Abstract
Background
Recently, some studies on the efficacy of the femoral neck system (FNS) in treating femoral neck fractures (FNFs) have been published. Therefore, a systematic review was performed to clarify the efficacy and safety of FNS versus cannulated screws (CS) for the treatment of FNFs.
Method
The PubMed, EMBASE, and Cochrane databases were systematically searched for studies comparing FNS and CS fixations in FNFs. Intraoperative indicators, postoperative clinical indicators, postoperative complications, and postoperative scores were compared between the implants.
Results
A total of eight studies were included in the study, involving 448 FNFs patients. The results showed that patients in FNS group were significantly lower than the CS group in the number of X-ray exposures (WMD = -10.16; 95% CI, -11.44 to -8.88; P < 0.001; I2 = 0%), fracture healing time (WMD = -1.54; 95% CI, -2.38 to -0.70; P < 0.001; I2 = 92%), length of femoral neck shortening (WMD = -2.01; 95% CI, -3.11 to -0.91; P < 0.001; I2 = 0%), femoral head necrosis (OR = 0.27; 95% CI, 0.08 to 0.83; P = 0.02; I2 = 0%), implant failure/cutout (OR = 0.28; 95% CI, 0.10 to 0.82; P = 0.02; I2 = 0%), and Visual Analog Scale Score (WMD = -1.27; 95% CI, -2.51 to -0.04; P = 0.04; I2 = 91%). And the Harris Score was significantly higher in the FNS group than in the CS group (WMD = 4.15; 95% CI, 1.00 to 7.30; P = 0.01; I2 = 89%).
Conclusions
Based on this meta-analysis, FNS shows better clinical efficacy and safety in treating FNFs compared to CS. However, due to the limited quality and number of included studies and the high heterogeneity of the meta-analysis; large samples and multicenter RCTs are needed to confirm this conclusion in the future.
Level of evidence
II, Systematic review and Meta-analysis.
Trial registration
PROSPERO CRD42021283646.
Similar content being viewed by others
Introduction
In clinical work, femoral neck fractures (FNFs) are a common fracture type. With rising life expectancy throughout the globe, it is estimated that the incidence of FNFs will increase from 1.7 million in 1990 to 6.3 million by 2050 [1]. It is a significant health problem that affects middle-aged and elderly people [2]. The cost of treatment is expensive, causing varying degrees of burden on families and society [3]. Internal fixation is a conventional surgical method for FNFs, especially in nondisplaced FNFs [4]. There are many kinds of internal fixation techniques for FNFs, but there is not one most suitable implant and postoperative complications such as femoral neck shortening, fracture nonunion, and femoral head necrosis are known adverse events [5,6,7,8].
Cannulated screws (CS) are currently among the most widely used implants in clinical practice [9, 10]. It has the advantages of minor soft tissue damage, low bleeding, and reliable fixation, but it has poor stability in unstable fracture types [11]. And the total postoperative complication rate is about 46.7% [12]. The Femoral neck system (FNS; DePuy Synthes, Zuchwil, Switzerland) is a new femoral neck internal fixation device launched in 2018. The original intention was to make it minimally invasive and stable. It is more stable than CS in biomechanical studies [11]. Some studies have found that FNS promotes fracture healing and reduces operative time and postoperative complications [13,14,15,16,17]. However, other studies have found that the treatment with FNS did not show significant differences in these aspects compared with CS [18,19,20].
Therefore, we conducted a meta-analysis to integrate existing data to study the safety and efficacy of FNS and CS in the treatment of FNFs. The study will be evaluated from the following aspects: intraoperative indicators (incision length, blood loss, X-ray exposure, operation time), postoperative clinical indicators (fracture healing time, hospital stay, length of femoral neck shortening), postoperative complications (nonunion/delayed union, femoral head necrosis, implant failure/cutout), and postoperative scores (Visual Analog Scale (VAS) Score, Harris Score). The aim of our study is to provide evidence for orthopedic surgeons to achieve better clinical outcomes when choosing between these two kinds of internal fixation for treating patients with FNFs.
Material and method
The systematic review was conducted following the PRISMA statement on preferred reporting items on systematic reviews and meta-analyses. The protocol has been registered to PROSPERO (registration number: CRD42021283646).
