Abstract
Background
This study aimed to determine the prognostic outcome of hip joint replacement after resection of proximal femoral tumors by reviewing original studies.
Methods
Two researchers independently searched PubMed, Embase, Cochrane Library, and Web of Science databases from inception to July 17, 2022. Then, the literature was screened by inclusion criteria. The basic information, primary outcomes, and secondary outcomes were extracted for weighted combined analysis. The quality of the included literature was evaluated using the Newcastle–Ottawa scale.
Results
Twenty-four retrospective cohort studies comprising 2081 patients were included. The limb salvage rate was 98%. The survival rates at 1, 2, 3, 4, and 5 years were 80, 72, 65, 64, and 55% for patients with primary tumors and the rate at 1, 2, 3, 4, and 5 years were 44, 25, 17, 14, and 11% for patients with bone metastases, respectively.
Conclusion
As chemotherapy and radiotherapy treatment progressed, joint reconstruction after proximal femoral tumor resection improved patients' function and quality of life.
Similar content being viewed by others
Background
Primary and secondary bone tumors can occur in bone and cartilage tissues [1]. Primary bone tumors occur in children and adolescents and are an important contributor to death and disability in this age group [2]. Secondary bone tumors, i.e., bone metastases, are 30–40 times more common than primary ones and are characterized by higher prevalence and poor quality of life [3]. Except for the spine, the proximal femur is the most frequent site of bone metastases (approximately 10%) and is the most commonly affected long bone [4]. The risk of pathologic fracture of the proximal femur metastases is high due to weight bearing and biomechanical conditions [5].
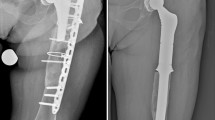
One of the most important objectives in treating proximal femoral tumors is to reduce pain to provide a better quality of life for the patient. Limb-preserving surgery has gradually become the main surgical modality for bone tumors [6]. With the advancement of relevant, comprehensive treatments, the goal of treatment for bone tumors requires improving patient survival and preserving good limb function [7]. Metal tumor-based artificial joints are currently the first choice for functional reconstruction after limb preservation surgery due to the advantages of immediate postoperative restoration of affected limb function, early mobility, and long-term functional satisfaction [8].
The preferred reconstruction method for patients with proximal femoral tumors is prosthetic replacement after tumor resection. Due to the low incidence and limited follow-up time, reports of clinical outcomes, survival, prosthetic survival, and function of patients after surgery vary widely in original studies. A systematic evaluation meta-analysis published by Thambapillary et al. [9] in 2013 reported a limb preservation rate of over 90%, a 5-year prosthetic survival rate of 84%, and an overall revision rate of 11% without addressing patient survival. In contrast, the systematic evaluation published by Brown et al. [10] in 2018 only qualitatively described the relevant data. Based on the publication of several relevant original studies in recent years, this study intends to update and supplement the analysis of clinical outcomes, complications, survival, prosthetic survival, and function of metal prosthesis replacement after proximal femoral tumor resection and subgroup analysis was according to follow-up time, prosthesis type, and tumor type to bring reference for clinical decision-making.
Material and methods
Literature search
This systematic review was reported according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analysis) guidelines. Two investigators independently conducted database searches, and arguments were resolved through discussion. PubMed, Embase, Cochrane Library, and Web of Science databases were searched from inception to July 17, 2022. The search strategy was "Neoplasms" AND "Arthroplasty, Replacement, Hip" and was limited to English-language papers.
Eligibility criteria
The inclusion criteria were: 1) patients diagnosed with a proximal femoral tumor; 2) hip replacement after tumor resection; 3) cohort study. The exclusion criteria were: 1) number < 10; 2) conference abstracts, and reviews; 3) revision surgery; 4) unavailability of the full text.
Literature screening and data extraction
Two investigators independently screened the literature and extracted data. After literature de-duplication, irrelevant literature was excluded by reading the title and abstract, and the full text of relevant literature was further analyzed. Data were extracted based on a pre-designed table, including authors, year of publication, country, total number, gender, age, and follow-up time. The primary outcomes included overall patient survival and limb preservation rate. The secondary outcomes included limb salvage rate (the proportion of patients who avoided amputation at end of follow-up period), prosthesis survival, revision rate, hemi to total hip conversion rate, tumor status, complications, and function based on the Musculoskeletal Tumor Society, 1993, MSTS.
