Abstract
Background
Hip dysplasia is a condition where the acetabulum is too shallow to support the femoral head and is commonly considered a risk factor for hip osteoarthritis. The objective of this study was to develop a deep learning model to diagnose hip dysplasia from plain radiographs and classify dysplastic hips based on their severity.
Methods
We collected pelvic radiographs of 571 patients from two single-center cohorts and one multicenter cohort. The radiographs were split in half to create hip radiographs (n = 1022). One orthopaedic surgeon and one resident assessed the radiographs for hip dysplasia on either side. We used the center edge (CE) angle as the primary diagnostic criteria. Hips with a CE angle < 20°, 20° to 25°, and > 25° were labeled as dysplastic, borderline, and normal, respectively. The dysplastic hips were also classified with both Crowe and Hartofilakidis classification of dysplasia. The dataset was divided into train, validation, and test subsets using 80:10:10 split-ratio that were used to train two deep learning models to classify images into normal, borderline and (1) Crowe grade 1–4 or (2) Hartofilakidis grade 1–3. A pre-trained on Imagenet VGG16 convolutional neural network (CNN) was utilized by performing layer-wise fine-turning.
Results
Both models struggled with distinguishing between normal and borderline hips. However, achieved high accuracy (Model 1: 92.2% and Model 2: 83.3%) in distinguishing between normal/borderline vs. dysplastic hips. The overall accuracy of Model 1 was 68% and for Model 2 73.5%. Most misclassifications for the Crowe and Hartofilakidis classifications were +/- 1 class from the correct class.
Conclusions
This pilot study shows promising results that a deep learning model distinguish between normal and dysplastic hips with high accuracy. Future research and external validation are warranted regarding the ability of deep learning models to perform complex tasks such as identifying and classifying disorders using plain radiographs.
Level of Evidence
Diagnostic level IV
Similar content being viewed by others
Introduction
Hip dysplasia is a condition where the acetabulum is too shallow to support the femoral head, which can lead to subluxation or luxation of the femoral head and disrupted anatomy of the hip joint (Fig. 1). The biomechanics of a dysplastic hip joint can cause labrum tear and cartilage damage due to abnormal center of rotation and load distribution. Hip dysplasia is commonly considered a risk factor for hip osteoarthritis (OA) [1]. Surgical interventions such as periacetabular osteotomy, could affect hip OA development within this population. Hence, accurate and timely diagnosis of hip dysplasia is of utmost importance.
Congenital hip dysplasia is usually diagnosed during routine screening of newborns [2]. Hip dysplasia can also manifest later in life in adolescence. Plain radiographs of the pelvis and hip are the foundation of diagnosing adult hip dysplasia. A recent study found that among general radiologists (and thus among the reports to general practitioners), the diagnosis of most (93%) adult hip dysplasia goes unrecognized and hence untreated [3]. Furthermore, the agreement between individual orthopaedic specialists reading the same radiographs to diagnose hip dysplasia has been shown to be highly variable, with weighted kappa coefficients ranging from 0.43 to 0.93 [4,5,6] (from moderate to almost perfect agreement).
Moreover, the prevalence of hip dysplasia varies in different demographics from 1– 13% [7,8,9,10,11]. The relative rarity and demographic variation in the incidence of hip dysplasia also mean that orthopaedic practitioners are not equally familiar with the diagnosis and management of hip dysplasia. Currently, no tool is available to help orthopaedic practitioners with a better diagnosis of hip dysplasia.
Deep learning is a relatively new sub-category of artificial intelligence mainly concerned with image analysis and pattern recognition. In recent years deep learning models have been successfully used for automated image analysis and diagnosis of different orthopaedic disorders. These studies have focused on a myriad of orthopaedic disorders such as diagnosis of total hip replacement (THR) aseptic loosening, detecting the type of a THR implant prior to the revision surgery, diagnosing hard to detect tibiofemoral cartilage defects, and bone fracture detection and classification to name a few [12,13,14,15,16,17,18,19]. In most of these applications, deep learning models have achieved on-par or better performance compared to orthopaedic practitioners performing the same task. Despite these successful applications, no deep learning model has been developed so far to diagnose hip dysplasia from plain radiographs. Deep learning models may offer a solution to overcome the current challenges in the radiographic diagnosis of hip dysplasia and provide a valuable tool for reducing the inter-reader variability, enabling inexperienced practitioners to find dysplasia cases in larger cohorts, and standardizing the reporting of clinical outcomes of dysplasia patients based on disease severity. Hence, the objective of this study was to develop a deep learning model to diagnose hip dysplasia from plain radiographs and classify dysplastic hips based on their severity.
