Abstract
Background
Few reports have examined the localized regional disparity in representative surgical procedures in orthopaedics and general surgery globally. This study aimed to clarify the inter-prefectural regional disparity and relationships between healthcare resources and representative surgical procedures using a nationwide database in Japan.
Methods
The number of medical specialists in orthopaedics, general surgery, and anaesthesiology, as well as the number of hospitals, and the incidence of representative surgical procedures in orthopaedics and general surgery were evaluated annually per 100,000 inhabitants/people by prefecture in Japan during 2015–2019. Medium-sized regional disparities were evaluated using the Gini coefficient. Correlation coefficients were calculated for the defined variables and ageing rate. We also compared the urban and rural regional disparities in all study variables.
Results
The annual average number/incidence and Gini coefficients were 110.6 and 0.11 for femur fracture surgery, 106.3 and 0.09 for cholecystectomy, 14.2 and 0.11 for orthopaedic surgeon specialists, 17.6 and 0.09 for general surgeon specialists, 5.9 and 0.13 for anaesthesiology specialists, and 8.1 and 0.21 for hospitals, respectively. The correlation coefficients by the incidence of femur fracture surgery were 0.74 for orthopaedic surgeon specialists (p < 0.001), 0.63 for hospitals (p < 0.001), and 0.62 for the ageing rate (p < 0.001); those by the incidence of cholecystectomy were 0.60 for general surgeon specialists (p < 0.001) and 0.59 for hospitals (p < 0.001). The number/incidence of orthopaedic surgeon specialists, hospitals, femur fracture surgery, and cholecystectomy, as well as the ageing rate, were significantly higher in rural prefectures than in urban prefectures (p < 0.05).
Conclusions
Inter-prefectural regional disparity was small, although certain items were unevenly distributed in the rural prefectures, which is contrary to our expectations. Higher prevalence was recognised in rural prefectures due to the higher ageing rate; however, supply and demand are balanced. This study provides basic data for healthcare policy development in a medium-sized community.
Level of evidence
III.
Similar content being viewed by others
Background
Japan is an island country in East Asia with a total area of approximately 380,000 km2 and a total population of approximately 125,000,000 (final estimates as of 1 February 2022 Statistics Bureau of Japan [1]), with the majority of individuals being Asian. According to World Bank data from 2021 (https://databank.worldbank.org/), Japan’s economy ranks third in the world by nominal gross domestic product (GDP) but 26th by nominal GDP per capita. The healthcare insurance system [2] is characterised by universal health coverage, allowing citizens to decide which medical facilities to visit, when and where needed, without financial hardship. The index of universal health coverage in Japan is one of the highest in the world [3]. Additionally, physicians can freely choose their departments and specialities. However, as in other countries [4, 5], the maldistribution of physicians to urban rather than rural areas has been an ongoing challenge [6,7,8]. In 2020, a limiting system (setting limits on the number of trainees in a prefecture for each department and allowing them to train in areas with a shortage of physicians) was launched to address the maldistribution.
The rapidly ageing population poses additional challenges to the healthcare system. In 2020, the ageing rate (the ratio of the elderly population aged ≥ 65 years to the total population) in Japan was the highest in the world at 28.7%. However, the ageing rate is expected to increase further by 2040, with a declining birth rate and a society with an ageing rate of 35.3% (https://www.stat.go.jp/data/topics/topi1261.html). As the working population declines, major changes in the quality and quantity of medical care are expected. Therefore, it is essential to understand the medical needs and demands of communities. In particular, surgical treatment is a common medical demand and a powerful tool for medical personnel to treat diseases. However, few reports have examined the localized regional disparity in representative surgical procedures globally.
Representative surgical procedures common within an ageing society in orthopaedics include osteosynthesis (fracture surgery) for acute trauma and arthroplasty (joint replacement) for chronic osteoarthritis. Recently, hip and knee arthroplasties have increased annually in Japan [9], while the occurrence of hip fractures is markedly increasing [10, 11]. Additionally, common general surgeries include cholecystectomy [12] and appendectomy [13]. Although an epidemiological survey of representative surgical procedures in general surgery [14], and some epidemiological studies on these representative surgical procedures have been reported in Japan, few reports have examined localized regional disparities in the world. Moreover, essential data related to the number of medical specialists and the incidence of surgical procedures are sparse worldwide [15] and the relationship between medical specialists, facilities, and representative surgical procedures have not been characterized using a large-scale database.