Risk of bias assessment
The quality of the included literature was assessed using the Newcastle–Ottawa scale (NOS). The following characteristics were assessed: representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, the demonstration that the outcome of interest was not present at the start of the study, comparability of cohorts based on the design or analysis, or outcome assessment, whether the follow-up was long enough for outcomes to occur, and adequacy of follow-up of cohorts.
Data synthesis and statistical analysis
Data were analyzed using R software (v. 6.0). Individual rates were combined using double inverse sine transformation [11], and the rate and 95% confidence intervals (CIs) were calculated. Cochran-Q test for heterogeneity and I2 evaluated the magnitude of heterogeneity. An I2 > 50% was considered high heterogeneity, and a random effects model was used; for I2 ≤ 50%, a fixed effects model was used. The survival data were captured from Kaplan–Meier (K-M) curves using Engauge Digitizer software. The subgroup analysis was performed according to follow-up time, prosthesis type, and tumor type. The publication bias was assessed using Egger's test, and the sensitivity analysis was performed by excluding individual studies on a case-by-case basis.
Results
Literature search results
A total of 4486 studies were searched. After excluding duplicates (1137), the title and abstract of 3349 studies were analyzed, and 70 studies were selected for full-text screening. Two studies with < 10 patients, three revision-related reports, two conference abstracts, 13 with unextractable data, 11 with irrelevant study content, and 15 non-proximal femoral tumors were excluded. Finally, 24 studies were included for analysis. The selection process is shown in Fig. 1.
Studies description
The 24 included papers were retrospective cohort studies (Table 1) comprising 2081 patients, with the number of males ranging from 4–236 in each study and the number of females ranging from 8–468. The age at surgery ranged from 27.8–66.1 years, and the follow-up period ranged from 3–216 months. The year of publication for each study ranged from 1998–2020. The countries with the most published studies were the United States (12), China (3), and the United Kingdom (2).
Methodological quality of included studies
The results of the NOS evaluation form showed that three of the 24 articles scored 8, 12 scored 7, and nine scored 6. There was no literature with a high risk of bias.
Intraoperative bleeding, operative time, hospital days, and postoperative function
Four studies (123 patients) reported intraoperative bleeding in patients with a bleeding volume of 630 mL (95% CI: 501.53–759.28, I2 = 94%). Five studies (827 patients) reported an operative time of 123.85 min (95% CI: 110.30–137.39, I2 = 100%). Four (154 patients) reported the number of hospital days (10.47 d, 95% CI: 8.64–12.30, I2 = 99%). Nine studies (265 patients) measured the postoperative patient function using the MSTS 93 scale, with a combined score of 22.5 (95% CI: 20.43–24.56, I2 = 98%) (Table 2).
Survival rate of patients
Patient survival rates at 1, 2, 3, 4, and 5 years were 69% (95% CI: 56–82%), 53% (95% CI: 37–69%), 46% (95% CI: 28–64%), 42% (95% CI: 22–62%), and 36% (95% CI: 24–48%), respectively (Additional file 2: Appendix Table 1). Patients with primary tumors, custom-made prostheses, and total hip replacements have a higher survival rate than those with metastases, modular-made prostheses, and hemi-hip replacements. The subgroup analysis according to tumor type showed that the survival rates at 1, 2, 3, 4, and 5 years were 80, 72, 65, 64, and 55% for patients with primary tumors and rate at 1, 2, 3, 4, and 5 years were 44, 25, 17, 14, and 11% for patients with bone metastases, respectively. The subgroup analysis according to the type of prosthesis showed that the 1, 2, 3, 4, and 5-year survival rates were 93, 80, 70, 67, and 60% for patients with custom-made prostheses, 66, 48, 38, 37, and 32% for patients with modular-made prostheses. The 1, 2, 3, 4, and 5-year survival rates were 73, 56, 51, 48, and 47% for patients with hemi-hip replacements and 93, 82, 74, 69, and 57% for patients with total hip replacements, respectively (Table 3).