Database and searching strategies
We performed a comprehensive, systematic literature search on PubMed, EMBASE and Cochrane. The publication dates were limited from 2018 to February 2022. Search terms included synonyms for FNFs and FNS as follows: ((("Femoral Neck Fractures"[Mesh]) OR ((((Femoral Neck Fractures) OR (Femoral Neck Fracture)) OR (Femur Neck Fractures)) OR (Femur Neck Fracture))) AND (((screw) OR (screws)) OR (implant))) AND ((femoral neck system) OR (fns)). After the search was completed, the relevant literature was searched manually to find potential eligible studies.
Inclusion criteria
We followed the population/intervention/comparator/outcome/study design (PICOS) principle to develop the inclusion criteria [21]. (1) Population: patients were adults and diagnosed with FNFs. (2) Intervention: patients were treated with FNS. (3) Comparator: patients treated with CS or similar implants [i.e., cannulated compression screw (CCS), inverted cannulated cancellous screw (ICCS), triple screw (TS), and inverted triangle cannulated screw (ITCS)]. (4) Outcomes: studies had at least one of the following clinical outcomes, including intraoperative indicators (incision length, blood loss, X-ray exposure, operation time), postoperative clinical indicators (fracture healing time, hospital stay, length of femoral neck shortening), postoperative complications (nonunion/delayed union, femoral head necrosis, implant failure/cutout), and postoperative scores (VAS Score, Harris Score). (5) Study design: randomized control trails (RCTs), retrospective control studies, and retrospective cohort studies.
Exclusion criteria
(1) Patients with pathological fractures of the femoral neck, old FNFs, fractures combined with rheumatoid osteoarthritis or hip osteoarthritis, or previous femoral head necrosis. (2) Animal studies. (3) Studies not published in English and Chinese. (4) Studies in which the relevant data could not be extracted, and the original author contacted without response; and (5) biomechanics research and finite element analysis, review articles, expert opinions, case reports, and letters to editors.
Data extraction
Two reviewers independently extracted the data from all the included studies using a standardized data extraction form to ensure uniform collection. The eligible full-text articles needed to have sufficient data to extract and pool. If the relevant data were not provided in the article, the authors were contacted via email to request the data. The following data were extracted from all eligible studies. Study characteristics: authors, publication year, study design, the sample size of different groups, type/classification of fracture, implants used for internal fixation, and follow-up duration. Clinical outcomes: intraoperative indicators (incision length, blood loss, X-ray exposures, operation time); postoperative clinical indicators (fracture healing time, hospital stay, length of femoral neck shortening); postoperative complications (nonunion/delayed union, femoral head necrosis, implant failure/cutout); and postoperative scores (VAS Score, Harris Score). A third investigator resolved any disagreements through discussion or verification.
Quality assessment
Non-randomized controlled studies used the MINORS scoring scale [22] to evaluate the following indicators: clearly stated aim; inclusion of consecutive patients; prospective collection of data; endpoints appropriate to the aim of the study; unbiased assessment of the study endpoint; follow-up period appropriate to the aim of the study; loss to follow-up less than 5%; prospective calculation of the study size; adequate control group; contemporary groups; baseline equivalence of groups; and adequate statistical analysis. According to the checklist for MINORS, the highest score for the comparative study was twenty-four. Two independent reviewers conducted a quality assessment and resolved differences through discussion with a third reviewer.
Statistical analysis
The results of the studies were analyzed using RevMan 5.4 (Copenhagen, The Nordic Cochrane Center, The Cochrane Collaboration, 2020). The weighted mean difference (WMD) with a 95% confidence interval (CI) was used to evaluate continuous outcomes such as blood loss. Odds ratio (OR) with 95% CI was used to assess dichotomous outcomes such as postoperative complications. To measure heterogeneity between studies, we used the I2 statistic. A random effect model was applied to combine statistics. Forest plots were used to graphically represent the difference in outcomes of groups of FNS and CS and for all included studies. If P was < 0.05, the results were considered statistically significant. The sensitivity analysis was performed to investigate the sources’ heterogeneity and verify the reliability of the results to exclude low-quality studies. We did not evaluate publication bias because when the number of studies was < 10, evaluation of publication bias was not required [23].