The National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB) contains most data (> 95%) regarding healthcare insurance claims for medical treatments, as monitored by the Ministry of Health, Labour, and Welfare [16, 17]. In fact, after complete anonymisation, > 1.7 billion records are annually registered in the NDB [17, 18]. Hence, the NDB is useful for evaluating nationwide surgical procedures.
We hypothesised that regional disparities in medical care are small across Japan, and healthcare resources and surgical procedures are correlated and concentrated in urban areas. Using the NDB, this study aimed to investigate the regional disparity and relationships among healthcare resources and representative surgical procedures in each medium-sized region (prefecture) in Japan.
Methods
Ethics statement
This study did not require institutional board approval or informed consent because of the use of legally anonymised public data.
Study design and population
Using the NDB Open Data Japan [19], the annual average number/incidence of medical specialists, facilities, and surgical procedures were surveyed from 2015 to 2019 in 47 prefectures. The incidences of outpatient and inpatient surgeries were summed for each year, whereas the annual nationwide incident subjects of total surgical procedures were calculated over five years. The NDB guidelines stipulate that when the incidence is < 10, the data cannot be reported for anonymisation. Biennial data (2016, 2018) on the number of physicians by prefecture from the Ministry of Internal Affairs and Communications open data [20] were used to determine the number of medical specialists in orthopaedics, general surgery and anaesthesiology. The number/incidence per 100,000 inhabitants/people was calculated based on the demographics of the Ministry of Internal Affairs and Communications [20]. We also evaluated the number of hospitals per 100,000 inhabitants and beds per 1,000 inhabitants, using open data from 2017 [20]. A hospital was defined as a facility that can accommodate ≥ 20 patients. Correlation coefficients were calculated for surgical procedures, medical specialists, hospitals, and beds, by prefecture. From the top 10 highest-volume surgical procedures in orthopaedics in 2020 in Japan [21], we examined the following seven surgical procedures assigned K-codes as per the Japanese coding system for surgical procedures: five fracture surgeries (femur, forearm, lower leg, upper arm [codes K046 1, 2], and femoral head replacement [code K081 1]), and two arthroplasty surgeries (total hip arthroplasty [code K082 1], and total knee arthroplasty [code K082 1]). The remaining three spine surgeries were excluded as neurosurgeons and orthopaedic surgeons performed the surgeries in Japan. According to the Organization for Economic Co-operation and Development (OECD) criteria, hip replacement was calculated as the sum of total hip arthroplasty and femoral head replacement. In general surgery, major surgical procedures were examined as surveyed by the OECD: cholecystectomy (open [code K672]; laparoscopic [code K672-2]) and appendectomy (open [code K718]; laparoscopic [code K718-2]). The ageing rate in each prefecture was calculated from the demographics of the Ministry of Internal Affairs and Communications [20]. The Gini coefficient (0–1; 0: complete equality, 1: complete inequality) was also calculated according to previous reports [6, 22, 23] to examine regional disparity among prefectures. The Gini coefficient is an indicator of the degree of income inequality and other factors that has been widely used in the field of economics and to assess the distribution of physicians in a region. It is categorized as low (< 0.2), moderate (≥ 0.2, < 0.3), high (≥ 0.3, < 0.4), or extreme inequality (≥ 0.4).
Prefectures and urban–rural definition
Japan has three administrative levels: the national government, prefectures, and municipalities. The country is divided into 47 prefectures (Fig. 1), with Hokkaido as the northernmost prefecture and Okinawa as the southernmost prefecture. Prefectures in Japan are medium-sized regions, resembling states in the United States, with only administrative power and not legislative power. There are 15 prefectures that have an ordinance-designated large city with a population > 500,000, including Hokkaido, Miyagi, Saitama, Tokyo, Chiba, Kanagawa, Niigata, Shizuoka, Aichi, Kyoto, Osaka, Hyogo, Okayama, Hiroshima, and Fukuoka. Referring to previous reports [22, 24], we investigated and compared two cases of urban–rural regional differences. (1) We defined the 15 prefectures as the large-city (urban) group and the other 32 as the non-large city (rural) group. (2) The top seven prefectures with a high population density > 1,000 persons per km2 were defined as the densely populated (urban) group and the remaining 40 prefectures as the sparsely populated (rural) group. The top seven most populated prefectures, namely Saitama, Tokyo, Chiba, Kanagawa, Aichi, Osaka, and Fukuoka, are located in the metropolitan areas and account for 45.7% of the total population in Japan.