Survival rate of prosthesis
The survival rates for prostheses at 1, 2, 3, 4, and 10 years were 98% (95% CI: 96–100%), 97% (95% CI: 95–100%), 89% (95% CI: 83–96%), 88% (95% CI: 80–95%), and 73% (95% CI: 58–89%) (Additional file 2: Appendix Table 1). Prosthesis survival did not differ between tumour types or prosthesis types. The subgroup analysis according to tumor type showed that the 1 and 2-year prosthesis survival rates were 100% for patients with primary tumors and bone metastases. The subgroup analysis according to prosthesis type showed that the 1- and 2-year survival rates were 100 and 95% for custom-made prostheses, 100% for modular-made prostheses, 94 and 93% for hemi-hip replacement, and 100 and 95% for total hip replacement, respectively (Table 4).
Prosthesis revision rate
The overall prosthesis revision rate was 9% (95% CI: 5–15%, I2 = 86%) (Fig. 2). The subgroup analysis based on follow-up time showed that the revision rates were 2, 8, 21, and 47% at 2, 5, 10, and 20 years, respectively. Moreover, the subgroup analysis based on prosthesis type showed that the revision rate was 11% for custom-made prostheses and 8% for modular-made prostheses (Additional file 2: Appendix Table 2). Additionally, three studies described the causes of revision, with the main causes being aseptic loosening and infection.
The rate of hemi to total hip conversion was 3% (95% CI: 1–6%, I2 = 74%) (Additional file 2: Appendix Fig. 1). The subgroup analysis based on follow-up time showed revision rates of 2 and 5% at 2–5 and 6–10 years of follow-up, respectively. Besides, the prosthesis type subgroup analysis showed a revision rate of 3% for custom-made prostheses (Additional file 2: Appendix Table 3).
Limb salvage rate
The overall limb salvage rate was 98% (95% CI: 95–99%, I2 = 65%) (Fig. 3). The follow-up time subgroup analysis showed that the limb preservation rates were 98 and 97% at 2–5 and 6–10 years, respectively. The prosthesis type subgroup analysis showed that the limb salvage rate was 91% for custom-made prostheses and 99% for hemiarthroplasty (Additional file 2: Appendix Table 4).
Local recurrence rate of tumors
Moreover, the local recurrence rate was 7% (95% CI: 4–11%, I2 = 75%) (Fig. 4). Based on the follow-up time subgroup analysis, the local recurrence rates were 6 and 8% at 2–5 and 6–10 years of follow-up, respectively. In the prosthesis type subgroup analysis, the recurrence rate was 13% for custom-made prostheses, 1% for modular-made prostheses, 4% for local hemi hip recurrence, and 5% for local recurrence of the total hip (Additional file 2: Appendix Table 5).
Complications
Forty-six complications, such as infections, dislocations, and visceral injuries, were reported in 2069 patients from 24 cohorts. The five main complications reported were infections, dislocations, acetabular wear, deep vein thrombosis, and aseptic loosening.
Sixty-eight patients reported infections, including deep and superficial infections. The overall infection rate was 5% (95% CI: 3–7%, I2 = 61%) (Fig. 5). Additionally, the infection rate was 1, 3, 7, and 12% for follow-up < 2, 2–5, 6–10, and > 10 years, respectively. In the tumor type subgroup analysis, the infection rate was 5% in patients with primary tumors and 2% in those with bone metastases. In the prosthesis type subgroup analysis, the infection rate was 4% for custom-made prostheses, 3% for modular-made prostheses, 3% for hemi hip replacement, and 8% for total hip replacement (Additional file 2: Appendix Table 6).
Furthermore, 63 patients reported dislocations, with an overall rate of 3% (95% CI: 1–5%, I2 = 82%) (Fig. 6). Based on the follow-up time subgroup analysis, the dislocation rate at < 2, 2–5, 6–10, and > 10 years was 0, 4, 6, and 12%, respectively. In the tumor type subgroup analysis, the dislocation rate was 5% in patients with primary tumors and 3% in patients with bone metastases. According to the subgroup analysis of prosthesis type, the dislocation rate was 5% for custom-made prostheses, 3% for modular-made prostheses, 2% for hemi hip replacement, and 4% for total hip replacement (Additional file 2: Appendix Table 7).
