Abstract
Background
Distal radius fractures are common fractures in older adults and associated with increased risk of future functional decline and hip fracture. Whether lower limb muscle strength and balance are impaired in this patient population is uncertain. To help inform rehabilitation requirements, this systematic review aimed to compare lower limb muscle strength and balance between older adults with a distal radius fracture with matched controls, and to synthesise lower limb muscle strength and balance outcomes in older adults with a distal radius fracture.
Methods
We searched Embase, MEDLINE, and CINAHL (1990 to 25 May 2022) for randomised and non-randomised controlled clinical trials and observational studies that measured lower limb muscle strength and/or balance using instrumented measurements or validated tests, in adults aged ≥ 50 years enrolled within one year after distal radius fracture. We appraised included observational studies using a modified Newcastle-Ottawa Scale and included randomised controlled trials using the Cochrane risk-of-bias tool. Due to the clinical and methodological heterogeneity in included studies, we synthesised results narratively in tables and text.
Results
Nineteen studies (10 case-control studies, five case series, and four randomised controlled trials) of variable methodological quality and including 1835 participants (96% women, mean age 55–73 years, median sample size 82) were included. Twelve included studies (63%) assessed strength using 10 different methods with knee extension strength most commonly assessed (6/12 (50%) studies). Five included case-control studies (50%) assessed lower limb strength. Cases demonstrated impaired strength during functional tests (two studies), but knee extension strength assessment findings were conflicting (three studies). Eighteen included studies (95%) assessed balance using 14 different methods. Single leg balance was most commonly assessed (6/18 (33%) studies). All case-control studies assessed balance with inconsistent findings.
Conclusion
Compared to controls, there is some evidence that older adults with a distal radius fracture have impaired lower limb muscle strength and balance. A cautious interpretation is required due to inconsistent findings across studies and/or outcome measures. Heterogeneity in control participants’ characteristics, study design, study quality, and assessment methods limited synthesis of results. Robust case-control and/or prospective observational studies are needed.
Registration
International prospective register of systematic reviews (date of registration: 02 July 2020, registration identifier: CRD42020196274).
Similar content being viewed by others
Introduction
Distal radius fractures are common, representing 18% of all fractures [1]. The economic burden of this injury is significant. In 2017, upper limb fractures incurred 33% of healthcare costs for fragility fractures in six European countries, around £1.7 billion [2]. After 50 years of age, women are nearly five times more likely than men to fracture their distal radius [3]. After this injury, postmenopausal women have a 48% increase in the odds of functional decline [4] and an approximately two-fold increase in three-year future hip fracture risk [5]. Given the high incidence of distal radius fractures, there are important implications for the healthcare system and wider society.
Most distal radius fractures in older adults occur following a fall from standing height onto an outstretched hand [6]. Clinical guidelines recommend that older adults attending healthcare services for a fall-related injury should undergo a falls-risk assessment which may include an assessment of balance and muscle strength [7]. If people are identified as being at increased risk of falls, muscle strengthening and balance exercises are recommended as part of an individualised multifactorial intervention [7]. This approach is supported by a systematic review which found high-certainty evidence that balance and functional exercises alone, or in addition to muscle strengthening exercises, reduce falls in community-dwelling older adults [8]. Previous literature has also recommended rehabilitation for older adults after distal radius fracture to reduce the risk of future fractures, falls, and functional decline [4, 6]. Despite this, interventions in trials evaluating rehabilitation for people with a distal radius fracture have focused on upper limb impairments, with limited prescription of balance and lower limb muscle strengthening exercises [9, 10].
However, older adults with a distal radius fracture are typically high functioning pre-injury [4] and younger than other fragility fracture populations [11]. Whether lower limb muscle strength and balance are impaired in this patient population compared to age- and sex/gender-matched controls is uncertain and to our knowledge has not been evaluated in a systematic review. To help inform whether rehabilitation targeting these modifiable variables is required, this systematic review aimed to: (1) compare lower limb muscle strength and balance between adults aged ≥ 50 years with a distal radius fracture and age- and sex/gender-matched controls, and (2) synthesise lower limb muscle strength and balance outcomes in adults aged ≥ 50 years with a distal radius fracture.
Methods
The systematic review protocol was prospectively registered on the international prospective register of systematic reviews (PROSPERO, registration identifier: CRD42020196274). This report was written following preferred reporting items for systematic review and meta-analyses (PRISMA) guidelines [12].
Search strategy
We searched Embase, MEDLINE, and CINAHL electronic databases on 18 June 2020, and updated this search on 25 May 2022. Search results were limited to studies published since 1990 so that included participants were more reflective of the current older adult population. No other search limitations were applied. The full search strategy for each database is presented in Additional file 1. To identify additional potentially eligible studies, we searched the reference lists of included studies and relevant systematic reviews.
Eligibility criteria
We included randomised and non-randomised controlled clinical trials, and observational studies except single-patient case reports. Published reports, including abstracts, were eligible. Participants had to be women or men aged ≥ 50 years (or ≥ 90% of the sample was comprised of participants aged ≥ 50 years) enrolled within one year after a distal radius fracture treated surgically or non-surgically. Participants had to be aged ≥ 50 years because this is the most commonly affected age group [3]. Enrolment within one year after fracture aimed to limit the influence of advancing age and/or other disease processes on lower limb muscle strength and balance outcomes. Lower limb muscle strength or balance had to be assessed using instrumented measurements or validated physical performance tests. Only English, or non-English language studies adequately translated with Google Translate, were eligible. There was no limitation on study setting or follow-up duration.
