Abstract
Background
Long-term consequences of posterior cruciate ligament (PCL) injury such as persistent posterior tibial translation and risk of osteoarthritis development are unclear. Additionally, little data is available describing the natural history of structural morphology of the ruptured PCL. The purpose of the study was to determine the long-term outcome after non-operatively treated PCL injury.
Methods
Over 6-years, all acute knee injuries were documented by subacute MRI (median 8 days [5–15, 25th − 75th percentile] from injury to MRI). Twenty-six patients with acute PCL injury were identified of whom 18 (69%) participated in the long-term follow-up after 11 years. Follow-up included radiographic posterior tibial translation (RPTT) determined using the Puddu axial radiograph. weight-bearing knee radiographs, MRI and KOOS (Knee injury and Osteoarthritis Outcome Score).
Results
On subacute MRI, 11 knees displayed total and 7 partial ruptures. At 11 (SD 1.9) years, the median RPTT was 3.7 mm (1.5–6.3, 25th − 75th percentile). Seven knees displayed radiographic osteoarthritis approximating Kellgren-Lawrence grade ≥ 2. All follow-up MRIs displayed continuity of the PCL. Patients with more severe RPTT (> 3.7 mm), had worse scores in the KOOS subscales for symptoms (mean difference 14.5, 95% CI 7–22), sport/recreation (30, 95% CI 0–65) and quality of life (25, 95% CI 13–57) than those with less severe RPTT (≤ 3.7 mm). This was also the case for the KOOS4 (22, 95% CI 9–34).
Conclusion
Acute PCL injuries treated non-surgically display a high degree of PCL continuity on MR images 11 years after injury. However, there is a large variation of posterior tibial translation with higher values being associated with poorer patient-reported outcomes.
Similar content being viewed by others
Background
Posterior cruciate ligament (PCL) rupture is a rare knee injury with an annual incidence of between 2 and 4 per 100 000 persons [1, 2]. Non-surgical treatment has been a well-accepted alternative to surgical reconstruction for many years, however, long term structural consequences are still unclear [3,4,5,6,7,8,9,10,11,12]. These include the continuity of the PCL itself as well as the risk of development of knee osteoarthritis (OA). Further, the relationship between persistent posterior tibial translation and long-term clinical outcomes is controversial. Some investigators have reported an association between greater laxity and worse outcome [8, 13] however, many have failed to demonstrate such an association [3, 10, 14,15,16]. One reason may be that the majority of studies are based on clinical stability tests rather than objective tibial translation measures derived from knee radiographs [17,18,19].
PCL injuries, including those with other concomitant ligament injury, have traditionally been treated with initial non-surgical management at Helsingborg hospital. Concomitant grade II and III collateral ligament injuries were, in addition prescribed a brace for 4–6 weeks. This study used a prospectively ascertained observational cohort of patients with acute knee injury with the aim of investigating radiographic posterior tibial translation (RPTT), frequency of radiographic OA, PCL continuity as visualized by magnetic resonance imaging (MRI) as well as patient-reported outcome measures 11 years after acute PCL rupture treated without surgery. An additional aim was to explore the potential relationship between RPTT and the other outcomes at follow-up. The hypotheses were that larger RPTT would be associated with poorer patient-reported outcomes and that the majority of PCLs would show continuity on follow-up MRI.
Materials and methods
Subjects
Between January 2002 and February 2008, a total of 1145 patients were consecutively registered after seeking care at either the emergency department or outpatient clinic at Helsingborg hospital due to acute knee trauma with hemarthrosis. If there was clinical suspicion of a fracture, the patient was referred for conventional radiography. Knees with fractures seen on conventional radiographs, apart from osteochondral and ligament avulsion fractures, were not eligible for the present study. All patients had their structural injuries determined by knee MRI at a median of 8 days (5–15, 25th − 75th percentile) after injury [1]. From this cohort a total of 33 patients with potential PCL injury were identified.