Methods
Study design
We conducted a retrospective study with institutional review board (IRB) approval, using previously collected imaging data. The study goal was to create and validate deep learning models for diagnosing hip dysplasia and classifying its severity from plain hip radiographs.
Data
Data sources
The following three data sources were used in this study:
-
1)
A prospective, international, multicenter study established in 2007, with the primary purpose of evaluating the outcomes of patients treated with total hip arthroplasty using vitamin-E infused highly cross-linked polyethylene liners [20]. The study consists of 16 centers in 8 countries.
-
2)
A retrospective single center cohort study from a Japanese hospital, with the primary purpose of studying outcomes following hip arthroplasty surgery.
-
3)
A retrospective single center cohort study from a Japanese hospital, with the primary purpose of studying dislocations following hip arthroplasty surgery.
All hospitals and the number of included hips are listed in Table 1. All patients were 18 years or older. Indication for all patients were degenerative joint disease, primary or secondary osteoarthritis. The contralateral hip was also assessed. We found no hips with Perthes disease, prior fracture or epiphysiolysis.
Ethics
For data source 1, written informed consent was collected for all participants in the clinical study. A separate IRB approval for continuing radiographic analysis exists, Partners Human Research, protocol no. 2007P001955. For data source 2 and 3, written informed consent was collected for all participants in the clinical study. IRB committee of Kanazawa Medical University. Receipt number: 134, date of approval: June 18, 2012.
Data preprocessing
The images existed in both JPEG and DICOM format. DICOM images were exported into JPEG format and kept as full-size images. All patient data was removed from the DICOMs. All images were anteroposterior pelvis radiographs that were subsequently cropped by a vertical split through the symphysis, creating two AP hip images. We only included the native hips and excluded hips with arthroplasty, prior osteotomy surgery, femoral head necrosis, and scanned radiographs with overlaying free-drawn preoperative planning templates and writing.
Ground truth
The most common radiographic measure to diagnose dysplasia is the acetabular center-edge (CE) angle (Fig. 2A) [21, 22]. The CE angle is the angle between a vertical line to the intra-teardrop line through the hip center and a line from the hip center to the boney lateral edge of the acetabulum. The CE angle measures the acetabular coverage of the femoral head. We used the original definition of the CE angle and measured the most lateral boney edge of the acetabulum. We used a matching circle on top of the femoral head to define the hip center. There is no universally accepted definition of hip dysplasia; however, a CE angle ≤ 20° is mostly considered dysplastic, whereas a CE angle between 20° − 25° is considered borderline, and a CE angle > 25° is considered normal [1, 23, 24].
To further expand the description of a dysplastic hip, the grade of subluxation can be classified. There are two such types of classification that are frequently used. The Crowe classification [25], established in 1979, uses the proportion of subluxation to divide disease severity into four classes:
-
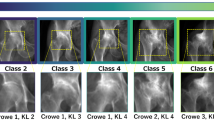
Crowe grade 1 corresponds to subluxation < 50% (Fig. 3A).
-
Crowe grade 2 subluxation between 50 and < 75% (Fig. 3B).
-
Crowe grade 3 subluxation between 75 and 100% (Fig. 3C).
-
Crowe grade 4 total luxation (Fig. 3D).
Hartofilakidis (HA) [26] classification categorizes dysplastic hips into three classes by considering the deformation of the acetabulum in addition to the degree of subluxation:
-
Dysplastic hip: The femoral head is contained within the original acetabulum despite the degree of subluxation (Fig. 3A & B).
-
Low dislocation: The femoral head articulates with a false acetabulum that partially covers the true acetabulum to a varying degree (Fig. 3C).