Fifty-four patients reported acetabular wear, comprising an overall rate of 0% (95% CI: 0–2%, I2 = 88%) (Additional file 2: Appendix Fig. 2). The acetabular wear rate was 0, 1, 0, and 0% for follow-up < 2, 2–5, 6–10, and > 10 years follow-up, respectively. In the tumor type subgroup analysis, the acetabular wear rate was 0% in patients with primary tumors and 0% in those with bone metastases. In the prosthesis type subgroup analysis, the rate of acetabular wear was 0% for custom-made prostheses, 2% for modular-made prostheses, 4% for hemi hip replacement, and 4% for total hip replacement (Additional file 2: Appendix Table 8).
Thirty patients reported deep venous thrombosis (DVT) with an overall rate of 0% (95% CI: 0–4%, I2 = 90%) (Additional file 2: Appendix Fig. 3). The follow-up time subgroup analysis showed DVT rate at < 2, 2–5, 6–10, and > 10 years of 0, 1, 0, and 0%, respectively. In the tumor type subgroup analysis, the DVT rate was 0% in patients with primary tumors and 0% in those with bone metastases. The prosthesis type subgroup analysis showed a DVT rate of 0% for custom-made prostheses, 2% for modular-made prostheses, 1% for hemi hip replacement, and 0% for total hip replacement (Additional file 2: Appendix Table 9).
Moreover, 28 patients reported aseptic loosening, with an overall rate of 1% (95% CI:0–2%, I2 = 72%), Fig. 7. The follow-up time subgroup analysis showed that the aseptic loosening rate was 0, 4, 6, and 12% for < 2, 2–5, 6–10, and > 10 years, respectively. In the tumor type subgroup analysis, the aseptic loosening rate was 5% in patients with primary tumors and 3% in patients with bone metastases. The prosthesis type subgroup analysis showed that the aseptic loosening rate was 5% for custom-made prostheses, 5% for modular-made prostheses, 2% for hemi hip replacement, and 4% for total hip replacement (Additional file 2: Appendix Table 10).
Sensitivity analysis and publication bias
The funnel plots and Egger regression presented p > 0.05, suggesting no publication bias. The exclusion of each study did not affect outcome indicators, indicating robust results.
Discussion
Herein, patient clinical and prosthetic outcomes were analyzed using data from 24 studies with 2081 patients with joint prosthesis replacement after proximal femoral tumor resection. The overall patient limb preservation rate was 98%. The total prosthesis revision rate was 9% and gradually increased with increasing follow-up time. The survival rates at 1, 2, 3, 4, and 5 years were 80, 72, 65, 64, and 55% for patients with primary tumors and the rate at 1, 2, 3, 4, and 5 years were 44, 25, 17, 14, and 11% for patients with bone metastases, respectively. The rate of infection, dislocation, acetabular wear, DVT, and aseptic loosening were 5, 3, 0, 0, and 1%, respectively.
According to the tumor type classification, patients with primary tumors still had more than a 50% survival rate in the fifth year, and the trend of survival rate decreased more slowly. Meanwhile, more than 50% of patients with bone metastases had already died in the first year, and survival rate decreased by almost half in the second year. This finding was consistent with Houdek et al. [19], where the overall patient survival was associated with the presence or absence of tumor metastasis [hazard ratio (HR) 2.96; 95% CI: 2.11–4.20]. The prosthesis type analysis showed that patients with total hip replacement had a higher survival rate than those with hemi-hip replacement. The total hip replacement studies in this systematic review [30, 32] included mostly patients with primary tumors of the proximal femur or chemotherapy-sensitive proximal femoral malignancies. They have a relatively better prognosis than chemotherapy-insensitive malignant patients with higher requirements for long-term function. The total hip replacement has a better socket-prosthesis head fit, with friction occurring at the prosthesis interface rather than the prosthesis-chondral interface, and has a better long-term postoperative function. The total hip replacement patients in this study used custom prostheses, so the subgroup analysis shown that patients with custom prostheses had a higher survival rate than those with modular-made prostheses. Meanwhile, survival rates for patients with modular tumors were worse may well be because these were used in patients with metastases who were not expected to live so long considering convenience and economy.
