Abstract
Background
Autologous bone grafts are the gold standard for spinal fusion; however, harvesting autologous bone can result in donor site infection, hematomas, increased operative time, and prolonged pain. Cellular bone allografts (CBAs) are a viable alternative that avoids the need for bone harvesting and may increase fusion success alone or when used as an adjunct material. The present study examined the efficacy and safety of CBA when used as an adjunct graft material to lumbar arthrodesis.
Methods
A prospective, single-arm, multicenter clinical trial (NCT 02969616) was conducted in adult subjects (> 18 years of age) undergoing lumbar spinal fusion with CBA graft (CBA used as primary (≥ 50% by volume), with augmentation up to 50%). Radiographic fusion status was assessed by an independent review of dynamic radiographs and CT scans. Clinical outcomes were assessed with the Oswestry Disability Index (ODI), and Visual Analog Scales (VAS) score for back and leg pain. Adverse events were assessed through the 24-month follow-up period. The presented data represents an analysis of available subjects (n = 86) who completed 24 months of postoperative follow-up at the time the data was locked for analysis.
Results
Postoperative 24-month fusion success was achieved in 95.3% of subjects (n = 82/86) undergoing lumbar spinal surgery. Clinical outcomes showed statistically significant improvements in ODI (46.3% improvement), VAS-Back pain (75.5% improvement), and VAS-Leg pain (85.5% improvement) (p < 0.01) scores at Month 24. No subject characteristics or surgical factors were associated with pseudoarthrosis. A favorable safety profile with a limited number of adverse events was observed.
Conclusions
The use of CBA as an adjunct graft material showed high rates of successful lumbar arthrodesis and significant improvements in pain and disability scores. CBA provides an alternative to autograft with comparable fusion success rates and clinical benefits.
Trial registration
NCT 02969616.
Similar content being viewed by others
Background
Lumbar fusion is frequently used for a variety of degenerative, traumatic, and oncologic conditions of the lumbar spine. Advancements in surgical techniques, including spinal instrumentation and combined anterior and posterior procedures have led to increased rates of fusion. Autologous iliac crest bone graft (ICBG) is the gold standard bone graft and offers osteoconductive, osteoinductive and osteogenic properties that aid in achieving successful fusion. However, harvesting ICBG may result in donor site infection, hematomas, increased operative time, prolonged pain, altered cosmesis, and in rare instances arterial and nerve injury [1,2,3]. Alternatives to autograft include bone marrow aspirate, bone graft allografts, synthetic bone void fillers, and bone morphogenetic protein [4, 5]. Although these alternative bone graft options provide one or two healing properties, they lack the complete trio of osteoconductive, osteoinductive and osteogenic properties found in autograft bone.
Cellular bone allografts (CBAs) provide an innovative addition to allograft technologies and are an alternative to other bone grafting options. From a structural standpoint, allograft may serve in the absence of revascularization and creeping substitution processes. Cellular bone allografts provide the same three osteometric properties promoted with ICBG without the complications of donor site morbidity associated with bone graft harvesting, which has been reported to be as high as 38% [6,7,8,9,10,11]. Although CBAs have been utilized in lumbar and cervical spinal fusion surgery, there is limited clinical literature detailing fusion rates and the impact of selected patient demographics and associated outcomes on clinical measures [12,13,14,15,16].
A prospective, post marketing, multicenter, open label, non-randomized clinical study was conducted to assess the efficacy and safety of CBA (Trinity Elite®) in lumbar fusion surgery. The current report presents an interim analysis of the clinical and radiographic outcomes at 24-months of postoperative follow-up.
