Abstract
Background
About 15–60% of individuals with ankle sprains may develop functional ankle instability (FAI), which is characterised by ankle pain, decreased muscle strength, limited range of motion, and impaired balance, causing a decline in social activity and quality of life. However, the relationship between those characters is still unclear. This study aimed to investigate whether a relationship existed between ankle pain, active range of motion (AROM), strength and balance and if ankle pain, AROM and strength can predict balance in individuals with FAI.
Methods
Seventy-seven subjects (46 males; 31 females) with unilateral FAI participated in this study. Ankle pain was measured by the visual analogue scale (VAS), ankle AROM was measured using a universal goniometer, ankle strength was measured using a handheld dynamometer, the static balance was measured by the Time in Balance Test (TBT) and the dynamic balance was measured by the modified Star Excursion Balance Test (mSEBT). Pearson product-moment correlations were used to determine the correlations between ankle pain, AROM, strength and balance. Multiple linear regressions were used to investigate if ankle pain, AROM and strength can predict balance in individuals with FAI.
Results
VAS and AROM-plantarflexion predicted 25.6% of the TBT (f2 = 0.344, P < 0.001). AROM-dorsiflexion predicted 24.6% of the mSEBT-anterior reach (f2 = 0.326, P < 0.001). VAS, AROM-plantarflexion and strength-plantarflexion predicted 33.5% of the mSEBT-posteromedial reach (f2 = 0.504, P < 0.001). AROM-plantarflexion and strength-plantarflexion predicted 28.2% of the mSEBT-posterolateral reach (f2 = 0.393, P < 0.001).
Conclusion
This study shows that ankle plantarflexion strength, AROM of dorsiflexion and plantarflexion and pain are predictors of balance in individuals with FAI. These factors could be considered in the rehabilitation of FAI.
Trial registration
Trial registration number: ChiCTR2200063532.
Similar content being viewed by others
Introduction
The ankle joint is one of the most often injured joints in sports [1], accounting for 10–30% of sports injuries [2]. Ankle sprains can result in serious complications, such as a chronic feeling of ankle instability and recurrent sprains if they are not promptly and appropriately treated [3]. About 15–60% of individuals with ankle sprains may develop functional ankle instability (FAI) [4], which is characterised by recurrent episodes of “giving-way,“ pain, self-reported disability, and/or ankle sprains in daily life without anatomic abnormalities in the ankle joint [5]. FAI causes a decline in social activity and quality of life [6].
Individuals with FAI frequently experience chronic ankle pain, decreased periarticular muscle strength, and restricted range of motion [7]. Additionally, studies have revealed that FAI individuals have impaired proprioceptive, static, and dynamic balance as well as increased postural sway [8, 9]. Clinical tests for static and dynamic balance, referred to as the Time in Balance Test (TBT) [10] and the modified Star Excursion Balance Test (mSEBT) [11] respectively, have been developed. Either mechanical instability, functional instability, or a combination of the two can be the cause of chronic ankle instability (CAI) [8]. It has been shown that weight-bearing dorsiflexion [12,13,14,15], open-chain dorsiflexion [14] and SEBT-anterior reach are correlated in individuals with CAI. Eversion strength [15] was discovered to be related to the SEBT-posteromedial and posterolateral reaches in CAI.
However, there are no studies that explain whether ankle strength, range of motion, or pain related to static or dynamic balance in FAI. Understanding the relationships between ankle pain, range of motion, strength, and balance may help to develop evidence-based and accurate rehabilitation strategies to treat balance deficits in individuals with FAI. Consequently, this study aimed to investigate the relationship between pain, range of motion, muscle strength and balance in individuals with FAI. We hypothesized that both static and dynamic balance should have a distinct set of predictors.
