Abstract
Background
Prevalence of musculoskeletal pain is high among eldercare workers, and therapeutic exercise has shown to be effective for its management. Although telerehabilitation is an increasingly used alternative for delivering therapeutic exercise, no studies have assessed synchronous group telerehabilitation interventions for the management of musculoskeletal disorders. Thus, the aim of this article is to describe the protocol of a randomized controlled trial that will assess the effects of a videoconference-based group therapeutic exercise intervention on the musculoskeletal pain of eldercare workers.
Methods
This multicenter trial will randomly assign 130 eldercare workers to either a control or experimental group. Participants in the control group will not receive any intervention, and participants in the experimental group will take part in a 12-week remote supervised videoconference-based intervention, consisting of 2 weekly 45-min group sessions. Each session will include 4 sets of 6 progressive resistance exercises for the lower limbs, upper limbs and trunk, performed with bodyweight and elastic bands at moderate-high intensity. Following the 12 weeks, participants in the experimental group will be provided with material for autonomously carry on the therapeutic exercises and advised to continue performing 2 weekly sessions on their own until a 48-week follow-up. Assessments will be performed at baseline, 12 and 48 weeks. Primary outcome will be average pain intensity in the low back during the last 7 days, measured by the 0–10 Numerical Rating Scale. Secondary outcomes will include additional measures of musculoskeletal pain, psycho-affective state, work-related variables, and physical fitness.
Discussion
This will be the first trial, to our knowledge, assessing whether a remote delivery of a group therapeutic exercise intervention via videoconference is effective for reducing the musculoskeletal pain, improving the psycho-affective state and physical fitness, and enhancing the work-related parameters in eldercare workers. If successful, this study will provide innovative tools for implementing effective, scalable and affordable interventions to tackle musculoskeletal disorders in the workplace. It will also highlight the utility of telehealth, and address the importance of therapeutic exercise to manage musculoskeletal pain in a critical population for the future of the aging societies as it is the eldercare workers.
Trial registration
The study protocol was prospectively registered at ClinicalTrials.gov (registration number: NCT05050526) on September 20, 2021.
Similar content being viewed by others
Introduction
Eldercare workers are qualified professionals who provide assistance to dependent elderly people at either home or long-term facilities [1]. Demographic projections for the coming decades suggest that the demand for eldercare will at least double by 2050 [2], which makes these professionals a cornerstone for facing the challenge of aging. Taking care of people with moderate or severe disability is a physically demanding task, involving lifting, transferring and other care activities that might lead to an overload of musculoskeletal tissues [3]. Several studies have shown that prevalence of pain is high among eldercare workers [4, 5], with 88% of these professionals reporting at least one body part with work-related musculoskeletal symptoms [6]. Besides, prospective studies with large samples have found that a higher intensity [7] and frequency [8] of pain, as well as a higher number of pain locations [9], are significant risk factors for long-term sickness absence in eldercare workers. Moreover, the presence of pain-related disability and a longer pain duration predict the risk of dropout or job turnover from the eldercare sector [10]. In eldercare workers, musculoskeletal pain is often accompanied by mental health disorders [11,12,13], which can be exacerbated by the high psychological demands of the profession [14,15,16].
Physical activity and therapeutic exercise interventions have been shown to be effective in reducing musculoskeletal pain in the general adult population [17], and are included as a first-line treatment in all high-quality clinical practice guidelines with the most up-to-date evidence [18]. Although the biological mechanisms leading to exercise-induced hypoalgesia are not yet fully understood, it seems that the activation of the endogenous opioid system during exercise plays a key role [19]. However, it has been suggested that the endocannabinoid, serotonergic, immune and autonomic nervous systems may also be involved, and there are several psychosocial factors that could influence the exercise modulation of pain [19]. From a biomechanical point of view, improvements in the structure and function of the musculoskeletal system, especially muscle strength, could explain the pain reduction induced by exercise [20].