Methods
As previously published and described in the 12-month interim analysis by Wind et al. [17], this prospective, single-arm, open label study enrolled subjects prospectively at nine clinical sites and screened for enrollment via preset inclusion/exclusion criteria. All participating sites received IRB approval prior to initiation of the study. Sites used a central IRB (Western IRB or WCG IRB) or local IRB (University of Virginia and the Oregon Health & Science University). Subjects older than 18 years of age, that had failed at least six months of conservative care, who planned to undergo posterolateral fusion (1–4 levels) or interbody fusion (1–2 levels), and met the predefined inclusion/exclusion criteria were enrolled. Subjects who underwent a prior lumbar spinal fusion surgery at a level currently scheduled for surgery, were undergoing treatment for malignancy, or had undergone treatment for malignancy within the last five years (benign skin cancer permitted), presented with an active local or systemic infection, or were undergoing adjunctive treatment for local or systemic infections were excluded. The surgical approach, technique, and placement/location of the bone graft was determined at the discretion of the treating surgeon. Subjects received CBA (Trinity Elite®, MTF Biologics, Edison NJ) as the primary bone graft substance (≥ 50% by volume), with augmentation of up to 50% of locally harvested autograft and/or cancellous allograft chips. No additional bone graft substitutes were allowed. No tissue was harvested from the iliac crest. Subject demographics and baseline characteristics including risk factors for pseudoarthrosis were recorded.
Dynamic x-rays (flexion/extension) were obtained at 3 months, 6 months, 12 months, and 24 months postoperatively, while computerized tomography (CT) scans were obtained at 12 and 24 months. Radiographic fusion at 24 months was assessed by an independent reviewer (TELOS Partners, Warsaw, IN, and MMI, Houston TX), with successful fusion being defined as: (1) lack of angular and translational motion (< 3° and < 3 mm, respectively) on Quantitative Motion Analysis (QMA) and (2) the presence of bridging bone across the adjacent endplates, or transverse processes on thin-cut CT scans. Both fusion criteria had to be met for the subject to be considered a fusion success. In multi-level procedures, all treated levels had to be fused to be considered a fusion success. Clinical outcomes included the Oswestry Disability Index (ODI), and Visual Analog Scales (VAS) for back and leg pain. Clinical outcomes were obtained preoperatively and 6 weeks, 3 months, 6 months, 12 months, and 24 months postoperatively. Adverse events were recorded from surgery through 24 months for each subject, including the event’s relatedness, severity, and outcome.
Subject data was analyzed with SAS Version 9.4 (SAS Institute, Cary, NC). Counts and percentages were reported for categorical baseline variables; the mean standard deviation (SD) and range were reported for continuous variables. Preoperative and postoperative subject reported outcomes were compared with a Wilcoxon signed rank test. Correlation of outcomes to risk factors were calculated by chi-square test. Alpha was set at 0.05 and a p-value of ≤ 0.05 was considered significant.
Results
Subject demographics and surgical procedure
At the time of this interim analysis, 86 subjects had completed 24-months postoperative radiographic and clinical evaluations. The mean age was 59.2 ± 11.9 years (range 28–82) and the subject population included a higher number of females (n = 57, 66.3%) to males (n = 29, 33.7%) with a mean body mass index (BMI) of 30.1 ± 6.3 kg/m2 (range 18.9–44.6). Twelve subjects were current smokers (14.0%), 17 were diabetic (19.8%) and 8 presented with osteoporosis (9.3%). Twenty-two subjects (25.6%) underwent multi-level lumbar arthrodesis. Subject demographics are presented in Table 1.
Radiographic fusion outcomes
Fusion success was confirmed in 95.3% of subjects (n = 82/86). There were 4 subjects (4.7%) with evidence of pseudoarthrosis, with ≥ 3° of angular motion on QMA, although bridging bone was present. No revisions were reported for these 4 subjects at the time of this report (Fig. 1). A representative image depicting successful fusion at 24-months is presented (Fig. 2).
Fusion success by levels treated
There were 60 subjects (69.8%) that underwent a 1-level procedure, 21 subjects (24.4%) underwent a 2-level procedure, and 1 subject (1.2%) underwent a 4-level procedure. Fusion rates for single and multi-level disease were 93.7% and 100.0%, respectively (Table 2).
