Abstract
Background
Physical activity is a guideline-recommended first-line intervention for people with knee osteoarthritis. Physical activity levels, and its potential correlates, is underexplored in Asian populations with knee osteoarthritis.
Methods
Participants enrolled in a longitudinal study in Singapore self-reported physical activity (UCLA activity score), function (Knee Osteoarthritis Outcome Score [KOOS-12]), kinesiophobia (Brief fear of movement [BFOM]), self-efficacy (ASES-8), and quality of life (EQ-5D-5 L). One-Way ANOVA was used to test the difference in outcomes between UCLA categories, while ordinal logistic regression was used to identify the associated factors to physical activity level.
Results
Seventy-three percent of all enrolled participants (n = 311/425) reported either inactivity or low physical activity (median 4, IQR 3–5). Significant, weak, positive correlations were observed be-tween UCLA activity score and either KOOS-12 (Spearman’s rho: 0.1961; p < 0.001), ASES-8 (0.1983; p = 0.004), or EQ-5D-5 L (0.2078; p < 0.001). A significant, weak, negative correlation was observed between physical activity and BFOM (-0.2183; p < 0.001). Significant differences in function between groups (moderate vs. inactive or low physical activity) were not clinically important. Participants with obesity, from the eldest age category (i.e. ≥75), or who identified as Malay or female, were less physically active than those with a healthy BMI, below the age of 54, or who identified as Chinese or male, respectively.
Conclusion
Healthcare professionals in Asia should be aware of the large proportion of people with knee osteoarthritis who are either inactive or have low physical activity levels. Screening for, and offering interventions to promote, physical activity and its correlates should be prioritised.
Similar content being viewed by others
Background
Knee osteoarthritis is a leading cause of disability worldwide [1], with symptomatic knee osteoarthritis affecting up to one in ten people over the age of 50 in Asia [2]. Personal and societal burdens related to knee osteoarthritis are predicted to rise significantly in the next decade, in part due to ageing populations, but also due to increased levels of obesity and physical inactivity/sedentary lifestyles [3, 4].
Physical inactivity for adults and older adults is defined as a failure to complete 150 min of moderate to vigorous physical activity across five or more days [5]. Physical inactivity is a modifiable risk factor for the development [6, 7] and progression [8, 9] of knee osteoarthritis. Conversely, physical activity is effective at reducing pain, and increasing function, performance and health related quality of life for people with knee osteoarthritis [10, 11]. Consequently, all major clinical practice guidelines for people with knee osteoarthritis advocate physical activity as first-line care alongside education, exercise therapy and, when appropriate, weight management [12,13,14,15]. Despite this, a recent systematic review estimated that just 13% of people with knee osteoarthritis meet current international physical activity guidelines [16]. However, it is worth noting that this review was heavily influenced by research in Western countries, with just 2 of the 27 included studies being performed in Asia [17, 18]. Further, both of these studies were performed in small, female only populations in Japan, representing just 55 participants out of the 3266 included. As such, further research is required to ascertain whether these estimates of physical activity/inactivity are representative of Asian populations with knee osteoarthritis outside of Japan.
Previous research has identified a number of factors that influence engagement with physical activity for people with knee osteoarthritis, namely increased age, non-white ethnicity, increased osteoarthritis symptoms, and female gender [19]. However, these findings are also informed primarily from trials performed in Western populations with just 2 of the 29 trials being performed in Asia (Japan) [20, 21]. Other factors such as kinesiophobia [22] and self-efficacy [23] may also contribute towards lower physical activity levels of people with knee osteoarthritis and are again underexplored in Asian populations. Research is therefore urgently needed to better understand physical activity and its potential correlates for Asian populations with knee osteoarthritis. Identification of this will help to inform targeted interventions to increase physical activity for people with knee osteoarthritis and facilitate subsequent improvements in patient outcomes, health and quality of life.
This study aims to identify the self-reported physical activity levels of a multi-cultural Asian group of people seeking care for knee osteoarthritis. We also aim to explore the relationship of self-reported physical activity with self-reported function, kinesiophobia, self-efficacy and quality of life.
Methods
Study design
This study analyzed baseline data collected as part of a pre-registered (clinicaltrials.gov, NCT04942236 first registered 28/06/2021) multi-center, prospective cohort study for people with knee osteoarthritis in Singapore [24]. This study is reported following the STROBE guidelines [25].
Ethical approval
Ethical approval was provided by the National Healthcare Group Domain Specific Review Board in Singapore (NHG DSRB; Reference number: WHC/2020-00076).
Participants and recruitment
Participants were recruited to the main multi-center, prospective cohort study between July 2020 and January 2022 when they presented for treatment at either the orthopedic or physiotherapy clinics at hospitals within the National Healthcare Group of Singapore (Tan Tock Seng Hospital and Khoo Teck Puat Hospital). Participants were eligible for the study if they met the NICE clinical diagnostic criteria for knee osteoarthritis [13] (i.e., they were i. are aged 45 or over, ii. have activity-related joint pain and, iii. have either no morning joint-related stiffness or morning stiffness that lasts no longer than 30 minutes) and they were independent community mobilisers (with or without walking aids). Participants were excluded if they had an alternative diagnosis for their knee symptoms (e.g., referred pain from hip/spine), had secondary arthritis (e.g., inflammatory), were unable to comply with the study protocol (e.g., significant cognitive impairment) or had severe medical comorbidities impairing activities of daily living (e.g., COPD on long-term oxygen therapy, cardiac failure with significantly impaired effort tolerance, stroke with significant residual functional weakness). Those who had received a previous knee arthroplasty, were wheelchair bound or who were pregnant, were also excluded from participating in the study. Potentially eligible participants were initially identified by pre-screening the relevant clinic appointment lists and/or accessing patients’ e-medical records. In an attempt to reduce persuasion from the participants primary care giver at the appointment, eligible participants were then approached by a study coordinator during the clinic visit to share and explain details about the study. Written consent was obtained from interested participants prior to enrolment.