Results
Included study
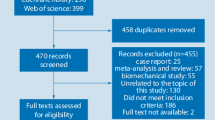
We obtained three hundred and forty-six studies through the search strategy. After excluding seventy-seven duplicate records, the remainders were filtered according to the title and abstract, and two hundred and fifty-three were removed. By reading the full text, we excluded eight studies that did not meet the inclusion criteria: four were not in our area of interest, two were ongoing research that has not yet been published, and two were replicated publications. Finally, the systematic review and meta-analysis included eight studies [13,14,15,16,17,18,19,20]. The literature search process is shown in Fig. 1.
Study characteristics
All included studies were retrospective cohort studies. 448 patients (204 in the FNS group and 244 in the CS group) were enrolled in our study. In these enrolled studies, six studies were conducted in China [13, 15,16,17,18, 20], and each one in Switzerland [19] and Japan [14]. The follow-up time ranged from three to twenty-four months. The types of fractures in included studies involved Pauwels I–III and Garden I–IV. The internal fixations used in the included articles compared FNS with CS or their analogs. See Table 1 for more details of the included studies.
Quality assessment in the included studies
The mean MINORS score for methodological quality assessment was 19/24 (range from 16 to 20) (Table 1). All studies received two points deduction for their retrospective study design, four studies [15, 16, 19, 20] lost points in the follow-up period (two studies [19, 20] did not mention the follow-up period, and two [15, 16] reported an inadequate follow-up period), and one study [19] lost point because of the baseline data inequality.
Meta-analysis of intraoperative indicators
The results of each indicator during the operation are shown in Table 2. Two studies reported the length of the surgical incision [16, 18]. The incision length of the CS group was significantly smaller than in the FNS group (WMD = 0.46; 95% CI, 0.03 to 0.89; P = 0.04) (Fig. 2A). Six studies provided data on intraoperative blood loss [13, 15,16,17,18, 20]. The results showed that blood loss during the operation was significantly less in the CS group than in the FNS group (WMD = 21.54; 95% CI, 10.16 to 32.91; P < 0.001) (Fig. 2B). Two studies compared the number of intraoperative X-ray exposures [18, 20]. The results showed that the number of fluoroscopies in the FNS group were significantly less than in the CS group (WMD = -10.16; 95% CI, -11.44 to -8.88; P < 0.001) (Fig. 2C). Eight studies [13,14,15,16,17,18,19,20] all reported the operation time, and the data of one study [16] was excluded due to the use of the median method for statistics. There was no difference in operation time between the two groups (WMD = -5.32; 95% CI, -14.32 to 3.67; P = 0.25) (Fig. 2D).
Meta-analysis of postoperative clinical indicators
The postoperative clinical indicators are shown in Table 2. Four studies [13, 15, 16, 18] reported fracture healing time. The FNS group was significantly better than the CS group in terms of fracture healing time (WMD = -1.54; 95% CI, -2.38 to -0.70; P < 0.001) (Fig. 3A). The length of hospital stay was extracted from four studies [15, 17,18,19]. There was no significant difference between the two groups (WMD = 0.17; 95% CI, -0.31 to 0.65; P = 0.49) (Fig. 3B). Three studies [13, 16, 19] provided data on the length of femoral neck shortening. Compared with CS, FNS can better prevent femoral neck shortening (WMD = -2.01; 95% CI, -3.11 to -0.91; P < 0.001) (Fig. 3C).
Meta-analysis of postoperative complications
The detailed results of postoperative complications are shown in Table 2. Six studies [13,14,15, 17, 18, 20] included patients with nonunion/delayed union after internal fixation. The results showed no significant difference between the two groups (OR = 0.43; 95% CI, 0.16 to 1.13; P = 0.09) (Fig. 4A). Six studies [13,14,15,16,17,18] reported the occurrence of postoperative femoral head necrosis. The incidence of femoral head necrosis in the FNS group was significantly lower than in the CS group (OR = 0.27; 95% CI, 0.08 to 0.83; P = 0.02) (Fig. 4B). Four studies [13, 16,17,18] reported the occurrence of implant failure/cutout. The incidence of implant failure/cutout was significantly lower in the FNS group than in the CS group (OR = 0.28; 95% CI, 0.10 to 0.82; P = 0.02) (Fig. 4C).