Methods
Seventy-seven subjects (46 males; 31 females) with unilateral FAI were recruited from September 2022 to December 2022 at the Department of Rehabilitation Medicine of a local hospital. All tests and measurements were performed by the same professional, experienced physiotherapist. The criteria for inclusion were (1)18–65 years old; (2) at least 1-time history of ankle sprains, initial strain occurred before the research more than 1 year; (3) at least 2 times of ipsilateral ankle giving way or instability in the past 6 months; (4) the Cumberland Ankle Instability Tool score ≤ 24 points. The exclusion criteria were (1) the anterior drawer’s test and talar tilts test were positive; (2) the history of bilateral ankle sprains or bilateral ankle giving way; (3) the history of fracture or musculoskeletal surgery in either lower extremity, visual impairment, vestibular or balance disorder; (4) any history of lower extremity acute musculoskeletal injury within 3 months. The study followed the guidelines laid out in the Declaration of Helsinki, received approval from the hospital’s ethics board, and was registered with ChiCTR.org.cn (www.chictr.org.cn, 10/09/2022, ChiCTR2200063532). Each participant signed an informed consent form before initiation of the study.
G * Power3.1.9.2 statistical software (NeuIsenburg, Aichach, Germany) calculated the sample as 77, based on the multiple linear regression model with medium effect sizes(f2) of 0.15, β of 0.2 and α of 0.05.
Basic demographic characteristics information of age, gender, affected side, weight, height and clinical outcomes of ankle pain, active range of motion (AROM), strength and balance (static and dynamic) were measured by the same qualified and experienced therapist. The Visual Analog Scale (VAS) was used to rate pain on a scale of 0 to 10 with an intraclass correlation value (ICC) of 0.71–0.99 [16]. The greater the score, the more severe the pain. A universal goniometer was used to assess active dorsiflexion, plantarflexion, inversion, and eversion ranges of motion. The subject was instructed to maximally and actively move the ankle in these four directions. Each direction was measured 3 times and an average degree was calculated. The tibia and fibula were stabilised by the same assistant to prevent knee motion and hip rotation [17]. For the dorsiflexion and plantarflexion, place the subject supine with the knee straight and the foot over the edge of the supporting surface. Place the goniometer with (1) the axis of rotation at the lateral malleolus, (2) the proximal arm parallel to the lateral midline of the fibula, using the head of the fibula for reference, and (3) the distal arm parallel to the lateral aspect of the fifth metatarsal. For the inversion and eversion, place the subject prone with the knee straight and the foot over the edge of the supporting surface. Place the goniometer with (1) the axis of rotation at the posterior aspect of the ankle midway between the lateral and medial malleolus, (2) the proximal arm parallel to the posterior midline of the lower leg, and (3) the distal arm parallel to the posterior midline of the calcaneus [18]. ICC values for the goniometer were 0.81–0.94 [19]. Using a handheld dynamometer (MicroFET2TM), the ankle’s dorsiflexion, plantarflexion, inversion and eversion strength were measured. Participants were required subjects to ramp up to a 5-second maximal effort contraction while being subjected to the examiner’s intense resistance. ICC values for handheld dynamometry were 0.77–0.97 [20]. Static balance was assessed using the Time in Balance Test (TBT). The maximum time (seconds) that the individual could maintain balance while standing on the single affected leg with the eyes closed was measured. ICC values for TBT were 0.98–0.99 [21]. Modified Star Excursion Balance Test (mSEBT) was used to measure the maximum distance the individual could reach in the anterior, posteromedial, and posterolateral directions of the contralateral leg while standing on the affected side and being able to maintain balance and return to the starting position. Reach distance = maximum distance/leg length X 100 [11]. ICC values for mSEBT were 0.88–0.96 [22]. All of the ICC results come from the study we are referring to and are not our results.
