Abstract
Purpose
To compare the postoperative rehabilitation of femoral neck fractures treated with robot-assisted nailing and freehand nailing.
Methods
We systematically searched the PubMed, EMBASE, Cochrane, China National Knowledge Infrastructure(CNKI), WanFang database, China Science and Technology Journal Database (VIP) and Web of Science databases to identify potentially eligible articles. Indispensable data such as the year of publication, country, study type, robot type, age, number of patients, sex distribution, study design, and outcome indicators were extracted. The outcome indicators of interest included healing rate, length of healing time, Harris score, operation time, frequency of X-ray fluoroscopy, frequency of guide pin insertion, and intraoperative blood loss. RevMan 5.4.1 was used for the meta-analysis.
Results
Fourteen studies with 908 participants were included in this meta-analysis. The results showed that in terms of healing rate (SMD = 2.75, 95% CI, 1.03 to 7.32, P = 0.04) and Harris score (SMD = 2.27, 95% CI, 0.79 to 3.75, P = 0.003), robot-assisted screw placement technique scores were higher than the traditional freehand technique. Additionally, operative time (SMD = -12.72, 95% CI, -19.74 to -5.70, P = 0.0004), healing time (SMD = -13.63, 95% CI, -20.18 to -7.08, P < 0.0001), frequency of X-ray fluoroscopy (SMD = − 13.64, 95% CI, − 18.32 to − 8.95, P < 0.00001), frequency of guide pin insertion (SMD = − 7.95, 95% CI, − 10.13 to − 5.76, P < 0.00001), and intraoperative blood loss (SMD = − 17.33, 95% CI, − 23.66 to − 11.00, P < 0.00001) were lower for patients who underwent robotic-assisted screw placement than those for patients who underwent the conventional freehand technique.
Conclusion
Compared to the freehand nailing technique, robot-assisted nailing helps improve postoperative healing rates in patients with femoral neck fractures; shortens healing times; better restores hip function; reduces the number of intraoperative fluoroscopies, guides pin placements; reduces intraoperative bleeding; and increases perioperative safety.
Similar content being viewed by others
Introduction
Femoral neck fractures are the most common hip fractures, accounting for 3–4% of all fractures and 50–60% of hip fractures [1, 2]. Currently, the mainstream treatment modalities include conservative treatment, internal fixation, external fixation, and hip arthroplasty. In clinical practice, there is a general consensus for early surgical treatment of patients with femoral neck fractures, as conservative treatment requires patients to be bedridden for long periods and carries the risk of infection and thrombosis [3]. Closed reduction with percutaneous hollow tension screw internal fixation is one of the main procedures used to treat femoral neck fractures [4, 5]. This method uses closed reduction, which avoids excessive medically induced injuries, and its three inverted triangular arrangements of screws [6] allow for dynamic compression, ensuring secure fixation while ensuring effective fixation [7]. However, this procedure relies on the surgeon’s experience in placing screws using X-ray fluoroscopy, which is not sufficiently precise, requires a high level of skill, and exposes the surgeon to high radiation doses. From a patient-healing perspective, the precision of freehand nail placement can also affect femoral neck healing. Schep et al. [8] found that the precise position and orientation of the intraoperative fixation screw are closely related to the prognosis of fracture stability, the occurrence of re-displacement, and fracture healing time. In contrast, the traditional C-arm-assisted freehand nail placement method not only requires the surgeon to constantly adjust the position of the C-arm, but also increases the risk of contamination of the operative area. Moreover, because of the limited precision of freehand nail placement, repeated drilling and puncturing can affect blood supply and bone destruction in cases of nail placement failure [9, 10], which in turn affects the healing rate [11]. Despite extensive efforts to improve and investigate the use of internal fixation for femoral neck fractures, an optimal fixation method has yet to be identified, and the incidence of postoperative osteonecrosis and femoral head necrosis remains high [12]. Accurate and minimally invasive screw placement while reducing radiation exposure to patients and surgeons during surgery, has become an urgent challenge. Currently, with the popularity of 2D and 3D digital imaging, computer-guided and robotic surgical systems assisted by minimally invasive internal fixation are increasingly used for the treatment of femoral neck fractures. Compared to traditional surgery, robot-assisted surgery has the advantages of shorter surgical time and less radiation damage; therefore,, so it is favoured by an increasing number of