Abstract
Background
Plantar fasciitis (PF) is a common orthopaedic problem, with heel pain worsening the quality of life. Although steroid injection is often used if the conservative treatment fails, Platelet-Rich Plasma (PRP) injection is gaining popularity due to its safety and long-lasting effect. However, the effect of PRP versus steroid injection in PF has not been studied yet in Nepal. Therefore, this study aimed to assess the effect of PRP compared with steroid injection in the treatment of PF.
Methods
This study was a single-center, hospital-based, open-label, parallel-group randomized clinical trial to compare the effect of PRP injection with steroid injection in plantar fasciitis between August 2020 and March 2022. A total of 90 randomly selected participants aged 18 to 60 years suffering from plantar fasciitis with failed conservative treatment were intervened. The American Orthopaedic Foot and Ankle Society (AOFAS) and the Visual Analog Scale (VAS) scoring system were used to evaluate functional mobility and pain before and after the intervention for three and six months, respectively. Statistical analyses were performed using a Student’s two-sample t-test. P-value < 0.05 was considered statistically significant.
Results
The PRP injection showed a better outcome than the steroid injection in six months follow-up. The mean (± SD) VAS score was significantly decreased in the PRP group (1.97 + 1.13) than in the steroid group (2.71 ± 0.94) with the group difference of -0.73 (95% CI: -1.18 to -0.28) at six months. Similarly, there was a significant increase in the AOFAS scores in the PRP group (86.04 ± 7.45) compared to the steroid group (81.23 ± 9.60) at six months of follow-up with a group difference of 4.80 (95% CI: 1.15 to 8.45). There was also a significant reduction of plantar fascia thickness in the PRP group compared to that of the steroid group (3.53 ± 0.81 versus 4.58 ± 1.02) at six months of follow-up with the group difference of -1.04 (95% CI: -1.44 to -0.65).
Conclusion
The PRP injection showed better outcomes than steroid injection in plantar fasciitis treatment over the course of six months. Further research with a larger population and longer follow-up than six months is needed to generalize the findings and their long-term efficacy.
Trial registration
NCT04985396. First registered on 02 August 2021. (https://clinicaltrials.gov/ct2/show/NCT04985396)
Similar content being viewed by others
Introduction
Plantar fasciitis (PF), better termed as plantar fasciosis [1, 2], is a degeneration of plantar fascia leading to an inflammatory reaction [3]. It occurs mostly due to the biomechanical stress on the plantar fascia [4]. The plantar fascia is a thin elastic fibrous band of connective tissue aligned in a longitudinal orientation with a rich extracellular matrix predominantly in the Hyaluronan [5]. Fasciacytes, a new cell found in the plantar fascia, first termed by Stecco et al., 2018 is devoted to the production of hyaluronan, which promotes the gliding function between the deep fascia and muscle [6]. Plantar fascia lies in close connectivity to the para tendon of Achilles through the heel periosteum. Therefore, any degenerative or inflammatory process within the para tendon of Achilles can hinder normal foot kinematics rendering plantar fascia thickness increment leading to plantar fasciitis [7].
The PF worsens the quality of life [8, 9] with a lifetime global prevalence of 10% [10], more common in females than males [11] due to the difference in lifestyle and health status between both sexes [12]. The prevalence of plantar fasciitis is 7.5% in the UK, 3.6% in Australia [13], 59% in India among the age group of 40 to 50 years [14], and 57.8% in Saudi Arabia [15]. Physicians have 8.14%, nurses have 13.11% [16], and athletes have 5 to 18% prevalence [13]. However, the prevalence of plantar fasciitis in Nepal is unknown.