During full-text screening, it became apparent that some studies included participants aged < 50 years, but participants’ mean age minus two standard deviations indicated ≥ 90% were aged ≥ 50 years [13,14,15,16]. Several studies did not specify if participants were enrolled within one year after distal radius fracture, instead they reported participants’ duration after distal radius fracture as a range, for example 6–24 months [16,17,18,19,20]. One study included a mixture of participants enrolled within, and more than, one year after distal radius fracture [21]. In all these instances we elected to be inclusive. Further details on these studies and reasons for inclusion are available in Additional file 2.
Study selection
After duplicate removal, two reviewers (PJAN, CV, CF, or DJK) independently screened study titles and abstracts (where available) for eligibility. One reviewer (DJK) resolved any disagreements. Full texts of potentially eligible studies were then independently screened for eligibility by two reviewers (PJAN, DJK, or CF) who discussed any disagreements until consensus was reached.
Data extraction
The following data was independently extracted by one reviewer (WS, CV, JCHP, or CF) and checked by another (PJAN, CF, CV): report characteristics (authors and publication year); study characteristics (design, location, eligibility criteria, intervention details, follow-up timepoints); participants’ characteristics (age, sex/gender, injury characteristics, duration from distal radius fracture, falls history); number of participants enrolled and that underwent lower limb muscle strength and/or balance assessment; and lower limb muscle strength and/or balance assessment method and results. Mistakes in extracted data were corrected by the second reviewer when an extraction error was clear. A third reviewer was consulted if there were uncertainties. We did not attempt to obtain missing data from the authors of included studies.
To identify multiple reports of the same study we compared the locations, authors’ names, participants’ characteristics, and duration of reports. We considered all reports of studies and combined data from multiple reports, where possible.
Quality assessments
Quality assessments were completed at the outcome level (lower limb muscle strength and/or balance). Case-control studies and case series were assessed using a modified Newcastle-Ottawa Scale [22]. We modified the scale by removing the question ‘same method of ascertainment for cases and controls’ for case-control studies as this question does not apply to this review. For case series, we removed the questions on selection of the non-exposed cohort and comparability of cohorts, as these do not apply to case series. Therefore, case-control studies could score a maximum of eight stars and case series a maximum of five stars. For this review, we defined a case series as a single-group study that only included participants with a distal radius fracture. Randomised controlled trials (RCTs) were assessed using the Cochrane risk-of-bias tool [23] under the following domains: ‘selection bias’, ‘performance bias’, ‘detection bias’, ‘attrition bias’, ‘reporting bias’, and ‘other bias’.
Two reviewers (CF, PJAN, or DJK) independently appraised included studies. One reviewer (DJK) resolved disagreements. We did not make an overall risk-of-bias judgement across all included studies because different appraisal tools were used and included studies varied in design.
Analysis
There was high clinical and methodological heterogeneity between included studies, so we did not complete a meta-analysis. Instead, we synthesised results narratively in tables and text.
We planned to group outcomes into short-term (≤ 4 months after fracture), medium-term (> 4–8 months after fracture) and long-term (> 8 months after fracture). However, the duration from distal radius fracture to strength and/or balance assessment was often not reported or unclear, so this was not completed.
To aid comparison of results between studies, we converted outcome data reported in pounds into kilograms (by multiplying pounds by 0.453592), and inches into centimetres (by multiplying inches by 2.54).
Changes from protocol
We did not plan to compare lower limb muscle strength and balance between adults aged ≥ 50 years with a distal radius fracture with age- and sex/gender-matched controls, but due to the high number of included case-control studies and the potential clinical relevance of this comparison, this was completed.
Impaired lower limb muscle strength and balance are associated with increased falls risk in older adults [24, 25]. Therefore, we extracted participants’ falls history, though this was not pre-planned, to better assess the characteristics of participants in included studies.
We planned to include walking and gait assessments within the balance outcomes category, however it was deemed during study selection that a narrower focus on balance-specific measures was indicated due to the considerable heterogeneity in outcome assessment methods.
To facilitate comparison of results across studies, we analysed results by lower limb muscle strength and balance assessment method. This was not pre-planned. No other subgroup or sensitivity analyses were planned or conducted.
Results
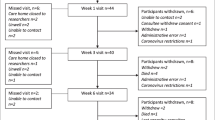
The search strategy identified 3053 records. After duplicate removal, 2841 titles and abstracts were screened for eligibility. Thirty-six full-text reports underwent eligibility assessment. Twenty-six reports of 19 studies were subsequently included in the review. The systematic review search and screening process is shown in Fig. 1.
Study characteristics
Of the 19 included studies, 10 (53%) were case-control studies, five (26%) were case series, and four (21%) were RCTs. Included studies were conducted in 11 different countries (Canada (four studies); Sweden and Japan (three studies); USA (two studies); China, Iceland, Iran, Ireland, Norway, South Korea, and UK (one study)). Fourteen (74%) studies were published since 2012. In total, studies included 1301 participants with a distal radius fracture (1835 participants including controls without a distal radius fracture). Almost all participants with a distal radius fracture were women (n = 1153/1211 (95%), data available in 18 studies). Twelve (63%) studies included women only. Participants’ mean age ranged from 55 to 73 years and the median sample size was 82 (interquartile range 66 to 103). Detailed characteristics of included studies are presented in Table 1. Additional file 3 describes the instrumented balance assessment procedures and scoring methods because these assessments are not commonly used in clinical settings.
