Abstract
Background and purpose
Clinical status of subjects with knee osteoarthritis (KOA) is influenced by a complex interaction of several biopsychosocial factors. The use of patient-reported measures (PROM) is considered the gold standard for their evaluation. However, considering that 1 in 5 subjects with KOA present with depressive symptoms, it is necessary to analyse how this psychological domain may influence the subjective perception of PROM. The objective was to study the impact that depressive symptoms have on functional outcome assessments, according to the degree of objectivity of diverse outcome measures.
Methods
Cross-sectional study. Subjects with severe KOA, verified with clinical and radiological symptoms, were assessed with patient-reported (Oxford Knee Score), clinician-reported (knee range of motion), and performance-based (Timed up and go test) measures. The existence of depressive symptoms was assessed with the Yesavage scale, and participants were classified for having no-, mild- or severe-symptoms. Linear correlations (r) and one-way analysis of variance compared groups (95% CI).
Results
244 participants were analysed, of which 75 (30.7%) had depressive symptoms. These symptoms had an inverse moderate association with Oxford Knee Score (r = -0.387). However, the correlation with the Timed up and go test was low (r = 0.176), while there was no correlation with knee ROM (r = -0.087).
Conclusions
This study supports that patient-reported questionnaires may offer biased information on the clinical status of patients with severe knee osteoarthritis who present with depressive symptoms. Consideration of such symptoms may be critical to ensure data collected to accurately reflect patients’ capacities and perceptions.
Similar content being viewed by others
Introduction
Patients with severe knee osteoarthritis (KOA) report persistent pain and limited functional capacity. Both clinical symptoms are influenced by a complex interaction between psychological, pathological, socio-demographic, and disability factors, commonly present in KOA [1,2,3]. Indeed, these patients frequently present with depressive symptoms associated with their condition [4, 5], with an approximate prevalence of 20% [6,7,8].
The diagnosis of KOA is verified through radiological evaluation after the appearance of clinical symptoms. A number of psychometrically validated outcome measures are available to assess such symptoms [9]. Regarding pain in KOA, it is considered nociceptive, and patients’ perceptions directly influence their routine assessment with PROM [2, 10, 11]. However, the assessment of functional capacity may depend on whether the point of view is that of the assessor or the patient, and on the degree of objectivity of the outcome measure used: firstly, the so-called clinician-reported measures are claimed to offer objective information (e.g. joint range of motion (ROM), strength); secondly, measures based on performance estimate functional capacity in basic tasks, such as walking or climbing stairs [12]; finally, patient-reported questionnaires are characterized by considering the patient’s perception in a wide range of functional activities, offering a more subjective view [9]. Precisely, these questionnaires have been for several decades the gold standard in KOA [13], and the most frequently used [14].
Previous studies have investigated the association between psychologic status and clinical symptoms in KOA, and how this status can impact on total knee replacement outcome [15]. This verified the existence of a significant association with pain [10, 11, 16]. Regarding functional capacity, some studies appraised such association using PROM specifically. The findings were non-consistent across trials and supported that depressive symptoms could either have an influence on functional assessment [17] or not [18]. Other studies also included performance-based measures to appraise this association [2, 19]. However, no study classified the findings considering the degree of objectivity of the outcome measure used, according to the previously exposed [20, 21].
Ensuring that PROM results accurately reflect clinical symptoms is crucial to successful application. The objective was to evaluate whether the existence of depressive symptoms could influence PROM resultant scores. To this end, the association between depressive symptoms and PROM scores was determined, and then, it was compared whether this association occurred when clinical symptoms were evaluated with outcome measures that provide information from other points of view (i.e., clinician-reported or based on performance).
Methods
Cross-sectional study recruiting the sample from two university hospitals, Hospital Clínico Universitario and Hospital Universitario y Politécnico La Fe from Valencia, Spain. The University of Valencia was responsible for the integrity and conduct of the study, which adhered to the Helsinki ethical guidelines and successive updates. The procedures were approved by the ethical boards of the institutions (no. 2018/0621 and no. 2018/280). All methods were performed in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement.