Prosthesis survival rates were much higher than patient survival rates at the same follow-up time. This finding suggested that for patients with poor oncologic outcomes, joint prostheses can successfully preserve functional limbs without revision and for long-term survivors for at least 5–10 years. However, implant survival steadily declined over time (mean 20-year implant survival: 39%, 95% CI: 12–66%), while tumor survival declined more slowly and eventually remained stable after 10 years of follow-up. This result is similar to Liang et al. [36] regarding joint reconstruction after resectioning periprosthetic tumors in the knee.
Infection is the main cause of limb salvage failure, with deep infection being a lifelong threat after prosthetic replacement. The subgroup analysis showed a gradual increase in infection rate with increasing follow-up time, but this result should be cautiously interpreted because most studies did not provide the type of infection. The risk factors for periprosthetic infection include prolonged and repeat surgery, malnutrition, and immune compromise during comorbidities such as chemotherapy, radiation therapy, extra-articular resection, poor soft tissue coverage, hematoma formation, and diabetes mellitus [37, 38]. Various methods are available to control deep periprosthetic infections, such as amputation, level 2 revision, level 1 revision, joint replacement, irrigation, debridement, and conservative antibiotic therapy, with level 2 revision the most likely cure for infection in most infected patients [7, 39].
The hemi hip replacement has better stability than the total hip replacement. Hip dislocation was the most common complication of the upper femoral prosthesis. The subgroup analysis showed a gradual increase in dislocation rate with increasing follow-up time and a higher rate of dislocation in total hip replacements than in hemi hip replacements, similar to Thambapillary et al. [9]. Aseptic loosening is also a major complication of prosthetic reconstruction. The subgroup analysis showed a gradual increase in aseptic loosening with increasing follow-up time and a higher rate of total hip replacement aseptic loosening than hemi hip replacement. Thambapillary et al. [9] reported a 5.2% aseptic loosening, higher than the 3% reported here, which might be related to the improved prosthesis design and the choice of fixation method, making recent cases reported no aseptic loosening occurred in any of the follow-up cases [40]. Aseptic loosening is more frequent in pediatric patients than in adults [41]. Thambapillary et al. [9] included pediatric patients, while the present study included only adult patients. The pooled DVT rate was lower than the 8.5% reported by Thambapillary et al. [9]. This might be due to the emphasis on prophylactic management of post-arthroplasty thrombosis and prophylactic management of thrombosis in oncology patients in the last decade, with all study patients undergoing perioperative and postoperative prophylactic use of anticoagulants.
However, this study also has some limitations. First, due to data limitations, it was not possible to analyze the relevant outcome for specific tumor types, different prosthesis brands, resection methods, margin sizes, radiotherapy types, the combination of adjuvant radiotherapy and fixation types, and compare the impact of each factor on the outcome. Second, due to incidence limitations, the number of cases reported so far is small, and more original studies are still needed to expand the sample size of the analysis.
Conclusion
The use of joint reconstruction after proximal femoral tumor resection to improve patients' function and quality of life has been solidified with advances in chemotherapy and radiotherapy. Proximal femoral arthroplasty has benefits in treating primary or metastatic tumors of the proximal femur. The prosthesis tends to outlive the patient, providing them with a relatively pain-free limb with good functional capacity, with limb salvage rates of 98%. Compared to total hip replacement, hemi-hip offers better stability and reduced dislocation and aseptic loosening rates.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Heymann D. Bone Cancer: Primary Bone Cancers and Bone Metastases. 2nd ed. Elsevier; 2014.
Niu XH, Xu HR, Zhang Q. Comprehensive treatment of osteosarcoma. Chin J Bone Joint. 2008;01:36–9.