-
High dislocation: The femoral head is completely out of the true acetabulum and migrated superiorly and posteriorly to varying degrees (Fig. 3D).
The radiographs were reviewed by two reviewers (one orthopaedic surgeon, specialized in dysplastic hip surgery [ET] and one resident orthopaedic surgeon [MM]) that after a training session together, classified all images independently. All discrepant measurements were remeasured together, and the final grading was done in consensus. All hips were assessed for dysplasia by measuring the CE angle (Fig. 2A). First, using the DICOM viewer software (Horos v.3.3.6) the hip center was found for each radiograph by drawing a circle covering the femoral head. Then a horizontal line was drawn from teardrop to teardrop. The line was moved so that the end was over the circle’s center (the hip’s center). A new line was drawn from the hip’s center to the lateral edge of the acetabulum. Subsequently, the CE angle was calculated by subtracting 90 degrees from the angle between the two lines. In some hips (N = 10), the femoral head was too deformed to find the hip center, and for these hips, we relied on Sharp’s angle instead (Fig. 2B) [27]. A Sharp’s angle > 42° was defined as dysplastic. The CE angle is a well-established measure for hip dysplasia and was therefore chosen as the primary measure. Sharp’s angle is one of several other acetabular measures, and there is no global consensus on which is the most accurate in describing dysplasia. We chose Sharp’s angle as the secondary measure of dysplasia due to ease of measurement. Sharp’s angle is based on two easily identifiable anatomic features: the lateral acetabulum edge (the same lateral point used for the CE angle) and the teardrop. After categorizing the entire dataset into “Normal,” “Borderline,” and “Dysplastic,” we further categorized all the dysplastic hips based on both Crowe and Hartofilakidis classification. The Cohen’s Kappa [28] for interrater reliability was 0.596 for diagnosis of dysplasia (based on CE angle) before the final consensus-based grading.
Deep learning models description
Two deep learning models were developed as follows:
-
Model 1: To categorize all radiographs into Normal, Borderline, and Crowe 1 to 4 categories.
-
Model 2: To categorize all radiographs into Normal, Borderline, and HA 1 to 3 categories.
Both models had a VGG16 convolutional neural network (CNN) base structure pre-trained on the ImageNet dataset [29]. VGG16 model is widely used in literature for analyzing radiographs [30]. We modified the number of neurons in the classification layer of each model according to the number of classification categories (Model 1: 6 neurons, Model 2: 5 neurons). The models were adopted for the task at hand by using a layer-wise fine-turning strategy [30]. The dataset (total 1,022 radiographs; Table 1) was divided into train, validation, and test subset containing 816, 103, and 103 radiographs respectively maintaining the same ratio in each data subset [18]. Data augmentation was used with a similar strategy as our previous work [18] to create new data by applying a series of minor translations (e.g., rotation, magnification, etc.) on the training subset to create effectively 40,000 radiographs for training. The models were trained using Adam optimizer with cross entropy loss function, for 1,000 epochs with early stoppage accuracy improvement criteria, with a batch size of 32, and an initial learning rate of 0.0001. The validation subset was used for tuning the hyper-parameters, and the test subset was used to measure the models’ performance after training. Saliency maps were implemented to indicate the importance of each pixel of a given radiograph on the models’ performance [31]. This was done for two reasons:
-
1)
As a sanity check that the model does not use confounding data in the radiographs. One such example was Japanese letters in the Japanese radiographs that contained more dysplastic hips and subluxated hips.
-
2)
To visualize new features that the AI could potentially find for diagnosing and categorizing hip dysplasia.
Tensorflow r1.6 with Keras backend on a workstation comprised of an Intel(R) Xeon(R) Gold 6128 processor, 64GB of DDR4 RAM, and a NVIDIA Quadro P5000 graphic card was used to implement the models.
Results
Data
We included pelvic radiographs from 571 patients. After exclusion, the final dataset consisted of 1,022 hip radiographs. The excluded hips either had handwritten letters and preoperative templating or a total hip arthroplasty in place. The number of images and the distribution of different classes are summarized in Table 1.