Lower limb muscle strength assessments in included studies
Lower limb muscle strength was assessed in 12/19 (63%) studies using 10 different methods. Knee extensor strength was most commonly assessed (6/12 (50%) studies) followed by the five times sit-to-stand test (3/12 (25%) studies) and the 30 s sit-to-stand test (3/12 (25%) studies). More broadly, assessments could be categorised into those that assessed strength during an isolated joint movement (used in 6/12 (50%) studies; hip flexion, hip extension, hip abduction, knee extension, knee flexion, ankle dorsiflexion, and ankle plantarflexion) or during a functional movement (used in 7/12 (58%) studies; five times sit-to-stand test, 30 s sit-to-stand test, leg extension power). Reported durations from distal radius fracture to lower limb muscle strength assessment ranged from 1 to 2 weeks to 24 months.
Balance assessments in included studies
Balance was assessed in 18/19 (95%) studies using 14 different methods. Single leg balance was most commonly assessed (6/18 (33%) studies), followed by postural sway (3/18 (17%) studies) and the functional reach test (3/18 (17%) studies). Five out of 14 (36%) balance assessment methods require specialist equipment not routinely available in clinical settings (used in 8/18 studies (41%): postural sway, Sensory Organisation Test, dynamic postural stability, Modified Clinical Test of Sensory Integration of Balance, balance on Biodex Balance System). Reported durations from distal radius fracture to balance assessment ranged from 1 to 2 weeks to 24 months.
Quality assessment
Full methodological quality assessments of included studies are presented in Additional file 4. Two of 10 (20%) case-control studies [26, 27] scored the maximum of eight stars on the modified Newcastle-Ottawa scale, two studies (20%) [14, 28] scored seven stars, three studies (30%) [19,20,21] scored six stars, and one study (10%) scored five stars [16], four stars [17] and three stars [18]. Seven case-control studies lost a star for ‘representativeness of cases’ [14, 16,17,18,19,20,21]. Two of the five (40%) case series [29, 30] scored the maximum five stars on the modified Newcastle-Ottawa scale, two case series (40%) [15, 31] scored four stars, and one (20%) [32] scored three stars. Two of the four (50%) RCTs [33, 34] were judged at high risk of bias in ≥ 2 domains of the Cochrane risk-of-bias tool.
Lower limb muscle strength results
In adults aged ≥ 50 years with a distal radius fracture compared to age- and sex/gender-matched controls
Five included case-control studies compared lower limb muscle strength between adults aged ≥ 50 years with a distal radius fracture with age- and sex/gender-matched controls [17, 18, 21, 26, 28]. Detailed results are presented in Table 2.
Control participants had no recent falls in two case-control studies that assessed lower limb muscle strength [26, 28]. Cho et al., [26] found women six months after distal radius fracture performed worse on the five times sit-to-stand test than age- and gender-matched controls with a unilateral upper-limb condition (cases: mean 11.2 (Standard Deviation (SD) 1.9) seconds, controls: 10.4 (1.5) seconds; p = 0.018). O’Reilly et al., [28] found older adults 12 months after distal radius fracture had worse knee flexion strength than healthy age- and gender-matched controls (right leg cases: 3.81 (1.52), controls: 4.78 (1.6), p = 0.01; left leg cases: 3.84 (1.62), controls: 4.86 (1.62), p = 0.02), but there was no difference in knee extension or ankle dorsiflexion strength between groups.
In Edwards et al., there was no difference in knee extension strength of the dominant leg between women 6–24 months after distal radius fracture [18] and age- and gender matched controls who both averaged one fall in the previous 12 months.
Participants’ falls history was not reported in two case-control studies that assessed lower limb muscle strength [17, 21]. Crockett et al., [17] found women 6–24 months after distal radius fracture performed worse on the 30 s sit-to-stand test than age-matched women with no distal radius fracture (mean difference: -2.8 (95% confidence interval (CI) -4.6 to -1) repetitions, p = 0.003), and Hakestad et al., [21] found post-menopausal osteopenic women mean 1.3 (SD 0.6) years after distal radius fracture had worse knee extensor peak torque in the left leg (mean difference − 18.6 (95% CI -34.6 to -2.6) Newton metre (Nm), p = 0.025) and worse total work in both legs (mean difference right leg: -259.9 (95% CI -464.9 to -54.9) joules, p = 0.016; left leg: -285.6 (95% CI -492.7 to -78.5), p = 0.01) compared to healthy age-matched women.
In adults aged ≥ 50 years with a distal radius fracture in all included studies
Detailed results from the 12 included studies that assessed lower limb muscle strength are presented in Table 3. Studies are listed in order of shortest duration after distal radius fracture to lower limb muscle strength assessment.
Five studies evaluated lower limb muscle strength at multiple time points [13, 29, 30, 33, 34], with four studies [29, 30, 33, 34] reporting strength progressively improved from initial assessment after distal radius fracture to extended follow-up.
Additional file 5 presents lower limb muscle strength outcomes by assessment method. Methods of assessing and reporting knee extension and flexion strength were highly variable limiting comparisons between studies. In participants with a distal radius fracture, mean five times sit-to-stand performance ranged from 9.3 to 11.7 s and mean 30 s sit-to-stand performance ranged from 11.9 to 15.1 repetitions.
Balance results
In adults aged ≥ 50 years with a distal radius fracture compared to age- and sex/gender-matched controls
Ten included case-control studies compared balance between adults aged ≥ 50 years with a distal radius fracture with age- and sex/gender-matched controls. Detailed results are presented in Table 4.
Cases had no recent falls in three case-control studies that assessed balance [16, 26, 28]. Cho et al., [26] found no difference in performance of the balance component of the short physical performance battery between women six months after distal radius fracture and age- and gender-matched controls with a unilateral upper-limb condition. Sharabiani et al., [16] found older adults 6–24 months after distal radius fracture had more postural sway than age- and sex-matched controls, but only when standing on foam (mean difference: 0.59 (95% CI 0.44 to 0.73) centimetres per second, p < 0.001). O’Reilly et al., [28] found older adults 12 months after distal radius fracture performed worse on the Modified Clinical Test of Sensory Integration of Balance than healthy age- and gender-matched controls (cases: 316.2 (63.32), controls 353.73 (17.72), p = 0.001).