All participants were informed verbally and in writing of the purpose of the study and signed an informed consent to participate. Patients aged between 60 and 80 years old, diagnosed with severe KOA, were eligible for the study. The condition was verified with radiography assessment, i.e., a result of 4 on the Kellgren-Lawrence scale (values from 0 to 4), and clinical symptoms, i.e. pain ≥ 3 on the visual analogue scale (VAS, values from 0 to 10). Those participants incapable to follow verbal instructions, or who suffered from some vestibular, neurological and/or cognitive alteration that did not allow the understanding or correct execution of the tests and questionnaires were excluded. The data were collected between May and June 2019.
Data collection
Potentially eligible participants were referred by two orthopaedic surgeons. Two researchers were in charge of collecting the data and verifying compliance with the eligibility criteria. One of them was assigned to collect demographic and clinical information and explain the tests, while the other supervised their correct execution.
In accordance with the objectives of the study, all patients were assessed for psychological and functional status. Data were collected in a single session.
Psychological status was assessed by determining the presence of depressive symptoms using the Spanish version of the Yesavage Geriatric Depression Scale, a standardised 15-question questionnaire, with yes or no answers, for a final score of 0 to 15, which determines three degrees of severity of depression. This scale has been shown to be a reliable tool to assess depressive symptoms among elderly people, with the Spanish version validated too [22]. The assessment was carried out in an isolated room, where there was only an assessor who verbally explained the instructions of the scale and wrote down the answers offered by the participants.
Functional status was measured in its 3 dimensions with varying degrees of objectivity: patient-, clinician-reported and performance-based. (I) The Spanish version of the Oxford Knee Score (OKS), a patient-reported outcome specifically designed and developed to assess people with severe knee OA, was used as PROM measurement. The Spanish version has been validated, revealing excellent test-retest reliability (ICC 0.993; IC 95%: 0.990–0.995) [23]. The scale consists of 12 questions about an individual’s functional activities of daily living and how they have been affected by typical symptoms of the disease over the past four weeks, reporting from none to maximum impossibility for each activity, resulting in a final score ranging from 0 (minimum functionality) to 48 (maximum functionality). The assessor explained the instructions verbally and the participants completed the questionnaire. (II) Clinician-reported functionality was obtained by measuring the knee range of motion by using a telescopic goniometer, being this measurement validated [24]. (III) Performance-based functionality for common daily tasks, such as walking or getting up from a chair, was estimated with the Timed up and go test (TUG). This test has been shown to describe dynamic balance and mobility, capacities with a relevant impact on functionality [25]. To perform the test, the patient gets up from a chair, walk 3 m, turn around a cone, go back and sit down again in the shortest possible time. Time was measured with a stopwatch, with the shortest time obtained being the highest functionality.
To reinforce analyses and verify the consistency of the results, this study compared the collected data with two factors that had been shown to associate with depressive symptoms: quality of life, estimated with the European Quality of Life-5 Dimensions (EQ-5D) health-related questionnaire [26], and pain, estimated with a visual analogue scale (VAS) with scores that ranged from 0, the worse possible pain, to 10, no pain. The EQ-5D results were calculated according to the database scores available for the Spanish population, with a VAS score from 0, the worse, and 1, the best possible health-related quality of life.
Analysis of data
A univariate analysis described the clinical and demographic characteristics of the sample, including means, standard deviations and frequencies (SPSS version 22.0, IBM®, licensed from the University of Valencia). The normality of the distribution for the quantitative variables was verified using Kolmogorov-Smirnov test. The possible association between depressive symptoms and function, pain and quality of life was sought. Pearson’s partial correlation coefficients, considered a low, moderate or high association between limits of r = 0.2 and 0.5. Furthermore, the sample was classified according to the severity of depressive symptoms, so that scores from < 5, < 10 and up to15, were considered as non-existent, mild or severe depressive symptoms respectively [27]. One-way analysis of variance was performed using the severity of depressive symptoms as an independent factor and the clinical variables (functional capacity, pain, and quality of life) as dependent. All confidence intervals were established at 95%. An estimate of the necessary sample was carried out with Z-correlation tests with independent variables in which an effect size q = 0.6 was intended, with α = 0.05 and β = 0.2 [28], for which a sample greater than 150 participants was necessary.