Finstein J, Welm AL, Stewart SA. Understanding the Bone in Cancer Metastasis. J Bone Miner Res. 2018. https://doi.org/10.1002/jbmr.3618.
Böhm P, Huber J. The surgical treatment of bony metastases of the spine and limbs. J Bone Joint Surg Br. 2002. https://doi.org/10.1302/0301-620x.84b4.12495.
Toma CD, Dominkus M, Nedelcu T, Abdolvahab F, Assadian O, Krepler P, et al. Metastatic bone disease: a 36-year single centre trend-analysis of patients admitted to a tertiary orthopaedic surgical department. J Surg Oncol. 2007. https://doi.org/10.1002/jso.20787.
Guo W. Principles and problems of limb-salvage treatment for malignant bone tumors. Chin J Joint Surg (Electronic Edition). 2007;05:257–61.
Guo W. The development and clinical application of the mega prosthesis. Chin J Bone Joint. 2022;27(03):129–37.
Guo W, Ji T, Yang R, Tang X, Yang Y. Endoprosthetic replacement for primary tumours around the knee: experience from Peking University. J Bone Joint Surg Br. 2008. https://doi.org/10.1302/0301-620X.90B8.20240.
Thambapillary S, Dimitriou R, Makridis KG, Fragkakis EM, Bobak P, Giannoudis PV. Implant Longevity, Complications and Functional Outcome Following Proximal Femoral Arthroplasty for Musculoskeletal Tumors a Systematic Review. J Arthroplasty. 2013. https://doi.org/10.1016/j.arth.2012.10.024.
Brown TS, Salib CG, Rose PS, Sim FH, Lewallen DG, Abdel MP. Reconstruction of the hip after resection of periacetabular oncological lesions: a systematic review. Bone Joint J. 2018. https://doi.org/10.1302/0301-620X.100B1.BJJ-2017-0548.R1.
Man L, Chen WS, Liu YX, Liu YQ, Yuan YD. Meta-analysis of single rates with zero events. Chin J Evid Based Med. 2020;20(10):1226–33.
Atalay IB, Öztürk R, Yapar A, Ulucakoy C, Engin EE, Güngör BS. Are Daily Life Activities of Patients with Proximal Femoral Tumor Resection Prosthesis as Good as those of Patients Undergoing Total Hip Prosthesis for Non-Tumor Causes? Folia Med (Plovdiv). 2020. https://doi.org/10.3897/folmed.62.e47150.
Bernthal NM, Schwartz AJ, Oakes DA, Kabo JM, Eckardt JJ. How long do endoprosthetic reconstructions for proximal femoral tumors last? Clin Orthop Relat Res. 2010. https://doi.org/10.1007/s11999-010-1369-6.
Bischel OE, Suda AJ, Böhm PM, Lehner B, Bitsch RG, Seeger JB. En-bloc resection of metastases of the proximal femur and reconstruction by modular arthroplasty is not only justified in patients with a curative treatment option—an observational study of a consecutive series of 45 patients. J Clin Med. 2020. https://doi.org/10.3390/jcm9030758.
Chandrasekar CR, Grimer RJ, Carter SR, Tillman RM, Abudu A, Buckley L. Modular endoprosthetic replacement for tumours of the proximal femur. J Bone Joint Surg Br. 2009. https://doi.org/10.1302/0301-620X.91B1.20448.
Farid Y, Lin PP, Lewis VO, Yasko AW. Endoprosthetic and allograft-prosthetic composite reconstruction of the proximal femur for bone neoplasms. Clin Orthop Relat Res. 2006. https://doi.org/10.1097/01.blo.0000181491.39048.fe.
Finstein JL, King JJ, Fox EJ, Ogilvie CM, Lackman RD. Bipolar proximal femoral replacement prostheses for musculoskeletal neoplasms. Clin Orthop Relat Res. 2007. https://doi.org/10.1097/BLO.0b013e31804f5474.
Hobusch GM, Bollmann J, Puchner SE, Lang NW, Hofstaetter JG, Funovics PT, et al. What Sport Activity Levels Are Achieved in Patients After Resection and Endoprosthetic Reconstruction for a Proximal Femur Bone Sarcoma? Clin Orthop Relat Res. 2017. https://doi.org/10.1007/s11999-016-4790-7.