Statistical analysis
Correlations were assessed using the Pearson correlation method. Data comparisons between urban and rural groups were performed using the unpaired t-test. A two-sided p-value < 0.05 was considered statistically significant. All statistical analyses were performed using EZR (Saitama Medical Centre, Jichi Medical University, Saitama, Japan) [25], a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Table 1 presents the annual nationwide incident subjects, number/incidence per 100,000 inhabitant/person-years and Gini coefficients for healthcare resources and representative surgical procedures during 2015–2019 for 47 prefectures. The Gini coefficients were low (< 0.2) in all, but moderate of 0.21 in the hospitals. Table 2 shows the relationships among representative surgical procedures, healthcare resources and the ageing rate. Femur fracture surgery and total knee arthroplasty were selected as the representative surgical procedures because in the general Japanese population, the femur fracture surgery had the highest incidence among the five types of fracture surgeries, and total knee arthroplasty had the higher incidence among arthroplasty surgery types (Table 1). Table 3 shows the results of the comparison between the two groups for regional differences in urban and rural prefectures. Supplementary Tables 1–7 show the individual data for each prefecture.
The national average ageing rate was 0.295, with the Akita Prefecture having the highest rate of 0.356 and Okinawa Prefecture having the lowest rate of 0.210.
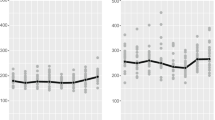
Meanwhile, correlation diagrams are shown in Figs. 2, 3, 4, 5, 6 and 7. The correlation coefficients by the incidence of femur fracture surgery were 0.74 for orthopaedic surgeon specialists (p < 0.001) (Fig. 2), 0.63 for hospitals (p < 0.001) (Fig. 3), and 0.62 for the ageing rate (p < 0.001) (Fig. 4); those by the incidence of total knee arthroplasty was 0.64 for orthopaedic surgeon specialists (p < 0.001) (Fig. 5). The correlation coefficients by the incidence of cholecystectomy were 0.60 for general surgeon specialists (p < 0.001) (Fig. 6), 0.59 for hospitals (p < 0.001), and 0.32 for the ageing rate. The correlation coefficient between general surgeon specialists and anaesthesiology specialists was 0.74 (p < 0.001) (Fig. 7).
The regional differences between urban and rural areas were as follows. (1) The number/incidence of femur fracture surgery, lower leg fracture surgery, total knee arthroplasty, cholecystectomy, and hospitals, as well as the ageing rate, were significantly higher in the non-large city than in the large city. (2) The number/incidence of femur fracture surgery, lower leg fracture surgery, total knee arthroplasty, cholecystectomy, orthopaedic surgeon specialists, hospitals and the ageing rate were significantly higher in the sparsely populated area than in the densely populated area.
Discussion
Using a nationwide database in Japan, we clarified regional disparities and relationships between healthcare resources and representative surgical procedures in orthopaedics and general surgery across 47 prefectures. Three factors (medical specialists, facilities, and representative surgical procedures) were found to correlate with each other. The inter-prefectural regional disparity was small, although certain items were unevenly distributed in the rural prefectures, which is contrary to our expectations.
