Abstract
Background
Medial meniscal posterior root tear (MMPRTs) is a common lesion of the knee joint, and repair surgery is a well-established treatment option. However, patients with obvious varus alignment are at an increased risk for MMPRT and can suffer from a greater degree of medial meniscus extrusion, which leads to the development of osteoarthritis following repair. The efficacy of high tibial osteotomy (HTO) as a means of correcting this malformation, and its potential benefits for MMPRT repair, remains unclear.
Purpose
To explore whether HTO influenced the outcome of MMPRT repair in clinical scores and radiological findings.
Study design
Systematic review.
Methods
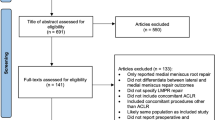
According to the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines, we searched PubMed, Embase, Web of Science, and the Cochrane Library databases for studies reporting the outcomes of MMPRT repair and extracted data about characteristics of patients, clinical functional scores and radiologic outcomes. One reviewer extracted the data and 2 reviewers assessed the risk of bias and performed a synthesis of the evidence. Articles were eligible if they reported the results of MMPRT repair with exact mechanical axis (registered in the International Prospective Register of Systematic Reviews, CRD42021292057).
Results
Fifteen studies with 625 cases of high methodological quality were identified. Eleven studies were assigned to the MMPRT repair group (M) with 478 cases performing MMPRT repair only, and others belonged to the MMPRT repair and HTO group (M and T) performing HTO and MMPRT repair. Most of the studies had significantly improved clinical outcome scores, especially in M groups. And the radiologic outcomes showed that the osteoarthritis deteriorated in both groups with similar degree in about 2-year follow-up.
Conclusion
HTO is a useful supplement in treating MMPRT patients with severe osteoarthritis and the clinical and radiological outcomes were similar with MMPRT repair alone. Which would be better for patients’ prognosis generally, performing MMPRT repair alone or a combination of HTO and MMPRT repair, was still controversial. We suggested taking K-L grade into account. Large-scale randomized control studies were called for in the future to help make better clinical decisions.
Level of evidence
III
Similar content being viewed by others

Introduction
The meniscal root tear is an avulsion injury or radial tear located within 1 cm of the meniscus root attachment [1], with the most common being the medial meniscal posterior root tear (MMPRT) first reported by Pagnani et al. [2]. This type of tear destroys the hoop construction of the meniscus and can have a long-term, detrimental impact on joint stresses and cartilage degeneration. Therefore, functional restoration of this injury is of utmost importance.
Various treatment options for MMPRT repair have been complemented, including non-operative treatment, partial meniscectomy, and MMPRT repair [3]. Biomechanical studies have confirmed that MMPRT repair can reverse the high contact pressure of the tibiofemoral joint [4, 5]. Clinical research has consistently concluded that MMPRT repair can delay the onset of osteoarthritis and the need for knee arthroplasty, when compared to non-operative and partial meniscectomy [6, 7]. However, when there is a varus abnormality and the mechanical axis of the lower limb deviates significantly from the normal range, MMPRT repair alone may not be sufficient. In such cases, high tibial osteotomy (HTO) can be used to correct lower limb alignment and reduce the burden on the medial meniscus [8]. While the effects of combining these surgeries have been studied [9], further research is needed to definitively determine the efficacy of this approach.
Our purpose was to investigate whether high tibial osteotomy (HTO) influences the outcome of medial meniscus posterior root tear (MMPRT) repair in terms of clinical scores and radiological findings. We hypothesized that the repair of MMPRT after HTO for patients with varus alignment could lead to better results than those with normal alignment without HTO.