Telerehabilitation is an increasingly used alternative for remotely delivering health services using telecommunications technologies [21, 22]. Although previous studies reported some positive effects on pain and other health-related outcomes, a recent review stated that it is imperative to conduct high quality clinical trials in order to identify effective telerehabilitation interventions [21]. To the knowledge of the authors, the great majority of internet-based interventions have consisted of websites with content for autonomous consultation, or individual home-videoconference sessions [21,22,23,24,25]. There are two positive experiences showing that synchronous supervised sessions are a feasible way to present group therapeutic exercise interventions in people with chronic obstructive pulmonary disease [26] and older adults [27], but no study has been addressed to assess their effectiveness on musculoskeletal disorders yet. Synchronous supervision and group dynamic could be important for designing exercise programs, as both features are related to higher participant adherence, what may therefore lead to a higher effectiveness [28, 29]. In addition, it could also allow for greater intervention safety, since participants can be continuously monitored for correct execution during exercising.
Thus, a study protocol for a randomized controlled trial was designed with the aim of assessing the effects of a videoconference-based group therapeutic exercise intervention in the medium and long term on the musculoskeletal pain of eldercare workers. Secondary outcomes will include measures related to the psycho-affective state, work-related variables and physical fitness.
Methods
Study design
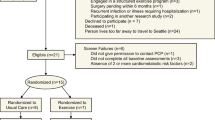
A parallel-assignment, multicenter randomized controlled trial will be carried out. Participants will be recruited from institutions providing eldercare services at home or in long-term facilities. In each of the institutions, and following baseline measurements, participants will be randomly assigned (1:1 ratio) through sealed opaque envelopes to either a control or experimental group by a coin-tossing sequence generation. Assessments of primary and secondary outcomes will be conducted at baseline and at 12 weeks (post-supervised phase) and 48 weeks (post-unsupervised phase) from the beginning of the intervention (Fig. 1). Outcome assessors and data analysts will be blinded to group allocation. Because of the nature of the study, blinding of the participants and the professional supervising the sessions is not possible. The study was designed, and the results will be reported according to the SPIRIT statement [30] and CONSORT guidelines for trials of nonpharmacologic treatment interventions [31].
Inclusion and exclusion criteria
Subjects will be considered eligible for the study if they meet all the following criteria: (a) are formal eldercare workers from eldercare institutions, (b) are ≥ 18 years of age, (c) have ≥ 3 months of experience in the profession, and (d) have an employment contract until at least the date of study completion. Participants will be excluded if (a) they are pregnant or (b) their participation is considered contraindicated according to the American College of Sports Medicine’s exercise preparticipation health screening guidelines [32].
Control group
Participants in the control group will not receive any intervention and will be instructed to continue with their usual lifestyle.
Experimental group
Supervised phase
Participants in the experimental group will take part in a 12-week exercise intervention, consisting of two videoconference-supervised sessions per week of 45 min each. A minimum interval of 48 h will be ensured between sessions. The sessions will be carried out in groups of a maximum of 10 participants, implemented in the workplace but outside of working hours, and remotely supervised in real-time by a professional with previous experience in delivering group exercise sessions. Real-time videoconference platforms such as Webex (Cisco Systems, Milpitas, USA) will be used, and audio and video will be continuously shared between participants and trainer to allow complete bidirectional feedback (Fig. 2).