SPSS24.0(IBM Corporation, Armonk, NY, USA) was used to process data and the demographic characteristics of the study population were described using descriptive statistical methods. The Shapiro-Wilk test was used for testing normal distribution. To investigate the relationship between the explanatory and criteria variables, Pearson product-moment correlations were used. Explanatory variables included VAS of pain, dorsiflexion, plantarflexion, eversion and inversion of ankle strength and AROM. Criterion variables included TBT and three reach directions of mSEBT. The variables that showed a fair correlation (r ≥ 0.25) with each criterion variable were chosen as predictor variables in the respective regression model. For TBT and each mSEBT reach direction, four unique backward multiple linear regression models were developed. To account for multicollinearity, variance inflation factors with values greater than 10 were checked. Statistical significance was set at 0.05. Effect sizes(f2) were utilized to measure the efficacy of the models and were interpreted as large (≥ 0.35), medium (0.15–0.34), and small (0.02–0.14) to determine the clinical significance of the final regression models. f2 ≥ 0.15 were considered clinically relevant [23].
Results
This study included 77 participants (46 males and 31 females) with an average age of 32.13 ± 8.79 years. The individual demographic characteristics are stated in Table 1. The means and standard deviation for variables can be found in Table 2. Results of Pearson product-moment correlations between VAS, strength, AROM and TBT, mSEBT are shown in Table 3.
Multiple linear regression analysis showed that ankle VAS (B=-2.145, P = 0.001) significantly negatively predicted TBT, and AROM-plantarflexion (B = 0.763, P = 0.005) significantly positively predicted TBT in individuals with FAI (Table 4). VAS and AROM-plantarflexion predicted 25.6% of the TBT (f2 = 0.344, P < 0.001).
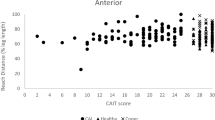
Multiple linear regression analysis showed that AROM-dorsiflexion (B = 0.558, P < 0.001) significantly positively predicted mSEBT-anterior reach (Table 4). AROM-dorsiflexion predicted 24.6% of the mSEBT-anterior reach (f2 = 0.326, P < 0.001) in individuals with FAI.
Multiple linear regression analysis showed that VAS (B=-1.193, P = 0.014) significantly negatively predicted mSEBT-posteromedial reach; AROM-plantarflexion (B = 0.581, P = 0.005) and strength-plantarflexion (B = 0.185, P = 0.025) significantly positively predicted mSEBT-posteromedial reach (Table 4). VAS, AROM-plantarflexion and strength-plantarflexion predicted 33.5% of the mSEBT-posteromedial reach (f2 = 0.504, P < 0.001) in individuals with FAI.
Multiple linear regression analysis showed that AROM-plantarflexion (B = 0.510, P = 0.019) and strength-plantarflexion (B = 0.189, P = 0.034) significantly positively predicted mSEBT-posterolateral reach (Table 4). AROM-plantarflexion and strength-plantarflexion predicted 28.2% of the mSEBT-posterolateral reach (f2 = 0.393, P < 0.001) in individuals with FAI.
Discussion
This study aimed to examine whether a relationship existed between ankle pain, AROM, strength and balance and if ankle pain, AROM and strength can predict balance in individuals with FAI. Our study showed that VAS and AROM-plantarflexion predicted 25.6% of TBT. AROM-dorsiflexion predicted 24.6% of the mSEBT-anterior reach. For mSEBT-posteromedial reach, VAS, AROM-plantarflexion and strength-plantarflexion predicted 33.5%. AROM-plantarflexion and strength-plantarflexion predicted 28.2% of the mSEBT-posterolateral reach.