PF resolves in 80–90% of cases within ten months [17,18,19]. Non-surgical treatments such as non-steroid anti-inflammatory drugs (NSAIDs), shoe inserts, stretching exercises, or extracorporeal shockwave therapy [20,21,22,23] are the first-line treatment of PF [24], successful in up to 90% of cases [25] and steroid as an injection (SI) therapy is traditionally practiced if non-operative treatment fails [26]. It is effective because of its anti-inflammatory properties, associated with the risk of plantar fascia rupture, heel fat pad atrophy [27], lateral plantar nerve injury secondary to injection, and calcaneal osteomyelitis and iontophoresis, burning of the underlying skin [28]. A steroid injection may offer short-term relief, but it did not find long-term benefit in six months follow-ups compared to a placebo in a recent review [29]. On the other hand, Platelet Rich Plasma (PRP) has strong anti-inflammatory properties with no adverse effects on the plantar fascia structure. It contains high levels of growth factors and anti-inflammatory cytokines, which potentially ameliorate degenerative conditions [30], prevent infections [31], and enhance wound healing, bone healing, and tendon healing [32]. Therefore, PRP has been a biological option in treating the PF [33].
PRP therapy is a relatively new approach in the regenerative medicine [34]. Nowadays, it has been a promising solution to many orthopaedic problems such as tendinopathies, non-union, and arthritis of the knee [35]. Of course, it has gained popularity in treating Achilles tendinopathies [36]. However, there is also controversy among orthopaedic surgeons about the effectiveness of the PRP [37]. The high cost of commercially available PRP kits demotivates the use of PRP therapy in most cases [38].
Furthermore, the PRP preparation in the laboratory is a lengthy process, taking approximately 35 to 40 min but yields an increase in initial platelet count from 104.47 to 196.82%, allowing excellent clinical application [39]. There is a paucity of evidence to compare the effect of PRP with steroid injection for the management of plantar fasciitis in poor resource countries like Nepal. As far as we know, there hasn’t been single research undertaken in Nepal to compare the efficacy of steroid injection and PRP. This study will be important in developing countries like Nepal from a different perspective. Developing countries have a high prevalence of barefoot activity [40], which leads to the anatomy of foot pronation [41] causing chronic PF [42], which accounts for about 70 − 86% of patients [20]. A large portion of the population (between 63 and 72% ) wears inappropriate shoes [43] leads to plantar fasciitis [44]. Similarly, an intra-articular or soft tissue steroid injection may lead to different health comorbidities [45]; one of them is the increase of acute coronary syndrome with seven folds [46], raising the medical cost as well as costs due to the loss of productivity [47]. On the other side, PRP treatment is low-cost, simple and minimally invasive in nature [48]. It is safer and more beneficial than steroid injection in PF [49, 50] and is considered superior to SI for long-term pain relief [51]. Different studies have also shown that the PRP treatment is an alternative to surgery [52,53,54,55,56], and data reveals that surgery may be required for approximately 5–10% of chronic plantar fasciitis [57]. As the handmade standard PRP is more reliable and cost-effective than commercially available PRP kits [38], the financial burden on the health care system can be minimized by establishing the standardized laboratory set-up and formulating the PRP preparation protocol in developing countries. Therefore, this study aimed to compare the effect of platelet-rich plasma injection with steroid injection for the treatment of plantar fasciitis in Nepal in terms of pain, functional mobility and also the change of plantar fascia thickness.
Methods
Study design and setting
The report of this trial followed the Consolidated Standards of Reporting Trials (CONSORT) 2010 updated guidelines for reporting randomized controlled trials [58]. This study was a single-centre, hospital-based, open-label, parallel-group randomized clinical trial to compare the effect of PRP injection with steroid injection in the treatment of Plantar fasciitis between August 2020 and March 2022. The study was conducted in the outpatient department of Nepal Orthopaedic Hospital, Kathmandu, Nepal. It is one of the Orthopaedic and Trauma care super-speciality centres in Nepal that provides only orthopaedic services. It is a 100 bedded charitable autonomous hospital run under the Nepal Disabled Association of Nepal with the support of the Patan Rotary club, Nepal, and different International Rotary Clubs [59]. The patients aged 18 to 60 years with a history of heel pain of more than six weeks with tenderness on palpation over medial calcaneum tuberosity and diagnosed as PF, those patients with failure of conservative treatment with physiotherapy, splints, and NSAIDs, those patients who were mentally fit, and those patients who provided written informed consent were included in the study. The patients with lumbar radiculopathy, existing trauma, previous surgery or any foot pathology, under aspirin treatment, bleeding disorders with low platelet counts, and systemic diseases like diabetes and rheumatoid arthritis were excluded.