Cases and control participants had recent falls in two studies that assessed balance [18, 19]. In Edwards et al., [18] there was no statistically significant difference in Berg Balance Scale performance between women 6–24 months after distal radius fracture and age- and gender-matched controls. In contrast, Louer et al., [19] found people 6–24 months after distal radius fracture performed worse on the PROPRIO 5000 than age- and sex-matched people with no distal radius fracture (dynamic motion analysis score cases: 933 (172), controls: 790 (75), p = 0.008; duration cases: 50.1 (17.4) seconds, controls: 63.8 (15.9), p = < 0.01).
Participants’ falls history was not reported in five case-control studies that assessed balance [14, 17, 20, 21, 27]. Hakestad et al., [21] found postmenopausal osteopenic women mean 1.3 (SD 0.6) years after distal radius fracture performed worse on the four-square step test than healthy age-matched women (mean difference: 2.4 (95% CI 1 to 3.7), p = 0.002). Crockett et al., [17] found post-menopausal women 6–24 months after distal radius fracture had worse Berg Balance Scale scores than age- and gender matched controls (cases: 53.9 (5.9), controls: 55.4 (1.2), p = 0.046), and also reported worse functional reach test and backwards tandem walk performance in cases, but no statistical comparison between groups for these tests were reported. Similarly, Sakai et al., [27] reported worse single leg balance performance in women six months after distal radius fracture surgery compared to age- and gender-matched controls, but no statistical comparison of results between groups was reported. In Ringsberg et al., [20] and Fujita et al., [14], only some subgroups of women with distal radius fractures performed worse than age-matched women with no distal radius fracture on the functional reach test and single leg balance test, respectively.
Balance in adults aged ≥ 50 years with a distal radius fracture in all included studies
Detailed results from the 18 included studies that assessed balance are presented in Table 5. Seven included studies evaluated balance at multiple timepoints [13, 14, 30, 31, 33,34,35]. Where reported, balance performance in people with a distal radius fracture progressively improved from initial assessment to follow-up in three studies [14, 31, 33], balance performance improved on some assessments and regressed on others in two RCTs [13, 34], and in Crockett et al.,[30] functional reach test and single leg stand performance initially improved from 3 weeks after distal radius fracture until 12 weeks and 26 weeks respectively, but improvements were not maintained at 52 weeks [35].
Additional file 6 presents balance outcomes by assessment method. Methods of assessing and reporting results for single leg balance, postural sway, and the Biodex Balance System were highly variable limiting comparisons of results for these tests between studies. In participants with a distal radius fracture, mean functional reach test performance ranged from 26.6 to 37.2 cm and mean Berg Balance Scale score ranged from 51.8 to 53.9.
Discussion
We found evidence that older adults with a distal radius fracture demonstrate impaired lower limb muscle strength and balance compared to age- and sex/gender-matched controls, but findings were inconsistent across studies and/or outcome measures. Included studies varied highly in terms of study design, quality, lower limb muscle strength and balance assessment methods used, and reporting of results. The characteristics of control participants in case-control studies also varied. This heterogeneity limited synthesis of results and requires careful consideration when interpreting the current evidence for lower limb muscle strength and balance impairments in adults aged ≥ 50 years with a distal radius fracture.
In this review, included case-control studies were cross-sectional. This differs from the classic case-control design which compares previous exposures between cases and controls to determine the association between previous exposures and a condition of interest [36]. In the classic design, recommendations to reduce bias include selecting controls independent of the exposure being investigated so that control participants do not have an abnormally high or low exposure [36]. In the cross-sectional case-control studies in this review, control participants should instead be independent of the outcomes of interest, that is control participants’ characteristics should not be associated with abnormally good or bad lower limb muscle strength and/or balance. This was not always the case. Several included case-control studies selected controls with characteristics, such as recent falls or pain. Pain is associated with increased falls risk [37, 38], and impaired balance [25] and lower limb muscle strength [24] are associated with falls risk. So, controls with pain or previous falls may have impaired lower limb muscle strength and/or balance. In other studies, participants’ falls history was unreported making interpretation of the adequacy of controls difficult. This potential source of bias is not assessed in the amended Newcastle-Ottawa Scale used to appraise case-control studies in this review.
Notwithstanding this limitation, there is some evidence that older adults with a distal radius fracture demonstrate impaired lower limb muscle strength during functional tests compared to age- and sex/gender-matched controls. Whether the magnitude of between group differences are clinically relevant is uncertain. In Cho et al., [26] the between group difference in five times sit-to-stand test performance is below the reported minimum clinically important difference (MCID) for older adults with stable chronic obstructive pulmonary disease (1.7 s) [39] and vestibular dysfunction (2.3 s) [40]. Furthermore, the precision of this difference could not be assessed because the 95% confidence interval was not reported. In Crockett et al., [17] the between group difference in 30 s sit-to-stand performance exceeds the reported major clinically important improvement (2.0 to 2.6) [41] for people with hip osteoarthritis but the wide confidence interval shows this estimate is imprecise [26, 17]. Control participants’ characteristics could also have been associated with lower limb muscle strength performance. In Cho et al., [26] controls had a painful upper limb condition, and in Crockett et al., [17] control participants’ falls history was not reported. Methodological quality also varied with Cho et al., [26] and Crockett et al., [17] scoring 8/8 and 4/8 stars, respectively, on the Modified Newcastle-Ottawa Scale. These limitations reduce confidence in the finding that lower limb muscle strength assessed functionally is impaired in older adults with a distal radius fracture compared to age- and sex/gender-matched controls.