Model performance
Table 2 summarizes Model 1 performance in classifying all radiographs in the test subset (103 radiographs) into Normal, Borderline, Crowe 1, Crowe 2, Crowe 3, and Crowe 4 classes. Model 1 diagnosed the normal hips with high accuracy (48 out of 51 correct classifications); however, it struggled to distinguish between Normal and Borderline hips and classified most of the Borderline hips as Normal (13 out of 15 Borderline hips were classified as Normal). On the other hand, Model 1 achieved high accuracy (92.2%) in distinguishing between dysplastic hips (Crowe 1–4) vs. Normal/Borderline hips. Considering the Crowe classification, most misclassification errors by the model were in the neighboring classes, i.e., +/- 1 Crowe classification error. Model 1 achieved an overall 68% accuracy.
Table 3 summarizes Model 2 performance in classifying all radiographs in the test subset (103 radiographs) into Normal, Borderline, HA 1, HA 2, and HA 3 classes. Model 2 also diagnosed the normal hips with high accuracy (41 out of 51 correct classifications); however, it struggled to distinguish between Normal and Borderline hips. On the other hand, Model 2 achieved high accuracy (83.3%) in distinguishing between dysplastic hips (HA 1–3) vs. Normal/ Borderline hips. Considering the HA classification, Model 2 also made +/- 1 HA classification error distinguishing between the neighboring classes. Model 2 achieved an overall 73.5% accuracy.
It is worth mentioning that while both Model 1 and Model 2 struggled to accurately identify the severity of dysplasia (Crowe and HA classification), they both achieved high performance in diagnosing a dysplastic hip (Normal/Borderline vs. Crowe 1–4/HA 1–3). Table 4 summarizes Model 1 performance in distinguishing between Normal/Borderline and Dysplastic hips.
Discussion
Main results
To the best of our knowledge, this is the first study to use deep learning to diagnose and classify the severity of hip dysplasia. In this study, we found that deep learning models trained on multicenter radiographs could classify hips into dysplastic or non-dysplastic with over 90% accuracy. These deep learning models were also successful in detecting the severity of hip dysplasia based on Crowe and HA classifications, where the most misclassifications were made in neighboring classes.
Strengths and limitations
A major strength of this study is the multicenter data source across different countries and healthcare institutions. By using multicenter radiographs, the models were externally validated and thereby are suitable for global use. Furthermore, the models learned to ignore the variations in how the radiographs were performed (some centers had higher consistency than others) as well as the patients’ demographics.
Another strength is that we used two reviewers for the data labeling. This gave us a measure of the dysplasia classification quality and how hard it is to classify dysplasia consistently. After the individual reviews, all discrepancies were adjusted with consensus between the two reviewers. Although this was a time-consuming process, it resulted in more objective labels than a single reviewer. The interrater agreement between the two reviewers was moderate for diagnosing dysplasia. Both reviewers found the measurement of the CE angle to be challenging. The main challenge was defining the most lateral boney point of the acetabular edge. Only a few millimeters difference in identifying that measurement point was enough to change the CE angle and hence the classification from borderline to dysplastic/normal.
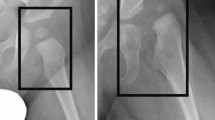
We tried to increase the understanding of the model by using saliency maps. Figure 4 shows examples of saliency maps for Normal/Borderline and Crowe 1–4 classifications. The saliency maps showed that the edge of the calcar region of the femur and its relation to the pelvic ring played an important role in the classification. This seems like a method resembling dysplasia classification by relying on Shenton’s line, which is a method that has high accuracy for determining femoral subluxation [32].
Furthermore, the model seemed to use the inferior cortex of the femoral neck arch and its relation to the inner and outer cortices of the pelvic ring (Fig. 5). For the more dysplastic hips that also had more femoral head deformity, the model seemed to recognize a narrower arch between the neck and the deformed head (Fig. 5, Crowe class 3). Although these interpretations are highly subjective and cannot be interpreted as a “logic” being used by the model, it is encouraging to see that the model learned to focus on relevant anatomical areas without any explicit training or “rules” to follow.