Our findings indicate that VAS of pain significantly negatively predicted TBT and mSEBT-posteromedial reaches in individuals with FAI. These results are consistent with several previous studies. Local pain was observed by Chen et al. [24] to have a substantial impact on balance control in CAI patients and to be connected to defects in both static balance of single-leg stance and dynamic balance of SEBT-anterior reach. According to research by Thompson et al. [25], the pain was found correlated with the inability to suppress soleus spinal reflexes during static single-leg stance balance tests in CAI individuals, which raised perceived instability and the risk of recurring sprains. The strong association between ankle pain and instability was identified in the study by Al Adal et al. [26], which showed that individuals with more severe perceived ankle instability, as determined by the Cumberland Ankle Instability Tool, were more likely to report ankle pain. In a study by Suttmiller et al. [27], the outcomes of questionnaires on pain and ankle function in individuals with CAI were analyzed. Ankle function was found to be negatively correlated with pain. Simsek et al.’s study [28] found a statistically significant negative correlation between pain severity and the SEBT-anterior reach distance, proving that methods to reduce pain intensity can also increase SEBT reach distances. The unbalanced loading due to biomechanical changes between the talus and mortis after ankle sprains resulting in articular cartilage deterioration with ankle pain may explain the negative association between balance and pain in individuals with CAI [29]. A similar correlation between pain and joint instability has been found in other body joints like the patellofemoral joint [30] and shoulder [31, 32]. The central sensitization, which occurs when people experience pain without any nociceptive inputs, was used to explain this [32]. However, according to one study [14], there was no connection between pain and SEBT reach distances in CAI. It should be emphasized that the study’s average VAS-pain score was low, therefore drawing firm conclusions may not be possible given the floor effect.
Our findings indicate that AROM-plantarflexion significantly positively predicted TBT, mSEBT-posteromedial and posterolateral reaches. AROM-dorsiflexion significantly positively predicted mSEBT-anterior reach in individuals with FAI. The literature on relationships between ankle range of motion and static balance is limited in FAI. Similar results were found in studies conducted on athletes [33] and young adults [34]. Trajković et al. [33] demonstrated that plantarflexion of ankle passive range of motion (PROM) is correlated with centre of pressure (COP) amplitude in medial-lateral reach during single-leg quiet stance in young trained athletes. This was confirmed by Kim et al. [34], which showed that ankle plantarflexion of AROM and PROM were significantly correlated with static postural sway in young adults, and it is mainly affected by PROM-plantarflexion particularly. However, no relationship was found between ankle PROM and static postural balance in younger adults in another study [35]. It should be noted that if the PROM of the ankle is larger than normal, it suggests that the ankle structures are loose, indicating that the relationship between range of motion and balance is negative [34]. As for the dynamic balance, there is considerable evidence linking ankle dorsiflexion to the SEBT-anterior reach performance. Consistent with the present study, Terada et al. [14] showed that AROM-dorsiflexion was significantly correlated with SEBT-anterior performance in CAI. What’s more, Terada et al.’s study [14] and other studies [12, 13, 15] also indicated that weight-bearing dorsiflexion contributed to the SEBT-anterior reach in CAI. Except for CAI, AROM-dorsiflexion [36] and weight-bearing dorsiflexion [37] were also identified as significant predictors of dynamic balance in the Dynamic Postural Stability Index and SEBT-anterior reach [37] in males. Reduced AROM-dorsiflexion was found in FAI but not in copers, which may be a risk factor for ankle instability [38]. What’s more, our study indicates that the AROM-plantarflexion can positively predict mSEBT-posteromedial and posterolateral reaches. However, it was the weight-bearing dorsiflexion that had a positive correlation with the SEBT-posterolateral reach in the study by Basnett et al. [13] in CAI. According to one study [15], ankle mechanical constraints and sensory deficiencies may have a greater impact on SEBT-anterior reach than its posteromedial and posterolateral reaches, which are more dependent on strength and postural control. To determine the connection between ankle range of motion restriction and dynamic balance in FAI, further investigation is necessary.