The technical content of the program is based on a literature review, authors’ expertise and field experience, as well as on the results of a previous pilot trial that we carried out between January and March 2020 with 20 eldercare workers [33], that allowed us to define the exercises, intensities, and feasibility of a program addressed for reducing the musculoskeletal pain in this population. Intervention details are reported based on the Template for Intervention Description and Replication (TIDieR) Checklist [34]. Sessions will start with a warm-up (5–10 min), including joint mobility and aerobic activation exercises focused on increasing heart rate. The main part of the session will consist of resistance exercises (30 min) performed at moderate-high intensity. In total, 9 exercises will be performed throughout the program (Fig. 3). In each session, 4 sets of 6 resistance exercises will be performed, with a 2-min active rest (dynamic stretching and breathing exercises) between sets. Exercises will be systematically varied between sessions so that each of them is evenly performed during the program. In each set, exercises for the different major muscle groups will be alternated in a circuit manner (e.g., lower limb, upper limb, trunk, lower limb, upper limb, trunk) (Table 1). Unilateral exercises will be alternated between sets so that both sides of the body are evenly worked in each session. Exercises will be performed with minimal equipment, combining body-weight and 2-m-long elastic band exercises. Three progression levels will be set for each of the exercises: progression 1 (weeks 1–4), progression 2 (weeks 5–8) and progression 3 (weeks 9–12) (Fig. 3). All participants will start in progression 1, and transition to a subsequent progression will only be allowed if the participant completes ≥ 4 sessions in the previous progression level. Progression levels are achieved by modifying the exercise technique (e.g., increasing the force lever) or utilizing elastic bands of different resistances (1.7, 2.1 and 2.6 kg at 100% elongation for progressions 1, 2 and 3, respectively) (Fig. 3). One minute will be dedicated to the completion of each exercise (including work and rest times), and within each progression level, the work:rest ratio will augment from 30:30 to 45:15 s, thus adding 5 s of work and reducing 5 s of rest each week (Fig. 4). Participants will be asked and monitored to work at a rate of perceived exertion between 3 (moderate) and 5 (strong) on the Borg's CR-10 scale [35] and not to reach failure in any of the exercises. If any of the exercises cause intolerable pain, the 4-stage exercise adjustment model proposed by Jakobsen et al. [36] will be used: (1) reduce loading intensity (e.g., returning to a previous progression level or even performing the exercise without external resistance), (2) reduce movement velocity, (3) reduce range of motion, and (4) interrupt exercise. If an exercise needs to be interrupted, it will be replaced by a pain-free exercise focused on the same muscle group. Sessions will finish with a cool-down (5–10 min), including static stretching and breathing/relaxing exercises. Daily attendance will be recorded by the professional who supervises the sessions. This professional will also collect information on the completion and intensity of each participant's training in each session. Adherence will be reported as the percentage of sessions in which participants performed the planned training regarding completion and intensity (i.e., 24 sessions = 100% of adherence) [37].
Unsupervised phase
When the 12-week supervised sessions are finished, participants in the experimental group will be encouraged to continue performing 2 weekly sessions on their own until the 48-week follow-up. To facilitate this autonomous training, we will create supportive material for the sessions that will include two 45-min recordings with the equivalent content to a session planned for the 12th week, explanatory videos of the 9 exercises performed in the supervised program and their corresponding progressions, as well as written instructions about how to perform the exercises. To record completion in this unsupervised phase, participants will be asked, every 12 weeks and until the 48-week assessments (Fig. 1), the following questions: (a) in the last 12 weeks, in how many weeks did you perform the exercises? (0–12) and (b) on average, in each of those weeks in which you performed the exercises, on how many days did you perform them? (0–7). The result of the multiplication of both answers will be considered the number of performed unsupervised sessions. In this case, self-reported completion will be calculated as a percentage of performed sessions (i.e., 72 sessions = 100% completion in the unsupervised phase).
Outcomes
Baseline descriptive data
Participants will report by a self-administered written questionnaire the following descriptive data at baseline: date of birth, sex (male/female), height (cm), mass (kg), marital status (single/married/divorced/widower), educational level (primary/secondary/tertiary education), number of children (n), children cohabiting at home (no/yes), care for dependent people outside the work environment (no/yes), working hours (hours/week), experience in the profession (years), type of work shift (rotative/fixed), night shift (no/yes), alcohol consumption (never/monthly or less/2–4 times a month/2–3 times a week/ ≥ 4 times a week) [38], tobacco consumption (daily/less than daily/not at all) [39], recreational physical activity (1–8) [40], and regular resistance-exercise training (no/yes).