This study is limited by the use of plain anteroposterior hip radiographs. The three-dimensional anatomy of the acetabulum cannot be fully captured in a two-dimensional image. For instance, the pelvic tilt and rotation can affect the CE angle and would most probably impact radiographs classification as dysplastic, borderline, or Crowe 1. There is computer software (Hip2norm) available that can compensate for the pelvic position, but to the best of our knowledge, this software has not been validated to be used for dysplastic hips [33]. Furthermore, three-dimensional modalities such as computed tomography and magnetic resonance tomography can give a more comprehensive image of the acetabular anatomy; however, plain radiographs are still the most widely used imaging modality to assess the hip joint.
There is no global consensus on the definition of hip dysplasia, and there are many different ways to measure the CE angle. A surgeon might perform several measurements and supplement them with their overall impression of the hip anatomy to make a diagnosis. This method is not as reproducible as using a single measure but could be implemented in future studies as a more clinically relevant method to diagnose dysplasia.
The dataset’s size, and more specifically the distribution of higher Crowe grade hips, is somewhat limited in this study. This is due to the lower prevalence of totally dislocated hips since these patients are usually treated before the total collapse of the hip joint. While our study yields promising outcomes in employing deep learning for hip dysplasia diagnosis, it is crucial to acknowledge that it is a pilot study and the potential for selection bias, factors that may impact the generalizability of the results. Future research with larger and diverse datasets is needed for comprehensive validation and broader applicability.
Another observation made during this study was that Crowe class 1 includes a wide range of hips from slight dysplastic with a CE angle just below 20° to more severe dysplastic hips approaching Crowe class 2. The radiograph from a slight dysplastic hip looks entirely different from a hip with, e.g., 49% subluxation. This is evident even to a person that is not used to reviewing hip radiographs. The symptoms are probably different for these two examples as well; however, they both get classified as Crowe class 1. This further explains the models’ performance in classifying the severity of hip dysplasia that they made +/- 1 Crowe or HA classification error.
Generally, the application of deep learning in the classification of adult hip dysplasia is somewhat limited. Several smaller studies, each demonstrating varying degrees of accuracy, have been conducted. For instance, Jensen et al. suggested the potential utility of their algorithm in quantifying specific landmarks of hip dysplasia, although their study was limited in size and lacked precision [34]. In another study, Archer et al. illustrated that machine learning could offer a quick and cost-saving approach for assessing certain hip dysplasia parameters, with external validation. However, their model faced challenges in identifying anatomical landmarks and had a smaller sample size compared to ours [35].
Future implications
Hopefully, this study will encourage researchers to conduct more extensive studies with larger datasets resulting in a model with even higher performance. A similar model trained on a large dataset assessed and labeled in consensus by a global expert panel could in the future be used as a benchmark for hip dysplasia diagnosis and classification.
Conclusion
We have developed two deep learning models to diagnose and classify hip dysplasia, archiving high performances. These models could be used by professionals who lack relevant experience and in large cohorts for automatic diagnoses and classification of hip dysplasia. Timely diagnosis of hip dysplasia and subsequent conservative treatments could potentially delay the development of OA and the requirement of more aggressive treatments.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- AI:
-
Artifical Intelligence
- CE:
-
Center-Edge
- CNN:
-
Convolutional Neural Network
- HA:
-
Hartofilakidis
- IRB:
-
Institutional Review Board
- JPEG:
-
Join Photographic Expert Group
- OA:
-
Osteoarthritis
- THR:
-
Total Hip Replacement
References
Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B. Hip dysplasia and osteoarthrosis: a survey of 4151 subjects from the Osteoarthrosis Substudy of the Copenhagen City Heart Study. Acta Orthop. 2005;76(2):149–58.
Peled E, Eidelman M, Katzman A, Bialik V. Neonatal incidence of hip dysplasia: ten years of experience. Clin Orthop Relat Res. 2008;466(4):771–5.
Leide R, Wenger D, Overgaard S, Tiderius C, Rogmark C. Hip dysplasia is not uncommon but frequently overlooked: a cross-sectional study based on radiographic examination of 1,870 adults. ACTA ORTHOP 2021 (June 4): 1–6.