Houdek MT, Watts CD, Wyles CC, Rose PS, Taunton MJ, Sim FH. Functional and oncologic outcome of cemented endoprosthesis for malignant proximal femoral tumors. J Surg Oncol. 2016. https://doi.org/10.1002/jso.24339.
Houdek MT, Rose PS, Ferguson PC, Sim FH, Griffin AM, Hevesi M, et al. How Often Do Acetabular Erosions Occur After Bipolar Hip Endoprostheses in Patients With Malignant Tumors and Are Erosions Associated With Outcomes Scores? Clin Orthop Relat Res. 2019. https://doi.org/10.1097/01.blo.0000534684.99833.10.
Jacofsky DJ, Haidukewych GJ, Zhang H, Sim FH. Complications and results of arthroplasty for salvage of failed treatment of malignant pathologic fractures of the hip. Clin Orthop Relat Res. 2004. https://doi.org/10.1097/01.blo.0000143572.96021.93.
Johnson JD, Perry KI, Yuan BJ, Rose PS, Houdek MT. Outcomes of Endoprosthetic Replacement for Salvage of Failed Fixation of Malignant Pathologic Proximal Femur Fractures. J Arthroplasty. 2019. https://doi.org/10.1016/j.arth.2018.12.009.
Liu H, Fang X, Yu Z, Lang Y, Xiong Y, Duan H. Surgical strategy for benign lesions in proximal femur: internal fixation or endoprosthetic replacement. Int Orthop. 2018. https://doi.org/10.1007/s00264-018-3922-y.
Manoso MW, Frassica DA, Lietman ES, Frassica FJ. Proximal femoral replacement for metastatic bone disease. Orthopedics. 2007. https://doi.org/10.3928/01477447-20070501-09.
Meynard P, Seguineau A, Laumonerie P, Fabre T, Foltran D, Niglis L, et al. Surgical management of proximal femoral metastasis: Fixation or hip replacement? A 309 case series. Orthop Traumatol Surg Res. 2020. https://doi.org/10.1016/j.otsr.2020.05.007.
Nakashima H, Katagiri H, Takahashi M, Sugiura H. Survival and ambulatory function after endoprosthetic replacement for metastatic bone tumor of the proximal femur. Nagoya J Med Sci. 2010;72(1–2):13–21.
Nooh A, Alaseem A, Epure LM, Ricard MA, Goulding K, Turcotte RE. Radiographic, Functional, and Oncologic Outcomes of Cemented Modular Proximal Femur Replacement Using the “French Paradox” Technique. J Arthroplasty. 2020. https://doi.org/10.1016/j.arth.2020.04.047.
Peterson JR, Decilveo AP, O’Connor IT, Golub I, Wittig JC. What Are the Functional Results and Complications With Long Stem Hemiarthroplasty in Patients With Metastases to the Proximal Femur? Clin Orthop Relat Res. 2017. https://doi.org/10.1007/s11999-016-4810-7.
Potter BK, Chow VE, Adams SC, Letson GD, Temple HT. Endoprosthetic proximal femur replacement: metastatic versus primary tumors. Surg Oncol. 2009;18(4):343–9.
Sokolovski VA, Voloshin VP, Aliev MD, Zubikov VS, Saravanan SA, Martynenko DV, et al. Total hip replacement for proximal femoral tumours: our midterm results. Int Orthop. 2006. https://doi.org/10.1016/j.suronc.2008.08.007.
Varady NH, Ameen BT, Hayden BL, Yeung CM, Schwab PE, Chen AF. Short-Term Morbidity and Mortality After Hemiarthroplasty and Total Hip Arthroplasty for Pathologic Proximal Femur Fractures. J Arthroplasty. 2019. https://doi.org/10.1016/j.arth.2019.06.019.
Wu YN, Wang DY, Bi WZ, Han G, Jia JP, Xu M. Neoadjuvant chemotherapy, wide resection and custom prosthetic replacement for tumors of the proximal femur. Int J Clin Exp Med. 2016;9(11):20474–83.