Methods
Searching strategy
The protocol of this review was registered in the International Prospective Registry of Systematic Reviews (CRD42021292057). Research of PubMed, Embase, Web of Science, and Cochrane Library databases was performed on March 30th, 2023 with the terms ((Medial meniscus[Title/Abstract]) OR (medial meniscal[Title/Abstract]) AND ([Root tear] OR [Root tears] OR [posterior root tear] OR [posterior root tears] OR [posterior horn tear] OR [posterior horn tears] OR [posterior horn root tear] OR [posterior horn root tears] OR [avulsion]) AND [repair]).
Eligibility criteria
The inclusion criteria were as follows: (1) randomized controlled trials, observational cohort studies, and case-control studies (Level of Evidence I, II, or III); (2) Patients with medial meniscus posterior root tear (as diagnosed by a clinician or using any recognized diagnostic criteria) who underwent MMPRT repair. The exclusion criteria were as follows: (1) Patients underwent combined knee surgeries: combined osteotomy surgery, combined ligament surgery, combined cartilage restoration surgery, and combined lateral meniscal repair surgery; (2) Patients suffering from MMPRT caused by acute injuries; (3) Patients with missing information on neural or varus alignment; (4) Patients with follow-up less than 1.5 years.
Any researches that failed to meet the eligibility criteria were excluded. If data of multiple literature come from the same patient population, the article with the longest follow-ups was reserved.
Data extraction and quality assessment
Date from included studies was extracted by two reviewers. Any controversy was resolved by further discussion with the corresponding author. The extraction included the following: (1) the basic characteristics of included studies (author, publication date, study design and duration of follow-up); (2) the details of surgeries conducted (MMPRT repair or MMPRT repair with HTO); (3) the details of radiological outcomes (IKDC, Lysholm, VAS, HSS, and Tegner activity scale, K-L grade, mechanical axis, medial joint space, meniscal extrusion, and healing status of medial meniscus). In our research, Newcastle-Ottawa Scale (NOS) was used to assess quality for cohort study.
Statistical anaylsis
The data analysis was conducted using RevMan Manager 5.4 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2022). Using the same format, two reviewers independently collected data and crosschecked the results. Disagreements were discussed with the corresponding author and reached consensus in order to ensure accuracy. Odds ratio (OR) with 95% confidence interval (CI) was calculated for dichotomous while mean difference (MD) with corresponding 95% CI was calculated for continuous outcomes.
Results
Finally, there were 11 papers [7, 10,11,12,13,14,15,16,17,18,19] in MMPRT repair group (M) and 4 papers [9, 20,21,22] in MMPRT repair + HTO group (M and T) meeting the criteria (Fig. 1). 80.0% of these studies had a level of evidence III, while 2 studies [13, 17] (13.3%) were of level IV and 1 study [9] (6.7%) was of level II. The number of knees in total was 625 (478 in M group versus 147 in M and T group). The sex ratio (male/female) was 108/474 (85/349 in M group versus 23/125 in M and T group). The mean age of all patients was 56.2 (56.8 in M group versus 56.0 in M and T group). The mean follow-up time ranged from 16.6 months [18, 23,24,25] to 125.9 months [7]. The quality of each article was estimated by Newcastle-Ottawa Scale (NOS), and all 15 articles were no less than 7 points. The detailed information could be seen in Table 1.
The functional scores including IKDC, Lysholm, VAS, HSS, and Tegner activity scale were summed up in Table 2. Most results were significantly different between pre-operation and post-operation. Mean pre-operation IKDC score ranged from 36.3 [18, 23] to 57.9 [10], while from 55.5 [19] to 92.6 [10] for post-operation. Moon et al. [19] didn’t come out with different results, because they just followed up for 2 years, which may be short to see the difference. Only Lee et al. [20] recorded a pre- and post-operative IKDC score in M and T group, but they did not make a statistical comparison. In M group, mean pre-operation Lysholm score ranged from 51.3 [19, 24] to 58.1 [18, 25], while from 72.0 [19] to 92.9 [10] for post-operation. Ke et al. [9] and Lee et al. [20] reported this score both pre- and post-operation, but neither compared directly. Only 2 [18, 19] studies in M group reported VAS scores, and 1 [18] of them got better after the operation. There was only 1 study in each group reporting HSS score. One [10] in M group significantly improved after the operation, while another [9] in M and T group didn’t. The Tegner activity scale was reported in 4 (36.4%) articles of M group and 1 (25.0%) article of M and T group. Most results [11, 12, 18] in M group were significant, while the one [20] in M and T group didn’t compare.