Upon enrollment, participants provided demographic details and completed a number of self-reported outcome measures using either a hard copy form during the clinic visit itself, or via a self-administered online form (FormSG), which the participant completed at their own convenience. Demographic details included age, gender, ethnicity, Body Mass Index (BMI), employment status, education level and whether they presented with unilateral or bilateral knee symptoms.
Outcomes
This study used baseline scores for the Knee Osteoarthritis Outcome Score (KOOS-12) [26], UCLA activity scale (1-10 version) [27], Arthritis Self-Efficacy Scale (ASES-8) [28], Brief Fear of Movement (BFOM) questionnaire [29] and the EQ-5D-5L [30]. These outcomes were selected primarily due to their frequent use in research for people with knee osteoarthritis [29, 31,32,33,34,35,36], but also due to the availability of valid and reliable English and Chinese versions of the outcomes [37,38,39,40,41]. The default language for outcomes was English, however, we used the Chinese versions when necessary (i.e. the participant did not speak English). The KOOS-12 is a 12-item, 4-domain assessment tool measuring participants’ perception of their knee function. Domains include pain, function and daily living, and quality of life, and are measured using 5-point Likert scales from 0 to 4, with 4 questions per domain [26]. Questions in each domain are used to calculate summative scores, with higher scores indicating more optimal outcomes. The UCLA activity score is a scale that assesses the self-reported physical activity level of a participant based upon 10 descriptive activity levels [27]. Higher scores indicate increased levels of physical activity. The ASES-8 assesses participant’s confidence in performing certain daily tasks [28]. Summative scores indicate the level of self-efficacy the participant has in managing their arthritis, with higher scores indicating higher levels of self-efficacy. The BFOM questionnaire assesses the fear of movement that the participant experiences [29]. The questionnaire consists of six questions with a 4-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). A summative score of the six questions is computed, with higher score indicating greater fear of movement. The EQ-5D-5L questionnaire is commonly used to assess quality of life and consisting of 5 domains (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) [30]. Each dimension contains 5 levels, from no problem to extreme problems. Relevant permission was granted for the use of the EQ-5D-5L and we used generated utility values for the outcome based on the Singapore value set provided by previous research [42].
Sample size
Sample size was calculated using STATA version 14.0 (STATACorp. 2015. Stata Statistical Software: Released 14. College Station, TX: StataCorp LP). As a weak correlation has been observed between the UCLA activity score and the KOOS-12 [43], sample size was estimated based on a correlation coefficient of 0.15 to produce a sample size that would be powered enough to detect even weak correlations between UCLA and KOOS-12, ASES-8, BFOM and EQ-5D-5L [44]. We therefore required data for a minimum of 347 participants considering 0.05 type I error and 80% power of study.
Data analysis and representation
At the time of data analysis, all recruited participants to the main longitudinal cohort study were included in data analysis, and complete case analysis was used as the missing data percentage was low and ignorable (<2.8%). Participant demographic and outcome measure responses were de-identified, given a unique identifier number and stored on a secure web-based application widely used for clinical data management in research (Research Electronic Data Capture [REDCAP]). Data were cleaned and analyzed by one member of the research team (LCJ), using SPSS version 26.0. The distribution of continuous variables were checked using skewness, kurtosis and histogram, and data were deemed to be normally distributed with skewness and kurtosis of between -2 and 2, as well as an approximately bell shaped histogram.
Descriptive statistics were used to summarize the participant demographics and raw UCLA activity scores (presented as median, 25th percentile; 75th percentile due to the ordinal nature of the outcome) and for determining correlations with KOOS-12, ASES-8, BFOM and EQ-5D-5L using Spearman’s correlation tests. In alignment with previous research for people with knee osteoarthritis [45], UCLA activity scores were also categorized to one of the following five domains; inactive (1-2), low physical activity level (3-4), moderate physical activity level (5-6), high physical activity level (7-8) and, very high activity level (9-10). The proportion (%) of people categorized to each level of physical activity was calculated, plus the difference in KOOS-12, ASES-8, BFOM and EQ-5D-5L between patients with different physical levels were tested using One Way ANOVA. Post-hoc pairwise comparison with Bonferroni or Dunnet C correction following the significance of One Way ANOVA was used to determine where the significant difference truly came from. Statistical significance was denoted as p< 0.05 throughout. Mean difference (MD) between different physical activity levels was compared against previously published Minimum Clinically Important Differences (MCID) for the KOOS-12 (MCID = 11.1) [46].
Ordinal logistic regression analyses were performed to identify factors associated with UCLA activity score. In line with previous research [47, 48], we used BMI categories specific to Asian populations for regression analyses (Healthy <23kg/m [2], Overweight 23-27.4kg/m2, Obesity ≥27.5 kg/m2) [49]. Univariable analysis was used to determine significant factors associated with physical activity. Variables with a p value less than 0.200 in the univariable analysis [50] were included into the multivariable model using stepwise variable selection process with ‘xi’ command from STATA package to expand the categorical variables into indicator variables. Multicollinearity of the final model was also tested. Finally, cross tabulation analyses were performed (either Fisher extract or Pearson’s Chi Squared test) to check for the association between categorical variables. The assumptions for various tests were checked before proceeding to the respective analysis to ensure they were fulfilled, and statistical significance was denoted as p< 0.05 throughout.