After thorough review of medical records, 7 patients did not meet the inclusion criteria and another 8 were lost-to-follow-up (Fig. 1). Follow-up was conducted between 2017 and 2018.
Medical records were assessed to determine the initial treatment and any registered subsequent injuries to the affected or contralateral knee.
Baseline knee MR imaging
Patients were examined with 1.0 or 1.5 Tesla MRI [1]. Images were assessed at baseline by musculoskeletal radiologists. MRI findings were classified and collected according to Khanna et al. [20]. PCL injuries were regarded as total ruptures unless a partial rupture was reported.
Follow-up radiographic examination
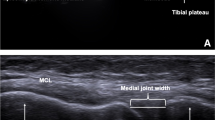
Three radiographic projections were obtained of both knees in all 17 patients who attended for examination (one patient completed only patient-reported outcomes). The anteroposterior projections were obtained in a weight-bearing position with the knee flexed 30° – 50° [21]. The Merchant view projection was obtained in standing with the knee flexed 40° – 60° [22]. RPTT was examined using the Puddu axial radiograph using the contralateral knee as the reference [17].
Radiographic assessment of images
Radiographic knee OA
Antero-posterior, lateral and Merchant view radiographs were classified for radiographic OA according to the OARSI-atlas in the tibiofemoral and patellofemoral joint [23] by a musculoskeletal radiologist. In agreement with previous publications the presence of radiographic OA was determined if any of the following criteria were fulfilled, approximating Kellgren-Lawrence grade 2 or worse [24, 25]:
-
joint space narrowing (JSN) of grade 2 or more.
-
the sum of the two marginal osteophyte grades from the same compartment ≥ 2.
-
grade 1 JSN in combination with a grade 1 osteophyte in the same compartment.
Radiographic posterior tibial translation (RPTT)
RPTT was quantified as the difference in posterior tibial translation between the affected and unaffected sides in mm on the Puddu axial radiograph [17]. Since two of the 17 patients who attended for radiographic follow-up had suffered a PCL injury to the contralateral knee after their original injury, RPTT measures were obtained from 15 individuals.
A low RPTT corresponds to little sagittal laxity whereas a high RPTT corresponds to large sagittal instability. For comparative analyses, those with RPTT at or below the median value were classified as having low RPTT and those above median as having high RPTT.
Continuity of the PCL at follow-up
Images were interpreted by a fellowship trained sports knee and shoulder surgeon (JSB). The PCL was defined as having continuity when low-intensity signals that represented the PCL were shown to be continuous from the femur to the tibia regardless of the shape and configuration [26, 27].
Patient reported outcome measures
Knee function and symptoms were evaluated using the Knee injury and Osteoarthritis Outcome Score (KOOS). The KOOS4 was used to measure the overall patient reported outcome. This is an average score of four of the five KOOS subscales (pain, symptoms, sports and recreation, and quality of life). It excludes the activities of daily living subscale to avoid a ceiling effect given that this group of patients are usually young and active [28, 29]. General health status was evaluated using the EQ-5D VAS. Activity level was assessed with the Tegner activity score and Activity Rating Scale (ARS) [30, 31].
Clinical examination
At long-term follow-up height and weight were recorded and range of motion and ligamentous stability were assessed. Valgus/varus stability was graded according to Fetto & Marshall [32]. Lachman was graded as per Hefti et al. [33]. Posterior drawer was graded according to Rubenstein et al. [34].
Statistical analysis
Microsoft excel (2016) and SPSS statistics (version 27) were used to analyse data. Comparisons of patient relevant outcome were evaluated using analysis of variance to produce means with 95% confidence intervals (CI’s). Differences between groups were evaluated using independent samples T-tests and Mann-Whitney U-tests and presented as the differences between means or medians (Lehmann- Hodges estimates) respectively with 95% CI´s. Intra- and inter-rater reliability for tibial translation were assessed using ICC.