orthopaedic surgeons and is gradually being used in clinical practices [13, 14]. Orthopaedic surgical robots provide data analysis and processing, surgical navigation, simulation planning, and precise positioning, and can place screws quickly, accurately, and safely; several studies have concluded that the accuracy of nail placement is over 98% [15]. Although robot-assisted nail placement has been shown to be superior to conventional nail placement in terms of accuracy, there is a lack of evidence that robot-assisted nail placement results in a better prognosis for patients with femoral neck fractures. Exploring the close relationship between robot-assisted surgery and patient prognosis is currently the focus of clinical research in robot-assisted femoral neck fracture surgeries [16]. Previous clinical studies have generally concluded that robot-assisted surgery has significant advantages [17, 18] in terms of short operative time, reduced number of fluoroscopic views and guide pin placements, and reduced intraoperative bleeding, and that these advantages facilitate the postoperative rehabilitation of patients. However, in terms of healing rate, healing time, and postoperative Harris score, several studies concluded that there was no difference between the robot-assisted nail placement technique and the traditional freehand nail placement technique, while some studies concluded that patients treated with robot-assisted surgery had a better prognosis. In conclusion, there is controversy among researchers regarding whether robot-assisted nailing provides better rehabilitation outcomes in patients with femoral neck fractures. This study aimed to summarise previous studies through a meta-analysis to verify the advantages of robot-assisted nail placement in intraoperative operations and to determine whether robot-assisted nail placement improves the rehabilitation outcomes of patients with femoral neck fractures. The indicators used to evaluate rehabilitation outcomes were healing rate, healing time, and postoperative Harris score.
Methods
Data search strategy
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) procedure [19]. We systematically searched PubMed, EMBASE, Cochrane, China National Knowledge Infrastructure (CNKI), WanFang database, China Science and Technology Journal Database (VIP), and Web of Science to identify potentially eligible articles. Notably, these databases were updated on January 19, 2024. We used the following keywords: ‘‘Robotics’’, “Robot”, “Robot-assisted”, ‘‘Fracture’’, “Femoral Neck Fractures”, and ‘‘Fracture Healing’’. For example, the search strategy employed for PubMed is presented in Table 1. Two reviewers (Li Yiyang and Sun Yadi) independently searched all the titles and abstracts, and the references of relevant studies were reviewed for additional valuable literature. Any divergence was resolved through discussion or consultation with a third reviewer (Wang Yan).
We used the Population, Intervention, Comparison, Outcomes and Study (PICOS) system [20] for this systematic review. This system frames the review’s aim, search strategy, and study inclusion and exclusion criteria. The critical items of our systematic review are described below:
-
P (Population): Patients with femoral neck fractures.
-
I (Intervention): Robot-assisted screw placement.
-
C (Comparison): Freehand screw placement.
-
O (Outcome): Healing rate, length of healing time, Harris score, operation time, frequency of X-ray fluoroscopy, frequency of guide pin insertion, and intraoperative blood loss.
-
S (Study design): Randomised controlled trial and cohort studies.
Study selection
Inclusion criteria were identified before the search, and the following criteria were used: articles involving robot-assisted femoral neck screw placement, quantitative indicators for evaluating patient rehabilitation outcomes, and providing sufficient data for meaningful comparison (> 10 patients per study group). The exclusion criteria were duplicate publications and articles without traditional freehand screw placement in the control group. Furthermore, only human studies were considered. The inclusion of studies was not limited by study size or publication type, and the excluded publications were review articles and commentaries.
Quality assessment and data extraction
Two reviewers independently assessed all included studies using the risk-of-bias tool. Retrospective cohort studies were evaluated using the Newcastle-Ottawa Quality Assessment Scale, which is rated using 0–9 stars. Seven or more stars indicate sufficiently high quality. The Cochrane risk-of-bias criteria were used to assess the quality of the randomized clinical trial (RCT) regarding selection, performance, detection, attrition, reporting, and other biases. We defined other biases as the difference in baseline characteristics between the experimental and control groups.