Compared to normative values in similarly aged healthy Danish (age 60–69, mean 18.57 (SD 5.94) reps) [42], Australian (age ≥ 60, mean 15.9 (SD 5.1) reps) [43], and Hong Kong women (age 65–69, mean 15.4 (SD 4.4) reps) [44], 30 s sit-to-stand test performance was worse in people with a distal radius fracture in included studies [15, 17, 30]. Five times sit-to-stand performance in people with a distal radius fracture in included studies [26, 33, 34] was also worse than normative values in similarly aged Italian women (age 60–64 to 70–74, mean 7.9 (SD 2) to 8.7 (SD2.3) seconds) [45] and older Japanese adults (age ≥ 60, mean 8.5s; 95% CI 7.93 to 9.07) [46], but comparable to cohorts of 60–69 year old UK females (median range 10.46 to 17.19 s) [47] and a meta-analysis of reference values for 60 to 69-year-olds (mean 11.4 s; 95% CI 11.4 to 11.4) [48]. Variability in published norms for the five times sit-to-stand test may reflect differences in the evaluated populations, or differences in testing procedures, a recognised problem with this test [48].
Three case-control studies assessed lower limb muscle strength during isolated joint movements [18, 21, 28]. All assessed knee extension strength with conflicting findings. In these studies, control participants either had no recent falls [28], recent falls [18], or falls history was not reported [21]. Assessment procedures and results reporting were also inconsistent. This heterogeneity limited our ability to draw inferences on the comparative knee extension strength between older adults with a distal radius fracture and age- and gender-matched controls. The comparative ankle dorsiflexion and knee flexion strength between older adults with a distal radius fracture and age- and gender-matched controls also remains uncertain because these were only assessed in one case-control study [28].
Though lower limb muscle strength assessment using isolated joint movements was common in included studies, comparison of results between included studies and with other cohorts was limited because of variability in measurement devices, assessment procedures, measurement units, and a lack of published normative values in large cohorts of healthy older adults. Until these limitations are addressed, functional tests, such as the 30 s sit-to-stand, may be preferable when assessing lower limb muscle strength in older adults with a distal radius fracture. The 30 s sit-to-stand and five times sit-to-stand tests have relatively standardised testing procedures, established normative values in large cohorts of healthy older adults, and do not require specialist equipment.
Though results and assessment methods were inconsistent across included case-control studies, there was an overall trend of impaired balance in older adults with a distal radius fractures compared to age and sex/gender-matched controls. Seven case-control studies evaluated balance using tests that do not require specialist equipment. Two of these found no difference in balance between groups [18, 26]. However, in Cho et al., [26] controls had a painful unilateral upper limb condition, and in Edwards et al., [18] controls had a similar falls history to cases. As described previously, these characteristics are associated with impaired balance, potentially explaining why these studies did not detect a between group difference in balance performance. The five other case-control studies that assessed balance without specialist equipment found cases, or sub-groups of cases, had impaired balance compared to controls [14, 20, 21, 27, 30], though the difference in Berg Balance Scale scores in Crockett et al. [30] was below the MCID values reported for older adults with other musculoskeletal conditions [49]. These five studies did not report participants’ falls history. If control participants did have recent falls, the between group differences in balance could be smaller than if control participants had no recent falls. Three case-control studies assessed balance using specialist equipment [16, 19, 28]. All found cases performed worse than age- and sex/gender-matched controls, except for Sharabiani et al., [16] which only found a difference between cases and controls when postural sway was assessed while standing on foam. Interpretation of results from case-control studies that assessed balance needs to consider variability in control participants’ characteristics; assessment methods; and the clinical relevance, magnitude, and precision (where reported) of between group differences. Nevertheless, the available evidence indicates that older adults with a distal radius fracture may have impaired balance compared to age- and sex/gender-matched controls, though confidence in this finding is low.
Single leg balance was the most common balance assessment method, but assessment procedures and/or reporting of results differed between all studies that used this assessment method. Test parameters, such as maximum test duration, gender, and age affect single leg balance scores [50] which limits comparison of results between studies and different cohorts. When included studies results are compared against normative values for adults aged ≥ 60 years without conditions that impair balance (weighted mean 26.9 s, 95% 23.6 to 30.2) [50] and single leg stand performance with eyes closed in healthy Australian women aged ≥ 60 years (mean 4.1 (SD 4.2) seconds) [43], no consistent trend was observed. Postural sway, the functional reach test, the Berg Balance Scale, and the Biodex Balance System were the next most common balance assessment methods. Compared to some cohorts of community-dwelling 70-year-olds, participants with a distal radius fracture in included studies performed marginally worse on the Berg Balance Scale [51]. The clinical relevance of this remains unclear as there is no high-quality evidence for cut-off scores that predict future falls [52]. There was a wide range of functional reach test scores across included studies which may be attributable to variability in testing procedures which can be a problem with this test [53]. However, performance in included studies typically exceeded normative values in community-dwelling older adults aged ≥ 60 years (mean 26.6 cm, 95% CI 25.14 to 28.06) [53], indicating that functional reach test performance may not detect balance impairments in older adults with a distal radius fracture if they exist.
There was a trend of improved lower limb muscle strength and balance over time in studies that assessed participants at multiple timepoints, indicating a possible decline in lower limb muscle strength and balance in older adults after distal radius fracture. Without prospective studies that assess lower limb muscle strength and balance before and after distal radius fracture, this remains uncertain.