Results
Cohort followed-up
Eighteen patients (15 men), with a mean age of 33 (SD 14.2) years at injury were followed-up at a mean of 11 (SD 1.9) years after acute PCL rupture (Table 1). The majority were injured during sporting activities (n = 13). Seven patients sustained partial and 11 total PCL ruptures. Nine patients had also suffered injury to other ligaments at the time of injury (Table 2). The characteristics of the cohort followed-up (n = 18) was similar to the cohort as a whole (n = 26) (Table 2).
Treatment and subsequent injuries
None of the patients followed-up were treated operatively for either PCL injury or collateral ligament injury however, 2 patients underwent a subsequent ACL reconstruction and 4 patients were treated with partial meniscal resection. Three of these 4 cases were related to meniscal injuries identified at the time of the subacute MRI.
None of the patients in the study were treated with a dedicated PCL brace however, patients with associated grade 2–3 collateral ligament injuries (n = 8) were treated in a hinged knee brace (0–90 degrees) for 4–6 weeks.
Two patients sustained a contralateral PCL rupture over the follow-up period. No other subsequent knee injuries to either knee were recorded in the cohort.
Outcomes in relation to RPTT and degree of ligament injury
Inter-rater reliability was determined by two assessors measuring RPTT for 14 patients. Intra-rater reliability was determined using re-assessment of radiographs from 14 patients 49 days apart. Intra class correlations (ICC) were excellent with 0.96 (95% CI 0.87–0.99) and 0.99 (95% CI 0.98-1.00) for inter- and intra-rater reliability respectively.
Median RPTT was 3.7 (25th-75th percentile 1.5–6.3) mm for the entire cohort (Table 1) with overall decreasing KOOS scores for those with higher RPTT (Fig. 2). Those with high RPTT (above median, n = 7) had lower KOOS scores in general, and results were statistically significantly worse for symptoms (mean difference 14.5, 95% CI 7–22), sport/recreation (median difference 30, 95% CI 0–65) and knee related quality of life (median difference 25, 95% CI 13–57) than those with low RPTT (at or below median, n = 8, Fig. 3). This was also the case for the KOOS4 (median difference 22, 95% CI 9–34). There were no corresponding statistically significant differences in the KOOS subscales for pain, or ADL, Eq. 5D VAS or for activity level as measured by the Tegner score and the Activity Rating Scale (data provided in additional data file).
Patients who had sustained a partial PCL rupture had a median RPTT of 2.1 (25th-75th percentile 1.1–3.5) mm whereas those who had sustained a total rupture had a median RPTT of 6.0 (25th-75th percentile 3.9–9.1) mm. The KOOS scores were generally lower in patients with total rupture but the differences were rather small and not statistically significantly different (Fig. 4). The other outcomes, Eq. 5D VAS, Tegner score or Activity Rating Scale showed a similar picture between the total rupture and partial rupture subgroups (data provided in additional data file).
There were no statistically significant differences in any of the outcome scores when comparing patients with isolated and combined ligament injuries (data provided in additional data file).
Radiographic OA
Seven patients had radiographic OA in one or more compartments of the injured knee. Five of these were in the high RPTT group. Three patients also had OA in the uninjured contralateral knee. Four patients showed signs of isolated patellofemoral OA, two of combined tibiofemoral and patellofemoral OA and one of isolated tibiofemoral OA.
Magnetic resonance imaging
Fourteen of 18 patients underwent an MRI of the index knee at follow-up. All 14 showed continuity of the PCL.
Discussion
The study suggests that larger RPTT at follow-up is associated with poorer patient-reported outcome. Seven patients displayed radiographic OA with patellofemoral OA being more prevalent than tibiofemoral. Interestingly all 14 knees with acute PCL rupture who underwent MRI follow-up displayed continuity of the PCL 11 years after the injury.