Primary outcome
The primary outcome will be average pain intensity in the low back during the last 7 days, measured by the 0–10 Numerical Rating Scale (NRS) [41] ranging from 0 (complete absence of pain) to 10 (worst imaginable pain) (Table 2).
Secondary outcomes
A detailed description of all the secondary outcomes is shown in Table 2. They will include validated questionnaires and tests for evaluating: (a) musculoskeletal pain [41] (intensity, frequency, and interference) of the low back, neck, shoulders and hands/wrists; (b) psycho-affective state [42,43,44,45,46] (subjective happiness, anxiety and depression, burnout, sleep quality, and quality of life) which will be collected by a self-administered written questionnaire; (c) work-related variables [47,48,49] (work ability, performance, physical exertion, and absenteeism) which will be obtained by a self-administered written questionnaire and from the official registry of the participating eldercare institution; and (d) physical fitness (trunk, lower and upper limbs muscle performance), which will be evaluated by a battery of physical performance tests [50,51,52] previously validated by our research group to be carried out remotely by real-time videoconference [53]. The participant's self-reported days of medication consumption of analgesics and hypnotics/anxiolytics during the last 7 days at each assessment point will also be recorded.
Adverse events
Adverse events occurring during the supervised exercise sessions will be collected by the professional supervising the sessions and divided into 2 types: a) technical (connection and/or operation problems with the videoconferencing system) and b) participant safety-related (pain, discomfort, or any other health-related problem appearing during the session). Adverse events will also be classified as minor (those that slightly hinder the development of the exercise session) and major (those that prevent the development of the exercise session).
Sample size calculation
The sample size was calculated to detect a significant change in low back pain that could be relevant in terms of absenteeism from work [54]. Taking into account the average low back pain intensity of 5.0 ± 2.6 in the 0–10 NRS for pain observed in previous studies carried out by our research group in eldercare workers [55] and accepting an alpha error of 0.05 and a beta error of 0.20 in a bilateral contrast, 108 participants are necessary to detect a difference equal to or greater than 1 unit. The sample size has been increased by 20% due to expected dropouts. Therefore, the required sample will be 130 participants (65 in the control group and 65 in the experimental group).
Statistical analysis plan
IBM SPSS Statistics 27 statistical software package (SPSS, Inc., Chicago, IL) will be used for data analysis. Normality of distribution will be checked using the Kolmogorov‒Smirnov test, and non-normally distributed variables will be square-root transformed for statistical analysis. Continuous and categorical data will be reported as mean (standard deviation) and frequency (percentage), respectively. The primary analysis will be based on intention-to-treat, including data from all participants regardless of adherence to the intervention. Additionally, a per-protocol analysis will be performed, including only data from participants with ≥ 50% adherence. Finally, a post-hoc subgroup analysis will be performed to assess the effects of the intervention on low back pain outcomes separately in participants with (≥ 1 in average 0–10 NRS) and without (< 1 in average 0–10 NRS) low back pain at baseline. Between-group comparisons at baseline will be performed with the independent samples T and Chi-squared tests for continuous and categorical variables, respectively. For continuous variables, intervention effects will be analyzed with a group-by-time ANCOVA including baseline measurements as covariates. This ANCOVA will be performed separately to assess intervention effects in two time periods: 0 vs 12 weeks and 0 vs 48 weeks. Within-group changes in each time period will be performed with the paired samples T test. Effect size will be estimated by partial eta squared (η2). Values for η2of 0.02, 0.13, and 0.26 will be considered small, medium and large, respectively [56]. For categorical variables, intervention effects will be analyzed with McNemar’s test. The level of statistical significance will be set at p < 0.05.
Trial status
The trial is currently ongoing, with the first participants taking part in the intervention. Recruitment is still active and will cease when the required sample size is achieved.