Our findings indicate that ankle strength-plantarflexion significantly positively predicted mSEBT-posteromedial and posterolateral reaches. For static postural control, ankle joints are chosen above other muscles. Due to the frequent activation of ankle dorsiflexor eccentric control during postural control in the standing posture, dorsiflexion strength in particular has a stronger relationship with postural sway than other muscles [39]. However, no relationship is found between ankle strength and static balance in FAI in the present study. To our knowledge, no similar study was conducted on FAI or CAI before, but on older adults and athletes. According to Bok et al. [35] and Melzer et al. [40], ankle strength-plantarflexion was significantly correlated with COP-sway in the elderly. Kouzaki et al. [41] confirmed that muscle volume decreases are associated with age-related increases in postural sway. And strength-plantarflexion as a significant predictor for COP-sway was also found in trained athletes [33]. This may be because the reduction in FAI muscle strength is less than the reduction in the elderly and is not sufficient to cause a change in static balance. It may also be that static balance is more easily compensated by other joint muscles in the lower extremity, and the demand on the ankle muscles is relatively small and insufficient to cause changes. Our findings show that ankle strength-plantarflexion is significantly associated with mSEBT-posteromedial and posterolateral reaches, and no relationship is found between ankle strength and mSEBT-anterior reach in FAI. However, it was discovered in a prior study [15] that the ankle strength-eversion affected the SEBT-posteromedial and posteromedial reaches in CAI. Similar results were found in the study by Williams et al. [36], which indicated that ankle inversion and eversion strength were significant predictors of the Dynamic Postural Stability Index. The peroneal and triceps calf muscles may be required to stabilize the postural control perturbations caused by the medial and lateral reach directions. On the contrary, another study [42] showed that ankle inversion and eversion strength were not strongly associated with dynamic postural stability in individuals with chronic lateral ankle instability that waiting for surgery. For those waiting for surgery, mechanical deficits may have a greater effect on dynamic stability than ankle strength.
This study shows that ankle plantarflexion strength, AROM of dorsiflexion and plantarflexion and pain are predictors of balance in individuals with FAI. The findings of this study are clinically relevant for individuals with FAI undertaking rehabilitation. These factors could be considered in the rehabilitation of FAI.
Limitations
In this study, we measured ankle open-chain AROM. However, both static and dynamic balance were measured in a one-leg standing posture. Future research should include ankle weight-bearing range of motion. In this investigation, ankle strength and AROM were assessed with handheld instruments. If available, more accurate measuring instrument with higher reliability should be used in future studies. Proprioception, range of motion strength at other joints in the lower extremities, trunk stability, and endurance are all potential contributors to balance. More investigation should be done to find out which potential factors may contribute to static and dynamic balance in FAI. With the cross-sectional study design used in this study, we could only conclude at a specific time point and a causal relationship between the explanatory and criterion variables could not be established. The determinants of postural control in individuals with FAI may be studied prospectively in future studies.
Conclusion
According to our findings, ankle pain, plantarflexion strength, AROM of dorsiflexion and plantarflexion are predictors of balance in individuals with FAI. VAS and AROM-plantarflexion significantly predicted TBT. AROM-dorsiflexion significantly predicted mSEBT-anterior reach. VAS, AROM-plantarflexion and strength-plantarflexion significantly predicted mSEBT-posteromedial reach. AROM-plantarflexion and strength-plantarflexion significantly predicted mSEBT-posterolateral reach in FAI. These factors could be considered in the rehabilitation for FAI.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- FAI:
-
Functional Ankle Instability
- VAS:
-
Visual Analog Scale
- AROM:
-
Active Range of Motion
- TBT:
-
Time in Balance Test
- mSEBT:
-
Modified Star Excursion Balance Test
- CAI:
-
Chronic Ankle Instability
- ICC:
-
Intraclass Correlation Value
- COP:
-
Center of Pressure
- PROM:
-
Passive Range of Motion
References
Jungmann PM, Lange T, Wenning M, et al. Ankle sprains in athletes: current epidemiological, clinical and imaging trends. Open Access J Sports Med. 2023;14:29–46.
Kosik KB, McCann RS, Terada M, et al. Therapeutic interventions for improving self-reported function in patients with chronic ankle instability: a systematic review. Br J Sports Med. 2017;51:105–12.