Sample size determination
The sample size was calculated based on a similar study conducted by Jain et al. (2015) in Wrightington Hospital, Wigan, UK, where the mean ± SD of the American Orthopaedic Foot and Ankle Society (AOFAS) score in both PRP Vs steroid groups were 88.50 ± 13.52 Vs 75.07 ± 20.13, respectively [60]. The sample size was calculated considering this data and taking a level of significance at 3% and power of 90%, using a test comparing independent two means in Stata/MP version 14.1 (StataCorp LP, College Station, Texas). The calculated sample size was 76. After adding a 20% dropout rate, the final sample size was 90 (45 participants in each group).
Randomization
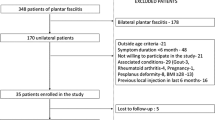
After the assessment of the participants by the orthopaedic surgeon, they were randomized in a 1:1 ratio and assigned either to the steroid group or the PRP groups through computer-generated random numbers [61] (Fig. 1). A statistician prepared a computer-generated random number list allocated to the steroid group and PRP group. The allocated numbers were put inside the envelope by the statistician. The data enumerator opened the sealed envelope consecutively, with no exception. According to the information provided inside the envelope, participants were allocated either to the steroid group or the PRP group. Upon confirmation of a participant’s eligibility, the next envelope in the sequence was opened, and the treatment allocation was entered on a randomization list. A similar procedure of randomization technique was used in the previous study [62].
Intervention
The patients diagnosed with plantar fasciitis by clinicians were randomized either into the steroid group or PRP group by the principal author and intervened by other research team members.
Steroid group
In the steroid group, 2ml of injection Depo-Medrol 80 mg (Methylprednisolone) along with 1 ml lignocaine (0.25%) were loaded in a 5 cc syringe. Then the cocktail was injected into the medial calcaneal tuberosity at the most tender point using an aseptic technique [63].
PRP group
The 30 ml blood of participants was collected into an acid citrate dextrose tube under aseptic conditions and subjected to centrifugation at 2000 rpm (soft spin) through a digital centrifuge machine speed control (REMI, R-8 C PLUS). There were three layers of blood; among them, the supernatant layer and buff coat of plasma were again subjected to centrifuge at 3000 rpm (hard spin). The upper two-thirds of the tube containing platelet-poor plasma was discarded, and the lower one-third of concentrated platelet plasma superficial buffy coat was injected into medial calcaneal tuberosity at the most tender point. The PRP preparation method and the way of injection technique were adapted from the previous study [64].
After the injection in both groups, the participants were advised not to engage in any rigorous activity with the affected foot for at least two days and then gradually return to their regular activities. All participants were counselled to follow up in the next visit at three months and six months. The midline and end-line data were recorded at three and six months, respectively.
Study variables
Outcome variables
The primary outcomes were the functional mobility and pain of the participants; the secondary outcome measure was the plantar fascia thickness. The American Orthopaedic Foot & Ankle Society (AOFAS) [65] was used for the evaluation of functional mobility in the clinical setting before intervention (baseline) and after intervention (midline) at three months and (end-line) at six months follow-up. It combined subjective scores of pain and function provided by the patient as well as objective scores evaluated by the orthopaedic surgeon with a physical examination of the participants. They were assessed by sagittal motion, hindfoot motion, ankle–hindfoot stability, and alignment of the ankle–hindfoot. The AOFAS included nine items divided into three subscales (pain, function, and alignment). Pain consists of one item with a maximal score of 40 points, indicating no pain; function consists of seven items with a maximal score of 50 points, indicating full function and alignment consists of one item with a maximal score of 10 points, indicating good alignment. The maximal score is 100 points, indicating no symptoms or impairments [65]. Like AOFAS, the pain was evaluated at baseline and the midline at three months and end-line at six months with the Visual Analog Scale (VAS) [66]. The VAS consisted of a 10 cm straight line with the endpoints defining the intensity of pain from zero to 10 indicating that zero indicated “no pain at all” and 10 indicated “worst pain”. They were asked to express their severity of pain at the time of data collection in a descriptive term as no pain, mild pain, moderate pain, severe pain, or worst pain, and they were ranked to numerical scores for analysis [62]. Another outcome was the plantar fascia thickness which was assessed before intervention (baseline) and after intervention at six months through high-resolution ultrasonography (Ultrasound machine-SONOACE X7) by a trained radiologist. The cut-off value for confirming PF was used if plantar fascia thickness was more than 4 mm [67].