Ethics
All workers from the participating eldercare institutions will receive oral and written information about the study, including objectives, assessments and intervention details. After fully understanding the study, volunteers who meet the selection criteria will sign an informed written consent form before enrolling in the study. The study protocol was approved by the Ethics Committee for Research Involving Human Beings of the University of the Basque Country (M10/2019/200MR2), was prospectively registered in ClinicalTrials.gov (NCT05050526), and complies with the Declaration of Helsinki.
Discussion
This manuscript describes the design of the first, to our knowledge, randomized controlled trial that will assess the effects of a videoconference-based exercise intervention on the musculoskeletal pain of eldercare workers in the medium and long term. The therapeutic exercise program is evidence-based, and has been well accepted in terms of modality, intensity and frequency, and considered useful by the eldercare population in a previous pilot study.
We have prioritized a design with simple exercises that allows clear instruction and easy execution, and that guarantees attainable remote supervision by videoconference. The intervention is also carried out with little material and at a low cost, which, if proven effective, might facilitate scaling it to different settings and populations. Moreover, videoconference-based delivery is compatible with situations in which interpersonal physical distancing is needed. Consequently, this study will provide scientific support to implement therapeutic exercise interventions in the workplace, providing innovative telehealth tools for the prevention and treatment of musculoskeletal pain.
Besides, it is widely accepted that increased wellbeing of eldercare workers could lead to a higher quality of care and, with that, a better state of health of the elderly individuals in need of assistance. In this regard, a previous study on informal caregivers found that a worse health status of the caregiver increased the risk of hospitalization of the elderly person they cared for [57]. In addition, prior studies analyzing the effects of face-to-face exercise interventions in eldercare workers reported improvements in work ability [58] and productivity [59], as well as reductions in lost work days [60] and costs of sickness absence [61]. Overall, this study could contribute to the development of more sustainable systems for long-term care, which is a global challenge included among the strategic objectives of the World Health Organization [62].
Some of the strengths of this study are its randomized controlled design, as well as its proper sample size calculation. In addition, methodological details have been thoroughly described, thus ensuring replicability. Besides, the unrestrictive selection criteria will allow the great majority of eldercare workers to participate, giving the study a pragmatic nature that allows it to be highly applicable to what would happen in a real work environment. Finally, the long-term effects of the intervention will be measured with an additional 48-week follow-up.
However, some limitations should be acknowledged. For example, the study might not be powered enough to assess the effects on the secondary outcomes, so it would probably be necessary to carry out new studies to establish reliable conclusions regarding those variables. In addition, compliance during the unsupervised phase of the study is self-reported. Lastly, due to the specificity of the sample in our study, the results may not be directly applicable to other professionals with high rates of musculoskeletal pain.
In conclusion, this study will assess the effectiveness of a videoconference-based therapeutic exercise program that, if successful, will allow to implement effective, scalable and affordable interventions to tackle musculoskeletal disorders in a critical population for the future of the aging societies as it is the eldercare workers.
Availability of data and materials
Not applicable.
References
Organization for Economic Cooperation and Development (OECD). Health at a glance 2019: OECD indicators. 2019.
World Health Organization (WHO). World report on ageing and health. 2015.
Hodder JN, Holmes MWR, Keir PJ. Continuous assessment of work activities and posture in long-term care nurses. Ergonomics. 2010;53:1097–107.
Davis KG, Kotowski SE. Prevalence of musculoskeletal disorders for nurses in hospitals, long-term care facilities, and home health care: a comprehensive review. Hum Factors. 2015;57:754–92.
Chang V, Hiller C, Keast E, Nicholas P, Su M, Hale L. Musculoskeletal disorders in support workers in the aged care sector. Phys Ther Rev. 2013;18:185–206.
Cheung K, Szeto G, Lai GKB, Ching SSY. Prevalence of and factors associated with work-related musculoskeletal symptoms in nursing assistants working in nursing homes. Int J Environ Res Public Health. 2018;15:265.