Results
Four hundred and twenty-five participants were enrolled in our study. Availability of data for each outcome, plus participant demographics are presented in Table 1. Mean age of participants was 63.59 (standard deviation [SD] 7.97) and BMI was 26.77 kg/m2 (SD 5.11). Median UCLA activity score was 4 (inter quartile range [IQR] 3-5). The number and proportion of participants for each category of the 1-10 UCLA activity score are presented in Table 2. See Additional file 1 (Table S1) for more details.
Correlates of raw (0-10) UCLA activity score to self-reported function, kinesiophobia, self-efficacy and quality of life
Significant, weak, positive correlations were observed between UCLA activity score and KOOS-12 (Spearman’s rho: 0.1961; p< 0.001), ASES-8 (0.1983; p= 0.004) and EQ-5D-5L (0.2078; p< 0.001). A significant, weak, negative correlation was observed between UCLA and the BFOM (-0.2183; p< 0.001). Refer to Fig. 1 (A-D) for more details.
Categorization of UCLA activity score
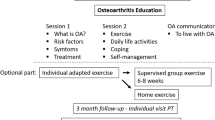
The proportion of people with knee osteoarthritis being classified as inactive or having low, moderate, high or very high physical activity levels are presented in Fig. 2. Most participants self-reported low physical activity levels (n=265/425, 62.35%).
Proportion (%) of people with knee osteoarthritis being categorized as inactive or having low, moderate, high or very high physical activity levels using the UCLA activity scor
BMI = Body Mass Index, OA = Osteoarthritis, Inactive = 1-2 on UCLA activity score, Low = 3-4 on UCLA activity score, Moderate = 5-6 on UCLA activity score, High = 7-8 on UCLA activity score, Very high = 9-10 on UCLA activity scoree
Correlates of categorized UCLA activity score to self-reported function, kinesiophobia, self-efficacy and quality of life
Comparisons of mean and standard deviation scores between differing UCLA activity score categorizations are presented in Table 3. Significant differences were observed between physical activity level and KOOS-12, EQ-5D-5L and BFOM (p< 0.05). Post-hoc pairwise comparison with Bonferroni correction was performed for KOOS-12 and for BFOM. For KOOS-12, participants with moderate physical activity level had significantly higher, but clinically unimportant differences (i.e., MD = <11.1 [46]), in KOOS-12 than those who are either inactive (mean difference [MD], 95% CI: 10.19, 2.27 to 18.16) or had low physical activity level (MD, 95% CI; 6.22, 0.87 to 11.56). For BFOM, participants with moderate physical activity level had significantly lower BFOM scores compared to inactive participants (MD, 95% CI: -3.18, -5.79 to -0.57). Post-hoc pairwise comparison with Dunnett C was performed for EQ-5D-5L as the homogeneity of variance was not met. For EQ-5D-5L, participants with moderate physical activity levels had significantly higher EQ-5D-5L compared to those who were either inactive (MD, 95% CI: 0.24, 0.05 to 0.44), or had low physical activity levels (MD, 95% CI: 0.10, 0.01 to 0.19). Participants with very high physical activity level had a significantly higher EQ-5D-5L compared to those who were inactive (MD, 95% CI: 0.42, 0.22 to 0.62), or who had low (MD, 95% CI: 0.27, 0.17 to 0.38) or moderate physical activity levels (MD, 95% CI: 0.17, 0.05 to 0.29). See Additional file 1 (Tables S2, S3, S4) for more details.
Regression analyses and cross tabulation
Ordinal logistic regression analyses of physical activity are presented in Table 4. In summary, participants with obesity, from the eldest age category (i.e. ≥75), or who identified as Malay or female, were less physically active compared to those who had a healthy BMI (adj OR, 95% CI: 0.47, 0.30 to 0.74), were below the age of 54 (adj OR, 95% CI: 0.29, 0.14 to 0.60), or who identified as Chinese (adj OR, 95% CI: 0.44, 0.22 to 0.88) or male (adj OR, 95% CI: 0.46, 0.29 to 0.73), respectively. Additionally, those with high KOOS12 score (adj OR, 95% CI: 1.98, 1.26 to 3.13), or had a diploma (adj OR, 95% CI: 1.85, 1.05 to 3.27) or university level education (adj OR, 95% CI: 2.26, 1.23 to 4.15) had higher physical activity compared to those with low KOOS12 score or with informal education, respectively. There were less participants aged over 75 years of age in the Malay group, compared to other groups (p= 0.002). Further details of cross tabulations are presented in Tables S5 & S6 in Additional file 1.
Discussion
This study offers novel insights into self-reported physical activity levels, and its correlates, for a multi-cultural Asian population of people with knee osteoarthritis who are seeking care. Most participants were categorized as having low physical activity levels, and those with obesity, from the eldest age category (i.e., ≥75), or who identified as Malay or female, were less physically active than those with a healthy BMI, younger (<54 years old), Chinese and males, respectively. We observed a significant, but weak, positive correlation between physical activity level and function, and statistically significant differences in function between those categorized as having moderate physical activity levels, compared to those who are either inactive or who have low physical activity levels. However, differences in function between groups may not be clinically important. We also observed significant, but weak, correlations between physical activity level and either kinesiophobia, self-efficacy or quality of life. Further exploration of these relationships is warranted to identify whether interventions targeting factors such as kinesiophobia and self-efficacy improve physical activity, or whether improvements in physical activity reduces kinesiophobia and improves quality of life. Understanding this further has great potential to facilitate creation of cost-effective, non-surgical interventions to improve symptoms, function, quality of life and health for people with knee osteoarthritis.