Fusion success by surgical approach
Nineteen subjects (22.1%) underwent anterior lumbar interbody fusion (ALIF), 21 subjects (24.4%) underwent lateral or oblique lateral lumbar interbody fusion (LLIF, DLIF, XLIF or OLIF), 35 subjects (40.7%) underwent a posterior interbody fusion (PLIF, MIDLIF or TLIF), and 11 subjects (12.8%) underwent posterolateral lumbar fusion (PLF). The rate of fusion success was high regardless of the surgical approach (Table 2).
Clinical outcomes
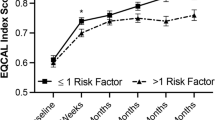
The percentage of disability as assessed by the ODI decreased from 44.7% ± 18.4 preoperatively, to 24.0% ± 21.2 (p < 0.001) at 24 months post-op (Fig. 3A). In subjects that did not have successful fusion (n = 4), the preoperative mean disability was 37.0% ± 7.4 and improved to 6.5% ± 11.7 (p = 0.13). An overall improvement of 75.5% was observed in VAS-Back scores at 24 months post-op. The preoperative mean VAS-Back pain score was 53.9 ± 28.6 and improved to 13.2 ± 23.3 (p < 0.0001) at 24 months post-op. In subjects that did not have successful fusion (n = 4), the preoperative mean VAS-Back pain score was 55.3 ± 29.8 and improved to 8.0 ± 14.1 (p = 0.03). An overall improvement of 85.5% was observed in VAS-Leg pain scores at 24 months post-op. The preoperative mean VAS-Leg pain score was 34.5 ± 25.9 and improved to 6.9 ± 15.6 (p < 0.0001) at 24 months post-op(Fig. 3B). In subjects that did not have successful fusion (n = 4), the preoperative mean VAS-Leg pain score was 26.4 ± 13.3 and improved to 1.1 ± 1.3 (p < 0.001).
Subjects were further evaluated for fusion success by risk factor. No risk factors significantly impacted fusion success (Table 3).
Adverse events
Adverse events (AEs) were reported and characterized by relatedness and severity. Three AEs were considered related to the graft/surgical procedure. A single serious AE (postoperative radiculopathy) was reported as definitely related to the bone graft. Surgical exploration revealed extrusion of the graft material from the interbody. This subject demonstrated successful fusion at 12 months. Two additional AEs reported as probably related to the surgical procedure included hyposthesia and increased lower back pain. Hypoesthesia, which resulted in numbness/loss of sensation in the left lower extremity, was categorized as non-serious and treated with unspecified medication. Increased lower-back pain resulted in the subject undergoing a two-level laminectomy and fusion. Demographics, baseline characteristics, and risk factors for these three subjects are presented in Table 4.
Discussion
Despite the dramatically higher number of lumbar spinal fusion procedures over the past decade, the potential for pseudoarthrosis persists [18, 19]. Surgical treatment using autologous ICBG is considered the gold standard for spinal fusion [20,21,22,23]. However, ICBG is associated with complications, such as donor site pain, infection, and prolonged recovery. While local bone at the surgical site may be available, the supply is limited; thus, the need for alternative bone grafting that can be used as a stand-alone graft or as an adjunct is of high interest [1, 2]. The current clinical trial evaluated CBA as an adjunct bone graft to autograft and demonstrated a high rate of fusion with improved clinical outcomes and a favorable safety profile.
Cellular bone allografts are an alternative to autograft given they have all three principal components of a bone graft, namely osteoconductivity, osteoinductivity, and osteogenicity. Several studies provide support for high fusion rates using CBA in keeping with the current report. Musante et al. report 90.0% fusion success in procedures using viable osteogenic cells, with no differences in reported fusion rates in patients with and without risk factors [24]. Other CBAs, including Vivigen (DepuySynthes, Raynham MA), have shown spinal fusion rates at 90.0% [25]. In a study of multi-level fusion in a posterolateral construct with CBA, a fusion rate of 98.7% was observed [15]. Elgafy et al., report a fusion rate of 91.7% with CBA in 96 patients and 222 treated levels [13]. Furthermore, Ammerman et al. report 91.3% successful fusion in minimally invasive TLIF cases using CBA in 23 patients totaling 26 levels [15]. In extreme lateral interbody (XLIF) procedures, Tohmeh et al. report a fusion rate of 90.2% in 40 patients with a total of 61 levels [16]. In comparison, fusion success rates with the gold standard autograft have been reported in a range from 65.0 to 93.0% [13, 20,21,22,23]. Altogether, the current report further supports data showing high fusion rates using CBA, comparable and even superior to those obtained using autograft.