Two reviewers independently extracted the data extraction. Any disagreements were resolved through discussion or consultation with a third reviewer. Indispensable data, such as publication year, study type, age, number of patients, gender distribution, study design, and outcomes, were extracted. Outcome indicators of interest included healing rate, length of healing time, Harris score, operation time, frequency of X-ray fluoroscopy, frequency of guide pin insertion and intraoperative blood loss.
Results
Characteristics of the included studies
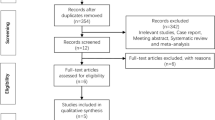
Figure 1 shows the process of study inclusion. Notably, 2606 relevant studies were obtained through a web search. In total, 676 studies were excluded because they were duplicates. After assessing the titles and abstracts, 1930 studies were excluded because their content did not meet the criteria. After verifying the full text of the remaining 46 studies, 13 retrospective cohort studies (RCS) [6, 17, 18, 21,22,23,24,25,26,27,28,29,30] and one RCT [30] with 908 patients were finally included in this meta-analysis. The RCT was shown to have a low risk of bias in Fig. 2. Table 2 summarises the main characteristics of the included studies. Baseline information was balanced and comparable across the 14 studies. The cohort studies all had evaluation scores greater than seven stars (Table 3), and all the included studies demonstrated satisfactory quality.
Healing rate and length of healing time
Seven studies provided data on the healing rate, and five studies provided data on the healing time. The results show that a higher percentage of patients recovered from robotic-assisted surgery (standardised mean difference (SMD) = 2.75, 95% confidence interval (CI), 1.03–7.32, P = 0.04; Fig. 3) with a shorter healing time (SMD = -13.63, 95% CI, -20.18 – -7.08, P < 0.0001; Fig. 4) than from unassisted surgery.
Harris score
Ten studies provided data on the Harris score. The results showed that the Harris score for patients who underwent robotic-assisted screw placement (SMD = 2.27, 95% CI, 0.79–3.75, P < 0.003; Fig. 5) was greater than that of those who underwent the conventional freehand technique.
Operation time
Eight studies provided data on operation time. The results showed that the robot-assisted technique requires less operation time (SMD = -12.72, 95% CI, -19.74 – -5.70, P < 0.0004; Fig. 6) than the freehand technique.
Frequency of X-ray fluoroscopy
Eight studies provided data on the frequency of X-ray fluoroscopy. The results showed that patients undergoing robot-assisted surgery require less fluoroscopy (SMD = -13.64, 95% CI, -18.32 – -8.95, P < 0.00001; Fig. 7) than those undergoing traditional surgery.
Frequency of guide pin insertion
Eight studies provided data on the frequency of guide pin insertion. The results showed that the robot-assisted technique requires fewer guide pin insertions (SMD = -7.95, 95% CI, -10.13 – -5.76, P < 0.00001; Fig. 8) than the freehand technique.
Intraoperative blood loss
Ten studies provided data on intraoperative blood loss. The results showed that patients with femoral neck fractures treated with robot-assisted surgery have less intraoperative blood loss (SMD = -17.33, 95% CI, -23.66 – -11.00, P < 0.00001; Fig. 9).
Sensitivity analysis and publication bias test
In case of significant heterogeneity in the Harris score, operation time, frequency of X-ray fluoroscopy, frequency of guide pin insertion, and intraoperative blood loss results, a sensitivity analysis was conducted by omitting one study in each turn, and then the others were analysed to estimate whether a single study markedly affected heterogeneity. This analysis confirmed the stability of the Harris score, operation time, frequency of X-ray fluoroscopy, frequency of guide pin insertion, and intraoperative blood loss results.
Funnel plots were performed to test for possible publication bias. Supplemental material 1 shows that the studies were nearly symmetrically distributed on both sides of the vertical line, indicating a relatively small publication bias.