Decking R, Brunner A, Decking J, Puhl W, Günther KP. Reliability of the Crowe und Hartofilakidis classifications used in the assessment of the adult dysplastic hip. Skeletal Radiol. 2006;35(5):282–7.
Yiannakopoulos CK, Chougle A, Eskelinen A, Hodgkinson JP, Hartofilakidis G. Inter- and intra-observer variability of the Crowe and Hartofilakidis classification systems for congenital hip disease in adults. J Bone Joint Surg Br. 2008;90(5):579–83.
Clavé A, Kerboull L, Musset T, Flecher X, Huten D, Lefèvre C, et al. Comparison of the inter- and intra-observer reproducibility of the Crowe, Hartofilakidis and modified Cochin classification systems for the diagnosis of developmental dysplasia of the hip. Orthop Traumatol Surg Res. 2014;100(6 Suppl):323–6.
Croft P, Cooper C, Wickham C, Coggon D. Osteoarthritis of the hip and acetabular dysplasia. Ann Rheum Dis. 1991;50(5):308–10.
Inoue K, Wicart P, Kawasaki T, Huang J, Ushiyama T, Hukuda S, et al. Prevalence of hip osteoarthritis and acetabular dysplasia in French and Japanese adults. Rheumatology (Oxford). 2000;39(7):745–8.
Matsuda DK, Wolff AB, Nho SJ, Salvo JP, Christoforetti JJ, Kivlan BR, et al. Hip dysplasia: prevalence, Associated findings, and procedures from large Multicenter Arthroscopy Study Group. Arthroscopy. 2018;34(2):444–53.
Smith RW, Egger P, Coggon D, Cawley MI, Cooper C. Osteoarthritis of the hip joint and acetabular dysplasia in women. Ann Rheum Dis. 1995;54(3):179–81.
Engesæter IØ, Laborie LB, Lehmann TG, Fevang JM, Lie SA, Engesæter LB, et al. Prevalence of radiographic findings associated with hip dysplasia in a population-based cohort of 2081 19-year-old norwegians. Bone Joint J. 2013;95–B(2):279–85.
Olczak J, Fahlberg N, Maki A, Razavian AS, Jilert A, Stark A, et al. Artificial intelligence for analyzing orthopedic trauma radiographs. Acta Orthop. 2017;88(6):581–6.
Chung SW, Han SS, Lee JW, Oh KS, Kim NR, Yoon JP, et al. Automated detection and classification of the proximal humerus fracture by using deep learning algorithm. Acta Orthop. 2018;89(4):468–73.
Kim CY, Sivasundaram L, LaBelle MW, Trivedi NN, Liu RW, Gillespie RJ. Predicting adverse events, length of stay, and discharge disposition following shoulder arthroplasty: a comparison of the Elixhauser Comorbidity measure and Charlson Comorbidity Index. J Shoulder Elb Surg. 2018.
Gan K, Xu D, Lin Y, Shen Y, Zhang T, Hu K, et al. Artificial intelligence detection of distal radius fractures: a comparison between the convolutional neural network and professional assessments. Acta Orthop. 2019;90(4):394–400.
Borjali A, Chen AF, Muratoglu OK, Morid MA, Varadarajan KM. Detecting mechanical loosening of total hip replacement implant from plain radiograph using deep convolutional neural network. arXiv:191200943 [cs, eess] [Internet]. 2019 Dec 2 [cited 2020 Oct 28]; Available from: http://arxiv.org/abs/1912.00943.
Urakawa T, Tanaka Y, Goto S, Matsuzawa H, Watanabe K, Endo N. Detecting intertrochanteric hip fractures with orthopedist-level accuracy using a deep convolutional neural network. Skeletal Radiol. 2019;48(2):239–44.
Borjali A, Chen AF, Muratoglu OK, Morid MA, Varadarajan KM. Detecting total hip replacement prosthesis design on plain radiographs using deep convolutional neural network. J Orthop Res. 2020.