Meta-analysis of postoperative scores
The detailed results of the postoperative scores are shown in Table 2. Two studies provided data on postoperative VAS Score [15, 17]. The VAS Score was significantly lower in the FNS group than in the CS group (WMD = -1.27; 95% CI, -2.51 to -0.04; P = 0.04) (Fig. 5A). Six studies [13, 15,16,17,18, 20] reported the Harris Score. The FNS group was significantly better than the CS group in the Harris Score (WMD = 4.15; 95% CI, 1.00 to 7.30; P = 0.01) (Fig. 5B).
Sensitivity analysis
A sensitivity analysis was performed by individually removing each study to determine whether the pooled results changed. When the study by Yan et al. [15] was removed, the heterogeneity of fracture healing time was reduced (P < 0.001, I2 = 25%). And when Tang et al.’s study [18] was removed, the length of hospital stays without additional heterogeneity (P = 0.88, I2 = 0%). The pooled results of blood loss, operation time, and Harris Score were stable.
Discussion
From the perspective of biomechanical studies compared with the CS, the FNS has a higher angle stability in the unstable femoral neck fracture model, and has a strong ability to resist varus deformity [11, 24]. However, due to the limited clinical application time, only a few studies have compared the therapeutic effects of the two types of implants, and the sample size in different studies was small. Therefore, we have formulated comprehensive and rigorous inclusion and exclusion criteria based on published studies to evaluate the safety and efficacy of FNS and CS in the treatment of FNFs. The results showed that FNS is more effective than CS in decreasing the number of X-ray exposures, fracture healing time, length of femoral neck shortening, femoral head necrosis, implant failure/cutout and postoperative VAS Score. It can also significantly improve the postoperative Harris Score.
Intraoperative indicators
The CS group could significantly reduce blood loss compared with the FNS group in terms of intraoperative indicators. Because when using CS to treat FNFs, only a small incision is needed to implant the screws. When FNS is used, a longitudinal incision is required to implant the FNS device due to its structural characteristics. CS should be more advantageous for soft tissue injuries and intraoperative blood loss. Regardless of the CCS, ICCS, TS, or ITCS, to maximize the stability of the structure and accelerate fracture healing, they all need a triangular distribution, and the screws should be implanted as parallel as possible in anteroposterior X-rays [7, 25]. But there is no correlation between the screws, and the position of the screws in the femoral neck needs to be adjusted multiple times. Therefore, various fluoroscopies cannot be avoided during the operation to determine the position of screws. The design of the FNS device simplifies the surgical procedure. It only needs to insert a 130° guide and a central positioning guide pin to complete the implantation of the internal fixation, which can effectively reduce the number of intraoperative fluoroscopies [18]. It is generally believed that repeated intraoperative fluoroscopies will prolong the operation time when CS is used, but we found no difference in the operation time between the two types of implants. The possible reason is the insufficient time of FNS devices for clinical application, and orthopedic surgeons have not fully mastered the surgical skills, which leads to the prolonged operation time. However, most studies did not report the seniority of surgeons. Only one indicated that the operation was performed by four residents under the supervision of a consultant and by seven surgeons [19].To explore the potential sources of heterogeneity, we performed a sensitivity analysis. The results were consistent with previous results.
Postoperative clinical indicators
In the postoperative clinical indicators, the FNS group was significantly better than the CS group in terms of femoral neck shortening and fracture healing time, and there was no difference in hospitalization time between the implants. One of the characteristics of FNS is dynamic compression [11]. The pre-collapsed insertion allows the anti-rotation screw and bolt slide in the maximum 20 mm packaging to meet femoral neck shortening during fracture healing. Because within a certain range, the impaction of the fracture gap can accelerate the healing of the fracture [26]. However, it is generally considered that shortening > 10 mm is severe femoral neck shortening, which is detrimental to fracture healing and postoperative function [27]. The biomechanical properties of multiple screws cannot fully resist the high shear force around the hip, and severe shortening is prone to occur after surgery [28]. Zlowodzki et al. [29] found that the shortening rates after fracture fixation with multiple cancellous screws of non-displaced and displaced femoral neck fractures were 31% and 27%, respectively. Angular stable devices, including dynamic hip screw and FNS, have advantages in resisting high shear forces and femoral neck shortening [11]. Our systematic review showed that Compared with CS, FNS can effectively prevent femoral neck shortening and accelerate fracture healing time, which is consistent with the results of previous in vitro studies [11]. The high heterogeneity of the results may be due to the different types of fractures included in the studies, but the limitation of the number of existing studies, we cannot perform subgroup analysis. More research should be conducted in the future.