Predictor variables
Socio-demographic information of the respondents, such as age, sex, ethnicity, and religion, was collected using a semi-structured questionnaire through a face-to-face interview. Similarly, a clinical parameter such as direct radiographs of the heel was performed to find out the presence/absence of calcaneum spur and other heel pathologies.
Safety issue
Most of the complications related to these interventions were analyzed. The side effect of the steroid varies based on the body site where it is injected; in the joint, muscle or spine. A review done by Hynes and Kavanagh, 2022 reveals that extra-articular steroid injection reports minor and major events in 0.81% and 0.5 to 8%, respectively while the injection in shoulder joints presents the major reaction in 18.1% [68]. As in our study, the injection was locally applied to the heel region; there were few chances of side effects like pain and discomfort for a few days, temporary bursitis, and flushing of the face for a few hours. The systemic side effects of local steroid injection are poorly understood and not well recognized, hence clinically insignificant [69]. Although there is a rise in blood glucose in diabetic participants, it is considered clinically insignificant [70, 71]. Plantar fascia rupture and heel fat pad atrophy are associated with local steroid injections in the long term which is around only 2.4–6.7% [72]. The steroid injection may develop temporary or permanent neural dysfunction leading to economic or social disabilities [73]. Hypopigmentation and atrophy of the skin may occur [74, 75], which is interestingly re-pigmented with exposure to ultraviolet light after a few months [76, 77]. Moreover, normal saline injection is considered a very effective modality to treat progressive cutaneous atrophy [78]. However, there were no such cases in our study. On the other side, PRP treatment is considered a safe and effective approach having very less side effects [33]. As this study was performed in a highly specialized tertiary hospital, the institution had a well-managed setup to handle in case of any immediate adverse reaction occurred.
Ethical consideration
Ethical clearance was obtained from the Ethical Review Board (ERB) of the Nepal Health Research Council (NHRC) (Ref. 3322). Similarly, the clinical trial was registered to clinicaltrilregistry.gov (Identifier: NCT04985396, registered on 02/08/2021). Formal permission was obtained from the Nepal Orthopaedic Hospital, Kathmandu, Nepal to conduct the study at their site. We constituted a Data and Safety Monitoring Board (DSMB) consisting of two orthopaedic surgeons and one statistician. The DSMB members prepared study-stopping rules and reviewed all the possible effects reported. The respondents were informed about the purpose of this study. The signing of informed consent was taken from eligible participants. Voluntary informed participation and freedom of refusal at any time during the study were strongly applied so that participants could withdraw from the study at any time without giving a reason and without fear. Privacy and confidentiality of collected information were ensured at all levels.
Data management and analysis
The collected data were entered in Epi-Data version 3.2 and analyzed based on the intention-to-treat (ITT) principle using Stata/MP version 14.1 (StataCorp LP, College Station, Texas). The normality of data was assessed using Shapiro–Wilk test. Socio-demographic data were analyzed using descriptive analysis. Since the data were normally distributed, the mean and standard deviation (SD) were calculated. Comparisons were made using the Student’s two-sample t-test. The Box and whisker plot was also used to display the PRP and steroid group outcome measures. All values less than 0.05 were considered statistically significant.
Results
Socio-demographic characteristics and clinical parameters of participants
At baseline, a total of 90 participants were included in this study (45 participants in the PRP and 45 in the steroid group). However, after six months of follow-up, a total of 87 participants completed the study (45 participants in the PRP group and 42 participants in the steroid group), whereas three participants lost follow in the steroid group, and none of the participants discontinued the trial in the PRP group (Fig. 1).