Discussion
This meta-analysis showed that robot-assisted screw placement significantly improved patient recovery and reduced intraoperative injuries compared with traditional freehand screw placement. Femoral neck fractures are currently increasing in middle-aged and older adults, and ischemic necrosis of the femoral head and non-union of the fracture remain major postoperative complications [32]. Weil et al. [33] reported that in surgeries for femoral neck fractures, selecting an appropriate implantation site and depth is crucial. Wang et al. [6] also showed that the direction and position of intraoperative hollow screw placement are closely associated with the re-displacement, fixed stability, and healing of the fractures postoperatively. The more accurate the hollow screw placement, the more stable the internal fixation of the femoral neck fracture, and the lower the risk of fracture bone discontinuity [34]. Robots are increasingly used in femoral neck repair surgery because of their accuracy. Experimental evidence shows that robot-assisted femoral neck repair surgery is more accurate than freehand nail placement. Zhu et al. [27] and He et al. [35] mention that the screw parallelism in the robot-operated group was better than that in the freehand-operated group. However, the prognostic outcomes of the robot- and freehand-operated groups have been evaluated differently in different studies, with Zhu et al. [27] concluding that patients in the robot-operated group had a higher postoperative healing rate, and Wan et al. [25] concluding that both groups showed no statistical difference regarding healing rates. This is inconsistent with previous studies theory that states that “greater precision in nail placement leads to a better prognosis.” Therefore, a meta-analysis was necessary to pool past studies.
Our research showed that robot-assisted treatment of femoral neck fractures leads to a better prognosis. The healing rate and time may be associated with the precise nail placement of the robot. Robotic precision nail placement leads to higher parallelism and discrete rates [35]. Zhou et al. [36] demonstrated that a standard, inverted triangle distribution and good parallelism can promote fracture healing. Regarding the operative length, the analysis showed that robotic surgery was significantly shorter than conventional surgery. However, other studies arrived at a contradictory conclusion. Cao et al. [23] suggested that the robot requires more time. Nassim et al. [37] and Zheng et al. [38] concluded that the robotic and freehand screw placement showed no difference in operative time. These studies indicated that there is still room for improvement in reducing the operative time with robot-assisted technology. Arand et al. [39] also cited experience as vital in the length of surgery, as the actual intraoperative needle may shift to a certain extent when it encounters resistance, and less experienced operators may spend more time adjusting the needle position. Notably, other studies have attributed the prolonged operative time to the operative steps of the robot-assisted procedure; however, Duan et al. [26] suggest that most of the time spent in robot-assisted surgery is spent on device placement and commissioning, image acquisition, and other non-invasive procedures. Furthermore, Cao et al. [23] suggest in more detail why robot-assisted techniques take longer in operative steps. These include longer image acquisition time, sometimes requiring multiple x-rays; longer image transfer time, with images currently acquired by the C-arm needing to be copied to the system workstation for path planning; and the fact that most systems do not support simultaneous planning of multiple screw paths, with only one screw being placed in a single pass.
Notably, most studies agree that robotic-assisted surgery is less invasive than conventional surgery in the number of X-ray fluoroscopies, intraoperative bleeding, and guide needle placements, providing strong evidence that robotic-assisted surgery helps patient recovery. Robotic-assisted techniques do not require repeated fluoroscopy to determine needle placement [21] and can significantly reduce the number of fluoroscopies. Semi-automated needle placement results in fewer errors and significantly fewer needle placements than unassisted placement, facilitating the healing of the patient’s incision. In middle-aged and elderly patients with reduced bone mass, repeated pin placement can cause punctate loss of bone in the access area, preventing the pin from being placed in the right place and affecting the accuracy of internal fixation placement. Such subtle changes may not be accurately analysed from radiographic data but can affect long-term outcomes [22]. Similarly, fewer needle placements result in less bleeding, which benefits the early postoperative recovery of older patients, especially those with poor systemic organ function, and improves perioperative safety.