Significant improvements in clinical outcomes evaluating patient-reported levels of disability and pain were observed. All clinical outcome measures met statistical and clinical significance criterion, further demonstrating the positive impact and meaningful improvement from lumbar spinal fusion in this population. These findings are consistent with other reports showing significant improvements in ODI and VAS disability and pain scores following surgical procedures with CBA. Tohmeh et al. report a 41.0%, 55.0% and 43.0% improvement in ODI, VAS-Back and VAS-leg pain scores postoperatively at 12 months, respectively [16] [13]. Our findings show greater improvements in these outcomes positing a benefit to the specific bone graft used (Trinity allograft) and the adjunctive use with autograft. Further investigation is necessary to determine optimized procedures that provide maximal impact on these patient-reported outcomes.
Of note, the small number of subjects that did not have successful fusion also showed improved clinical outcomes. If a solid fusion is not obtained, but stability to the spine is supported through the instrumentation, the patient may still achieve clinical improvements. Lack of angular and translational motion in addition to bridging bone was the per-protocol definition of fusion. For the majority of subjects with a failed fusion, bridging bone was present which likely contributed to the stability of the spine even though they failed the QMA assessment.
Fusion success and clinical outcomes may be affected by patient risk factors for pseudoarthrosis, including older age, osteoporosis, alcoholism, malnutrition, and smoking [26,27,28]. In this study, subset analysis of subjects with known risk factors for pseudoarthrosis found that fusion rates were not significantly different between subjects with a single risk factor or multiple risk factors. These findings corroborate other reports of successful fusion and improvements in patient reported outcomes, despite comorbidities and risk factors that are known to negatively impact these outcomes [13].
The study presented several limitations that should be noted. Varying surgical approaches (e.g., TLIF, ALIF, PLF) were included within this analysis, as opposed to a single approach. This analysis does not include a control arm for comparison, the only comparison to outcomes identified within come from the available scientific literature. Despite these limitations, the preliminary data provided within this report demonstrates that CBA is an effective bone graft alternative and adjunct for patients being treated with lumbar spinal fusion.
Allograft infection can lead to disastrous complications such as nonunion of the graft-host junction and fracture of the graft requiring surgical intervention. While there has been a recent report of disease transmission through the usage of a different CBA where multiple tuberculosis cases in graft recipients were traced to a single donor lot [29], allogeneic bone has an extensive clinical safety record and Trinity allografts have never been linked to donor-derived infections after more than 13 years of being commercially available [30,31,32]. Prior to this incident, only one other occurrence of suspected tuberculosis disease transmission through the transplantation of allograft bone was identified in the published literature and that was reported nearly 70 years ago before modern donor screening criteria were established [33]. In order to address the risk of disease transmission with Trinity allografts, the medical and social history of each donor is carefully screened prior to donation for medical conditions or disease processes that would contraindicate the donation of tissue in accordance with current policies and criteria that have been established by FDA and the American Association of Tissue Banks (AATB). Subsequently, the processing and packaging of Trinity Elite allografts are performed under controlled aseptic conditions in an ISO Class 4 environment. Following processing, all donor batches are evaluated for sterility and must show no evidence of microbial growth complying with USP < 71 > Sterility Testing. Donor consent, infectious disease test results, medical history interviews, available medical records and any other information that may pertain to donor eligibility are evaluated by a medical director and must be deemed to be sufficient to indicate that donor tissues are suitable for transplantation [34, 35].