The majority, 76 (84.4%), were female, and 14 (15.6%) were male. The mean ± SD age of the participants was 43.8 ± 10.9 years (42.9 ± 10.3 in the PRP group and 44.7 ± 11.6 in the steroid group). Almost two-thirds of the participants (75.6%) were Hindu believers, while the remaining (24.4%) were of non-Hindu origin. Approximately equal proportions (48.9% and 51.1%) were from advantaged and disadvantaged ethnic groups, respectively. Most of the participants (58.9%) had the problem of plantar fasciitis on the right foot, and only 41.1% had the occurrence on the left side. Similarly, the presence of calcaneum spur was found in 52.2% of participants, while it was absent in 47.8% of participants (Table 1).
Primary outcomes in steroid injection and PRP injection
The mean ± SD VAS scores for pain at baseline were 5.22 ± 1.34 and 4.77 ± 0.95 in PRP and SI groups, respectively with a group difference of 0.44 (95% CI: -0.04 to 0.93). The mean baseline pain scores were changed to 4.22 ± 1.04 in the PRP group and 3.14 ± 0.81 in the SI group in three months follow-ups with a group difference of 1.07 (95% CI: 0.67 to 1.47). Similarly, the baseline pain score was significantly decreased in the PRP group than the SI group (1.97 ± 1.13 versus 2.71 ± 0.94) with a group difference of -0.73 (95% CI: -1.18 to -0.28) in six months follow-up.
The functional mobility measured with the AOFAS scores were 52.53 ± 14.87 and 58.14 ± 11.47 in PRP and SI groups, respectively with a difference of 0.44 (95% CI: -0.04 to 0.93) at the baseline study. The mean AOFAS score was improved to 63.80 ± 12.04 in the PRP group and 75.76 ± 7.18 in the SI group in three months with a group difference of -11.96 (95% CI: -16.22 to -7.69). Similarly, the AOFAS score was significantly increased in PRP than SI group (86.04 ± 7.45 versus 81.23 ± 9.60) with a group difference of 4.80 (95% CI: 1.15 to 8.45) in six months (Table 2; Fig. 2).
Secondary outcomes
The plantar fascia thickness between PRP and steroid groups was comparable (5.56 ± 0.95 mm versus 5.69 ± 0.88 mm) with the group difference of -0.12 (95% CI: -0.51 to 0.25) at baseline data which was decreased to 3.53 ± 0.81 mm and 4.58 ± 1.02 mm in six months, respectively with a difference of -1.04 (95% CI: -1.44 to -0.65) (Table 2; Fig. 2).
Discussion
The study aimed to compare the effect of PRP injection with steroid injection for the treatment of plantar fasciitis. This study shows that steroids had better results than PRP in three months, but in six months, PRP decreased the massive pain and had a more improved AOFAS score compared with steroids.
The well-being of the participants, assessed in terms of pain and functional mobility, was found to be better in the steroid group at three months; however, long-lasting relief from pain and higher mobility function was achieved at six months in the PRP group. These findings are consistent with other studies [60, 79]. Different systematic reviews have shown that steroid injection had a quick recovery in reducing the symptoms than PRP, which has a slower improvement but long-term permanent effect [50, 80]. Yang et al., 2017 found that the PRP is better than steroid injection for long-term pain reduction in plantar fasciitis, but there was no noticeable observed field difference between short- and intermediate-term effects [51]. This can be explained by the fact that PRP has growth factors and many other molecules with biological regenerative properties for the healing [81]. About 70% of growth factors are released after 10 min of PRP injection within one hour, which synthesize and secrete further growth factors for about eight days until the platelets die. It needs six to eight weeks for full activities after injection [82]. Steroids lack this property and interrupt the inflammatory and immune cascade, which is short-lived [80, 83]. Ang et al., 2019 found in the context of lateral epicondylitis that corticosteroid relieves acute pain but not in the long term, which may be due to the short half-life of the steroid [37]. It might be the reason that local steroid leads to a quick recovery in patients. So, they resume injurious activity without proper rehabilitation, which may lead to recurrence at a higher rate [27, 37]. Besides these, current knowledge reveals that PF occurs through a degenerative rather than an inflammatory process [84]. Histologically, PF has a small tear of fascia, which is replaced with normal fascia and surrounding tissue by angiofibroblastic hyperplastic tissue during the healing process. It is possible with the presence of anti-inflammatory and pro-inflammatory cytokines and interleukins, such as interleukin 4, 8, 13, interferon-α, and tumour necrosis factor-α in PRP [51]. Similarly, plantar fasciitis lacks the different growth factors due to hyper-vascularity and hypo-cellularity, and PRP provides these factors [85].