The application of orthopaedic robots in traumatic orthopaedics is still new compared with spinal and joint replacement surgeries, and robot-assisted femoral neck fracture treatment is currently the scenario that most commonly uses robots in traumatic orthopaedics. Therefore, studying the clinical outcomes and rehabilitation results of patients undergoing this kind of surgery is significant in selecting treatment modalities for femoral neck fractures and has reference values for developing orthopaedic robots. We believe that applying robotics to femoral neck fractures will ultimately improve the healing rate and shorten the healing time. This study determined the statistical differences between robot-assisted femoral neck fracture surgery and the freehand nail placement technique regarding healing rate, healing time, and postoperative Harris scores. The results showed that the robot-assisted technique was more effective than the unassisted screw placement technique in improving healing rates, reducing healing times, and improving patients’ postoperative Harris scores. This study also demonstrated the advantages of robotics in reducing the number of fluoroscopies, needle placements, and bleeding.
Our study had some limitations. First, most of the included studies were RCSs, and the level of evidence was not as high as that of RCTs. Second, most robot models are made in China, making the conclusions of this study non-generalizable to other robot models. However, despite these limitations, the RCSs included in this meta-analysis all had scores of seven stars or above and remained of high quality.
Conclusion
Robot-assisted nailing technique helps improve postoperative healing rates in patients with femoral neck fractures, shortens healing times, restores hip function, reduces the number of intraoperative fluoroscopies, guides pin placements, reduces intraoperative bleeding in patients, and increases perioperative safety than the freehand nailing technique.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Abbreviations
- RCT:
-
Randomised controlled trial
- RCS:
-
Retrospective cohort study
- RA:
-
Robot-assisted
- FH:
-
Freehand
- SMD:
-
Standardised mean difference
- CI:
-
Confidence interval
References
Zhan S, Jiang D, Ling M, et al. Fixation effects of different types of cannulated screws on vertical femoral neck fracture: a finite element analysis and experimental study. Med Eng Phys. 2021;97:32–9. https://doi.org/10.1016/j.medengphy.2021.09.007.
Archibeck MJ, Carothers JT, Tripuraneni KR, et al. Total hip arthroplasty after failed internal fixation of proximal femoral fractures. J Arthroplast. 2013;28(1):168–71. https://doi.org/10.1016/j.arth.2012.04.003.
Li X, Luo J. Hemiarthroplasty compared to total hip arthroplasty for the treatment of femoral neck fractures: a systematic review and meta-analysis. J Orthop Surg Res. 2021;16:172. https://doi.org/10.1186/s13018-020-02186-4.
Zhang J, Zhuang Y, Dai L, et al. A comparative study between proximal femoral locking plate and multiple cannulated screws for fixation of femoral neck fractures in young adults. J Healthc Eng. 2022;2022. https://doi.org/10.1155/2022/1286419.
Wang G, Tang Y, Wang B, Yang H. Minimally invasive open reduction combined with proximal femoral hollow locking plate in the treatment of Pauwels type III femoral neck fracture. J Int Med Res. 2019;47(7):3050–60. https://doi.org/10.1177/0300060519850962.
Wang X, Lan H, Li KN. Treatment of femoral neck fractures with cannulated screw invasive internal fixation assisted by orthopaedic surgery robot positioning system. Orthop Surg. 2019;11(5):864–72. https://doi.org/10.1111/os.12548.
Zhang GZ, Wang MY, Jiang XY. Three nonparallel screws for the treatment of femoral neck fractures. Zhongguo Gu Shang. 2012;25(12):1002–4. https://doi.org/10.3969/j.issn.1003-0034.2012.12.008.
Schep NWL, Heintjes RJ, Martens EP, et al. Retrospective analysis of factors influencing the operative result after percutaneous osteosynthesis of intracapsular femoral neck fractures. Injury. 2004;35(10):1003–9. https://doi.org/10.1016/j.injury.2003.07.001.
Wang Y, Shi S, Zheng Q, Jin Y, Dai Y. Application of 3-dimensional printing technology combined with guide plates for thoracic spinal tuberculosis. Medicine (Baltimore). 2021;100(6):e24636. https://doi.org/10.1097/MD.0000000000024636.
Gu Y, Yao Q, Xu Y, Zhang H, Wei P, Wang L. A clinical application study of mixed reality technology assisted lumbar pedicle screws implantation. Med Sci Monit. 2020;26:e924982. https://doi.org/10.12659/MSM.924982.