Andersen LL, Clausen T, Burr H, Holtermann A. Threshold of musculoskeletal pain intensity for increased risk of long-term sickness absence among female healthcare workers in eldercare. PLoS ONE. 2012;7:e41287.
Andersen LL, Clausen T, Mortensen OS, Burr H, Holtermann A. A prospective cohort study on musculoskeletal risk factors for long-term sickness absence among healthcare workers in eldercare. Int Arch Occup Environ Health. 2012;85:615–22.
Melkevik O, Clausen T, Pedersen J, Garde AH, Holtermann A, Rugulies R. Comorbid symptoms of depression and musculoskeletal pain and risk of long term sickness absence. BMC Public Health. 2018;18:981.
Faber A, Giver H, Strøyer J, Hannerz H. Are low back pain and low physical capacity risk indicators for dropout among recently qualified eldercare workers? A follow-up study. Scand J Public Health. 2010;38:810–6.
Kennedy BR. Stress and burnout of nursing staff working with geriatric clients in long-term care. J Nurs Scholarsh. 2005;37:381–2.
Madsen IEH, Aust B, Burr H, Carneiro IG, Diderichsen F, Rugulies R. Paid care work and depression: a longitudinal study of antidepressant treatment in female eldercare workers before and after entering their profession. Depress Anxiety. 2012;29:605–13.
Cooper SL, Carleton HL, Chamberlain SA, Cummings GG, Bambrick W, Estabrooks CA. Burnout in the nursing home health care aide: a systematic review. Burn Res. 2016;3:76–87.
Geiger-brown J, Muntaner C, Lipscomb J, Trinkoff A. Demanding work schedules and mental health in nursing assistants working in nursing homes. Work Stress. 2004;18:292–304.
Zhang Y, Punnett L, Mawn B, Gore R. Working conditions and mental health of nursing staff in nursing homes. Issues Ment Health Nurs. 2016;37:485–92.
Liang YW, Hsieh Y, Lin YH, Chen WY. The impact of job stressors on health-related quality of life of nursing assistants in long-term care settings. Geriatr Nurs. 2014;35:114–9.
Geneen LJ, Moore RA, Clarke C, Martin D, Colvin LA, Smith BH. Physical activity and exercise for chronic pain in adults: an overview of Cochrane reviews. Cochrane Database Syst Rev. 2017;1:CD011279.
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54:79–86.
Rice D, Nijs J, Kosek E, Wideman T, Hasenbring MI, Koltyn K, et al. Exercise-induced hypoalgesia in pain-free and chronic pain populations: state of the art and future directions. J Pain. 2019;20:1249–66.
Vaegter HB, Jones MD. Exercise-induced hypoalgesia after acute and regular exercise: experimental and clinical manifestations and possible mechanisms in individuals with and without pain. Pain Rep. 2020;5:e823.
Seron P, Oliveros MJ, Gutierrez-Arias R, Fuentes-Aspe R, Torres-Castro RC, Merino-Osorio C, et al. Effectiveness of telerehabilitation in physical therapy: a rapid overview. Phys Ther. 2021;101:1–18.
Joseph RP, Durant NH, Benitez TJ, Pekmezi DW. Internet-based physical activity interventions. Am J Lifestyle Med. 2014;8:42–68.
Grona SL, Bath B, Busch A, Rotter T, Trask C, Harrison E, et al. Use of videoconferencing for physical therapy in people with musculoskeletal conditions: a systematic review. J Telemed Telecare. 2018;24:341–55.
Turolla A, Rossettini G, Viceconti A, Palese A, Geri T. Musculoskeletal physical therapy during the covid-19 pandemic: is telerehabilitation the answer? Phys Ther. 2020;100:1260–4.
Gao Z, Wang R. Application of e-health programs in physical activity and health promotion. J Sport Health Sci. 2022;11:131–2.
Polkey MI, Qiu ZH, Zhou L, Zhu MD, Wu YX, Chen YY, et al. Tai Chi and pulmonary rehabilitation compared for treatment-naive patients with COPD: a randomized controlled trial. Chest. 2018;153:1116–24.
