-operation fluoroscopy to cause challenges for accurately located lesion vertebrae and puncture point. Although each technique has its inherent benefits, none guarantees safety and accuracy in this situation, and none is easily conducted by surgeons with little experience. Therefore, an accurate puncture for PKP is difficult for a rotated osteoporotic spine with asymmetric pedicles.
According to our knowledge, there was no research to describe a specific method to treat P-OVCF with scoliosis. Therefore, we presented an enhanced method of unilateral puncture on the convex side to conduct PKP surgery for the treatment of P-OVCF with scoliosis. This study seeks to describe and assess this method as to its clinical safety, accuracy, and efficacy.
Materials and methods
Study population and inclusion criteria
Between January 2018 and December 2021, 416 patients having P-OVCF who had PKP surgery in our department were regarded as a candidate for screening. Based on the following inclusion and exclusion criteria: (1) P-OVCF patients with scoliosis (P-OVCF was determined by typical clinical presentation and MRI demonstration; scoliosis was defined as the Cobb angle more than 10°); (2) the lesion vertebrae located in the curve of scoliosis; (3) using unilateral puncture on the convex side; (4) osteoporosis ( ≤ − 2.5 T-score measured using dual-energy X-ray bone mineral density scan);5) patients with complete medical records and radiographic data for more than 12 months;
Exclusion criteria: (1) patients with chronic mechanic back pain (BP) for more than 1 year (Visual Analog Scale [VAS] > 4); (2) patients with pathologic vertebral lesions including vertebral metastatic carcinoma, vertebral hemangioma, and myeloma; (3) patients with neurological deficits caused by spinal cord or nerve root compression. This retrospective study was authorized by Ethics Committee of the Affiliated Hospital of Southwest Medical University, and strictly followed the guidelines of the Declaration of Helsinki (No. KY2023024). All patients finally included in this study signed informed consent.
Surgical technique
The patient is kept in a prone position and routinely disinfected and the operation was conducted under general or local anesthesia. First, a C-arm fluoroscope is placed at the target vertebra for a poster-anterior (PA) image. The C-arm is gradually rotated until a true PA view of the rotated vertebral body is achieved and both pedicles are approximately symmetrically visualized (Fig. 1A–D). Once the symmetrical pedicle shadows are obtained, the C-arm is rotated in the sagittal plane to try to create a tangential view of both upper and lower endplates. The puncture point was selected at the skin location which ranged from 2.4 to 5.15 cm lateral to the midline on the convex side based on the target vertebrae level. The puncture was performed via a transverse process-pedicle approach [13], in the thoracic spine via the costotransverse joint. The IIA of puncture on the convex side was clearly lower than that on the concave side (Fig. 2). Based on the oval pedicle outline on intraoperative fluoroscopy, the entry points are determined at 9-o’clock and 3-o’clock positions on the left and right pedicles, respectively (Fig. 1D). When the needle tip reached the midpoint of the pedicle in the PA view, the C-arm position was changed to obtain a true lateral view. We can now observe and adjust the inclination angle of the sagittal view in the lateral view, as well as the IIA of the puncture. After making corresponding judgments and adjustments, the C-arm position was changed to obtain a true PA view. The puncture was continued until the needle tip reached the pedicle’s medial margin. The C-arm position was changed to obtain a true lateral view, and the puncture was considered ideal if the needle tip was located in the posterior one-fourth of the vertebral body. The guide wire was inserted to reach the anterior one-fourth of the vertebral body in lateral view and was at or crossed the midline in PA view (Fig. 1E, F). The expansion cannula, working cannula and inflatable balloon were inserted sequentially and expanded under fluoroscopy guidance. The prepared bone cement is slowly inserted and stopped as the cement reached the posterior one-sixth of the posterior wall of the vertebra [18]. After the bone cement penetrates and distributes well in the fractured vertebral body, the cannula is removed and the operation is finalized (Fig. 1G–J). All patients were given anti-osteoporosis medication after the operation and got out of bed on the day after the operation and were advised to avoid extreme physical strain for 3 months.