The Gini coefficient indicated inequality and showed similar trends. The Gini coefficient was approximately 0.1 for all three medical specialists (Table 1), indicating that the regional disparity was small and homogeneous healthcare was provided at the prefectural level. Hence, the universal health insurance system in Japan [3] was effective at the prefectural level. Among the three types of specialists, the general surgeon specialists had the smallest Gini coefficient, followed by the orthopaedic surgeon specialists and anaesthesiology specialist, which increased slightly. This difference may result from the effect of the parameter size. Meaningful maldistribution of physicians was not confirmed at the prefectural level, although it has been reported at the municipal level previously [6]. It has also been reported that the inter-prefectural disparity in the incidence of paediatricians was smaller than the inter-municipal (intra-prefectural) disparity [22], which should be interpreted with caution. However, there have been no reports of regional disparities in the incidence of surgical procedures using the Gini coefficient. Among surgical procedures in orthopaedics, the Gini coefficient was the lowest (0.09) for lower limb fracture surgery. When comparing representative surgical procedures between orthopaedics and general surgery, those in general surgery had slightly lower Gini coefficients (0.08 and 0.09, respectively). This reflects the necessity or urgency of the lower limb fracture surgery and the two general surgeries (cholecystectomy and appendectomy). The Gini coefficient of medical facilities was higher for hospitals than for beds. This was also considered to be due to the effect of the parameter size. Regardless, all Gini coefficients were approximately 0.1–0.2 (Table 1), indicating that the regional differences were small at the prefectural level.
Correlation analysis revealed strong to moderate positive correlations between the number/incidence of certain surgical procedures, orthopaedic surgeon specialists, general surgeon specialists, and hospitals (Table 2, Figs. 2, 3, 4, 5, 6 and 7). The incidences of femur fracture surgery and total knee arthroplasty showed strong to moderate positive correlations with the ageing rate, orthopaedic surgeon specialists, and hospitals, while the cholecystectomy incidence exhibited a moderate positive correlation with general surgeon specialists and hospitals. The appendectomy incidence showed a moderate positive correlation with general surgeon specialists and a moderate negative correlation with the ageing rate. This may reflect surgical characteristics such as urgency, necessity, and the age structure of the disease (Supplementary Figures 1, 2, 4, and 5). Additionally, medical specialists and facilities correlated with each other, reflecting a symbiotic relationship. The incidence of surgical procedures is determined by patient demand and medical/healthcare supply. On the patient side, the demand for surgery may be influenced by disease prevalence, the nature of the disease (urgency), the patient’s knowledge of the disease (literacy), and their willingness to undergo surgery. Meanwhile, the supply on the medical side may depend on the number of physicians and facilities and the quality of both (surgeon’s criteria for surgery and ability to diagnose and perform surgery). Accordingly, in this study, we found that the number/incidence of medical specialists, facilities, and surgical procedures were correlated, as expected.
However, unexpectedly, the number/incidence of certain surgical procedures in orthopaedics and general surgery, orthopaedic surgeon specialists (only in sparsely populated areas), and the ageing rate were all higher in rural prefectures than in urban prefectures (Table 3). Investigating the age-stratified data in 2019 for femur fracture surgery, total knee arthroplasty, lower leg fracture surgery, and cholecystectomy revealed that a peak was centred on the elderly in all cases (Supplementary Figures 1–4). However, the distributions differ significantly, suggesting that the population ageing affected other parameters. Although it was biased toward rural prefectures, we considered that the supply–demand balance was maintained among the three parties (medical specialists, facilities, and surgical procedures).
Few studies have examined localized regional disparities in healthcare using the incidence of surgical procedures. A Swedish study [26] of orthopaedic foot surgery speculated that the concentration of specialists increased the incidence of surgery in urban areas. Evidently, the data documented in Japan provided a different spectrum in which the incidence in urban prefectures was slightly lower than that in rural prefectures. However, it is difficult to make simple direct comparisons due to differences in the definitions of urban–rural, race, culture, social structure, and other factors across countries.
Collectively, the present study’s results indicate that, at the prefectural level in Japan, the supply–demand balance in medical specialists, facilities, and representative surgeries has been maintained and that there is little disparity among medium-sized regions. Sufficient healthcare is guaranteed in rural areas, even with the growing ageing population. The Japanese medical system for typical surgical treatments in orthopaedics and general surgery was successful from 2015 to 2019. Accordingly, the results of this study provide important insights to inform healthcare policy planning. Additional validation is needed to follow the longitudinal data in the future.