Elder AJS, Scott WS, Kluge MA, Elder CL. CyberEx internet-based group exercise for rural older adults: a pilot study. Act Adapt Aging. 2016;40:107–24.
Brouwer W, Kroeze W, Crutzen R, de Nooijer J, de Vries NK, Brug J, et al. Which intervention characteristics are related to more exposure to internet-delivered healthy lifestyle promotion interventions? A systematic review. J Med Internet Res. 2011;13:e2.
Burke SM, Carron AV, Eys MA, Ntoumanis N, Estabrooks PA. Group versus individual approach? A meta-analysis of the effectiveness of interventions to promote physical activity. Sport Exer Psy Review. 2006;2:19–35.
Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med. 2013;158:200–7.
Boutron I, Altman DG, Moher D, Schulz KF, Ravaud P, CONSORT NPT Group. CONSORT statement for randomized trials of nonpharmacologic treatments: a 2017 update and a CONSORT extension for nonpharmacologic trial abstracts. Ann Intern Med. 2017;167:40–7.
Riebe DE, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal ME, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47:2473–9.
Espin A, Latorre U, Esain I, Bidaurrazaga-Letona I, Sayas A, Irazusta J. Relación del estado psicoafectivo y la condición física con la capacidad de trabajo y el desempeño laboral en auxiliares del servicio de ayuda a domicilio. In: IX congreso internacional de salud laboral y prevención de riesgos. 2022.
Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Br Med J. 2014;348:g1687.
Borg G. A category scale with ratio properties for intermodal and interindividual comparisons. In: Psychophysical judgment and the process of perception. 1982. p. 25–34.
Jakobsen MD, Sundstrup E, Brandt M, Kristensen AZ, Jay K, Stelter R, et al. Effect of workplace- versus home-based physical exercise on pain in healthcare workers: study protocol for a single blinded cluster randomized controlled trial. BMC Musculoskelet Disord. 2014;15:119.
Hawley-Hague H, Horne M, Skelton DA, Todd C. Review of how we should define (and measure) adherence in studies examining older adults’ participation in exercise classes. BMJ Open. 2016;6:e011560.
Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addiction. 1993;88:791–804.
Palipudi KM, Morton J, Hsia J, Andes L, Asma S, Talley B, et al. Methodology of the global adult tobacco survey - 2008–2010. Glob Health Promot. 2016;23:3–23.
Jackson AW, Morrow JR Jr, Bowles HR, FitzGerald SJ, Blair SN. Construct validity evidence for single-response items to estimate physical activity levels in large sample studies. Res Q Exerc Sport. 2007;78:24–31.
Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14:798–804.
Lyubomirsky S, Lepper HS. A measure of subjective happiness: preliminary reliability and construct validation. Soc Indic Res. 1999;46:137–55.
Goldberg D, Bridges K, Duncan-Jones P, Grayson D. Detecting anxiety and depression in general medical settings. BMJ. 1988;297:897–9.
Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory. 3rd ed. Lanham: Scarecrow Education; 1997.
Snyder E, Cai B, DeMuro C, Morrison MF, Ball W. A new single-item sleep quality scale: results of psychometric evaluation in patients with chronic primary insomnia and depression. J Clin Sleep Med. 2018;14:1849–57.
Szende A, Oppe M, Devlin N. EQ-5d value sets: inventory, comparative review and user guide. New York: Springer; 2006.
El Fassi M, Bocquet V, Majery N, Lair ML, Couffignal S, Mairiaux P. Work ability assessment in a worker population: comparison and determinants of work ability index and work ability score. BMC Public Health. 2013;13:305.
Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The World Health Organization health and work performance questionnaire (HPQ). J Occup Environ Med. 2003;45:156–74.
Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990;16:55–8.
Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:85–94.
American College of Sports Medicine (ACSM). ACSM’s guidelines for exercise testing and prescription. 10th ed. Alphen aan den Rijn: Wolters Kluwer; 2018.