Inadequate physical activity levels of an Asian population seeking care for knee osteoarthritis
Consistent with research around the world [16, 51], three-quarters of participants in our study reported being either inactive or having low physical activity levels. Therefore, the majority are not optimally engaging with guideline-recommended first-line care for the management of knee osteoarthritis [12,13,14,15]. Engaging in, or increasing level of, physical activity for people with knee osteoarthrosis is recommended due to its potential to improve symptoms, function, joint health and overall health, whilst minimizing the personal and societal burdens they create [11, 52]. Healthcare professionals should therefore routinely be screening for, and offer interventions to facilitate improvements in, physical activity for people with knee osteoarthritis. However, evidence indicates that healthcare professionals are failing to implement this clinically, as many people with knee osteoarthritis fail to receive physical activity and lifestyle advice prior to orthopedic or physiotherapy consultations [53,54,55]. Our findings may support this notion considering that participants would have already attended a primary healthcare consultation prior to being referred to an orthopedic surgeon or physiotherapist for enrollment in the study, yet still reported low physical activity levels. A lack of knowledge, confidence, skills, time and/or resources have all been identified as potential barriers to screening for, and provision of, physical activity interventions by healthcare professionals outside of Asia [56,57,58,59,60]. Exploration of the barriers and enablers to the provision of physical activity interventions by healthcare professionals in Asia is warranted to improve implementation of guideline-recommended first-line care.
Participants with obesity, from the eldest age category (i.e., ≥75), or who identified as Malay or female, were less physically active than those with a healthy BMI, younger (<54 years old), or who identified as Chinese or male, respectively. These findings align to previous research for people with, and without, knee osteoarthritis [19, 61]. Future research is warranted to understand why certain sub-populations were less physically active considering that physical activity is recommended for all people with knee osteoarthritis regardless of comorbidities, age, gender or race [13]. Conscious or unconscious attitudes and biases of people with knee osteoarthritis, or by healthcare professionals, may contribute towards engagement in, or the quality and provision of, physical activity interventions. For example, weight stigma [62], ageism [63] and beliefs that osteoarthritis is a ‘wear and tear’ condition [64] are potential barriers to physical activity, and these may all contribute to lower perceived levels of physical activity. However, investigation of such factors is underexplored in Asia. We recommend that future physical activity interventions and initiatives are co-designed in collaboration with diverse groups of people with knee osteoarthritis, and healthcare professionals, to reduce implementation and engagement barriers.
Relationship between physical activity and function, kinesiophobia, self-efficacy and quality of life
Supporting previous findings in Western and Caucasian populations with knee osteoarthritis [22, 23], lower physical activity levels of people in our study were correlated with increased self-reported function and kinesiophobia, plus decreased self-efficacy and quality of life. The relationship between physical activity and these outcomes is complex and may be partially underpinned by common inaccurate beliefs about symptoms, the condition and its management [65, 66]. For example, people with knee osteoarthritis commonly believe that; i) pain is a sign of increasing damage, ii) physical activity will ‘wear down’ their joints or, iii) that surgery is inevitable [64, 67, 68]. Such beliefs may be due to pervasive inaccurate online information about the condition and its management [69], and be exacerbated by common misconceptions of healthcare professionals [64, 70]. When viewed through a fear avoidance model lens [65], these beliefs have the potential to contribute towards decreased function, catastrophizing of symptoms, kinesiophobia and a decrease in one’s self-efficacy for, and engagement in, physical activity. This in turn may reduce an individual with knee osteoarthritis’ quality of life.
Combining education with physical activity/exercise therapy interventions is more effective than providing the physical activity/exercise therapy intervention alone for improving physical activity, symptoms, self-efficacy, psychological distress and quality of life for people with knee osteoarthritis [32, 71,72,73]. Future physical activity interventions for people with knee osteoarthritis are therefore encouraged to include education to empower positive attitudes and behaviors towards active lifestyles, including dispelling common misconceptions that physical activity or exercise therapy is unsafe or harmful [67].
Additionally, initiatives to improve knowledge of, and promote screening for, psychological factors such kinesiophobia and self-efficacy by healthcare professionals is encouraged. This will allow the early identification of higher risk, psychologically vulnerable patients and facilitate the provision of targeted interventions to address these psychological factors and subsequent reductions in physical activity.
Limitations and future directions
To our knowledge this is the first investigation of self-reported physical activity and its possible correlates for an Asian population with knee osteoarthritis. The large proportion of people with knee osteoarthritis who self-report inactivity or low levels of physical activity is consistent with previous literature in Western populations [16, 51] and should be cause for concern. However, our results may not be representative of all Asian communities with knee osteoarthritis. For example, we cannot assume that all Malay communities throughout Asia will be less physically active compared to Chinese communities. Our findings are therefore limited to Singapore’s highly urbanized and multiethnic population. It is also important to note that although the UCLA activity score is widely used in knee osteoarthritis research and has been demonstrated to have a strong correlation to average steps per day [27, 74], it is not an objective measure of physical activity. Therefore, there may be a discrepancy between participants perceived and actual physical activity. Additionally, recruitment to our study occurred during the COVID-19 pandemic when rates of inactivity may have been at their highest due to national level restrictions [75]. Future research involving both self-reported and objective measures of physical activity may be required to confirm our findings at a time when COVID-19 restrictions are no longer in enforcement. We did not identify the presence, or stage, of radiographic osteoarthritis for enrolled participants. Although conflicting evidence exists regarding stage of radiographic osteoarthritis and its association to outcomes including pain, function and physical activity [76,77,78,79,80], we cannot determine whether this was an important factor, or correlate of physical activity, for our study population. Future research is encouraged to explore the relationship of radiographic osteoarthritis and physical activity levels within Asian populations.