Hamelinck HKM, Haagmans M, Snoeren MM. Safety of computer-assisted surgery for cannulated hip screws. Clin Orthop Relat Res. 2007;455:241–5. https://doi.org/10.1097/01.blo.0000238815.40777.d2.
Parker MJ, Raghavan R, Gurusamy K. Incidence of fracture-healing complications after femoral neck fractures. Clin Orthop Related Res. 2007;458:175–9. https://doi.org/10.1097/BLO.0b013e3180325a42.
Wang W, Yeung KWK. Bone grafts and biomaterials substitutes for bone defect repair: a review. Bioactive Mater. 2017;2(4):224–47. https://doi.org/10.1016/j.bioactmat.2017.05.007.
Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American pain society, the American Society of Regional Anesthesia and Pain Medicine, and the American society of anesthesiologists’ committee on regional anesthesia, executive committee, and administrative council. J Pain. 2016;17(2):131–57. https://doi.org/10.1016/j.jpain.2015.12.008.
Ye XJ. Robotic surgery plays a precise, safe, minimally invasive and efficient role in spinal surgery. Zhongguo Gu Shang. 2022;35(2):99–100. https://doi.org/10.12200/j.issn.1003-0034.2022.02.001.
Makris UE, Abrams RC, Gurland B, et al. Management of persistent pain in the older patient: a clinical review. JAMA. 2014;312(8):825–37. https://doi.org/10.1001/jama.2014.9405.
Nie DX, Sun WG, Wang XQ, et al. Comparison of curative effect between Tianji robot assisted screw placement and traditional cannulated screw internal fixation for femoral neck fracture. Zhongguo Gu Shang. 2023;36(3):221–5. https://doi.org/10.12200/j.issn.1003-0034.2023.03.005.
Huang B, Rong S, LI J, et al. Bi-planar robot navigation for cannulated screw fixation in the treatment of femoral neck fractures. Chin J Orthop. 2017;528–34. https://doi.org/10.3760/cma.j.issn.0253-2352.2017.09.003.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. https://doi.org/10.1016/j.ijsu.2021.105906.
Amir-Behghadami M, Janati A. Population, Intervention, Comparison, Outcomes and Study (PICOS) design as a framework to formulate eligibility criteria in systematic reviews. Emerg Med J. 2020. https://doi.org/10.1136/emermed-2020-209567.
Tong Y, Luo X, Wu G, et al. Comparative study on fixation with percutaneous cannulated screws assisted by robot navigation and conventional surgery with manual positioning for femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2016;30(6):685–9. https://doi.org/10.7507/1002-1892.20160139.
Jing Y, Zhang S, Han Z, et al. Short-term effectiveness of orthopedic robot-assisted femoral neck system fixation for fresh femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022;36(8):946–50. https://doi.org/10.7507/1002-1892.202203093.
Cao Y, Zhao Y, Hu L, et al. Clinical application of computer-assisted cannulated screw internal fixation system based on error correction method for femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2017;31(3):257–61. https://doi.org/10.7507/1002-1892.201611066.
Liu J, Liu L, Huang J, et al. Fixation with percutaneous cannulated screws assisted by robot navigation for femoral neck fractures. Chin J Orthop Trauma. 2015. https://doi.org/10.3760/cma.j.issn.1671-7600.2015.08.010.
Wan L, Zhang X, Wu D, et al. Application of robot positioning for cannulated screw internal fixation in the treatment of femoral neck fracture: retrospective study. JMIR Med Inform. 2021;9(1). https://doi.org/10.2196/24164.
Duan S, Liu H, Wu W, et al. Robot-assisted percutaneous cannulated screw fixation of femoral neck fractures: preliminary clinical results. Orthopaedic Surgery. 2019;11(1):34–41. https://doi.org/10.1111/os.12430.
Zhu Z, Xiao C, Tan B, et al. TiRobot-assisted percutaneous cannulated screw fixation in the treatment of femoral neck fractures: a minimum 2‐year follow‐up of 50 patients. Orthop Surg. 2021;13(1):244–52. https://doi.org/10.1111/os.12915.
Chen J, Zhou G, Chen X, et al. Robot-assisted percutaneous cannulated screw fixation of femoral neck fracture. Orthop J China. 2023;31(4):295–9. https://doi.org/10.3977/j.issn.1005-8478.2023.04.02.