A, C-arm is gradually rotated until a true PA image of the rotated vertebral body is obtained and both pedicles are mostly symmetrically visualized en face; B, the X-ray of PA view at pre-operation; C, the intraoperative PA image revealed asymmetrical pedicle shadows (red arrows); D, C-arm position is modified and gradually rotated to obtain a true PA image of the rotated vertebral body and both pedicles are nearly symmetrical (red arrows); E and F, the guide wire was at or cross the midline in PA view (E) and reached the anterior one-fourth of the vertebral body at the lateral view (F); G and H, the final intraoperative PA (G) and lateral (H) images; I and J, the PA (I) and lateral (J) X-ray after surgery
A, a schematic diagram of standard unilateral puncture, in which IIA was 33.2° and the LD was 5.21 cm; B, the IIA of puncture on non-rotated vertebrae; C, a schematic diagram of unilateral puncture on rotated vertebrae, in which IIA was 1.1° on the convex side and 62.6° on the concave side, respectively; LD and PCL were lower on the convex side than the concave side; D, the C-arm was rotated, and the puncture was nearly vertical (IIA was 1.1°). T, target point; M, midpoint of the pedicle; PCL, puncture course length; PSPP, planned skin puncture point; LD, the lateral distance between PSPP and the spinous process; IIA, inner inclination angle
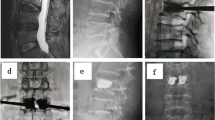
A representative case is shown in Fig. 3.
A and B, the X-ray of PA and lateral view at pre-operation; C, the intraoperative PA image revealed asymmetrical pedicle shadows; D, C-arm position is rotated and both pedicles are nearly symmetrical; E and F, the guide wire was at or cross the midline in PA view (E) and reached the anterior one-fourth of the vertebral body at the lateral view (F); G and H, the PA (G) and lateral (H) X-ray after surgery; I, the axial CT image revealed adequate cement distribution and the puncture track; J, the sagittal CT reconstruction image revealed the vertebral height and sufficient cement distribution
Evaluation methods and parameters
Clinical efficacy parameters
Patients’ subjective BP perception was evaluated by VAS. The patient’s quality of life was evaluated using Oswestry Disability Index (ODI) scores. These parameters were examined by two independent observers before surgery, 1 day after surgery, and at the final follow-up. Furthermore, as these OVCF patients with scoliosis and some had noticeable sagittal and or coronal imbalance of the whole spine, we further assessed the living quality before the acute BP onset and regarded it as a critical reference of our treatment goal.
Radiographic parameters
The X-ray was conducted before surgery, 1 day after surgery, and at the final follow-up. The local kyphosis angle (LKA) of the injured vertebral body in the lateral X-ray was measured to assess the extent of vertebral damage and restoration and its improvement after surgery. LKA was the angle formed by lines drawn parallel to the upper endplate of the upper adjacent vertebrae and the lower endplate of the lower adjacent vertebrae. The scoliosis Cobb angle (SCA) and the local scoliosis Cobb angle (LSCA) in the PA view were documented to assess the difference between pre-operation and post-operation. SCA was the angle of scoliosis in which the lesion vertebrae were involved. LSCA was the Cobb angle formed by lines drawn parallel to the upper endplate of the upper adjacent vertebrae and the lower endplate of the lower adjacent vertebrae. The vertebral rotation was examined by the method proposed by Nash-Moe [19].
The 256-line multi-slice CT-Scanner (Siemens SOMATOM Definition Flash, Siemens Healthcare, Germany) was conducted before surgery, and at 1 day postoperatively for all patients, providing 1-mm thick axial helical with three-dimensional reconstructions. The width of pedicle (POW), IIA, the lateral distance (LD) between the planned skin puncture point (PSPP) and the spinous process, and the puncture course length (PCL) at convex and concave sides of the target vertebrae were documented and compared. In the axial CT view, the cross-point between the anterior one-third of the vertebral body and the midline of the body was the target point (T); the middle point of the pedicle was presented as point M. PCL was the line from point T to M and its extended line to the skin. PSPP was the cross-point between PCL and skin (Fig. 2).
The cement distribution, cement leakage, and puncture track were assessed. The criteria for cement leakage were divided into five types: type B (through the basivertebral vein), type S (through the segmental vein), type C (through a cortical defect), and type D (intradiscal leakage)], and mixed type (two or more types existing [20]. Insufficient cement distribution was the distribution of less than half of the fracture area of the index vertebra demonstrated on postoperative axial and sagittal or coronal CT scans [21]. The axial CT images were used to examine the puncture tract to investigate if the pedicle medial wall is intact.
All radiographic parameters were evaluated three times at multiple time points by two independent observers (2 senior spinal surgeons). Any disagreements for non-quantitative parameters between the observers were addressed by reassessment and consensus.