The radiological outcomes composed of K-L grade, mechanical axis, medial joint space, meniscal extrusion, and healing status of medial meniscus were shown in Table 3. Four articles [12,13,14] had significant improvements in K-L grade after repair surgery, while others didn’t compare directly or had no significant difference. The distribution of patients with different K-L grades with about 2-year follow-up was shown in Fig. 2 [9,10,11, 17, 20, 21]. Neither group made significant progress although the M and T group had a larger mechanical axis before surgery than M group, which could attribute to the selection bias brought by indication of HTO. There was no obvious difference in medial joint space between the 2 groups, except Chung et al. [12] got significantly narrower results. The pre- and post-operation meniscal extrusions were mentioned in 3 [10, 15, 16] studies in M group and 2 [9, 21] in M and T group. In addition, 5 studies just reported pre- or post-operation data. The repair operation tended to decrease meniscal extrusion, but the sample was too small. The healing status of menisci could be seen in 6 articles, while Lee et al. [20] reported different classification methods from others.
Discussion
The findings of this systematic review suggest that the outcomes of MMPRT repair can be excellent, regardless of whether HTO is performed. Furthermore, the K-L grade progression at two-year follow-up was found to be comparable between the M and T and HTO groups, even though the pre-operative osteoarthritis in the M and T group was more severe.
From the perspective of clinical outcomes, there was no difference between MMPRT repair only and combination with HTO. Multiple reviews reported similar results with MMPRT repair only: Edwards et al. [26] reported an improvement of IKDC from 43.9 to 75.7 and Lysholm from 54.8 to 85.1 at a mean follow-up of 34 months; Chang et al. [27] reported that at midterm follow-up of 44 months, IKDC improved from 42.3 to 71.4, Lysholm from 53.4 to 84.1, HSS from 57.6 to 91.8, and Tegner activity scale from 2.8 to 3.8; and Krivicich et al. [28] reported a long-term follow-up of 64.8 months, with an IKDC score of 74.1. Kyun-Ho et al. [29] also compared the difference in HTO with or without MMPRT repair, finding no significant difference between groups in Lysholm and WOMAC, although the HTO with MMPRT repair group still had a higher mean Lysholm score. In our review, most articles in the MMPRT repair only (M) group had significantly improved Lysholm scores, while the improvement was not significant in the combination (M and T) group. However, the baseline Lysholm scores were worse in the M and T group, indicating that this difference was not an advantage of the M group.
The results of K-L grade supported the potential relief of progression of osteoarthritis through the repair of MMPRT. Moon et al. [30] documented that pullout repair of MMPRT improved clinical outcomes significantly. However, there were still 3 out of 31 patients having chondral lesions after the surgery, as well as meniscus extrusion progression being related to preoperative meniscus extrusion. Contrarily, Krych et al. [31] reported that 52 patients with MMPRT receiving non-operative therapy resulted in 31% of patients undergoing total knee arthroplasty (TKA) at a mean of 30 months after diagnosis, with K-L grade and arthritis becoming more severe with time, and 87% of patients failing in the end. Despite this, the benefit of surgical repair was still disputed. Masuda et al. [32] found that medial meniscus posterior extrusion increased when the knee flexed to 90 degrees in MMPRT, and Hopkins et al. [33] reported a high portion of patients having K-L progression after pullout repair. Additionally, it is unclear if the combination of MMPRT repair and HTO is more effective than either treatment alone. Kim et al. [34] concluded that HTO could yield similar results in both the intact meniscus group and the MMPRT group. Thus, more convincing studies are required to elucidate the functions of MMPRT repair and HTO.