Results
Of the 283 potential participants with diagnosed knee OA who were assessed for eligibility, 244 subjects were finally included in the study and analysed. The mean age of the participants was 71.2 (SD 6.9) years, of which 69.3% (n = 169) were women; 75 patients (30.7%) reported mild to severe depressive symptoms (score > 5 Yesavage scale), with a mean response of 4.3 (SD 3.1). The detailed characteristics of the individuals are shown in Table 1 and the diagram of the participants in Fig. 1.
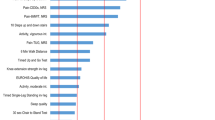
The data analyses revealed that depressive symptoms did impact self-reported functionality. Specifically, correlation study demonstrated a moderate and inverse relation between depressive symptoms and PROM (Table 2). That implies that as the Yesavage score increases, the OKS score decreases. Furthermore, ANOVA results revealed the significance of symptoms severity on OKS scores (p < 0.001), as illustrated in Fig. 2. However, the correlation coefficient between depressive symptoms and the Timed up and go test was low, while there was no correlation with clinician-reported assessment.
People with no depressive symptoms (DS), moderate DS, or severe DS. Three types of assessments are presented: (1) left side of the figure: patient-reported (OKS: Oxford Knee Score); (2) center, based on performance (TUG: Timed up and go) and (3) right side, clinician-reported (ROM: Knee range of motion). * p < 0.001 in one-way ANOVA looking for group (i.e. no, moderate or severe DS) differences. * Indicates between-groups differences with p < 0.01
As expected, pain and quality of life showed a positive association with the Yesavage scale, so that the higher the scores, the lower the quality of life and the greater the pain, as it can be observed in Table 2. Again, there were significant differences according to the severity of the symptoms (p < 0.05).
Discussion
This research found that PROM scores were associated with the existence of depressive symptoms in patients with severe knee OA. However, these symptoms had little or no association with performance-based and clinician-reported functional assessments, respectively. Therefore, this study supports that (1) the existence of depressive symptoms should be evaluated in routine assessments; especially, considering that PROM have been the gold standard for clinical verification in subjects with KOA, and that the rate of depressive symptoms is high (consistently, it was registered an approximate of 30% [7, 8]); (2) functional measures based on both the perception of patients and assessors should be also used in practice. These findings contribute to a more complete picture of the functional status of patients with KOA, and how psychological status influences the patient’s self-perception of health.
It is well established in the current literature that functional status depends on the interaction of various physical and bio-psycho-social factors [16, 29], which has led to a renewed interest over the last decade in understanding how these factors interact with each other and concretely, how depression can impact on a patient’s functional status.16 In this context, the results obtained in this study, showing a significant association between depressive symptoms and patient-reported outcomes, are consistent with previous studies [2, 16, 19, 20], although some others failed to demonstrate this association [10, 18]. Therefore, a firm conclusion regarding the existence of an association between depressive symptoms and functional reports cannot yet be drawn, as shown in the review by Calders et al. [21]. In addition, this review also found a large heterogeneity in the sample analyzed, which meant that the overall quality of this evidence was rated as very low. To address this issue, standardization of diagnostic criteria, the adoption of uniform assessment tool, and a large emphasis to identifying and controlling those variables that may interfere with the results (i.e. body mass index, i.e. age) could provide a more comprehensive understanding of the status of patients with KOA and facilitate more robust conclusions [30].
In the present study, while depressive symptoms were significantly correlated with patient-reported outcome, this correlation was low with performance-based measure, and nonexistent with knee ROM. This result supported that depressive symptom may influence the perception that patients with KOA have about their functional capacity, but not necessarily the outcome of less subjective measures or not reliant on patients’ perception. Therefore, when a patient with KOA presents with depressive symptoms, functional outcomes may differ depending on whether objective or self-reported measures are used. Different reasons have been proposed to explain the link between depression and worsening PROMs, as the direction of the cause-effect relationship is not entirely clear, and it is not known what precedes it [31]. It has been suggested that depression contributes to fear-avoidance behavior and kinesiofobia, which may have a negative impact on perceived capacity [32]. On the other hand, patients with KOA who report lower coping skills require more medical attention and are more dissatisfied with the treatment they receive [33]. As poorer functional perception and depression are bidirectionally related and feedback negatively on each other [34], it is first necessary to correctly identify these situations and address them together, providing self-care management programs, in order to break the vicious circle [35].