Due to the nature of our study, we cannot determine whether lower self-reported physical activity levels cause/result in worse self-reported outcomes, or whether worse self-reported outcomes cause/result in lower self-reported physical activity levels. The collection of longitudinal data is encouraged to determine any relationship between, and changes within, physical activity level and outcomes such as kinesiophobia, self-efficacy and quality of life. It is also important to note that this study only explored person-level correlates of physical activity. However, social and environmental factors are also known to influence physical activity levels [81]. Research investigating social and environmental correlates of physical activity are again under explored with Asian populations [82] and should be prioritised in future.
Conclusion
Three quarters of people with knee osteoarthritis seeking care in our study reported being inactive or having low physical activity levels. Future research is encouraged to understand barriers and enablers to increasing physical activity from both an individual with knee osteoarthritis’ and from a healthcare professional's viewpoint. Co-designing and implementing interventions to increase engagement in physical activity has great potential to improve symptoms, function, health, and quality of life for the majority of people with knee osteoarthritis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASES:
-
Arthritis self-efficacy scale
- BFOM:
-
Brief fear of movement
- BMI:
-
Body Mass Index
- KOOS:
-
Knee Osteoarthritis Outcome Score
References
Safiri S, Kolahi A-A, Smith E, Hill C, Bettampadi D, Mansournia MA, Hoy D, Ashrafi-Asgarabad A, Sepidarkish M, Almasi-Hashiani A. Global, regional and national burden of osteoarthritis 1990–2017: a systematic analysis of the global burden of Disease Study 2017. Ann Rheum Dis. 2020;79(6):819–28.
Leung YY, Ma S, Noviani M, Wong SBS, Lee CM, Soh IAL, Thumboo J. Validation of screening questionnaires for evaluation of knee osteoarthritis prevalence in the general population of Singapore. Int J Rheum Dis. 2018;21(3):629–38.
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, Bridgett L, Williams S, Guillemin F, Hill CL. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73(7):1323–30.
Ackerman IN, Bohensky MA, Zomer E, Tacey M, Gorelik A, Brand CA, De Steiger R. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord. 2019;20(1):90.
Australian-Institute-of-Health-and-Welfare-(AIHW), available at https://www.aihw.gov.au/reports/risk-factors/insufficient-physical-activity/contents/insufficient-physical-activity.
Wallace IJ, Worthington S, Felson DT, Jurmain RD, Wren KT, Maijanen H, Woods RJ, Lieberman DE. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci. 2017;114(35):9332–6.
Whittaker JL, Runhaar J, Bierma-Zeinstra S, Roos EM. A lifespan approach to osteoarthritis prevention. Osteoarthr Cartil. 2021;29(12):1638–53.
Simic M, Harmer AR, Agaliotis M, Nairn L, Bridgett L, March L, Votrubec M, Edmonds J, Woodward M, Day R. Clinical risk factors associated with radiographic osteoarthritis progression among people with knee pain: a longitudinal study. Arthritis Res Therapy. 2021;23(1):1–10.
Zhu J, Chen W, Hu Y, Qu Y, Yang H, Zeng Y, Hou C, Ge F, Zhou Z, Song H. Physical activity patterns, genetic susceptibility, and risk of hip/knee osteoarthritis: a prospective cohort study based on the UK Biobank. Osteoarthritis Cartilage. 2022;30(8):1079–90.
Peprah K, Argáez C. Physical Activity for Chronic Osteoarthritic Knee Pain: A Review of Clinical Effectiveness. CADTH Rapid Response Report: Summary with Critical Appraisal. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. 2020; p. 1–22.
Kraus VB, Sprow K, Powell KE, Buchner D, Bloodgood B, Piercy K, George SM, Kraus WE. Effects of physical activity in knee and hip osteoarthritis: a systematic Umbrella Review. Med Sci Sports Exerc. 2019;51(6):1324–39.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, Callahan L, Copenhaver C, Dodge C, Felson D. 2019 American College of Rheumatology/Arthritis Foundation guideline for the management of osteoarthritis of the hand, hip, and knee. Arthritis Rheumatol. 2020;72(2):220–33.
National Institute for Health and Care Excellence (NICE). London: Osteoarthritis: Care and Management in Adults; 2014.
Fernandes L, Hagen KB, Bijlsma JW, Andreassen O, Christensen P, Conaghan PG, Doherty M, Geenen R, Hammond A, Kjeken. I., EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125–35.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, Kraus VB, Lohmander LS, Abbott JH, Bhandari M, Blanco FJ, Espinosa R, Haugen IK, Lin J, Mandl LA, Moilanen E, Nakamura N, Snyder-Mackler L, Trojian T, Underwood M, McAlindon TE. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartilage. 2019;27(11):1578–89.
Wallis J, Webster K, Levinger P, Taylor N. What proportion of people with hip and knee osteoarthritis meet physical activity guidelines? A systematic review and meta-analysis. Osteoarthr Cartil. 2013;21(11):1648–59.
Watanabe H, Urabe K, Takahira N, Ikeda N, Fujita M, Obara S, Hendona T, Aikawa J, Itoman M. Quality of life, knee function, and physical activity in Japanese elderly women with early-stage knee osteoarthritis. J Orthop Surg. 2010;18(1):31–4.
Michishita R, Shono N, Kasahara T, Katoku M, Tsuruta T. The possible influence of osteoarthritis of the knee on the accumulation of coronary risk factors in postmenopausal obese women. Obes Res Clin Pract. 2008;2(1):29–34.
Stubbs B, Hurley M, Smith T. What are the factors that influence physical activity participation in adults with knee and hip osteoarthritis? A systematic review of physical activity correlates. Clin Rehabil. 2015;29(1):80–94.
Hirata S, Ono R, Yamada M, Takikawa S, Nishiyama T, Hasuda K, Kurosaka M. Ambulatory physical activity, disease severity, and employment status in adult women with osteoarthritis of the hip. J Rhuematol. 2006;33(5):939–45.