Borjali A, Magnéli M, Shin D, Malchau H, Muratoglu OK, Varadarajan KM. Natural language processing with deep learning for medical adverse event detection from free-text medical narratives: a case study of detecting total hip replacement dislocation. Comput Biol Med. 2020;129:104140.
Sillesen NH, Greene ME, Nebergall AK, Huddleston JI, Emerson R, Gebuhr P, et al. 3-year follow-up of a long-term registry-based multicentre study on vitamin E diffused polyethylene in total hip replacement. Hip Int. 2016;26(1):97–103.
Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. With special referance to the complication of osteoarthritis. 1939. (Acta Chir Scand. Suppl.).
Wiberg G. Shelf operation in congenital dysplasia of the acetabulum and in subluxation and dislocation of the hip. J Bone Joint Surg Am. 1953;35–A(1):65–80.
Fredensborg N. The CE angle of normal hips. Acta Orthop Scand. 1976;47(4):403–5.
Tönnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res. 1976;(119):39–47.
Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15–23.
Hartofilakidis G, Stamos K, Ioannidis TT. Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br. 1988;70(2):182–6.
Sharp IK. Acetabular dysplasia. J Bone Joint Surg Br Volume. 1961;43–B(2):268–72.
Cohen J. A coefficient of Agreement for Nominal scales. Educ Psychol Meas. 1960;20(1):37–46.
Li F-F. ImageNet: crowdsourcing, benchmarking & other cool things [Internet]. CMU VASC Seminar; 2010 Mar. Available from: http://www.image-net.org/papers/ImageNet_2010.pdf.
Morid MA, Borjali A, Del Fiol G. A scoping review of transfer learning research on medical image analysis using ImageNet. Comput Biol Med. 2021;128:104115.
Borjali A, Chen AF, Muratoglu OK, Morid MA, Varadarajan KM. Deep Learning in Orthopedics: How Do We Build Trust in the Machine? Healthcare Transformation [Internet]. 2020 Mar 30 [cited 2021 Jan 15]; Available from: https://www.liebertpub.com/doi/full/https://doi.org/10.1089/heat.2019.0006.
Rhee PC, Woodcock JA, Clohisy JC, Millis M, Sucato DJ, Beaulé PE, et al. The Shenton line in the diagnosis of acetabular dysplasia in the skeletally mature patient. J Bone Joint Surg Am. 2011;93(Suppl 2):35–9.
Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, et al. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–90.
Jensen J, Graumann O, Overgaard S, Gerke O, Lundemann M, Haubro MH, et al. A deep learning algorithm for Radiographic measurements of the hip in Adults—A reliability and agreement study. Diagnostics. 2022;12(11):2597.
Archer H, Reine S, Alshaikhsalama A, Wells J, Kohli A, Vazquez L, et al. Artificial intelligence-generated hip radiological measurements are fast and adequate for reliable assessment of hip dysplasia: an external validation study. Bone Jt Open. 2022;3(11):877–84.
Acknowledgements
We would like to thank David Shin for helping with data acquisition and cleaning.
Funding
The authors did not receive any external funds for this work and do not have any financial disclosures relevant to this study.
Open access funding provided by Karolinska Institute.
Author information
Authors and Affiliations
Contributions
MM collected, prepared, and labeled the data, contributed to the study design, and drafting of the manuscript. AB designed and ran the deep learning models, contributed to the study design, and drafting of the manuscript. ET labeled the data and revised the manuscript critically. MA revised the manuscript critically. HM, OM, and KV contributed to the design of the study and revised the manuscript critically.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
For data source 1, written informed consent was collected for all participants in the clinical study. A separate IRB approval for continuing radiographic analysis exists, Partners Human Research, protocol no. 2007P001955. For data source 2 and 3, written informed consent was collected for all participants in the clinical study. IRB committee of Kanazawa Medical University. Receipt number: 134, date of approval: June 18, 2012.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Magnéli, M., Borjali, A., Takahashi, E. et al. Application of deep learning for automated diagnosis and classification of hip dysplasia on plain radiographs. BMC Musculoskelet Disord 25, 117 (2024). https://doi.org/10.1186/s12891-024-07244-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07244-0