Statistical analysis
SPSS (version 24.0, IBM Corp., Armonk, NY, USA) was used for data analysis in this study. The Shapiro–Wilk test was employed for testing the normality of data. Continuous data were presented as mean and standard deviation when normally distributed or as median and interquartile range when not normally distributed. Continuous data were assessed using a Student t-test for parametric data and a Mann–Whitney U test for nonparametric data. The repeated-measures data were assessed using repeated-measures analysis of variance and the Bonferroni correction for multiple comparisons. P < 0.05 signified statistical significance.
Results
Demographics characteristics and surgical data
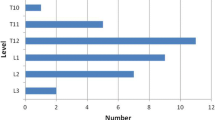
Thirty-six patients, 23 women, and 13 men, with a mean age of 76.31 ± 6.28 years were enrolled and examined. The follow-up period was 17.69 ± 4.70 months. The duration of symptoms was 21.25 ± 12.42 days. The body mass index was 22.97 ± 2.90 and the median bone mineral density was minus 3.6. The surgical levels were T5–T10 in 4, T11–L2 in 26, and L3–L5 in 6 patients. One-vertebrae PKP surgery was conducted in 8 patients, 2-vertebrae in 22, and 3-vertebrae in 6. Thirty-four patients underwent local anesthesia and the remaining two had general anesthesia. There were 11 patients with rotation grade 1, 19 with grade 2, and 6 with grade 3 according to the classification of Nash-Moe [19]. The median surgical duration of single vertebrae was 35 min (IQR, 30–40 min). The mean intraoperative fluoroscopy of single vertebrae was 39.43 ± 5.40 times. The volume of bone cement for single vertebrae was 3.81 ± 0.87 ml and the proportion of sufficient cement distribution of the patients was 97.22. The postoperative hospital stay was 2.67 ± 0.89 days. Table 1 detailed more information.
Clinical and radiographic results
The mean pre-injured BP VAS score was 1.44 ± 0.88, which elevated to 6.58 ± 0.69 at pre-operation and improved to 1.81 ± 0.79 after surgery, and 1.58 ± 0.81 at the last follow-up (P = 0.000; Fig. 4A). The mean pre-injured ODI was 22.94 ± 8.23, which rose to 59.36 ± 5.84 at Pre-operation, and improved to 31.72 ± 9.30 after surgery, and 22.33 ± 7.24 at the last follow-up (P = 0.000; Fig. 4B).
A Visual Analog Scale scores for back pain at the pre-injured, pre-operation, post-operation, and last follow-up assessments; B, Oswestry Disability Index scores at the pre-injured, pre-operation, post-operation, and last follow-up evaluations; * indicates statistical significance between preoperative score and score of any other time point
LKA considerably improved from 17.00 ± 3.00 preoperatively to 12.00 ± 2.39 after surgery, and 12.38 ± 2.54 at the last follow-up (P = 0.000). SCA and LSCA were not substantially modified between these three-time points (P > 0.05). Table 2 detailed additional information.
The POW of the injured vertebrae was considerably wider on the convex side than the concave side (0.62 ± 0.17 cm vs. 0.52 ± 0.11 cm, P = 0.003). IIA was considerably smaller on the convex side than the concave side (12.64° ± 8.04° vs. 50.15° ± 9.63°, P = 0.000). PCL was considerably shorter on the convex side than the concave side (7.37 ± 1.27 cm vs. 10.95 ± 2.26 cm, P = 0.000). Similarly, LD was shorter on the convex side than on the concave side (3.82 ± 0.75 cm vs. 6.70 ± 1.74 cm, P = 0.000). Table 3 showed detailed information.
Complications
Cement leakage (7 patients, 19.4%) was the main complication and fortunately, it did not lead to severe consequences. Among them, three patients with type D leakage, two with type C leakage, one with type S leakage, and one with mixed leakage (type C + D). These patients without any discomfort symptoms received no additional treatment and had a careful follow-up. Puncture complications occurred in two patients and did not cause neurological injury. The inner wall of the pedicles was a break and the puncture course slightly intruded into the spinal canal according to the postoperative CT outcome. The adjacent level vertebral fracture occurred in two patients (Table 1).
Discussion
To the best of our knowledge, this is the first research to treat P-OVCF patients with scoliosis using PKP surgery through unilateral puncture at the convex side. Safe and effective results of this approach were observed for an average of 17 months of follow-up.