The findings of this study showed the comparable thickness of the plantar fascia in both PRP and steroid groups (5.56 ± 0.95 mm versus 5.69 ± 0.88 mm) at baseline which confirmed the plantar fasciitis; the cut-off value of more than 4 mm thickness of plantar fascia is suggested of plantar fasciitis [67, 86]. Our study found an immense reduction of plantar fascia thickness in the PRP group than in the steroid group in six months, which was clinically and statistically significant. Kalia et al., 2021 mention that steroid injection significantly reduces the plantar fascia thickness at one and three months than that of PRP but no difference in six months [87]. McMillan et al., 2012 explore that steroid injection reduces abnormal swelling of plantar fascia for up to three months [88]. Data reveals a 35.45% reduction in the thickness of plantar fascia in the PRP group and a 29.16% reduction in the corticosteroid group within six months of follow-up [85]. The mechanism of reducing the plantar fascia thickness due to the steroid and PRP injection has not been well explored. However, it can be justified through the fact that plantar fascia thickening is related to the inflammation episode [5], and both steroid and PRP have anti-inflammatory properties, and it reduces the inflammation [26, 89]. However, PRP may be advantageous over steroid injection as PRP may modulate the plantar fascia degeneration because of its regenerative properties, which steroid lacks and thus short-lived [26]. In fact, plantar fasciitis is degenerative pathology rather than a primarily inflammatory condition [90]. Steroid only reduces the pain temporarily but has no role in healing [91]. Unlike steroid, the effect of PRP does not wear off with time after six months [60]. The bioactive components of PRP help in tissue repair and wound healing by stimulating new blood cell formation and, thus, bringing nutrients and increased blood flow to the injury site [34]. The growth factors and cytokines present in PRP enhance the production of hyaluronan [92, 93], which is anti-inflammatory and increases the gliding between the deep fascia and muscle, reducing the plantar fascia thickness [6]. Furthermore, PRP contains a higher concentration of platelet [94], and higher percentages of lymphocytes and monocytes than whole blood, enhancing safe and natural healing [95] and thus, considered as an alternative to surgery [52,53,54,55,56]. Bohlen et al., 2020 conclude that PRP therapy has clinically similar outcomes compared to those of surgery in the treatment of type 1 medial epicondylitis [52]. Besides these, the success rate of surgical release accounts for 70–90%, with the complications of flattening the longitudinal arch at more than 50% complication rate and hypoesthesia [57]. On subjective evaluation, surgery presents about 80% of patients satisfied [57, 96], while PRP injection has 64% patient satisfaction [97].
This study has a few limitations. As this study was conducted in a specialized orthopaedic hospital, most of the patients had a treatment done earlier in another center which might affect our intervention’s outcomes. Also, most of the patients with plantar fasciitis preferred conservative treatment over injection therapy which could not make the larger sample size to generalize the findings in a large population. Similarly, the multivariate analysis could not be applied as we had no confounders of the plantar fasciitis. Besides these, we did not collect data on anthropometric measurements to find out the body mass index, which is associated with the mechanical properties of the plantar fascia and heel pad [98]. Similarly, we could not assess the participants’ plantar fascia thickness for three months to observe the pattern of changes in the thickness due to high cost. In addition, the data collection time has coincided with the COVID-19 pandemic, which distracted the data collection process due to the worrying scenario and lack of communication with participants. We developed a rapport with participants through compassionate empathy for the initiation of information sharing in data collection. Despite these few limitations, our study has some strengths too. First, we measured the plantar fascia thickness in six months follow-up, which was not found in any other previous studies. To the best of our knowledge, this might be the first study to evaluate the effect of PRP injection compared with SI in terms of the plantar fascia thickness. Second, we prepared PRP in the laboratory through double spinning centrifugation methods, which have a uniform and high concentration of platelet in the PRP. The commercially available PRP kits have a high cost, limited volume of drawn blood, and wide variation in platelet concentration [38]. Manually prepared PRP with double spin methods has high platelet capture efficiency (mean 47.11%, median 41.75%) than commercially available kits (mean 31.89%, median 29.51%) [99].