Postoperative complications
In terms of postoperative complications, we observed a significant reduction in femoral head necrosis and internal fixation failure/cut-out in the FNS group. Although the nonunion/delayed union of the fracture of the two types of implants was not significantly different, the incidence in the FNS group was lower. This is a meaningful discovery for clinical treatment. The most commonly used internal fixation device for treating FNFs in clinics is the CS, which has the advantage of minimal intraoperative soft tissue damage and compression fixation of the fracture site. However, its resistance to shear and rotational stresses is insufficient, and even with good intraoperative repositioning, postoperative complications such as nonunion of the fracture, screw excision, and femoral head necrosis are prone to occur, especially in unstable FNFs [30]. These complications are also the main cause of post-operative reoperation, bringing huge risks to the patient's quality of life and financial burden [31]. There are also adjuvant therapies combined with surgery that can decrease the rate of femoral head necrosis, such as platelet-rich plasma or stem cells [32,33,34]. However, there are no reports of FNS in combination with other adjuvant therapies. Our systematic review results showed that FNS effectively reduces the incidence of postoperative complications, which is beneficial for clinical application and demonstrates the safety and efficacy of this new internal fixation device.
Postoperative scores
The VAS Score is an important indicator to assess the degree of pain in patients. A lower score is associated with lower postoperative pain. Harris Score is the most frequently used scale to evaluate the postoperative function of the hip joint. It mainly evaluates four aspects: pain, daily activities, deformity, and range of motion. The higher the score, the better the individual's postoperative recovery [35]. The results of our systematic review showed that the FNS group could significantly improve the Harris Score compared to the CS group. We believe that the FNS group had a better score because it can effectively prevent postoperative femoral neck shortening. Many studies have found that shortening of the femoral neck leads to inferior hip function. The more severe the shortening, the worse the function [27, 29].
Limitations
This study had the following limitations: (1) all the included studies were retrospective and observational, there was a risk of selection bias, and systemic and random errors were prone to occur; (2) the follow-up duration of the included studies is relatively short, and some postoperative complications may not occur; and (3) the number of included studies is small, and the level of evidence is not high due to the lack of RCTs, more high-quality researches are needed in the future to improve the reliability of the results.
Conclusion
This systematic review indicates that FNS is a safe and effective internal fixation device. However, due to the limited quality and number of included studies and the high heterogeneity of the meta-analysis; large samples and multicenter RCTs are needed to confirm this conclusion in the future.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- FNS:
-
Femoral Neck System
- FNFs:
-
Femoral Neck Fractures
- CS:
-
Cannulated Screws
- VAS:
-
Visual Analog Scale
- PRISMA:
-
Pre-ferred Items Reporting for Systematic Reviews and Meta-Analysis
- PROSPERO:
-
International Prospective Register of Systematic Reviews
- PICOS:
-
Population/Intervention/Comparator/Outcome/Study Design
- RCTs:
-
Randomized Control Trails
- CCS:
-
Cannulated Compression Screw
- ICCS:
-
Inverted Cannulated Cancellous Screw
- TS:
-
Triple Screw
- ITCS:
-
Inverted Triangle Cannulated Screw
- MINORS:
-
Methodological Index for Non-randomized Studies
- WMD:
-
Weighted Mean Difference
- CI:
-
Confidence Interval
- OR:
-
Odds Ratio
References
Dhanwal DK, Dennison EM, Harvey NC, Cooper C. Epidemiology of hip fracture: Worldwide geographic variation. Ind J Orthop. 2011;45(1):15–22.