The potential advantage of HTO was to correct the lower limb mechanical axis, which was essential for normal biomechanical functions. Moon et al. [30] confirmed that patients with varus alignment of > 5° had poorer results than those with varus alignment of < 5°. Theoretically, HTO could correct the malignment of the lower limb, thus improving the stress distribution on the meniscus and accelerating its healing. Chung et al. [35] observed 37 MMPRT patients who underwent pullout repair for more than 10 years, 8 of whom underwent TKA. Compared to the others, these 8 had greater varus alignment degrees, larger portions, and more progression of meniscus extrusion values. They suggested that 5 degrees of varus and 0.7 mm differences in meniscus extrusion values between preoperative and 1-year postoperative values could be used as the cutoff values to predict failure of MMPRT repair. However, the clinical outcomes in more recent studies challenge this hypothesis. Ridley et al. [36] compared the outcomes of MMPRT patients, divided by whether concomitant HTO was performed and varus was greater than 5 degrees. They found that patients with HTO had worse outcomes, regardless of alignment contrary to the hypothesis. This suggests that the effect of HTO is unclear and the preoperative varus degree plays an important role, with 5 degrees not being a reliable predictor. In our results, patients’ K-L grades in M and T group were mainly concentrated on 3. A multicenter cohort study revealed that the K-L 2 grade and 3 grade had totally different cartilage morphologies [37]. Thus, we suggest taking K-L grade into account when distinguishing high-risk patients and deciding whether or not to do HTO, which has been taken into account in some articles [20].
Noticeably, the potential innovation of combining MMPRT with combined tibial surgeries might provide further benefits for patients with mechanical malalignment. Chiba et al. reported that tibial condylar valgus osteotomy (TCVO) can improve pain and activities of daily living, along with valgus correction of the lower extremity and stabilization of the femorotibial joint in advanced medial knee osteoarthritis [38]. It’s indications, detailed surgical techniques, and outcomes were also reported by Capella et al. [39]. This opens up the possibility of further exploring the clinical efficacy of combining TCVO with MMPRT and assessing if similar outcomes to those found in this study can be replicated in those patients.
This article had several limitations. Firstly, the heterogeneity of study procedures resulted in outcomes that could not be directly aggregated, making the analysis complex. Secondly, there was a lack of long-term studies, with most studies (83.3%) having a follow-up period of less than 5 years, preventing us from making conclusions about long-term prognosis. Thirdly, the majority of studies were retrospective and non-randomized comparative studies, introducing selection bias into the conclusions. Nevertheless, this article was the first to examine the effect of HTO on the results of MMPRT repair in terms of lower limb alignment. Although there were several limitations, this article firstly reviewed and compared the outcomes of MMPRT repair with and without HTO, which provided evidence for clinical decision-making. To draw more reliable conclusions, higher evidence studies such as randomized control trials and prospective cohort studies are needed in the future.
Conclusion
The use of HTO as a supplement in treating MMPRT patients with severe osteoarthritis has been found to yield similar clinical and radiological outcomes to MMPRT repair alone. Nevertheless, it is still controversial as to which of the two treatments is better for patients’ prognosis. It is suggested to take K-L grade into account when choosing the most suitable treatment. To make more informed clinical decisions, large-scale randomized control studies should be conducted in the future.
Availability of data and materials
All data generated or analyzed during this study are included in this manuscript.
Abbreviations
- MMPRT:
-
medial meniscal posterior root tear
- HTO:
-
High tibial osteotomy
- NOS:
-
Newcastle-Ottawa Scale
- SD:
-
Standard deviation
- K-L:
-
Kellgren-Lawrence
- IKDC:
-
International Knee Documentation Committee
- K-L:
-
Kellgren-Lawrence
- VAS:
-
Visual analogue scale
- HSS:
-
Hospital for Special Surgery
References
Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C, LaPrade RF. Meniscal Root tears: current concepts review. Arch Bone Jt Surg. 2018;6(4):250–9.