Objective measurements, such as knee motion or performance-based test (TUG) seems to be less influenced by the depress level of the patient. However, not all the literature seems to agree with this perspective, and some authors did find a significant association between higher depression and worse results of objective functional capacity [2, 16, 35, 36], emphasizing that pain also plays a determining role [2] – consistent with our results. As the literature offers different points of view, it is worth considering the factors that might lead to different results. Some studies analyzed specific populations (i.e. only women [16]) or those with comorbidities (e.g. obese, women [16, 35]). The association between depressive symptoms and functional capacity had already been investigated in patients with KOA, but no study analyzed this relationship by classifying the findings according to the degree of objectivity of the outcome measure. For such reason, it was assessed two additional factors for which the influence of depressive symptoms had been well established: pain and quality of life [10]. As expected, we found a significant association between these factors, which reinforces the findings.
PROMs are considered the gold standard in the functional evaluation of patient with KOA, and the results largely determines the therapeutic procedure to be applied, with those with high levels of pain and disability being eligible to undergo total knee replacement [37]. However, despite their widespread use, PROMs have also faced criticism, due to patient’s reports may be susceptible to influences such as social desirability bias or difficulties in accurately quantifying and recalling pas emotions and experiences [38]. Furthermore, this study suggests that, given the high prevalence of depressive symptoms in patients with KOA, it is important to interpret PROMs results while considering the potential influence of depression, which can confound patients’ perceptions [1].
Regarding clinical application, the findings of this study align with the emerging perspective for comprehending pain in individuals with KOA, transitioning from a purely mechanical viewpoint to a biopsychosocial paradigm [39]. This research contributes new evidence on understanding the influence of psychological state in the patient’s functional status. Within this framework, several actions may be taken. Firstly, a comprehensive assessment of psychological well-being may aid in the recognition of depressive symptoms and the identification of potential barriers affecting patients’ self-assessments of their health. Secondly, the incorporation of objective or self-reported measures can contribute to a more comprehensive and reliable evaluation of the patient, reducing the likelihood of bias. Additionally, this approach may assist in resolving potential discrepancies between radiological and clinical findings [12], ultimately leading to greater specificity when considering personalized or elective treatment options.
As a strength, the sample size and possible external validity should be highlighted, given that the sample was collected in two centers and, in terms of age and sex, it is generalizable to the population suffering from KOA [8].
On the other hand, it is necessary to mention limitations, such as that depressive symptoms and their association with different functional and patient-reported parameters were analyzed, but not with other factors that may be likely related to worse patient-reported functionality, such as the social environment or work of the individual, sex, weight or increasing age. Likewise, in future research it would be interesting to assess the existence and degree of sarcopenia in a population with knee OA, since it is a frequent finding in elderly individuals that is also negatively related to functionality [40]. The prevalence of depressive symptoms in the sample of this study was within the established ranges, although it was slightly higher than the average of other studies (20% vs. 30%) [8], which may influence a more marked decrease in physical activity performed by individuals.
Conclusion
This study supports that the existence of depressive symptoms associates with worse outcome in patient-reported functional assessments. However, the correlation is very low with functional capacity and non-existent with knee function. Therefore, patient-reported questionnaires may offer a biased perspective of the functional status of patients with severe knee osteoarthritis who present with depressive symptoms. It is recommended to assess the psychological status on a routine basis, and to include functional measures that consider the perspective of clinicians and patients, as this can help in the design of individualized treatments.
Data availability
The datasets generated or analysed during the current study are available from the corresponding author on reasonable request.
6. References
Helminen EE, Arokoski JPA, Selander TA, Sinikallio SH. Multiple psychological factors predict pain and disability among community-dwelling knee osteoarthritis patients: a five-year prospective study. Clin Rehabil. 2020;34(3):404–15.
Iijima H, Aoyama T, Fukutani N, Isho T, Yamamoto Y, Hiraoka M, et al. Psychological health is associated with knee pain and physical function in patients with knee osteoarthritis: an exploratory cross-sectional study. BMC Psychol. 2018;6(1):1–10.
Stegenga BT, Nazareth I, Torres-González F, Xavier M, Švab I, Geerlings MI, et al. Depression, anxiety and physical function: exploring the strength of causality. J Epidemiol Community Health. 2012;66(7):1–8.