Ito T, Shirado O, Suzuki H, Takahashi M, Kaneda K, Strax TE. Lumbar trunk muscle endurance testing: an inexpensive alternative to a machine for evaluation. Arch Phys Med Rehabil. 1996;77:75–9.
Espin A, García-García J, Latorre Erezuma U, Aiestaran M, Irazusta J, Rodriguez-Larrad A. Videoconference-based physical performance tests: reliability and feasibility study. Int J Environ Res Public Health. 2022;19:7109.
Holtermann A, Hansen JV, Burr H, Søgaard K. Prognostic factors for long-term sickness absence among employees with neck-shoulder and low-back pain. Scand J Work Environ Health. 2010;36:34–41.
Rodriguez-Larrad A, Espin A, Bidaurrazaga-Letona I, Esain I, Mujika I, Arizaga N, et al. Psycho-affective state and quality of life of female caregivers working in a long-term nursing home are related to practice regular physical activity. In: 9th International Association of Gerontology and Geriatrics European Region Congress. 2019.
Bakeman R. Recommended effect size statistics for repeated measures designs. Behav Res Methods. 2005;37:379–84.
Bonin-Guillaume S, Durand AC, Yahi F, Curiel-Berruyer M, Lacroix O, Cretel E. Predictive factors for early unplanned rehospitalization of older adults after an ED visit: role of the caregiver burden. Aging Clin Exp Res. 2015;27:883–91.
Andersen LN, Juul-Kristensen B, Roessler KK, Herborg LG, Sørensen TL, Søgaard K. Efficacy of “tailored physical activity” on reducing sickness absence among health care workers: a 3-months randomised controlled trial. Man Ther. 2015;20:666–71.
Christensen JR, Overgaard K, Hansen K, Søgaard K, Holtermann A. Effects on presenteeism and absenteeism from a 1-year workplace randomized controlled trial among health care workers. J Occup Environ Med. 2013;55:1186–90.
Gundewall B, Liljeqvist M, Hansson T. Primary prevention of back symptoms and absence from work. A prospective randomized study among hospital employees. Spine. 1993;18:587–94.
Suni JH, Kolu P, Tokola K, Raitanen J, Rinne M, Taulaniemi A, et al. Effectiveness and cost-effectiveness of neuromuscular exercise and back care counseling in female healthcare workers with recurrent non-specific low back pain: a blinded four-arm randomized controlled trial. BMC Public Health. 2018;18:1376.
World Health Organization (WHO). Global strategy and action plan on ageing and health. 2017.
Acknowledgements
We would like to thank all the institutions that have previously allowed us to study the eldercare sector and have therefore made it possible to launch this project: Caser Residencial Betharram, Fundación Aspaldiko, Grupo Servicios Sociales Integrados, IMQ Igurco, and Grupo Colisée.
Funding
This work is funded by the Basque Government (IT1538-22 and PRE_2021_2_0056) and the University of the Basque Country (GIU20/06). The funders played no role in the design, conduct, or reporting of this study.
Author information
Authors and Affiliations
Contributions
AE, JI and ARL designed the study and wrote the manuscript. AE coordinates the intervention. JI and ARL manage the project, obtained funding and will analyze data. ISC, AML and VGT recruited participants and provided facilities, and are helping with data collection. All authors read and approved the final manuscript.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee for Research Involving Human Beings of the University of the Basque Country (M10/2019/200MR2), and all participants will sign an informed written consent form before enrolling in the study.
Consent for publication
Written informed consent for publication has been obtained from all the people in Figs. 2 and 3.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Espin, A., Irazusta, J., Segovia Celaya, I. et al. Effects of a videoconference-based therapeutic exercise intervention on the musculoskeletal pain of eldercare workers: protocol for the ReViEEW randomized controlled trial. BMC Musculoskelet Disord 24, 463 (2023). https://doi.org/10.1186/s12891-023-06584-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06584-7