Pagnani MJ, Cooper DE, Warren RF. Extrusion of the medial meniscus. Arthroscopy. 1991;7(3):297–300.
Bhatia S, LaPrade CM, Ellman MB, LaPrade RF. Meniscal root tears: significance, diagnosis, and treatment. Am J Sports Med. 2014;42(12):3016–30.
Allaire R, Muriuki M, Gilbertson L, Harner CD. Biomechanical consequences of a tear of the posterior root of the medial meniscus. J Bone Joint Surg Am Volume. 2008;90A(9):1922–31.
Kim JG, Lee YS, Bae TS, Ha JK, Lee DH, Kim YJ, Ra HJ. Tibiofemoral contact mechanics following posterior root of medial meniscus tear, repair, meniscectomy, and allograft transplantation. Knee Surg Sports Traumatol Arthrosc. 2013;21(9):2121–5.
Bernard CD, Kennedy NI, Tagliero AJ, Camp CL, Saris DBF, Levy BA, Stuart MJ, Krych AJ. Medial Meniscus posterior Root tear treatment: a matched cohort comparison of Nonoperative Management, partial meniscectomy, and repair. Am J Sports Med. 2019;48(1):128–32.
Chung KS, Ha JK, Ra HJ, Yu WJ, Kim JG. Root Repair Versus partial meniscectomy for medial Meniscus posterior Root tears: comparison of long-term survivorship and clinical outcomes at Minimum 10-Year follow-up. Am J Sports Med. 2020;48(8):1937–44.
Nha KW, Lee YS, Hwang DH, Kwon JH, Chae DJ, Park YJ, Kim JI. Second-look arthroscopic findings after open-wedge high tibia osteotomy focusing on the posterior root tears of the medial meniscus. Arthroscopy. 2013;29(2):226–31.
Ke X, Qiu J, Chen S, Sun X, Wu F, Yang G, Zhang L. Concurrent arthroscopic meniscal repair during open-wedge high tibial osteotomy is not clinically beneficial for medial meniscus posterior root tears. Knee Surg Sports Traumatol Arthrosc. 2021;29(3):955–65.
Kim JH, Chung JH, Lee DH, Lee YS, Kim JR, Ryu KJ. Arthroscopic suture anchor repair versus pullout suture repair in posterior root tear of the medial meniscus: a prospective comparison study. Arthroscopy. 2011;27(12):1644–53.
Lee DW, Kim MK, Jang HS, Ha JK, Kim JG. Clinical and radiologic evaluation of arthroscopic medial Meniscus Root tear Refixation: comparison of the Modified Mason-Allen stitch and simple stitches. Arthroscopy. 2014;30(11):1439–46.
Chung KS, Ha JK, Yeom CH, Ra HJ, Jang HS, Choi SH, Kim JG. Comparison of clinical and radiologic results between partial meniscectomy and refixation of medial Meniscus posterior Root tears: a minimum 5-Year follow-up. Arthroscopy. 2015;31(10):1941–50.
Chung KS, Ha JK, Ra HJ, Lee HS, Lee DW, Park JH, Kim DH, Kim JG. Pullout fixation for medial meniscus posterior root tears: clinical results were not age-dependent, but osteoarthritis progressed. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):189–96.
Kim C-W, Lee C-R, Gwak H-C, Kim J-H, Park D-H, Kwon Y-U, Jung S-H. Clinical and radiologic outcomes of patients with lax Healing after Medial Meniscal Root Repair: comparison with Subtotal Meniscectomy. Arthroscopy. 2019;35(11):3079–86.