Martín AG, Soler RS, Picart PA, Comas Casanovas P. Niveles De Ansiedad Y depresión en enfermos hospitalizados y su relación con la gravedad de la enfermedad. Med Clin (Barc) [Internet]. 2003;120(10):370–5. https://doi.org/10.1016/S0025-7753(03)73707-5.
Pereira D, Severo M, Barros H, Branco J, Santos RA, Ramos E. The effect of depressive symptoms on the association between radiographic osteoarthritis and knee pain: a cross-sectional study. BMC Musculoskelet Disord [Internet]. 2013;14(1):1.
Sale JEM, Gignac M, Hawker G. The relationship between Disease symptoms, life events, coping and treatment, and depression among older adults with osteoarthritis. J Rheumatol. 2008;35(2):335–42.
Stubbs B, Aluko Y, Myint PK, Smith TO. Prevalence of depressive symptoms and anxiety in osteoarthritis: a systematic review and meta-analysis. Age Ageing. 2016;45(2):228–35.
Vergés Milano J, Herrero Barbero M, Giménez Basallote S, Vergara Martín J, Viles Lladó E, Martínez Serrano H, et al. Anxiety and depression in knee osteoarthritic patients: results from EMARTRO study. Osteoarthr Cartil. 2016;24(2016):218–9.
Veronese N, Stubbs B, Solmi M, Smith TO, Noale M, Cooper C, et al. Association between lower limb osteoarthritis and incidence of depressive symptoms: data from the osteoarthritis initiative. Age Ageing. 2017;46(3):470–6.
Samuel AJ, Kanimozhi D. Outcome measures used in patient with knee osteoarthritis: With special importance on functional outcome measures. Int J Health Sci (Qassim) 2019;13(1):52–60. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC6392485.
Zullig LL, Bosworth HB, Jeffreys AS, Corsino L, Coffman CJ, Oddone EZ, et al. The association of comorbid conditions with patient-reported outcomes in veterans with hip and knee osteoarthritis. Clin Rheumatol. 2015;34(8):1435–41.
Kim KW, Han JW, Cho HJ, Chang CB, Park JH, Lee JJ, et al. Association between comorbid depression and osteoarthritis symptom severity in patients with knee osteoarthritis. J Bone Jt Surg - Ser A. 2011;93(6):556–63.
Dobson F, Hinman RS, Hall M, Terwee CB, Roos EM, Bennell KL. Measurement properties of performance-based measures to assess physical function in hip and knee osteoarthritis: a systematic review. Osteoarthr Cartil [Internet]. 2012;20(12):1548–62. https://doi.org/10.1016/j.joca.2012.08.015.
Samuel AJ, Kanimozhi D. Outcome measures used in patient with knee osteoarthritis: with special importance on functional outcome measures. Int J Health Sci (Qassim) [Internet]. 2019;13(1):52–60.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40.
Wolfe F, Kong XS. Rasch analysis of the Western Ontario MacMaster Questionnaire (WOMAC) in 2205 patients with osteoarthritis, rheumatoid arthritis, and fibromyalgia. Ann Rheum Dis. 1999;58(9):563–8.
Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res. 2010;468(3):798–806.
Mora JC, Przkora R, Cruz-Almeida Y. Knee osteoarthritis: pathophysiology and current treatment modalities. J Pain Res. 2018;11:2189–96.
Creamer P, Lethbridge-Cejku M, Hochberg MC. Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology. 2000;39(5):490–6.
Sheng L, Christopher M. AM HHS Public Access Physiol Behav. 2016;176(1):100–6.
Nur H, Sertkaya BS, Tuncer T. Determinants of physical functioning in women with knee osteoarthritis. Aging Clin Exp Res. 2018;30(4):299–306.
Zambon S, Siviero P, Denkinger M, Limongi F, Van Der Castell MV, et al. Role of Osteoarthritis, Comorbidity, and Pain in determining functional limitations in older populations: European Project on Osteoarthritis. Arthritis Care Res. 2016;68(6):801–10.
Calders P, Van Ginckel A. Presence of comorbidities and prognosis of clinical symptoms in knee and/or hip osteoarthritis: a systematic review and meta-analysis. Semin Arthritis Rheum. 2018;47(6):805–13.