Treatment goal and surgical decision
Clinically, P-OVCF or scoliosis can cause BP separately; sometimes the symptoms of BP are induced by both two. It is difficult to differentiate which is the main cause of BP from the aspect of symptomatology, however, by combining medical history with MRI, we can extensively clear the responsibility of BP. Patients with scoliosis may have BP or not. The BP symptoms resulting from scoliosis always reveal a chronic course and accumulated progression and have characteristics of mechanic BP due to the unstable spine [22, 23]. However, patients with P-OVCF are usually identified with acute or sub-acute BP, and most of them had a mild injury history such as fallen [24]. Therefore, careful medical history taking is critical to assess the life status of the P-OVCF patient with scoliosis before the acute BP onset to try to clear which is the main cause of BP?
An exact understanding of patient healthy expectations and acquiring collaboration with patients are important for surgeons. For patients with mild BP before acute BP onset, conducting a PKP to lower the acute pain may be the rational treatment, and scoliosis which did not induce severe BP underwent careful follow-up may be sound. For patients with chronic moderate to severe BP before acute BP onset, both P-OVCF and scoliosis may be the causes of symptoms, only PKP surgery may be insufficient to alleviate the patient’s symptoms, however, open surgery should be extra careful with these aging patients. These patients usually had several coexisting medical conditions and a high risk of open surgery [25, 26]. Therefore, the rational treatment goal and proper minimally invasive surgical method were equally critical to balance and achieve satisfactory clinical results and perioperative safety [27].
In this study, a careful assessment of the life status of the patients before the acute BP onset was conducted. The BP and ODI outcomes between pre-injured and pre-operation showed that the life status of the patients is tolerable (Fig. 4). Therefore, we presume that the acute BP was mostly due to the P-OVCF and PKP surgery can relieve the BP. Importantly, the patients should be clear that the acute BP was the ultimate treatment goal, and correction for scoliosis was unnecessary this time and should undergo careful follow-up.
Unilateral puncture in convex side
The unilateral puncture method for PKP to treat P-OVCF in our center was last for over 10 years and excellent clinical outcomes were obtained [13, 28]. In clinical practice, we discovered that in P-OVCF patients with scoliosis, the puncture conducted on the convex side had several benefits including shorter PCL, lesser IIA, and bigger POW. These advantages would make the puncture simpler to achieve the target point and symmetrical bone cement distribution. Furthermore, the spinal cord or dural sac was usually on the concave side. Therefore, the puncture on the convex side may be easier and safer. The current study findings proved the aforementioned advantages and demonstrated safe and effective outcomes (Table 3; Fig. 4) which was even similar to that of prior studies including patients without scoliosis [9, 10, 17].
Cement leakage occurred in seven patients (19.4%) and puncture complications occurred in two patients (5.6%) in this research without severe consequences. The cement leakage complication rate was less than that of previous reports which ranged from 4.8 to 39% [17]. Despite the high rates, works of literature reported that only a few cases are symptomatic or have related complications [17]. The success rate of puncture in this study was 94.4%, which revealed the high safety of this puncture method and the findings were even similar to a previous study in which the puncture was assisted by a robot with success rates ranging from 92.9 to 100% [8].
However, being unable to correct scoliosis or the likelihood of causing severer scoliosis was a theoretical disadvantage of this puncture in contrast with a bilateral puncture or unilateral puncture through the concave side. PKP through the concave side has the possible advantage of correction in a patient with scoliosis, however, this correction ability may be weak for the whole spine and followed by higher technique challenges and risks (Table 3). This study’s outcomes revealed that after achieving a satisfactory puncture and symmetrical bone cement distribution in these patients, severer scoliosis was not observed after surgery, and SCA and LSCA were not statistically substantial between pre-operation, post-operation, and the last follow-up (Table 2). Same to previous studies [4, 7, 17], the LKA was enhanced significantly after surgery (Table 2). This enhanced sagittal alignment of the spine combined with anti-osteoporosis drug treatment may reduce the risk of re-fracture of the spine to some degree.
Technical notes
Asymmetric, rotated vertebrae and pedicles combined with osteoporosis prevent visualization of round pedicle shadows. It is difficult to conduct an accurate puncture into such pedicles, which have a highly variable and complex three-dimensional orientation. Furthermore, small pedicles are often found in scoliosis, particularly on the concave side, study reported that the proportion of extremely small pedicles was 7.8% [29]. Therefore, two technique notes were critical in PKP surgery for P-OVCF patients with scoliosis. The first is to obtain symmetrical or nearly symmetrical pedicle shadows on a true PA view via a rotating C-arm fluoroscope. The second was to conduct a puncture on the convex side. These procedures allow surgeons to carry out the PKP surgery under relatively high-quality visualization, with lesser anatomical difficulties, and technique issues.