Despite the generally held belief that persistent posterior translation leads to a poorer outcome after PCL rupture this is one of very few studies confirming this notion at long-term follow-up. This may be due to the fact that many previous studies have based their estimation of tibial translation on clinical examination findings rather than objective radiographic measurement [3, 10, 14,15,16]. There are several methods of measuring RPTT in the literature. The Puddu method was chosen as this is reported to be reliable, less painful than stress radiography and can be carried out relatively quickly with standard radiology department equipment [35]. Studies have shown that PCL deficiency and the resultant instability leads to increased contact pressures particularly in the medial and patellofemoral compartments [36, 37]. This may explain to some degree the symptomatic and radiographic changes demonstrated in this study.
The ability of the PCL to heal has been documented previously [6, 38, 39] and this study adds further weight to this evidence.
The management of PCL injury remains controversial but in recent years brace treatment of acute injuries has gained increasing acceptance [6, 7, 38]. PCL specific braces aim to correct the posterior tibial translation allowing the PCL to heal with the knee in an appropriate position. Given that posterior tibial translation is associated with worse patient related outcome it would seem logical that a treatment that can minimise this phenomenon may improve results. It remains to be proven whether the best method of achieving this is through non-surgical brace treatment or reconstruction.
Limitations
Despite the study being based on a large cohort of 1145 knee-injured patients collected over a 6-year period there were only 26 patients with acute PCL ruptures and many of these had concomitant ligament injury. As non-operative treatment is utilised for all PCL ruptures, we were not able to compare outcome with a control group of surgically treated patients. The final cohort of 18 patients who attended follow-up included both those with partial and total PCL ruptures. The small sample only makes it possible to ascertain large differences between subgroups. Still, this is mostly a descriptive paper in character. While all the differences presented as statistically significant had p values < 0.05 the research group chose to present comparisons between groups using differences in means/medians and 95% CI´s in order to demonstrate the degree of uncertainty associated with the findings. PCL injury is rare and the study has for the first time performed a systematic follow up of a prospective cohort, including both patient-reported outcomes as well as imaging, 11 years after the injury.
Conclusions
Acute PCL injuries treated non-surgically, display PCL continuity on MR images 11 years after injury at a very high frequency. However, non-surgical treatment results in a large variation of posterior tibial translation with increased instability being associated with poorer self-reported outcomes.
Data availability
The datasets analysed during the current study are not publicly available due to ongoing research but are available from the corresponding author on reasonable request.
Abbreviations
- PCL:
-
posterior cruciate ligament
- OA:
-
osteoarthritis
- RPTT:
-
radiographic posterior tibial translation
- MRI:
-
magnetic resonance imaging
- ACL:
-
anterior cruciate ligament
- MCL:
-
medial collateral ligament
- LCL:
-
lateral collateral ligament
- JSN:
-
joint space narrowing
- ICC:
-
Intra class correlation
- KOOS:
-
Knee injury and Osteoarthritis Outcome Score
- ARS:
-
Activity Rating Scale
- CI:
-
Confidence interval
References
Olsson O, Isacsson A, Englund M, Frobell RB. Epidemiology of intra- and peri-articular structural injuries in traumatic knee joint hemarthrosis – data from 1145 consecutive knees with subacute MRI. Osteoarthr Cartil. 2016;24:1890–7.
Sanders TL, Pareek A, Barrett IJ, Kremers HM, Bryan AJ, Stuart MJ et al. Incidence and long-term follow-up of isolated posterior cruciate ligament tears. Knee Surgery, Sport Traumatol Arthrosc 2016 2510. 2016;25:3017–23.
Parolie JM, Bergfeld JA. Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med. 1986;14:35–8.
Fowler PJJ, Messieh SSS. Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med. 1987;15:553–7.
Torg JS, Barton TM, Pavlov H, Stine R. Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res. 1989;:208–16.
Jacobi M, Reischl N, Wahl P, Gautier E, Jakob RP. Acute isolated injury of the posterior cruciate ligament treated by a dynamic anterior drawer brace: a preliminary report. J Bone Joint Surg Br. 2010;92:1381–4.