Huang F, Zhang X, Li W, et al. Comparison of robot assisted and freehand percutaneous cannulated screwing for femoral neck fractures in the middle aged and young patients. Chin J Orthop Traum. 2023;25(11):979–85. https://doi.org/10.3760/cma.j.cn115530-20230524-00259.
Liao Y, Zhang M, Xu J, et al. TiRobot assisted biplane double supported screw fixation for femoral neck fractures in middle aged and young patients. Chin J Orthop Traum. 2022;24(12):1069–74. https://doi.org/10.3760/cma.j.cn115530-20220802-00414.
Yi S, Zhang D, Wang J, et al. Clinical effect evaluation of robot navigation for percutaneous cannulated screw fixation in treatment of femoral neck fractures. Chin J Bone Joint Injury. 2022;37(4):337–41. https://doi.org/10.7531/j.issn.1672-9935.2022.04.001.
Kumar MN, Belehalli P, Ramachandra P. PET/CT study of temporal variations in blood flow to the femoral head following low-energy fracture of the femoral neck. Orthopedics. 2014;37(6):e563-570. https://doi.org/10.3928/01477447-20140528-57.
Weil YA, Qawasmi F, Liebergall M, et al. Use of fully threaded cannulated screws decreases femoral neck shortening after fixation of femoral neck fractures. Arch Orthop Trauma Surg. 2018;138:661–7. https://doi.org/10.1007/s00402-018-2896-y/metrics.
Gjertsen JE, Vinje T, Engesaeter LB, et al. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. JBJS. 2010;92(3):619–28. https://doi.org/10.2106/JBJS.H.01750.
He M, Han W, Zhao C, et al. Evaluation of a Bi-planar robot navigation system for insertion of cannulated screws in femoral neck fractures. Orthop Surg. 2019;11(3):373–9. https://doi.org/10.1111/os.12450.
Zhou L, Wang Y, Wang H, et al. Biplane orthopaedic robotic system assisted femoral neck fracture experimental study of internal fixation. Chinese J Orthop Trauma. 2009;11(2):147–51. https://doi.org/10.3760/cma.j.issn.1671-7600.2009.02.013.
Al-Naseem AO, Gonnah AR, Al-Ali H, et al. Robot-assisted versus conventional freehand fluoroscopy-guided percutaneous screw fixation in femoral neck fractures: a systematic review and meta-analysis. Cureus. 2022;14(4):e24258. https://doi.org/10.7759/cureus.24258.
Zheng Y, Yang J, Zhang F, et al. Robot-assisted vs freehand cannulated screw placement in femoral neck fractures surgery: a systematic review and meta-analysis. Medicine. 2021;100(20). https://doi.org/10.1097/MD.0000000000025926.
Arand M, Kinzl L, Gebhard F. Computer-guidance in percutaneous screw stabilization of the iliosacral joint. Clin Orthop Relat Res. 2004;422:201–7. https://doi.org/10.1097/01.blo.0000128644.46013.08.
Acknowledgements
The manuscript has been edited by Editage to ensure language and grammar accuracy and is errorfree in these aspects. Editing certificates have been uploaded in Supplemental material 2.
Funding
This work was supported by the National Key R&D Program Projects (2022YFC3601904); Tianjin Natural Science Foundation Key Projects (22JCZDJC00340); Tianjin Health Science and Technology Project(TJWJ2022QN053).
Author information
Authors and Affiliations
Contributions
YL and YW: conception and design, interpretation of the data, drafting, final approval; BD and PY: supervision, revision, final approval; : supervision, final approval; YS and LZ: conceptualisation, revision, final approval; JS: supervision, final approval; XM and JM: drafting, final approval. All authors have agreed to the final version to be published and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, Y., Wang, Y., Dong, B. et al. Comparison of rehabilitation outcomes between robot-assisted and freehand screw placement in treatment of femoral neck fractures: a systematic review and meta-analysis. BMC Musculoskelet Disord 25, 208 (2024). https://doi.org/10.1186/s12891-024-07325-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07325-0