Xing F, Luo R, Liu M, Zhou Z, Xiang Z, Duan X. A New Random Forest Algorithm-Based Prediction Model of Post-operative Mortality in Geriatric Patients With Hip Fractures. Front Med. 2022;9: 829977.
Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–7.
Dolatowski FC, Frihagen F, Bartels S, Opland V, Šaltytė Benth J, Talsnes O, et al. Screw Fixation Versus Hemiarthroplasty for Nondisplaced Femoral Neck Fractures in Elderly Patients: A Multicenter Randomized Controlled Trial. J Bone Joint Surg Am. 2019;101(2):136–44.
Duffin M, Pilson HT. Technologies for Young Femoral Neck Fracture Fixation. J Orthop Trauma. 2019;33(Suppl 1):S20–6.
Slobogean GP, Stockton DJ, Zeng BF, Wang D, Ma B, Pollak AN. Femoral neck shortening in adult patients under the age of 55 years is associated with worse functional outcomes: Analysis of the prospective multi-center study of hip fracture outcomes in China (SHOC). Injury. 2017;48(8):1837–42.
Augat P, Bliven E, Hackl S. Biomechanics of Femoral Neck Fractures and Implications for Fixation. J Orthop Trauma. 2019;33(Suppl 1):S27-s32.
Shu DP, Xiao YP, Bei MJ, Ji T, Peng YJ, Ma B, et al. Dynamic compression locking system versus multiple cannulated compression screw for the treatment of femoral neck fractures: a comparative study. BMC Musculoskelet Disord. 2020;21(1):1–9.
Zhang Q, Ling M, Wang X, Cui D. A Comparison of Two Peripheral Nerve Blocks Combined With General Anesthesia in Elderly Patients Undergoing Arthroplasty for Hip Fractures: A Pilot Randomized Controlled Trial. Front Surg. 2022;9: 715422.
Wahlsten LR, Palm H, Gislason GH, Brorson S. Sex differences in incidence rate, and temporal changes in surgical management and adverse events after hip fracture surgery in Denmark 1997–2017: a register-based study of 153,058 hip fracture patients. Acta Orthop. 2021;92(4):424–30.
Stoffel K, Zderic I, Gras F, Sommer C, Eberli U, Mueller D, et al. Biomechanical Evaluation of the Femoral Neck System in Unstable Pauwels III Femoral Neck Fractures: A Comparison with the Dynamic Hip Screw and Cannulated Screws. J Orthop Trauma. 2017;31(3):131–7.
Zhang LL, Zhang Y, Ma X, Liu Y. Multiple cannulated screws vs. dynamic hip screws for femoral neck fractures : A meta-analysis. Der Orthopade. 2017;46(11):954–62.
Hu H, Cheng J, Feng M, Gao Z, Wu J, Lu S. Clinical outcome of femoral neck system versus cannulated compression screws for fixation of femoral neck fracture in younger patients. J Orthop Surg Res. 2021;16(1):370.
Nibe Y, Matsumura T, Takahashi T, Kubo T, Matsumoto Y, Takeshita K. A comparison between the femoral neck system and other implants for elderly patients with femoral neck fracture: A preliminary report of a newly developed implant. Journal of Orthopaedic Science. 2021:1–5.
Yan CWX, Xiang C, Jiang K, Li Y, Chen Q, Deng C, Chen L. Comparison of effectiveness of femoral neck system and cannulate compression screw in treatment of femoral neck fracture in young and middle-aged patients. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(10):1–7.
Yang J, Zhou X, Li L, Xu L, Zhu W, Xu W, et al. Comparison of femoral neck system and inverted triangle cannulated screws fixations in treatment of Pauwels typle III femoral neck fractures. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(9):1111–8.
Zhou XQ, Li ZQ, Xu RJ, She YS, Zhang XX, Chen GX, et al. Comparison of Early Clinical Results for Femoral Neck System and Cannulated Screws in the Treatment of Unstable Femoral Neck Fractures. Orthopaedic Surgery. 2021;9999.