Jung YB, Tae SK, Lee YS, Jung HJ, Nam CH, Park SJ. Active non-operative treatment of acute isolated posterior cruciate ligament injury with cylinder cast immobilization. Knee Surg Sports Traumatol Arthrosc. 2008;16:729–33.
Agolley D, Gabr A, Benjamin-Laing H, Haddad FS. Successful return to sports in athletes following non-operative management of acute isolated posterior cruciate ligament injuries medium-term follow-up. Bone Jt J. 2017;99B:774–8.
Wang SH, Chien WC, Chung CH, Wang YC, Lin LC, Pan RY. Long-term results of posterior cruciate ligament tear with or without reconstruction: a nationwide, population-based cohort study. PLoS ONE. 2018;13:e0205118.
Shelbourne KD, Clark M, Gray T. Minimum 10-year follow-up of patients after an acute, isolated posterior cruciate ligament injury treated nonoperatively. Am J Sports Med. 2013;41:1526–33.
Logan CA, Beaulieu-Jones BR, Sanchez G, Chahla J, Kennedy NI, Cinque ME, et al. Posterior cruciate ligament injuries of the knee at the National Football League combine: an imaging and epidemiology study. Arthrosc - J Arthrosc Relat Surg. 2018;34:681–6.
Winkler PW, Zsidai B, Wagala NN, Hughes JD, Horvath A, Senorski EH, et al. Evolving evidence in the treatment of primary and recurrent posterior cruciate ligament injuries, part 2: surgical techniques, outcomes and rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2021;29:682–93.
Boynton MD, Tietjens BR. Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med. 1996;24:306–10.
Patel DV, Allen AA, Warren RF, Wickiewicz TL, Simonian PT. The nonoperative treatment of acute, isolated (partial or complete) posterior cruciate ligament-deficient knees: an intermediate-term follow-up study. HSS J. 2007;3:137–46.
Shelbourne KD, Davis TJ, Patel DV. The natural history of Acute, isolated, nonoperatively treated posterior cruciate ligament injuries a prospective Study*. Am J Sports Med. 1999;27:276–83.
Dandy DJ, Pusey RJ. The long-term results of unrepaired tears of the posterior cruciate ligament. J Bone Joint Surg Br. 1982;64:92–4.
Puddu G, Gianni E, Chambat P, De Paulis F. The axial view in evaluating tibial translation in cases of insufficiency of the posterior cruciate ligament. Arthroscopy. 2000;16:217–20.
Stäubli HU, Jakob RP. Posterior instability of the knee near extension. A clinical and stress radiographic analysis of acute injuries of the posterior cruciate ligament. J Bone Joint Surg Br. 1990;72:225–30.
Schulz MS, Russe K, Lampakis G, Strobel MJ. Reliability of stress radiography for evaluation of posterior knee laxity. Am J Sports Med. 2005;33:502–6.
Khanna AJ, Cosgarea AJ, Mont MA, Andres BM, Domb BG, Evans PJ et al. Magnetic resonance imaging of the knee: Current techniques and spectrum of disease. J Bone Jt Surg - Ser A. 2001;83 SUPPL. 2 II:128–41.
Boegård TL, Rudling O, Petersson IF, Jonsson K. Joint space width of the tibiofemoral and of the patellofemoral joint in chronic knee pain with or without radiographic osteoarthritis: a 2-year follow-up. Osteoarthr Cartil. 2003;11:370–6.
Boegård T, Rudling O, Petersson IF, Sanfridsson J, Saxne T, Svensson B, et al. Joint-space width in the axial view of the patello-femoral joint. Acta radiol. 1998;39:24–31.
Altman RD, Gold GE, Doherty M, Sturmer T, Gunther KP, Altman RD, et al. Atlas of individual radiographic features in osteoarthritis, revised. Osteoarthr Cartil. 2007;15(Suppl A):A1–56.