In future, researchers should consider large-scale robust case-control studies, or prospective observational studies that evaluate lower limb muscle strength and/or balance before and after distal radius fracture, to address current limitations in the evidence base. To facilitate synthesis of results in future systematic reviews, assessments with standardised procedures and units of measurements should be used. Prioritisation of assessments that can be used in clinical environments to enable larger-scale research, without requiring specialist equipment, and where published normative values in healthy populations already exist, should be considered. For clinicians, the results suggest that older adults with distal radius fractures may have impaired lower limb muscle strength and/or balance, compared to controls. Therefore, the available evidence supports current guidelines that recommend older patients presenting with a fall-related distal radius fracture should be assessed for muscle strength and balance deficits as part of a falls-risk assessment [7].
This review has methodological limitations. Relevant studies may have been missed: only studies published since 1990 were eligible and we did not search grey literature. To minimise the risk of missing relevant studies, we screened the reference lists of included studies and relevant systematic reviews. Two reviewers did not extract data independently, but all extracted data was checked by a second reviewer against the published report(s). We used a modified version of the Newcastle-Ottawa scale to appraise case-control studies and case series. The Newcastle-Ottawa scale has been criticised for its poor reliability [54] and attribution of equal weight to individual domains [55], but we are not aware of another appraisal tool that caters for the study designs and outcomes of interest in this systematic review.
With respect to included studies, none assessed participants before and after distal radius fracture, so it cannot be ruled out that reported impairments in case-control studies existed pre-injury. Only 5% of participants with a distal radius fracture in included studies were men and most studies conducted assessments ≥ 6 months after fracture, so findings may not be generalisable to older men or those with a recent distal radius fracture. Where relevant, between group differences were often imprecise or not reported. This has added relevance as we did not conduct a meta-analysis.
Strengths of this systematic review include prospective registration of the systematic review protocol, independent screening of titles and abstracts and full-text reports by two reviewers, and reporting of our methods and search strategy so that this systematic review is reproducible.
Conclusions
Compared to matched control participants, there is some evidence that adults aged ≥ 50 years with a distal radius fracture have impaired lower limb muscle strength and balance, but findings are inconsistent across studies and/or outcome measures. Variability in control participants’ characteristics, study design, study quality, and lower limb muscle strength and balance assessment methods, limited synthesis of results. Given the high prevalence of distal radius fractures and the increased risk of future fractures, falls, and functional decline in older adults after this injury, this remains an area of important clinical concern. Large-scale robust case-control and/or prospective observational studies are needed to address limitations in the current literature. This would inform rehabilitation requirements for these patients. To facilitate synthesis of results in future systematic reviews, future studies should consider using lower limb muscle strength and balance assessments that have standardised assessment procedures and measurement units.
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CI:
-
Confidence interval
- MCID:
-
Minimum clinically important difference
- Nm:
-
Newton metre
- PROSPERO:
-
international prospective register of systematic reviews
- PRISMA:
-
Preferred reporting items for systematic review and meta-analyses
- RCT:
-
Randomised controlled trial
- SD:
-
Standard Deviation
References
Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006;37:691–7.
Borgström F, Karlsson L, Ortsäter G, et al. Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos. 2020. https://doi.org/10.1007/s11657-020-0706-y.
Abrahamsen B, Jørgensen NR, Schwarz P. Epidemiology of forearm fractures in adults in Denmark: national age- and gender-specific incidence rates, ratio of forearm to hip fractures, and extent of surgical fracture repair in inpatients and outpatients. Osteoporos Int. 2015;26:67–76.
Edwards BJ, Song J, Dunlop DD, Fink HA, Cauley JA. Functional decline after incident wrist fractures - study of osteoporotic fractures: prospective cohort study. BMJ. 2010;341:189.
Barrett-Connor E, Sajjan SG, Siris ES, Miller PD, Chen YT, Markson LE. Wrist fracture as a predictor of future fractures in younger versus older postmenopausal women: results from the National osteoporosis Risk Assessment (NORA). Osteoporos Int. 2008;19:607–13.
MacIntyre, Dewan N. Epidemiology of distal radius fractures and factors predicting risk and prognosis. J Hand Ther. 2016;29:136–45.
National Institute for Health and Care Excellence. (2013) NICE clinical guideline 161 falls: assessment and prevention of falls in older people. https://www.nice.org.uk/Guidance/CG161.
Sherrington C, Fairhall N, Wallbank G, Tiedemann A, Michaleff ZA, Howard K, Clemson L, Hopewell S, Lamb S. Exercise for preventing falls in older people living in the community: an abridged Cochrane systematic review. Br J Sports Med. 2020;54:885–91.
Handoll HHG, Elliott J. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev. 2015. https://doi.org/10.1002/14651858.CD003324.pub3
Bruder AM, Shields N, Dodd KJ, Taylor NF. Prescribed exercise programs may not be effective in reducing impairments and improving activity during upper limb fracture rehabilitation: a systematic review. J Physiother. 2017;63:205–20.
Abtahi S, Driessen JHM, Vestergaard P, van den Bergh J, Boonen A, de Vries F, Burden AM. Secular trends in major osteoporotic fractures among 50 + adults in Denmark between 1995 and 2010. Osteoporos Int. 2019;30:2217–23.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009. https://doi.org/10.1371/journal.pmed.1000100.
Armstrong AL, Oborne J, Coupland CA, Macpherson MB, Bassey EJ, Wallace WA. Effects of hormone replacement therapy on muscle performance and balance in post-menopausal women. Clin Sci. 1996;91:685–90.
Fujita K, Kaburagi H, Nimura A, Miyamoto T, Wakabayashi Y, Seki Y, Aoyama H, Shimura H, Kato R, Okawa A. Lower grip strength and dynamic body balance in women with distal radial fractures. Osteoporos Int. 2019;30:949–56.