Mahler EAM, Boers N, Bijlsma JWJ, Van Den Hoogen FHJ, Den Broeder AA, Van Den Ende CHM. Patient acceptable symptom state in knee osteoarthritis patients succeeds across different patient-reported outcome measures assessing physical function, but fails Across Other dimensions and Rheumatic Diseases. J Rheumatol. 2018;45(1):122–7.
Gomez-Angulo C, Campo-Arias A. Geriatric depression scale (GDS-15 and GDS-5): a study of the internal consistency and factor structure | escala de yesavage para depresi?n geri?trica (GDS-15 y GDS-5): Estudio de la consistencia interna y estructura factorial. Univ Psychol. 2011;10(3):735–44.
Martín-Fernández J, García-Maroto R, Sánchez-Jiménez FJ, Bau-González A, Valencia-García H, Gutiérrez-Teira B et al. Validation of the Spanish version of the Oxford knee score and assessment of its utility to characterize quality of life of patients suffering from knee osteoarthritis: a multicentric study. Health Qual Life Outcomes. 2017;15(1).
Módica M, Ostolaza M, Abudarham J, Barbalaco L, Dilascio S, Drault-Boedo ME, et al. Validación Del timed up and go test como predictor de riesgo de caídas en sujetos con artritis reumatoide. Parte I: confiabilidad y aplicabilidad clínica. Rehabilitacion [Internet]. 2017;51(4):226–33. https://doi.org/10.1016/j.rh.2017.07.001.
Szende A, Williams A. Measuring Self-Reported Population Health: An International Perspective based on EQ-5D. EuroQol Group. 2004.
Scott W, Weiss R. Sample size and power calculations for correlations between bivariate longitudinal data. Stat Med. 2010;31(1):1–7.
Yázigi F, Espanha M, Marques A, Teles J, Teixeira P. Predictors of walking capacity in obese adults with knee osteoarthritis. Acta Reumatol Port. 2018;2018(4):256–63.
Sharma L, Cahue S, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of Psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–70.
Pereira D, Ramos E, Branco J, Osteoarthritis. Revista Cient De Orden dos médicos. 2015;28(1):99–106.
Cruz-Almeida Y, King CD, Goodin BR, et al. Psychological profiles and Pain characteristics of older adults with knee osteoarthritis. Arthritis Care Res. 2013;65(11):1786–94. https://doi.org/10.1002/acr.22070.
Fingleton C, Smart K, Moloney N, Fullen BM, Doody C. Pain sensitization in people with knee osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(7):1043–56. https://doi.org/10.1016/j.joca.2015.02.163.
Pitsillides A, Stasinopoulos D, Giannakou K. The effects of cognitive behavioural therapy delivered by physical therapists in knee osteoarthritis pain: a systematic review and meta-analysis of randomized controlled trials. J Bodyw Mov Ther. 2021;25:157–64. https://doi.org/10.1016/j.jbmt.2020.11.00233.
Morandi A, Onder G, Fodri L, Sanniti A, Schnelle J, Simmons S, et al. The Association between the probability of Sarcopenia and Functional outcomes in older patients undergoing In-Hospital Rehabilitation. J Am Med Dir Assoc [Internet]. 2015;16(11):951–6.
Song MR, Lee YS, Baek JD, Miller M. Physical activity status in adults with Depression in the National Health and Nutrition Examination Survey, 2005–2006. Public Health Nurs. 2012;29(3):208–17.
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conception: JMB, FDN, JPM. Design: All the authors. Data acquisition: JPM, SRC, BDD. Method, statistical and economic analysis counselling: JMB, SRC, CGG, FQG. Redaction of the article: FDN, JPM and JMB. Revising it critically for important intellectual content: FDN, JPM, SRS, JMB, FQG. All authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Ethics approval
The trial was approved by the Ethical Committee for Clinical Research and by the Scientific Committee of the Hospital Clínico Universitario and the Hospital Politécnico y Universitario de La Fe de Valencia (no. 2018/0621 and no. 2018/280).
Informed consent
Informed consent was obtained from all participants.
Conflicts of interest/Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Pérez-Maletzki, J., Domínguez-Navarro, F., Roig-Casasús, S. et al. Patient, clinician, and performance-based measures provide different information about clinical symptoms in patients with severe knee osteoarthritis presenting with depressive symptoms: a cross-sectional study. BMC Musculoskelet Disord 24, 833 (2023). https://doi.org/10.1186/s12891-023-06971-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06971-0