The OECD [27] publishes annual data on representative surgical procedures, including total knee arthroplasty, hip replacement, appendectomy, and cholecystectomy. Accordingly, we compared the surgical incidence per 100,000 people reported in OECD countries in North America, Europe, and East Asia between 2015 and 2019 with our results (Table 4). In Japan, the incidence of the four surgeries was lower than in other countries, except for hip replacement in South Korea. However, these data cannot be directly compared due to differences in race, ethnicity, and social systems, including healthcare, as well as subtle differences in surgical codes indicating the slightly different definitions of surgeries. Nevertheless, this study of regional epidemiology is intended to provide important information for international medical societies.
This study has several limitations. (1) The study did not focus on disease prevalence but on surgical procedures. (2) The number of medical specialists was surveyed using a biennial questionnaire. However, the estimated registry rate was reported to be 87–90% [28]. (3) The survey on the number of medical facilities was conducted every three years, and the results for only 2017 were used. (4) As aforementioned, the survey methods of surgical procedures are not standardised and may differ slightly from country to country; this issue has also been previously reported [15].
In conclusion, this is the first observational epidemiological study on regional disparities and relationships between healthcare resources and representative surgical procedures in orthopaedics and general surgery. Inter-prefectural regional disparity was small, although certain items were unevenly distributed in the rural prefectures. Higher prevalence was recognised in rural prefectures than urban prefectures due to the higher ageing rate; however, supply and demand were relatively balanced. This study provides basic data for healthcare policy development in a medium-sized community.
Availability of data and materials
The datasets used during the current study are available from the following public domain resources: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177182.html
References
Statistics Bureau of Japan. https://www.stat.go.jp/english/data/jinsui/tsuki/index.html [Accessed 3 Nov 2022].
Ministry of Health, Labour, and Welfare. https://www.mhlw.go.jp/bunya/iryouhoken/iryouhoken01/dl/01_eng.pdf [Accessed 3 Nov 2022].
GBD 2019 Universal Health Coverage Collaborators. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396:1250–84.
Makaroff LA, Green LA, Petterson SM, Bazemore AW. Trends in physician supply and population growth. Am Fam Physician. 2013;87(7):Online.
Ono T, Schoenstein M, Buchan J. Geographic imbalances in doctor supply and policy responses. OECD Health Working Paper No. 69. Paris: OECD Publishing, 2014.
Matsumoto M, Inoue K, Bowman R, et al. Self-employment, specialty choice, and geographical distribution of physicians in Japan: A comparison with the United States. Health Policy. 2010;96:239–44.
Ishikawa M. Changes in the characteristics of rehabilitation physicians over two decades: analysis of national physician census surveys in Japan. Prog Rehabil Med. 2020;17(5):20200012.
Ishikawa M. Distribution and Retention Trends of Obstetricians and Gynecologists in Japan: A Longitudinal Study. JMA J. 2021;15(4):262–9.
Katano H, Ozeki N, Kohno Y, et al. Trends in arthroplasty in Japan by a complete survey, 2014–2017. J Orthop Sci. 2021;26:812–22.
Hagino H, Endo N, Harada A, et al. Survey of hip fractures in Japan: Recent trends in prevalence and treatment. J Orthop Sci. 2017;22(5):909–14.
Takusari E, Sakata K, Hashimoto T, et al. Trends in hip fracture incidence in japan: estimates based on nationwide hip fracture surveys from 1992 to 2017. JBMR Plus. 2020;5(2):e10428.
Rosenmuller M, Haapamaki MM, Nordin P, et al. Cholecystectomy in Sweden 2000–2003: a nationwide study on procedures, patient characteristics, and mortality. BMC Gastroenterol. 2007;17(7):35. https://doi.org/10.1186/1471-230X-7-35.
Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(1):27. https://doi.org/10.1186/s13017-020-00306-3.
Marubashi S, Takahashi A, Kakeji Y, et al. Surgical outcomes in gastroenterological surgery in Japan: Report of the National Clinical Database 2011–2019. Ann Gastroenterol Surg. 2021;5(5):639–58. https://doi.org/10.1002/ags3.12462. eCollection 2021 Sep.
Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569–624.
Sugihara T, Yasunaga H, Matsui H, Kamei J, Fujimura T, Kume H. Regional clinical practice variation in urology: usage example of the Open Data of the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Int J Urol. 2019;26:303–5.