Englund M, Lohmander LS. Patellofemoral osteoarthritis coexistent with tibiofemoral osteoarthritis in a meniscectomy population. Ann Rheum Dis. 2005;64:1721–6.
Englund M, Roos EM, Lohmander LS. Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum. 2003;48:2178–87.
Akisue T, Kurosaka M, Yoshiya S, Kuroda R, Mizuno K. Evaluation of healing of the injured posterior cruciate ligament: analysis of instability and magnetic resonance imaging. Arthroscopy. 2001;17:264–9.
Peterson DC, Thain LMF, Fowler PJ. Imaging of the Posterior Cruciate Ligament. Posterior Cruciate Ligament Injuries.Springer New York; 2001. 77–85.
Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for Acute Anterior Cruciate ligament tears. N Engl J Med. 2010;363:331–42.
Bergerson E, Persson K, Svantesson E, Horvath A, Olsson Wållgren J, Karlsson J, et al. Superior Outcome of Early ACL Reconstruction versus initial non-reconstructive treatment with late crossover to surgery: a study from the Swedish National knee ligament Registry. Am J Sports Med. 2022;50:896–903.
Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;:43–9.
Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29:213–8.
Fetto JF, Marshall JL. Medial collateral ligament injuries of the knee: a rationale for treatment. Clin Orthop Relat Res. 1978;:206–18.
Hefti E, Müller W, Jakob RP, Stäubli H-U. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sport Traumatol Arthrosc. 1993;1:226–34.
Rubinstein RA, Shelbourne KD, McCarroll JR, VanMeter CD, Rettig AC. The Accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med. 1994;22:550–7.
Jung TM, Reinhardt C, Scheffler SU, Weiler A. Stress radiography to measure posterior cruciate ligament insufficiency: a comparison of five different techniques. Knee Surgery, Sport Traumatol Arthrosc. 2006;14:1116–21.
Skyhar MJ, Warren RF, Ortiz GJ, Schwartz E, Otis JC. The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. J Bone Joint Surg Am. 1993;75:694–9.
Gill TJ, DeFrate LE, Wang C, Carey CT, Zayontz S, Zarins B, et al. The effect of posterior cruciate ligament reconstruction on patellofemoral contact pressures in the knee joint under simulated muscle loads. Am J Sports Med. 2004;32:109–15.
Ahn JH, Lee SH, Choi SH, Wang JH, Jang SW, Hwan Ahn J, et al. Evaluation of clinical and magnetic resonance imaging results after treatment with casting and bracing for the acutely injured posterior cruciate ligament. Arthrosc J Arthrosc Relat Surg. 2011;27:1679–87.
Shelbourne KD, Jennings RW, Vahey TN. Magnetic resonance imaging of posterior cruciate ligament injuries: assessment of healing. Am J Knee Surg. 1999;12:209–13.
Acknowledgements
Kerstin Åkesson Günther for co-ordinating patient follow-up.
Funding
Open access funding provided by Lund University. This work was supported by Stig and Ragna Gorthons foundation for medical research, and Governmental Funding of Clinical Research within National Health Service (ALF). The funding bodies had no role in the design of the study, collection, analysis, or interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
J.S.B: study design, data collection, data analysis, manuscript writing, corresponding author. K.M: study design, data collection, data analysis, manuscript writing. F.W.R: data analysis, manuscript writing. A.I: study design, manuscript writing. JK: data analysis, manuscript writing. R.F: study design, manuscript writing. O.O: study design, data analysis, manuscript writing. M.E: study design, data analysis, manuscript writing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from Lund university ethics committee. Informed consent was obtained from all participants. All methods were performed in accordance with relevant regulations and in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Brown, J.S., Mogianos, K., Roemer, F.W. et al. Clinical, patient-reported, radiographic and magnetic resonance imaging findings 11 years after acute posterior cruciate ligament injury treated non-surgically. BMC Musculoskelet Disord 24, 365 (2023). https://doi.org/10.1186/s12891-023-06480-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06480-0