Hiranaka T, Furumatsu T, Masuda S, Okazaki Y, Okazaki Y, Kodama Y, Kamatsuki Y, Kajiki Y, Zhang X, Ozaki T. A repair technique using two simple stitches reduces the short-term postoperative medial meniscus extrusion after pullout repair for medial meniscus posterior root tear. Eur J Orthop Surg Traumatol. 2020;30(5):901–8.
Ulku TK, Kaya A, Kocaoglu B. Suture configuration techniques have no effect on mid-term clinical outcomes of arthroscopic meniscus root repairs. Knee. 2020;27(3):676–82.
Dzidzishvili L, Isabel Lopez-Torres I, Saez D, Manuel Arguello J, Calvo E. A comparison of the transtibial pullout technique and all-inside meniscal repair in medial meniscus posterior root tear: prognostic factors and midterm clinical outcomes. J Orthop. 2021;26:130–4.
Furumatsu T, Hiranaka T, Okazaki Y, Kintaka K, Kodama Y, Kamatsuki Y, Ozaki T. Medial meniscus posterior root repairs: a comparison among three surgical techniques in short-term clinical outcomes and arthroscopic meniscal healing scores. J Orthop sci. 2021;27(1):181–9.
Moon H-S, Choi C-H, Yoo J-H, Jung M, Lee T-H, Jeon B-H, Kim S-H. Mild to moderate Varus Alignment in Relation to Surgical repair of a Medial Meniscus Root tear: a matched-cohort controlled Study with 2 years of follow-up. Am J Sports Med. 2021;49(4):1005–16.
Lee DW, Lee SH, Kim JG. Outcomes of medial meniscal posterior Root Repair during Proximal Tibial Osteotomy: is Root Repair Beneficial? Arthroscopy. 2020;36(9):2466–75.
Lee OS, Lee SH, Lee YS. Comparison of the Radiologic, Arthroscopic, and clinical outcomes between repaired versus unrepaired medial Meniscus posterior Horn Root tear during Open Wedge High Tibial Osteotomy. J Knee Surg. 2021;34(1):57–66.
Suh DW, Yeo WJ, Han SB, So SY, Kyung BS. Simple medial Meniscus posterior Horn Root Repair using an All-Inside Meniscal Repair device combined with high tibial osteotomy to maintain Joint-Space Width in a patient with a repairable tear. Indian J Orthop. 2021;55(2):397–404.
Furumatsu T, Okazaki Y, Kodama Y, Okazaki Y, Masuda S, Kamatsuki Y, Takihira S, Hiranaka T, Yamawaki T, Ozaki T. Pullout repair using modified Mason-Allen suture induces better meniscal healing and superior clinical outcomes: a comparison between two surgical methods. Knee. 2019;26(3):653–9.
Yanagisawa S, Kimura M, Hagiwara K, Ogoshi A. Association between postoperative meniscal extrusion and clinical outcomes of the pullout fixation technique for medial meniscus posterior root tear. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2020;21:27–31.
Okazaki Y, Furumatsu T, Hiranaka T, Kodama Y, Kamatsuki Y, Kintaka K, Ozaki T. Two simple stitches for medial meniscus posterior root repair prevents the progression of meniscal extrusion and reduces intrameniscal signal intensity better than modified Mason-Allen sutures. Eur J Orthop Surg Traumatol. 2021;31(6):1005–13.
Edwards C, Goldman BH, Turley J, Richey B, Deal MJ, Kalbac D. Outcomes after Surgical Repair of Medial Meniscal Root tears: a review. J Knee Surg. 2021;34(14):1599–602.
Chang PS, Radtke L, Ward P, Brophy RH. Midterm outcomes of posterior medial Meniscus Root tear repair: a systematic review. Am J Sports Med. 2022;50(2):545–53.
Krivicich LM, Kunze KN, Parvaresh KC, Jan K, DeVinney A, Vadhera A, LaPrade RF, Chahla J. Comparison of long-term Radiographic Outcomes and Rate and Time for Conversion to total knee arthroplasty between repair and meniscectomy for medial Meniscus posterior Root tears: a systematic review and Meta-analysis. Am J Sports Med. 2021:3635465211017514.