Mehta SP, MacDermid JC, Richardson J, Macintyre NJ, Grewal R. Reliability and validity of selected measures associated with increased fall risk in females over the age of 45 years with distal radius fracture - A pilot study. J Hand Ther. 2015;28:2–10.
Sharabiani PTA, Jafari D, Mehdizadeh H, et al. Can Postural instability in individuals with distal Radius Fractures be alleviated by concurrent cognitive tasks? Clin Orthop Relat Res. 2019;477:1659–71.
Crockett K, Kontulainen SA, Farthing JP, Chilibeck PD, Bath B, Baxter-Jones ADG, Arnold CM. Differences in function and fracture risk in Postmenopausal Women with and without a recent distal Radius fracture. J Aging Phys Act. 2018;26:136–45.
Edwards BJ, Langman CB, Martinez K, Johnson M, Mille ML, Rogers MW. Women with wrist fractures are at increased risk for future fractures because of both skeletal and non-skeletal risk factors. Age Ageing. 2006;35:438–41.
Louer CR, Boone SL, Guthrie AK, Motley JR, Calfee RP, Wall LB. Postural stability in older adults with a distal radial fracture. J Bone Joint Surg - Am Volume. 2016;98:1176–82.
Ringsberg K, Johnell O, Obrant K. Balance and speed of walking of women with Colles’ fractures. Physiotherapy. 1993;79:689–92.
Hakestad KA, Nordsletten L, Torstveit MK, Risberg MA. Postmenopausal women with osteopenia and a healed wrist fracture have reduced physical function and quality of life compared to a matched, healthy control group with no fracture. BMC Womens Health. 2014;14:92.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. Newcastle - Ottawa Quality Assessment Scale. http://www.ohri.ca/programs/clinical_epidemiology/nosgen.pdf. Accessed 3 Jan 2020.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://www.handook.cochrane.org
Moreland JD, Richardson JA, Goldsmith CH, Clase CM. Muscle weakness and falls in older adults: a systematic review and Meta-analysis. J Am Geriatr Soc. 2004;52:1121–9.
Muir SW, Berg K, Chesworth B, Klar N, Speechley M. Quantifying the magnitude of risk for balance impairment on falls in community-dwelling older adults: a systematic review and meta-analysis. J Clin Epidemiol. 2010;63:389–406.
Cho YJ, Gong HS, Song CH, Lee YH, Baek GH. Evaluation of physical performance level as a fall risk factor in women with a distal radial fracture. J Bone Joint Surg - Ser A. 2014;96:361–5.
Sakai A, Oshige T, Zenke Y, Yamanaka Y, Otsuka H, Nakamura T. Shorter unipedal standing time and lower bone mineral density in women with distal radius fractures. Osteoporos Int. 2010;21:733–9.
O’Reilly, Keogan F, Breen R, Moore A, Horgan NF. Falls risk factors and healthcare use in patients with a low-trauma wrist fracture attending a physiotherapy clinic. Int J Ther Rehabil. 2013;20:480–6.
Maeda K, Imatani J, Moritani S, Kondo H. Effects of eldecalcitol alone or a bone resorption inhibitor with eldecalcitol on bone mineral density, muscle mass, and exercise capacity for postmenopausal women with distal radius fractures. J Orthop Sci. 2020. https://doi.org/10.1016/j.jos.2020.11.009.
Crockett K, Farthing JP, Basran J, Dal Bello-Haas V, Johnston G, Haver CRA, Arnold CM. Changes in fall risk and functional status in women aged 50 years and older after distal radius fracture: a prospective 1-year follow-up study. J Hand Ther. 2019;32:17–24.
Nordell E, Jarnlo GB, Thorngren KG. Decrease in physical function after fall-related distal forearm fracture in elderly women. Adv Physiother. 2003;5:146–54.
Dewan N, Macdermid JC, Grewal R, Beattie K. Association of modifiable risk factors with bone mineral density among people with distal radius fracture: a cross-sectional study. Physiotherapy Can. 2019;71:58–68.
Baldursdottir B, Whitney SL, Ramel A, Jonsson PV, Mogensen B, Petersen H, Kristinsdottir EK. Multi-sensory training and wrist fractures: a randomized, controlled trial. Aging Clin Exp Res. 2020;32:29–40.
Hansson EE, Dahlberg LE, Magnusson M. Vestibular Rehabilitation affects vestibular asymmetry among patients with fall-related wrist fractures - a Randomized Controlled Trial. Gerontology. 2015;61:310–8.
Wong RMY, Ho WT, Tso CY, Ng WKR, Chow SKH, Tang TN, Cheung WH. Vibration therapy as an intervention for postural training and fall prevention after distal radius fracture in elderly patients: a randomized controlled trial. Osteoporos Int. 2019;30:766–S766.
Schulz KF, Grimes DA. Case-control studies: research in reverse. Lancet. 2002;359:431–4.
Leveille SG, Jones RN, Kiely DK, Hausdorff JM, Shmerling RH, Guralnik JM, Kiel DP, Lipsitz LA, Bean JF. Chronic Musculoskeletal Pain and the occurrence of Falls in an older Population. JAMA. 2009;302:2214–21.
Li W, Gamber M, Han J, Sun W, Yu T. The Association between Pain and fall among Middle-Aged and older chinese. Pain Manage Nurs. 2021;22:343–8.
Jones SE, Kon SSC, Canavan JL, Patel MS, Clark AL, Nolan CM, Polkey MI, Man WD-C. The five-repetition sit-to-stand test as a functional outcome measure in COPD. Thorax. 2013. https://doi.org/10.1136/thoraxjnl.