Conclusions
The use of CBA as a graft or primary adjunct material resulted in fusion rates comparable to ICBG and consistent across the entire patient population. Successful fusion was attained regardless of risk factor reported, and without the drawback of donor site morbidity and complications associated with bone morphogenetic protein products. This study adds significant value to current literature regarding CBAs and their efficacy in spinal fusion and provides an update to previously published data from the 12-month interim analysis of the study [17]. By preserving the inherent properties of these grafts, including the osteoinductive and osteogenic components retained within the bone matrix, CBAs provide a unique alternative and adjunct graft material to autograft.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Van Heest A, Swiontkowski M. Bone-graft substitutes. Lancet, 1999. 353 Suppl 1: p. Si28-9.
Migliorini F et al. Autologous bone grafting in trauma and orthopaedic Surgery: an evidence-based narrative review. J Clin Med, 2021. 10(19).
Younger EM, Chapman MW. Morbidity at bone graft donor sites. J Orthop Trauma. 1989;3(3):192–5.
Kwon B, Jenis LG. Carrier materials for spinal fusion. Spine J. 2005;5(6 Suppl):224S–30.
Buser Z, et al. Synthetic bone graft versus autograft or allograft for spinal fusion: a systematic review. J Neurosurg Spine. 2016;25(4):509–16.
Arrington ED et al. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res, 1996(329): p. 300–9.
Goulet JA, et al. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res. 1997;339:76–81.
Fernyhough JC, et al. Chronic donor site pain complicating bone graft harvesting from the posterior iliac crest for spinal fusion. Spine (Phila Pa 1976). 1992;17(12):1474–80.
Fowler BL, Dall BE, Rowe DE. Complications associated with harvesting autogenous iliac bone graft. Am J Orthop (Belle Mead NJ). 1995;24(12):895–903.
Ahlmann E, et al. Comparison of anterior and posterior iliac crest bone grafts in terms of harvest-site morbidity and functional outcomes. J Bone Joint Surg Am. 2002;84(5):716–20.
Gruskay JA, et al. Short-term adverse events, length of stay, and readmission after iliac crest bone graft for spinal fusion. Spine (Phila Pa 1976). 2014;39(20):1718–24.
Diaz RR, et al. Investigating the efficacy of allograft cellular bone matrix for spinal fusion: a systematic review of the literature. Neurosurg Focus. 2021;50(6):E11.
Elgafy H, et al. Lumbar spine fusion outcomes using a cellular bone allograft with lineage-committed bone-forming cells in 96 patients. BMC Musculoskelet Disord. 2021;22(1):699.
Hall JF, et al. Multilevel instrumented posterolateral lumbar spine fusion with an allogeneic cellular bone graft. J Orthop Surg Res. 2019;14(1):372.
Ammerman JM, Libricz J, Ammerman MD. The role of Osteocel Plus as a fusion substrate in minimally invasive instrumented transforaminal lumbar interbody fusion. Clin Neurol Neurosurg. 2013;115(7):991–4.
Tohmeh AG et al. Allograft cellular bone matrix in extreme lateral interbody fusion: preliminary radiographic and clinical outcomes ScientificWorldJournal, 2012. 2012: p. 263637.
Wind J et al. Twelve-month results from a prospective clinical study 2 evaluating the efficacy and safety of cellular bone allograft in 3 subjects undergoing lumbar spinal fusion. Neurol Int, 2022(14): p. 875–83.
Martin BI, et al. Trends in lumbar Fusion Procedure Rates and Associated Hospital costs for degenerative spinal Diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976). 2019;44(5):369–76.
Sengupta DK, et al. Outcome of local bone versus autogenous iliac crest bone graft in the instrumented posterolateral fusion of the lumbar spine. Spine (Phila Pa 1976). 2006;31(9):985–91.
Ohtori S, et al. Single-level instrumented posterolateral fusion of the lumbar spine with a local bone graft versus an iliac crest bone graft: a prospective, randomized study with a 2-year follow-up. Eur Spine J. 2011;20(4):635–9.