Limitations
This study has several limitations. First, the retrospective study may have presented selection bias. Second, anterior vertebral height was not included in the assessment parameters, for the height was unable to accurate measurement on the X-ray in scoliosis. Finally, the follow-up period of this study was relatively short and the time point of the last follow-up was different due to patient compliance.
Conclusion
This study presented an enhanced method of unilateral puncture on the convex side to conduct PKP surgery for the treatment of P-OVCF with scoliosis. In combination with adequate assessment of the pre-injured life status of patients, this technique for P-OVCF with scoliosis can achieve safe, excellent clinical, and radiographic outcomes.
Data availability
The datasets in the current study are available from the corresponding author on reasonable request.
Abbreviations
- BP:
-
back pain
- IIA:
-
inner inclination angle
- SCA:
-
scoliosis Cobb angle
- LD:
-
lateral distance
- LSCA:
-
local scoliosis Cobb angle
- LKA:
-
local kyphosis angle
- ODI:
-
Oswestry disability index
- PA:
-
posterior-anterior
- PCL:
-
puncture course length
- PKP:
-
percutaneous kyphoplasty
- P-OVCF:
-
painful osteoporotic vertebral compression fractures
- PSPP:
-
planned skin puncture point
- POW:
-
width of pedicle
- VAS:
-
visual analog scale
References
Bae H, Shen M, Maurer P, et al. Clinical experience using Cortoss for treating vertebral compression fractures with vertebroplasty and kyphoplasty: twenty four-month follow-up. Spine (Phila Pa 1976). 2010;35:E1030–6.
Wardlaw D, Cummings SR, Meirhaeghe JV, et al. Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet. 2009;373:1016–24.
Feltes C, Fountas KN, Machinis T, et al. Immediate and early postoperative pain relief after kyphoplasty without significant restoration of vertebral body height in acute osteoporotic vertebral fractures. Neurosurg Focus. 2005;18(3):e5.
Santiago FR, Chinchilla AS, Álvarez LG, et al. Comparative review of vertebroplasty and kyphoplasty. World J Radiol. 2014;6:329–43.
Chevalier Y, Pahr D, Charlebois M, et al. Cement distribution, volume, and compliance in vertebroplasty: some answers from an anatomybased nonlinear finite element study. Spine (Phila Pa 1976). 2008;33:1722–30.
Liebschner MA, Rosenberg WS, Keaveny TM. Effects of bone cement volume and distribution on vertebral stiffness after vertebroplasty. Spine (Phila Pa 1976). 2001;26:1547–54.
Zhang YJ, Liu H, He F, Chen A, et al. Safety and efficacy of percutaneous kyphoplasty assisted with O-arm navigation for the treatment of osteoporotic vertebral compression fractures at T6 to T9 vertebrae. Int Orthop. 2020;44:349–55.
Yuan W, Cao WH, Meng XT, et al. Learning curve of Robot-assisted Percutaneous Kyphoplasty for Osteoporotic Vertebral Compression fractures. World Neurosurg. 2020;138:e323–9.
Beall DP, Chambers MR, Thomas S, et al. Prospective and Multicenter Evaluation of Outcomes for Quality of Life and Activities of Daily Living for Balloon Kyphoplasty in the treatment of Vertebral Compression fractures: the EVOLVE Trial. Neurosurgery. 2019;84:169–78.
Zhang YT, Chen XJ, Ji JC, et al. Comparison of unilateral and bilateral percutaneous kyphoplasty for bone cement distribution and clinical efficacy: an analysis using three-Dimensional computed tomography images. Pain Physician. 2022;25:E805–13.
Sun H, Lu PP, Liu YJ, et al. Can Unilateral Kyphoplasty replace bilateral Kyphoplasty in Treatment of Osteoporotic Vertebral Compression fractures? A systematic review and Meta-analysis. Pain Physician. 2016;19:551–63.
Kobayashi K, Takizawa K, Koyama M, et al. Unilateral transpedicular percutaneous vertebroplasty using puncture simulation. Radiat Med. 2006;3:187–94.