Yu ZP, Xiong Y, Shi R, Min L, Zhang WL, Liu HY, et al. Surgical management of metastatic lesions of the proximal femur with pathological fractures using intramedullary nailing or endoprosthetic replacement. Mol Clin Oncol. 2018. https://doi.org/10.3892/mco.2017.1503.
Clarke HD, Damron TA, Sim FH. Head and neck replacement endoprostheses for pathologic proximal femoral lesions. Clin Orthop Relat Res. 1998. https://doi.org/10.1097/00003086-199808000-00024.
Kabukcuoglu Y, Grimer RJ, Tillman RM, Carter SR. Endoprosthetic replacement for primary malignant tumors of the proximal femur. Clin Orthop Relat Res. 1999;358:8–14.
Haijie L, Dasen L, Tao J, Yi Y, Xiaodong T, Wei G. Implant Survival and Complication Profiles of Endoprostheses for Treating Tumor Around the Knee in Adults: A Systematic Review of the Literature Over the Past 30 Years. J Arthroplasty. 2018. https://doi.org/10.1016/j.arth.2017.10.051.
Jeys LM, Grimer RJ, Carter SR, Tillman RM. Periprosthetic infection in patients treated for an orthopaedic oncological condition. J Bone Joint Surg Am. 2005. https://doi.org/10.2106/JBJS.C.01222.
Grimer RJ, Aydin BK, Wafa H, Carter SR, Jeys L, Abudu A, et al. Very long-term outcomes after endoprosthetic replacement for malignant tumours of bone. Bone Joint J. 2016. https://doi.org/10.1302/0301-620X.98B6.37417.
Hardes J, Gebert C, Schwappach A, Ahrens H, Streitburger A, Winkelmann W, et al. Characteristics and outcome of infections associated with tumor endoprostheses. Arch Orthop Trauma Surg. 2006. https://doi.org/10.1007/s00402-005-0009-1.
Ward WG, Johnston KS, Dorey FJ, Eckardt JJ. Extramedullary porous coating to prevent diaphyseal osteolysis and radiolucent lines around proximal tibial replacements. A preliminary report. J Bone Joint Surg Am. 1993; https://doi.org/10.2106/00004623-199307000-00003
Gupta A, Meswania J, Pollock R, Cannon SR, Briggs TW, Taylor S, et al. Non-invasive distal femoral expandable endoprosthesis for limb-salvage surgery in paediatric tumours. J Bone Joint Surg Br. 2006. https://doi.org/10.1302/0301-620X.88B5.17098.
Acknowledgements
No.
Funding
This study is funded by Natural Science Foundation of Gansu Province (grant numbers 21JR7RA615) and Lanzhou Science and Technology Development Guidance Program Project (grant numbers 2020-ZD-19).
Author information
Authors and Affiliations
Contributions
Bo Li: Data curation, Writing Original draft preparation, and Writing- Reviewing. Yongzhi Yu: Validation and Formal analysis. Yun Bao: Software and Data Curation. Jianmin Song: Writing- Reviewing and Editing. These authors contributed equally: Bo Li, Yongzhi Yu. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 2: Appendix Figure 1.
Incidence of hemi to total hip conversion. Appendix Figure 2. Rate of acetabular wear. Appendix Figure 3. Rate of deep vein thrombosis. Appendix Table 1. Patient and prosthesis survival rates. Appendix Table 2. Subgroup analysis of prosthetic revision rate. Appendix Table 3. Subgroup analysis of hemi hip to total hip. Appendix Table 4. Subgroup analysis of Limb salvage rate. Appendix Table 5. Subgroup analysis of local recurrence rate. Appendix Table 6. Infection. Appendix Table 7. Dislocation. Appendix Table 8. Acetabular wear. Appendix Table 9. Deep Vein Thrombosis. Appendix Table 10. Aseptic loosening.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, B., Yu, Y., Bao, Y. et al. Proximal femoral tumor resection followed by joint prosthesis replacement: a systematic review and meta-analysis. BMC Musculoskelet Disord 24, 779 (2023). https://doi.org/10.1186/s12891-023-06913-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06913-w