Yokochi M, Watanabe T, Ida K, Yoshida K, Sato Y. Effects of physical exercise prescribed by a medical support team on elderly lower extremity osteoarthritis combined with metabolic syndrome and/or type 2 diabetes. Geriatr Gerontol Int. 2012;12(3):446–53.
Aykut Selçuk M, Karakoyun A. Is there a relationship between kinesiophobia and physical activity level in patients with knee osteoarthritis? Pain Med. 2020;21(12):3458–69.
Degerstedt Å, Alinaghizadeh H, Thorstensson CA, Olsson CB. High self-efficacy–a predictor of reduced pain and higher levels of physical activity among patients with osteoarthritis: an observational study. BMC Musculoskelet Disord. 2020;21(1):1–13.
Tan BY, Goh ZZS, Lim CJ, Pereira MJ, Yang SY, Tan KG, Tan ACK, Liang P, Abbott JH, Briggs AM, Hunter DJ, Skou ST, Thumboo J, Car J. Singapore KneE osTeoarthritis CoHort (SKETCH): protocol for a multi-centre prospective cohort study. BMC Musculoskelet Disord. 2023;24(1):104.
Cuschieri S. The STROBE guidelines. Saudi J Anaesth. 2019;13(Suppl 1):31.
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96.
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–5.
Brady TJ. Measures of self-efficacy: arthritis self‐efficacy scale (ASES), Arthritis Self‐Efficacy Scale‐8 item (ASES‐8), Children’s arthritis self‐efficacy scale (CASE), Chronic Disease Self‐Efficacy Scale (CDSES), parent’s arthritis self‐efficacy scale (PASE), and Rheumatoid Arthritis Self‐Efficacy Scale (RASE). Arthritis Care Res. 2011;63(S11):473–S485.
Shelby RA, Somers TJ, Keefe FJ, DeVellis BM, Patterson C, Renner JB, Jordan JM. Brief fear of movement scale for osteoarthritis. Arthritis Care Res. 2012;64(6):862–71.
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res. 2011;20(10):1727–36.
Terwee C, Bouwmeester W, Van Elsland S, De Vet H, Dekker J. Instruments to assess physical activity in patients with osteoarthritis of the hip or knee: a systematic review of measurement properties. Osteoarthr Cartil. 2011;19(6):620–33.
Martinez-Calderon J, Flores-Cortes M, Morales-Asencio JM, Pineda-Galán C, García-Rios MC, Torrontegui-Duarte M, Luque-Suarez A. Is it possible to Reduce Pain-related fear in individuals with knee osteoarthritis? A systematic review of Randomised clinical trials. Physiother Theory Pract. 2023;39(6):1106–32.
Brand E, Nyland J, Henzman C, Mcginnis M. Arthritis self-efficacy scale scores in knee osteoarthritis: a systematic review and meta-analysis comparing arthritis self-management education with or without exercise. J Orthop Sports Phys Ther. 2013;43(12):895–910.
Bilbao A, García-Pérez L, Arenaza JC, García I, Ariza-Cardiel G, Trujillo-Martín E, Forjaz MJ, Martín-Fernández J. Psychometric properties of the EQ-5D-5L in patients with hip or knee osteoarthritis: reliability, validity and responsiveness. Qual Life Res. 2018;27(11):2897–908.
Wilcox S, Schoffman DE, Dowda M, Sharpe PA. Psychometric properties of the 8-item english arthritis self-efficacy scale in a diverse sample. Arthritis. 2014;2014:385256.
Huang CC, Chen WS, Tsai MW, Wang WT. Comparing the Chinese versions of two knee-specific questionnaires (IKDC and KOOS): reliability, validity, and responsiveness. Health Qual Life Outcomes. 2017;15(1):238.
Xia J, Wu N-W, Ma T-P, Yu C, Li N-X. [Evaluation of reliability and validity of EQ-5D-5L based on residents in Southwest China]. Sichuan Da Xue Xue Bao Yi Xue Ban. 2020;51(5):691–4.
Xie F, Li SC, Roos EM, Fong KY, Lo NN, Yeo SJ, Yang KY, Yeo W, Chong HC, Thumboo J. Cross-cultural adaptation and validation of Singapore English and Chinese versions of the knee injury and osteoarthritis outcome score (KOOS) in asians with knee osteoarthritis in Singapore. Osteoarthritis Cartilage. 2006;14(11):1098–103.
Wong WS, Kwok HY, Luk KD, Chow YF, Mak KH, Tam BK, Wong ET, Fielding R. Fear of movement/(re)injury in Chinese patients with chronic pain: factorial validity of the Chinese version of the Tampa Scale for Kinesiophobia. J Rehabil Med. 2010;42(7):620–9.
Cao S, Liu N, Li L, Lv H, Chen Y, Qian Q. Simplified Chinese version of University of California at Los Angeles Activity Score for Arthroplasty and Arthroscopy: cross-cultural adaptation and validation. J Arthroplasty. 2017;32(9):2706–11.
Gao L, Zhang XC, Li MM, Yuan JQ, Cui XJ, Shi BX. Psychometric properties of the Chinese version of arthritis self-efficacy Scale-8 (ASES-8) in a rheumatoid arthritis population. Rheumatol Int. 2017;37(5):751–6.
Yang F, Devlin N, Luo N. Cost-utility analysis using EQ-5D-5L data: does how the utilities are derived matter? Value in Health. 2019;22(1):45–9.
Eckhard L, Munir S, Wood D, Talbot S, Brighton R, Walter B, Baré J. The KOOS-12 shortform shows no ceiling effect, good responsiveness and construct validity compared to standard outcome measures after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021;29:608–15.