Sarcon AK, Heyrani N, Giza E, et al. Lateral ankle sprain and chronic ankle instability. Foot Ankle Orthopedics. 2019;4(2):2473011419846938.
Doherty C, Bleakley C, Hertel J, et al. Recovery from a first-time lateral ankle sprain and the predictors of chronic ankle instability: a prospective cohort analysis. Am J Sports Med. 2016;44:995–1003.
Freeman M, Dean M, Hanham I. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Br. 1965;47:678–85.
Arnold BL, Wright CJ, Ross SE. Functional ankle instability and health-related quality of life. J Athl Train. 2011;46:634–41.
Roos KG, Kerr ZY, Mauntel TC, et al. The epidemiology of lateral ligament complex ankle sprains in national collegiate athletic association sports. Am J Sports Med. 2017;45:201–9.
Hertel J, Corbett RO. An updated model of chronic ankle instability. J Athl Train. 2019;54:572–88.
Arnold BL, De La Motte S, Linens S, et al. Ankle instability is associated with balance impairments: a meta-analysis. Med Sci Sports Exerc. 2009;41:1048–62.
Ross SE, Guskiewicz KM. Examination of static and dynamic postural stability in individuals with functionally stable and unstable ankles. Clin J Sport Med. 2004;14:332–8.
Ko J, Wikstrom E, Li Y, et al. Performance differences between the modified Star Excursion Balance Test and the Y-Balance test in individuals with chronic ankle instability. J Sport Rehabil. 2020;29(6):748–53.
Hoch MC, Staton GS, Medina McKeon JM, et al. Dorsiflexion and dynamic postural control deficits are present in those with chronic ankle instability. J Sci Med Sport. 2012;15:574–9.
Basnett CR, Hanish MJ, Wheeler TJ, et al. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int J Sports Phys Ther. 2013;8:121–8.
Terada M, Harkey MS, Wells AM, et al. The influence of ankle dorsiflexion and self-reported patient outcomes on dynamic postural control in participants with chronic ankle instability. Gait Posture. 2014;40:193–7.
Gabriner ML, Houston MN, Kirby JL, et al. Contributing factors to Star Excursion Balance Test performance in individuals with chronic ankle instability. Gait Posture. 2015;41:912–6.
Alghadir AH, Anwer S, Iqbal A et al. Test–retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res. 2018: 851–6.
Cox RW, Martinez RE, Baker RT et al. Validity of a smartphone application for measuring ankle plantar flexion. J Sport Rehabil. 2018. 27(3).
Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry. 5th ed. Philadelphia, PA: F. A. Davis Company; 2016.
Pandya S, Florence JM, King WM, et al. Reliability of goniometric measurements in patients with Duchenne muscular dystrophy. Phys Ther. 1985;65:1339–42.
Kelln BM, McKeon PO, Gontkof LM, et al. Hand-held dynamometry: reliability of lower extremity muscle testing in healthy, physically active, young adults. J Sport Rehabil. 2008;17:160–70.
Oza K, Shah P, Patel Y, et al. Inter-rater reliability of time-in-balance test among young individuals with ankle instability. Multimed Syst. 2019;6:1443.
Hyong IH, Kim JH. Test of intrarater and interrater reliability for the star excursion balance test. J Phys Ther Sci. 2014;26:1139–41.
Cohen J. A power primer. Psychol Bull. 1992;112:155–9.
Chen Y, Cao S, Qian L, et al. The influence of local pain on balance control in patients with chronic ankle instability. BMC Musculoskelet Disord. 2022;23:699.
Thompson CS, Hiller CE, Schabrun SM. Altered spinal-level sensorimotor control related to pain and perceived instability in people with chronic ankle instability. J Sci Med Sport. 2019;22:425–9.
Al Adal S, Mackey M, Pourkazemi F, et al. The relationship between pain and associated characteristics of chronic ankle instability: a retrospective study. J Sport Health Sci. 2020;9:96–101.