Kato G. History of the secondary use of National Database of Health Insurance Claims and Specific Health Checkups of Japan (NDB). Trans Jpn Soc Med Biol Eng. 2017;55:143–50.
Matsuda S, Fujimori K. The claim database in Japan. Asian Pac J Dis Manag. 2014;6:55–9.
Ministry of Health, Labour and Welfare. NDB Open Data, https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000177182.html [Accessed 3 Nov 2022].
Portal Site of Official Statistics of Japan (e-Stat). https://www.e-stat.go.jp/en/stat-search/ [Accessed 3 Nov 2022].
Annual Report 2020. Japanese Orthopaedic Association National Registry (JOANR). (https://www.joanr.org)
Sakai R, Wang W, Yamaguchi N, et al. The impact of Japan’s 2004 postgraduate training program on intra-prefectural distribution of pediatricians in Japan. PLoS One. 2013;8(10):e77045.
Maeda M, Fukuda H, Matsuo R, et al. Regional disparity of reperfusion therapy for acute ischemic stroke in japan: a retrospective analysis of nationwide claims data from 2010 to 2015. J Am Heart Assoc. 2021;10(20):e021853.
Kido A, Miyake M, Tamura H, et al. Incidence of central serous chorioretinopathy (2011–2018): a nationwide population-based cohort study of Japan. Br J Ophthalmol. 2021:bjophthalmol-2021–319403.
Kanda Y. Investigation of the freely-available easy-to-use software “EZR” (Easy R) for medical statistics. Bone Marrow Transplant. 2013;48:452–8. https://doi.org/10.1038/bmt.2012.244. advance online publication 3 December 2012.
Saro C, Bengtsson AS, Lindgren U, et al. Surgical treatment of hallux valgus and forefoot deformities in Sweden: a population-based study. Foot Ankle Int. 2008;29:298–304.
Organisation for Economic Co-operation and Development (OECD.Stat) https://stats.oecd.org/Index.aspx?DatasetCode=HEALTH_STAT [Accessed 3 Nov 2022].
Shimada N, Kondo T. Estimated registry rate using individual data of survey of physicians, dentists, and pharmacologists. Japanese Journal of Public Health. 2004;51:117–32 (In Japanese).
Acknowledgements
We would like to thank De-Qi Yuan for proofreading and Editage (www.editage.com) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
KI, MK, KT, and RU designed the study. MK, YK, and MM contributed substantially to write the main manuscript. KS and DI supervised the manuscript regarding the general surgery. SO prepared all figures. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Figure 1.
Age-stratified incidence of femur fracture surgery in 2019. Supplementary Figure 2. Age-stratified incidence of knee arthroplasty in 2019. Supplementary Figure 3. Age-stratified incidence of lower leg fracture surgery in 2019. Supplementary Figure 4. Age-stratified incidence of cholecystectomy in 2019. Supplementary Figure 5. Age-stratified incidence of appendectomy in 2019. Supplementary Table 1. Prefectural incidence of femur fracture surgery during 2015–2019 (per 100,000 people). Supplementary Table 2. Prefectural incidence of knee arthroplasty during 2015–2019 (per 100,000 people). Supplementary Table 3. Prefectural incidence of cholecystectomy during 2015–2019 (per 100,000 people). Supplementary Table 4. Prefectural incidence of appendectomy during 2015–2019 (per 100,000 people). Supplementary Table 5. Prefectural number of medical specialists in orthopaedics, general surgery, and anaesthesiology during 2015–2019 (per 100,000 inhabitants). Supplementary Table 6. Prefectural number of medical facilities (hospitals and beds) during 2015–2019 (per 100,000 inhabitants for hospitals and per 1,000 inhabitants for beds). Supplementary Table 7. Prefectural index of the ageing rate during 2015–2019
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kido, M., Ikoma, K., Kobayashi, Y. et al. The inter-prefectural regional disparity of healthcare resources and representative surgical procedures in orthopaedics and general surgery: a nationwide study in Japan during 2015–2019. BMC Musculoskelet Disord 24, 726 (2023). https://doi.org/10.1186/s12891-023-06820-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06820-0