Hulley SB, Cummings SR, Browner WS, Grady D, Newman TB. Designing Clinical Research: an epidemiologic approach. 4th Edition. Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA, 2013. Appendix 6 C, page 79.
Skou ST, Bricca A, Roos EM. The impact of physical activity level on the short-and long-term pain relief from supervised exercise therapy and education: a study of 12,796 Danish patients with knee osteoarthritis. Osteoarthr Cartil. 2018;26(11):1474–8.
Eckhard L, Munir S, Wood D, Talbot S, Brighton R, Walter WL, Baré J. Minimal important change and minimum clinically important difference values of the KOOS-12 after total knee arthroplasty. Knee. 2021;29:541–6.
Jih J, Mukherjea A, Vittinghoff E, Nguyen TT, Tsoh JY, Fukuoka Y, Bender MS, Tseng W, Kanaya AM. Using appropriate body mass index cut points for overweight and obesity among Asian americans. Prev Med. 2014;65:1–6.
Chen KK, Wee S-L, Pang BWJ, Lau LK, Jabbar KA, Seah WT, Ng TP. Relationship between BMI with percentage body fat and obesity in Singaporean adults–the Yishun Study. BMC Public Health. 2021;21:1–9.
Appropriate body-mass. Index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129(1):125–37.
Shim H-Y, Park M, Kim H-J, Kyung H-S, Shin J-Y. Physical activity status by pain severity in patients with knee osteoarthritis: a nationwide study in Korea. BMC Musculoskelet Disord. 2018;19(1):1–9.
Skou ST, Pedersen BK, Abbott JH, Patterson B, Barton C. Physical activity and Exercise Therapy Benefit more than just symptoms and impairments in people with hip and knee osteoarthritis. J Orthop Sports Phys Ther. 2018;48(6):439–47.
Bennell KL, Bayram C, Harrison C, Brand C, Buchbinder R, Haas R, Hinman RS. Trends in management of hip and knee osteoarthritis in general practice in Australia over an 11-year window: a nationwide cross-sectional survey. Lancet Reg Health-Western Pac. 2021;12:100187.
Baumbach L, Roos EM, Lykkegaard J, Thomsen KS, Kristensen PL, Christensen AI, Thorlund JB. Patients with osteoarthritis are least likely to receive lifestyle advice compared with patients with diabetes and hypertension: a national health survey study from Denmark. Osteoarthr Cartil Open. 2020;2(3):100067.
Ingelsrud LH, Roos EM, Gromov K, Jensen SS, Troelsen A. Patients report inferior quality of care for knee osteoarthritis prior to assessment for knee replacement surgery–a cross-sectional study of 517 patients in Denmark. Acta Orthop. 2020;91(1):82–7.
Barton C, King M, Dascombe B, Taylor N, de Oliveira Silva D, Holden S, Goff A, Takarangi K, Shields N. Many physiotherapists lack preparedness to prescribe physical activity and exercise to people with musculoskeletal pain: a multi-national survey. Phys Ther Sport. 2021;49:98–105.
Lowe A, Littlewood C, McLean S, Kilner K. Physiotherapy and physical activity: a cross-sectional survey exploring physical activity promotion, knowledge of physical activity guidelines and the physical activity habits of UK physiotherapists. BMJ open Sport & Exercise Medicine 2017, 3 (1), e000290.
Egerton T, Nelligan RK, Setchell J, Atkins L, Bennell KL. General practitioners’ views on managing knee osteoarthritis: a thematic analysis of factors influencing clinical practice guideline implementation in primary care. BMC Rheumatol. 2018;2(1):1–11.
Hébert ET, Caughy MO, Shuval K. Primary care providers’ perceptions of physical activity counselling in a clinical setting: a systematic review. Br J Sports Med. 2012;46(9):625–31.
Nissen N, Holm PM, Bricca A, Dideriksen M, Tang LH, Skou ST. Clinicians’ beliefs and attitudes to physical activity and exercise therapy as treatment for knee and/or hip osteoarthritis: a scoping review. Osteoarthritis Cartilage. 2022;30(2):260–9.
Fong JH. Leisure-time physical activity and its correlates in a multi-ethnic sample of adults over age 50 in Singapore. BMC Public Health. 2021;21(1):1–8.
Setchell J, Watson B, Jones L, Gard M, Briffa K. Physiotherapists demonstrate weight stigma: a cross-sectional survey of Australian physiotherapists. J Physiotherapy. 2014;60(3):157–62.
Eswaran A, Meisner BA. Influence of ageism on physical activity prescription for Prediabetes Management. J Aging Phys Act. 2022;1(aop):1–5.
Wallis JA, Ackerman IN, Brusco NK, Kemp JL, Sherwood J, Young K, Jennings S, Trivett A, Barton CJ. Barriers and enablers to uptake of a contemporary guideline-based management program for hip and knee osteoarthritis: a qualitative study. Osteoarthr Cartil Open. 2020;2(4):1–7.
Somers TJ, Keefe FJ, Pells JJ, Dixon KE, Waters SJ, Riordan PA, Blumenthal JA, McKee DC, LaCaille L, Tucker JM. Pain catastrophizing and pain-related fear in osteoarthritis patients: relationships to pain and disability. J Pain Symptom Manag. 2009;37(5):863–72.
Morcos MW, Teeter MG, Somerville LE, Lanting B. Correlation between hip osteoarthritis and the level of physical activity as measured by wearable technology and patient-reported questionnaires. J Orthop. 2020;20:236–9.
Wallis JA, Taylor NF, Bunzli S, Shields N. Experience of living with knee osteoarthritis: a systematic review of qualitative studies. BMJ open 2019, 9 (9), e030060.