Tang Y, Zhang Z, Wang L, Xiong W, Fang Q, Wang G. Femoral neck system versus inverted cannulated cancellous screw for the treatment of femoral neck fractures in adults: a preliminary comparative study. J Orthop Surg Res. 2021;16(1):504.
Vazquez O, Gamulin A, Hannouche D, Belaieff W. Osteosynthesis of non-displaced femoral neck fractures in the elderly population using the femoral neck system (FNS): short-term clinical and radiological outcomes. J Orthop Surg Res. 2021;16(1):477.
Yang Y, Ma T, Zhang X, Luo X, Fan T, Wang Y. Short-term effectiveness of femoral neck system in the treatment of femoral neck fracture. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2021;35(5):539–43.
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17(24):2815–34.
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–6.
Higgins JPT GS. Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011. http://handbook.cochrane.org/ : The Cochrane Collaboration; 2011.
Schopper C, Zderic I, Menze J, Müller D, Rocci M, Knobe M, et al. Higher stability and more predictive fixation with the Femoral Neck System versus Hansson Pins in femoral neck fractures Pauwels II. J Orthop Transl. 2020;24:88–95.
Macke C, Werner M, Herold L, Krause O, Graulich T, Clausen JD, et al. No Consequence for Lateral View X-Ray in Displaced Proximal Femoral Fractures in the Elderly. Front Surg. 2021;8: 652528.
Augat P, Simon U, Liedert A, Claes L. Mechanics and mechano-biology of fracture healing in normal and osteoporotic bone. Osteoporosis Int. 2005;16(Suppl 2):S36-43.
Felton J, Slobogean GP, Jackson SS, Della Rocca GJ, Liew S, Haverlag R, et al. Femoral Neck Shortening after Hip Fracture Fixation Is Associated with Inferior Hip Function: Results from the FAITH Trial. J Orthop Trauma. 2019;33(10):487–96.
Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. N Engl J Med. 2017;377(21):2053–62.
Zlowodzki M, Ayeni O, Petrisor BA, Bhandari M. Femoral neck shortening after fracture fixation with multiple cancellous screws: incidence and effect on function. J Trauma. 2008;64(1):163–9.
Slobogean GP, Sprague SA, Scott T, Bhandari M. Complications following young femoral neck fractures. Injury. 2015;46(3):484–91.
Richards JT, Overmann AL, O’Hara NN, D’Alleyrand JC, Slobogean GP. Internal Fixation Versus Arthroplasty for the Treatment of Nondisplaced Femoral Neck Fractures in the Elderly: A Systematic Review and Meta-Analysis. J Orthop Trauma. 2020;34(1):42–8.
Jiang J, Xing F, Luo R, Liu M. Effectiveness of Platelet-Rich Plasma for Patients With Carpal Tunnel Syndrome: A Systematic Review and meta-Analysis of Current Evidence in Randomized Controlled Trials. Front Pharmacol. 2022;13: 834213.
Xu HH, Li SM, Fang L, Xia CJ, Zhang P, Xu R, et al. Platelet-rich plasma promotes bone formation, restrains adipogenesis and accelerates vascularization to relieve steroids-induced osteonecrosis of the femoral head. Platelets. 2021;32(7):950–9.
Lin RLC, Sung PH, Wu CT, Tu YK, Lu YD, Yip HK, et al. Decreased Ankyrin Expression Is Associated with Repressed eNOS Signaling, Cell Proliferation, and Osteogenic Differentiation in Osteonecrosis of the Femoral Head. J Bone Joint Surg Am. 2022;104(Suppl 2):2–12.
Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51(4):737–55.
Acknowledgements
Not applicable.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
J.J. and J.C. contributed equally to this study. J.J. contributed to search the database, extract the data, analyze the data and manuscript writing. J.C. helped to extract the data and review the manuscript. F.X. and H.L. helped to searched the database and extracted the data. Z.X. helped to review the manuscript. J.C. is the correspondence author who responsible for the correspondence, topic identification and manuscript reviewing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jiang, J., Chen, J., Xing, F. et al. Comparison of femoral neck system versus cannulated screws for treatment of femoral neck fractures: a systematic review and meta-analysis. BMC Musculoskelet Disord 24, 285 (2023). https://doi.org/10.1186/s12891-023-06378-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06378-x