Meretta BM, Whitney SL, Marchetti GF, Sparto PJ, Muirhead RJ. The five times sit to stand test: responsiveness to change and concurrent validity in adults undergoing vestibular rehabilitation. J Vestib Res. 2007;16:233–43.
Wright AA, Cook CE, Baxter GD, Dockerty JD, Abbott JH. A comparison of 3 methodological approaches to defining major clinically important improvement of 4 performance measures in patients with hip osteoarthritis. J Orthop Sports Phys Ther. 2011;41:319–27.
Suetta C, Haddock B, Alcazar J, et al. The Copenhagen Sarcopenia Study: lean mass, strength, power, and physical function in a danish cohort aged 20–93 years. J Cachexia Sarcopenia Muscle. 2019;10:1316–29.
McKay MJ, Baldwin JN, Ferreira P, et al. Reference values for developing responsive functional outcome measures across the lifespan. Neurology. 2017;88:1512–9.
Chung PK, Zhao Y, Liu JD, Quach B. Functional fitness norms for community-dwelling older adults in Hong Kong. Arch Gerontol Geriatr. 2016;65:54–62.
Landi F, Calvani R, Martone AM, Salini S, Zazzara MB, Candeloro M, Coelho-Junior HJ, Tosato M, Picca A, Marzetti E. Normative values of muscle strength across ages in a ‘real world’ population: results from the longevity check-up 7 + project. J Cachexia Sarcopenia Muscle. 2020;11:1562–9.
Nakazono T, Kamide N, Ando M. The reference values for the chair stand test in healthy japanese older people: determination by meta-analysis. J Phys Ther Sci. 2014;26:1729–31.
Cooper R, Hardy R, Sayer A, et al. Age and gender differences in physical capability levels from mid-life onwards: the harmonisation and meta-analysis of data from eight UK cohort studies. PLoS ONE. 2011. https://doi.org/10.1371/journal.pone.0027899.
Bohannon RW. Reference values for the five-repetition sit-to-stand test: a descriptive meta-analysis of data from elders. Percept Mot Skills. 2006;103:215–22.
Low DC, Walsh GS. The minimal important change for measures of balance and postural control in older adults: a systematic review. Age Ageing. 2022. https://doi.org/10.1093/ageing/afac284.
Bohannon RW, Tudini F. Unipedal balance test for older adults: a systematic review and meta-analysis of studies providing normative data. Physiotherapy. 2018;104:376–82.
Downs S, Marquez J, Chiarelli P. Normative scores on the Berg Balance Scale decline after age 70 years in healthy community-dwelling people: a systematic review. J Physiother. 2014;60:85–9.
Lima CA, Ricci NA, Nogueira EC, Perracini MR. The Berg Balance Scale as a clinical screening tool to predict fall risk in older adults: a systematic review. Physiotherapy. 2018;104:383–94.
Rosa MV, Perracini MR, Ricci NA. Usefulness, assessment and normative data of the functional Reach Test in older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. 2019;81:149–70.
Hartling L, Milne A, Hamm MP, Vandermeer B, Ansari M, Tsertsvadze A, Dryden DM. Testing the Newcastle Ottawa Scale showed low reliability between individual reviewers. J Clin Epidemiol. 2013;66:982–93.
Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Crockett K, Arnold C, Farthing J, Chilibeck P, Johnston J, Bath B, Baxter-Jones A, Kontulainen S. Bone strength and muscle properties in postmenopausal women with and without a recent distal radius fracture. Osteoporos Int. 2015;26:2461–9.
Acknowledgements
We would like to thank the information specialists at the Bodleian Health Care Libraries, Oxford, for their expertise in developing the search strategy.
Funding
This study was funded as part of a National Institute of Health and Care Research (NIHR) Postdoctoral Fellowship (ref. PDF-2016-09-056) awarded to David J Keene and a personal Fellowship awarded to Colin Forde by the NIHR Biomedical Research Centre, based at Oxford University Hospitals Trust, Oxford.
Author information
Authors and Affiliations
Contributions
David J Keene developed the study idea. Matthew L Costa and Sarah E Lamb reviewed the review protocol. David J Keene, Philippa JA Nicolson, Charlotte Vye, and Colin Forde screened study reports. Charlotte Vye, Warren Sheehan, Jessica CH Pun, Philippa JA Nicolson, and Colin Forde extracted and/or checked extracted data. Colin Forde, David J Keene, and Philippa JA Nicolson appraised the quality of included studies. Colin Forde and Philippa JA Nicolson synthesised the data. The first draft of the manuscript was written by Colin Forde. Critical feedback on the manuscript and data interpretation was provided by Matthew L Costa, Sarah E Lamb, David J Keene, and Philippa JA Nicolson. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
David J Keene is supported by a NIHR Postdoctoral Fellowship (ref. PDF-2016-09-056). Colin Forde is supported by a NIHR Doctoral Fellowship (ref. NIHR301759). Philippa JA Nicolson is supported by a Versus Arthritis Foundation Fellowship (ref. 22428). Jessica CH Pun is supported by a Versus Arthritis Nurse and Allied Health Professionals Internship Programme. Matthew L Costa is a NIHR Senior Investigator. This study was supported by the NIHR Oxford Biomedical Research Centre. The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS or the UK Department of Health and Social Care. Sarah E Lamb, Warren Sheehan, and Charlotte Vye declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12891_2023_6711_MOESM5_ESM.docx
Additional file 5: Lower limb muscle strength in adults aged ≥ 50 years with a distal radius fracture by assessment method
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Forde, C., Nicolson, P.J., Vye, C. et al. Lower limb muscle strength and balance in older adults with a distal radius fracture: a systematic review. BMC Musculoskelet Disord 24, 741 (2023). https://doi.org/10.1186/s12891-023-06711-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06711-4