Cronström A, Dahlberg LE, Nero H, Hammarlund CS. I was considering surgery because I believed that was how it was treated: a qualitative study on willingness for joint surgery after completion of a digital management program for osteoarthritis. Osteoarthr Cartil. 2019;27(7):1026–32.
Goff AJ, Barton CJ, Merolli M, Quah ASZ, Hoe CKC, De Oliveira Silva D. Comprehensiveness, accuracy, quality, credibility and readability of online information about knee osteoarthritis. Health Inf Manag J. 2023;52(3):185–93.
Bunzli S, O’Brien P, Ayton D, Dowsey M, Gunn J, Choong P, Manski-Nankervis J-A. Misconceptions and the acceptance of evidence-based nonsurgical interventions for knee osteoarthritis. A qualitative study. Clin Orthop Relat Research®. 2019;477(9):1975–83.
Briani RV, Ferreira AS, Pazzinatto MF, Pappas E, Silva DDO, de Azevedo FM. What interventions can improve quality of life or psychosocial factors of individuals with knee osteoarthritis? A systematic review with meta-analysis of primary outcomes from randomised controlled trials. Br J Sports Med. 2018;52(16):1031–8.
Goff AJ, de Oliveira Silva D, Merolli M, Bell EC, Crossley KM, Barton CJ. Patient education improves pain and function in people with knee osteoarthritis with better effects when combined with exercise therapy: a systematic review. J Physiotherapy. 2021;67(3):177–89.
Bell E, Wallis J, Goff A, Crossley K, O’Halloran P, Barton C. Does land-based exercise-therapy improve physical activity in people with knee osteoarthritis? A systematic review with meta-analyses. Osteoarthr Cartil. 2022;30(11):1420–33.
Mørup-Petersen A, Skou ST, Holm CE, Holm PM, Varnum C, Krogsgaard MR, Laursen M, Odgaard A. Measurement properties of UCLA Activity Scale for hip and knee arthroplasty patients and translation and cultural adaptation into Danish. Acta Orthop. 2021;92(6):681–8.
Violant-Holz V, Gallego-Jiménez MG, González-González CS, Muñoz-Violant S, Rodríguez MJ, Sansano-Nadal O, Guerra-Balic M. Psychological health and physical activity levels during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2020;17(24):9419.
White DK, Tudor-Locke C, Felson DT, Gross KD, Niu J, Nevitt M, Lewis CE, Torner J, Neogi T. Do radiographic disease and pain account for why people with or at high risk of knee osteoarthritis do not meet physical activity guidelines? Arthr Rhuem. 2013;65(1):139–47.
Bricca A, Wirth W, Juhl CB, Kemnitz J, Hunter DJ, Kwoh CK, Eckstein F, Culvenor AG. Moderate physical activity and prevention of cartilage loss in people with knee osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res. 2019;71(2):218–26.
Bedson J, Croft PR. The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord. 2008;9(1):1–11.
Özden F, Karaman ÖN, Tuğay N, Kilinç CY, Kilinç RM, Tuğay BU. The relationship of radiographic findings with pain, function, and quality of life in patients with knee osteoarthritis. J Clin Orthop Trauma. 2020;11:512–S517.
Pereira D, Severo M, Santos RA, Barros H, Branco J, Lucas R, Costa L, Ramos E. Knee and hip radiographic osteoarthritis features: differences on pain, function and quality of life. Clin Rheumatol. 2016;35:1555–64.
Bauman AE, Reis RS, Sallis JF, Wells JC, Loos RJ, Martin BW. Correlates of physical activity: why are some people physically active and others not? The Lancet. 2012;380(9838):258–71.
Sawyer A, Ucci M, Jones R, Smith L, Fisher A. Simultaneous evaluation of physical and social environmental correlates of physical activity in adults: a systematic review. SSM-population Health. 2017;3:506–15.
Acknowledgements
Nil.
Funding
This research was funded by National Hospital Group (NHG) Population Health Grant (PHG20/S/T/1/4).
Author information
Authors and Affiliations
Contributions
Conceptualization, A.J.G., L.E.J., T.B.Y. Methodology, A.J.G., L.E.J., L.C.J., T.B.Y.Software, N.A.Validation, N.A.Formal Analysis, A.J.G., L.E.J., L.C.J., T.B.Y.Investigation, A.J.G., L.E.J., L.C.J., T.B.Y.Resources, A.J.G., L.E.J., L.C.J., T.B.Y.Data Curation, T.B.Y.Writing – Original Draft Preparation, Review & Editing, plus Visualization, A.J.G., L.E.J., L.C.J., T.B.Y.Supervision, N.AProject Administration, A.J.G., L.E.J., L.C.J., T.B.Y.Funding Acquisition, B.T.Y.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the National Healthcare Group Domain Specific Review Board (NHG DSRB) Singapore (Reference number: WHC/2020-00076) on 30th April 2021. All participants provided informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Table S1. Summarised participant characteristics and UCLA data for all participants. Table S2. Ordinal UCLA activity score and knee osteoarthritis outcome score (KOOS-12). Table S3. Ordinal UCLA activity score and brief fear of movement (BFOM). Table S4. Ordinal UCLA activity score and EQ-5D-5L. Table S5. Cross tabulation for race and age (Fisher Extract test). Table S6. Cross tabulation for gender and age (Pearson chi-squared test).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Goff, A.J., Jones, L.E., Lim, C.J. et al. A cross sectional study exploring the relationship of self-reported physical activity with function, kinesiophobia, self-efficacy and quality of life in an Asian population seeking care for knee osteoarthritis. BMC Musculoskelet Disord 25, 74 (2024). https://doi.org/10.1186/s12891-024-07181-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-024-07181-y