Ohtori S, et al. Single-level instrumented posterolateral fusion versus non-instrumented anterior interbody fusion for lumbar spondylolisthesis: a prospective study with a 2-year follow-up. J Orthop Sci. 2011;16(4):352–8.
Inage K et al. One, two-, and three-level instrumented posterolateral fusion of the lumbar spine with a local bone graft: a prospective study with a 2-year follow-up Spine (Phila Pa 1976), 2011. 36(17): p. 1392-6.
Lee SC, et al. In situ local autograft for instrumented lower lumbar or lumbosacral posterolateral fusion. J Clin Neurosci. 2009;16(1):37–43.
Copay AG, et al. Minimum clinically important difference in lumbar spine Surgery patients: a choice of methods using the Oswestry Disability Index, Medical outcomes Study questionnaire short form 36, and pain scales. Spine J. 2008;8(6):968–74.
Darveau SC, et al. Existing clinical evidence on the use of cellular bone matrix grafts in spinal fusion: updated systematic review of the literature. Neurosurg Focus. 2021;50(6):E12.
Derman PB, Singh K. Surgical strategies for the Treatment of Lumbar Pseudarthrosis in degenerative spine Surgery: a Literature Review and Case Study. Hss j. 2020;16(2):183–7.
Raizman NM, et al. Pseudarthrosis of the spine. J Am Acad Orthop Surg. 2009;17(8):494–503.
Yavin D, et al. Lumbar Fusion for degenerative Disease: a systematic review and Meta-analysis. Neurosurgery. 2017;80(5):701–15.
Schwartz NG, et al. Nationwide Tuberculosis outbreak in the USA linked to a bone graft product: an outbreak report. Lancet Infect Dis. 2022;22(11):1617–25.
Kasis AG, et al. Novel bone grafting technique in stand-alone ALIF procedure combining allograft and autograft (‘Northumbria technique’)-Fusion rate and functional outcomes in 100 consecutive patients. Eur Spine J. 2021;30(5):1296–302.
Li R, et al. Notes from the field: Tuberculosis outbreak linked to a contaminated bone graft product used in spinal Surgery - Delaware, March-June 2021. MMWR Morb Mortal Wkly Rep. 2021;70(36):1261–3.
Kappe T, et al. Infections after bone allograft Surgery: a prospective study by a hospital bone bank using frozen femoral heads from living donors. Cell Tissue Bank. 2010;11(3):253–9.
Mroz TE, et al. The use of allograft bone in spine Surgery: is it safe? Spine J. 2009;9(4):303–8.
James JI. Tuberculosis transmitted by banked bone. J Bone Joint Surg Br, 1953. 35–b(4): p. 578.
Gocke DJ. Tissue donor selection and safety. Clin Orthop Relat Res, 2005(435): p. 17–21.
Acknowledgements
We thank Stephanie E. Tedford, PhD, of Pharmacologics, Inc, who, on the behalf of Orthofix, Inc assisted in the implementation of author revisions and Deanna Naomi Schreiber-Gregory, MS, Biostatistician for data analysis.
Funding
This study was supported by Orthofix Medical, Inc. (Lewisville, TX, USA).
Author information
Authors and Affiliations
Contributions
All authors have contributed to at least (1) study concept/design, (2) Data acquisition, (3) Statistical analysis and/or Data interpretation. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board (IRB) at each respective clinical site for studies involving humans. Primary approval was obtained from Western IRB and WCG IRB. Institutional IRB approvals were obtained from the Univ. of Virginia IRB and the Oregon Health & Science University IRB. None of the authors on this study are members of the IRB approval committees. Informed consent was obtained from all subjects involved in the study.
Consent for publication
Not applicable.
Competing interests
All authors disclose research support provided by Orthofix. The authors declare there are no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, D.K., Wind, J., Lansford, T. et al. Twenty-four-month interim results from a prospective, single-arm clinical trial evaluating the performance and safety of cellular bone allograft in patients undergoing lumbar spinal fusion. BMC Musculoskelet Disord 24, 895 (2023). https://doi.org/10.1186/s12891-023-06996-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06996-5