Suttmiller AMB, Cavallario JM, Baez SE, et al. Perceived instability, pain, and psychological factors for prediction of function and disability in individuals with chronic ankle instability. J Athl Train. 2022;57:1048–54.
Simsek S, Yagci N. Acute effects of distal fibular taping technique on pain, balance and forward lunge activities in chronic ankle instability. J Back Musculoskelet Rehabil. 2019;32:15–20.
Valderrabano V, Horisberger M, Russell I, et al. Etiology of ankle osteoarthritis. Clin Orthop Relat Res. 2009;467:1800–6.
Sanchis-Alfonso V. Anterior knee pain and patellar instability. Springer Sci Bus Media; 2011.
Boileau P, Zumstein M, Balg F, et al. The unstable painful shoulder (UPS) as a cause of pain from unrecognized anteroinferior instability in the young athlete. J Shoulder Elbow Surg. 2011;20:98–106.
Gasson A, Jaggi A, Alexander S, et al. Differences in reported severity of pain and the location of pain in patients with recurrent structural and non-structural shoulder instability. Man Ther. 2016;25:e103.
Trajković N, Kozinc Ž, Smajla D, et al. Relationship between ankle strength and range of motion and postural stability during single-leg quiet stance in trained athletes. Sci Rep. 2021;11:1–8.
Kim SG, Kim WS. Effect of ankle range of motion (rom) and lower-extremity muscle strength on static balance control ability in young adults: a regression analysis. Med Sci Monit. 2018;24:3168–75.
Bok SK, Lee TH, Lee SS. The effects of changes of ankle strength and range of motion according to aging on balance. Ann Rehabil Med. 2013;37:10–6.
Williams VJ, Nagai T, Sell TC, et al. Prediction of dynamic postural stability during single-leg jump landings by ankle and knee flexibility and strength. J Sport Rehabil. 2016;25:266–72.
Nakagawa TH, Petersen RS. Relationship of hip and ankle range of motion, trunk muscle endurance with knee valgus and dynamic balance in males. Phys Ther Sport. 2018;34:174–9.
Wright CJ, Arnold BL, Ross SE, et al. Clinical examination results in individuals with functional ankle instability and ankle-sprain copers. J Athl Train. 2013;48:581–9.
Lord SR, Clark RD, Webster IW. Postural stability and associated physiological factors in a population of aged persons. J Gerontol. 1991;46:M69–76.
Melzer I, Benjuya N, Kaplanski J, et al. Association between ankle muscle strength and limit of stability in older adults. Age Ageing. 2009;38:119–23.
Kouzaki M, Masani K. Postural sway during quiet standing is related to physiological tremor and muscle volume in young and elderly adults. Gait Posture. 2012;35:11–7.
Ko KR, Lee H, Lee W-Y, et al. Ankle strength is not strongly associated with postural stability in patients awaiting Surgery for chronic lateral ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28:326–33.
Acknowledgements
Not applicable.
Funding
The study did not receive any specific funding from funding agencies in the public, commercial or non-profit sectors.
Author information
Authors and Affiliations
Contributions
L.W. participated in the data collection/analysis and writing of the manuscript. G.Y. and X.Z. participated in the data collection and analysis. Y.W. participated in the data analysis. Y.C. provided experimental guidance during the study and revised the paper critically. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in accordance with the Declaration of Helsinki. All participants were informed about the study and signed an informed consent before the study. This study was approved by the ethics committee of Beijing Tongren Hospital Capital Medical University and registered with ChiCTR.org.cn (ChiCTR2200063532).
Consent for publication
The evaluation data involved in the paper were published with the informed consent of the patients.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, L., Yu, G., Zhang, X. et al. Relationship between ankle pain, range of motion, strength and balance in individuals with functional ankle instability: a cross-sectional study. BMC Musculoskelet Disord 24, 955 (2023). https://doi.org/10.1186/s12891-023-07079-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-07079-1