Wang S, Wang Q, Kang JP, et al. An imaging anatomical study on percutaneous kyphoplasty for lumbar via a unilateral transverse process-pedicle approach. Spine (Phila Pa 1976). 2014;39:701–6.
Chen CM, Chen L, Gu Y, et al. Kyphoplasty for chronic painful osteoporotic vertebral compression fractures via unipedicular versus bipedicular approachment: a comparative study in early stage. Injury. 2010;41:356–9.
Chen L, Yang H, Tang T. Unilateral versus bilateral balloon kyphoplasty for multilevel osteoporotic vertebral compression fractures: a prospective study. Spine (Phila Pa 1976). 2010;36:534–40.
Liu X, Yang H, Liang D. A study of clinical significance on measuring the angles between the pedicles and the center of their anterior-inferior parts. Chin J Clin Anat. 2004;22:249–53.
Yang HL, Liu H, Wang SH, et al. Review of Percutaneous Kyphoplasty in China. Spine (Phila Pa 1976). 2016;41:B52–8.
Zhang S, Wang GJ, Wang Q, et al. A mysterious risk factor for bone cement leakage into the spinal canal through the Batson vein during percutaneous kyphoplasty: a case control study. BMC Musculoskelet Disord. 2019;20:423.
Nash C Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg. 1969;51:223e9.
Tang BQ, Xu SJ, Chen XM, et al. The impact of intravertebral cleft on cement leakage in percutaneous vertebroplasty for osteoporotic vertebral compression fractures: a case-control study. BMC Musculoskelet Disord. 2021;22:805.
Ye LQ, Liang D, Jiang XB, et al. Risk factors for the occurrence of insufficient cement distribution in the fractured area after percutaneous vertebroplasty in osteoporotic vertebral compression fractures. Pain Physician. 2018;21:E33–42.
Yamada K, Nakamae T, Nakanishi K, et al. Long-term outcome of targeted therapy for low back pain in elderly degenerative lumbar scoliosis. Eur Spine J. 2021;30:2020–32.
Daffner SD, Vaccaro AR. Adult degenerative lumbar scoliosis. Am J Orthop (Belle Mead NJ). 2003;32:77–82. discussion 82.
Musbahi O, Ali AM, Hassany H, et al. Vertebral compression fractures. Br J Hosp Med (Lond). 2018;79:36–40.
Chang LL, Devereaux PJ, Slobogean G. Choice of Admitting services for older adults with hip fracture. N Engl J Med. 2022;387:2466–8.
HIP ATTACK Investigators. Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. Lancet. 2020;395:698–708.
Yang J, Wu H, Kong QQ, et al. Full endoscopic transforaminal decompression surgery for symptomatic lumbar spinal stenosis in geriatric patients. World Neurosurg. 2019;127:e449–59.
Huang JH, Yang J, Chen LJ, et al. A novel puncture approach via point O for percutaneous kyphoplasty in patients with L4 or L5 osteoporotic vertebral compression fracture. Sci Rep. 2022;12:18868.
Lee CS, Park SA, Hwang CJ, et al. A novel method of screw placement for extremely small thoracic pedicles in scoliosis. Spine (Phila Pa 1976). 2011;36:E1112–6.
Acknowledgements
We thank the patients for their participation and contributions in this present study. We thank the doctor Xu and doctor Wang for the technical assistance.
Funding
This research was supported by the Project of Sichuan Provincial Department of Science and Technology (No: 23ZDYF2773; No: 2023YFS0097) and the Strategic Cooperation Project of Sichuan University - Luzhou Municipal People’s Government (NO.2020CDLZ-5).
Author information
Authors and Affiliations
Contributions
LQH, YPJ and WS were major contributors in data collection, and drafted the original manuscript. WQ and YJ conceptualized the study and reviewed and edited the original draft of the manuscript. YPJ, LQH and YJ were contributors in project administration and supervision. WS and LQH were major contributors in data analysis. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This study was approved by the Medical Ethics Review Committee of Affiliated Hospital of Southwest Medical University (No: KY2023024). All patients provided written informed consent prior to their inclusion in this study. The methods were carried out in accordance with the relevant guidelines and regulations.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Q., Wang, S., Wang, Q. et al. Percutaneous kyphoplasty through unilateral puncture on the convex side for the treatment of painful osteoporotic vertebral compression fracture with scoliosis. BMC Musculoskelet Disord 25, 294 (2024). https://doi.org/10.1186/s12891-024-07399-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07399-w