Kyun-Ho S, Hyun-Jae R, Ki-Mo J, Seung-Beom H. Effect of concurrent repair of medial meniscal posterior root tears during high tibial osteotomy for medial osteoarthritis during short-term follow-up: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22(1):623.
Moon H-K, Koh Y-G, Kim Y-C, Park Y-S, Jo S-B, Kwon S-K. Prognostic factors of Arthroscopic pull-out repair for a posterior Root tear of the medial Meniscus. Am J Sports Med. 2012;40(5):1138–43.
Krych AJ, Reardon PJ, Johnson NR, Mohan R, Peter L, Levy BA, Stuart MJ. Non-operative management of medial meniscus posterior horn root tears is associated with worsening arthritis and poor clinical outcome at 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):383–9.
Masuda S, Furumatsu T, Okazaki Y, Kodama Y, Hino T, Kamatsuki Y, Miyazawa S, Ozaki T. Medial meniscus posterior root tear induces pathological posterior extrusion of the meniscus in the knee-flexed position: an open magnetic resonance imaging analysis. Orthop Traumatol Surg Res. 2018;104(4):485–9.
Hopkins NDM, Lawrie S. Improvement of clinical and radiological outcomes of root repair patients with advanced articular cartilage degeneration and osteoarthritis. J Experimental Orthop. 2021;8(1):82.
Kim KI, Bae JK, Jeon SW, Kim GB. Medial Meniscus posterior Root tear does not affect the outcome of Medial Open-Wedge High Tibial Osteotomy. J Arthroplasty. 2021;36(2):423–8.
Chung KS, Ha JK, Ra HJ, Kim JG. Preoperative varus alignment and postoperative meniscus extrusion are the main long-term predictive factors of clinical failure of meniscal root repair. Knee Surg Sports Traumatol Arthrosc. 2021;29(12):4122–30.
Ridley TJ, Ruzbarsky JJ, Dornan GJ, Woolson TE, Poulton RT, LaPrade RF, Provencher MT, Vidal AF. Minimum 2-Year clinical outcomes of Medial Meniscus Root tears in relation to coronal alignment. Am J Sports Med. 2022;50(5):1254–60.
Roemer FW, Felson DT, Stefanik JJ, Rabasa G, Wang N, Crema MD, Neogi T, Nevitt MC, Torner J, Lewis CE, et al. Heterogeneity of cartilage damage in Kellgren and Lawrence grade 2 and 3 knees: the MOST study. Osteoarthritis Cartilage. 2022;30(5):714–23.
Chiba K, Yonekura A, Miyamoto T, Osaki M, Chiba G. Tibial condylar valgus osteotomy (TCVO) for osteoarthritis of the knee: 5-year clinical and radiological results. Arch Orthop Trauma Surg. 2017;137(3):303–10.
Capella M, Risitano S, Sabatini L, Faccenda C, Barberis L, Camazzola D, Bosco F, Giustra F, Massè A. Tibial condylar valgus osteotomy for the treatment of intra-articular varus deformity of the knee. Ann Joint. 2022;7:37.
Acknowledgements
We thank Xiaoqing Hu for her help in statistical analysis of this study.
Funding
This manuscript was supported by National Natural Science Foundation of China (grant number 81802153).
Author information
Authors and Affiliations
Contributions
QY.M and Y.M conceived and designed the study. HL.W, YT.G, JW.Z and LY.X collected and analyzed the data. HL.W and Q.M wrote the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, H., Man, Q., Gao, Y. et al. The efficacy of medial meniscal posterior Root tear Repair with or without high tibial osteotomy: a systematic review. BMC Musculoskelet Disord 24, 464 (2023). https://doi.org/10.1186/s12891-023-06520-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06520-9