Conclusion
The PRP injection showed better performance than the steroid injection for the treatment of plantar fasciitis in six months. To generate robust evidence comparing the efficacy of PRP to steroid injection for the treatment of plantar fasciitis, larger multi-centre trials with more than six months of follow-up are required.
Data availability
The data supporting this study’s findings are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restriction.
Abbreviations
- AOFAS:
-
American Orthopaedic Foot and Ankle Society
- DSMB:
-
Data and Safety Monitoring Board
- ERB:
-
Ethical Review Board
- NHRC:
-
Nepal Health Research Council
- NSAIDs:
-
Non-Steroid Anti-inflammatory Drugs
- OPD:
-
Outpatient Department
- PF:
-
Plantar Fasciitis
- PRP:
-
Platelet Rich Plasma
- SI:
-
Steroid Injection
- VAS:
-
Visual Analogue Score
References
Schwartz EN, Su J. Plantar fasciitis: a concise review. Perm J. 2014;18.
Alanazi M, Khan R, Muqri A, Alnosaier Z, Dalak M, Alajlani S, et al. Plantar fasciitis in primary care: a review. Int J Med Dev Ctries. 2022;6(7):1002–5.
Luffy L, Grosel J, Thomas R, So E. Plantar fasciitis: a review of treatments. J Am Acad Physician Assist. 2018;31:20–4.
Chen CM, Lee M, Lin CH, Chang CH, Lin CH. Comparative efficacy of corticosteroid injection and non-invasive treatments for plantar fasciitis: A systematic review and meta-analysis. Sci Rep. 2018;8.
Todros S, Biz C, Ruggieri P, Pavan PG. Experimental analysis of plantar fascia mechanical properties in subjects with foot pathologies. Appl Sci. 2021;11:1–11.
Stecco C, Fede C, Macchi V, Porzionato A, Petrelli L, Biz C, et al. The fasciacytes: a new cell devoted to fascial gliding regulation. Clin Anat. 2018;31:667–76.
Stecco C, Corradin M, Macchi V, Morra A, Porzionato A, Biz C, et al. Plantar fascia anatomy and its relationship with Achilles tendon and paratenon. J Anat. 2013;223:665–76.
Poenaru D, Badoiu S, Ionescu A. Therapeutic considerations for patients with chronic plantar fasciitis (Review). Med Int. 2021;1.
Cotchett M, Rathleff MS, Dilnot M, Landorf KB, Morrissey D, Barton C. Lived experience and attitudes of people with plantar heel pain: A qualitative exploration. J Foot Ankle Res. 2020;13.
Trojian T, Tucker AK. Plantar Fasciitis. Am Fam Physician. 2019;99:744–50.
Orchard J. Plantar fasciitis. 2012;35–9.
Palomo-López P, Becerro-De-Bengoa-Vallejo R, Losa-Iglesias ME, Rodríguez-Sanz D, Calvo-Lobo C, López-López D. Impact of plantar fasciitis on the quality of life of male and female patients according to the foot health status questionnaire. J Pain Res. 2018;11:875–80.
Thomas MJ, Whittle R, Menz HB, Rathod-Mistry T, Marshall M, Roddy E. Plantar heel pain in middle-aged and older adults: population prevalence, associations with health status and lifestyle factors, and frequency of healthcare use. BMC Musculoskelet Disord. 2019;20.
Lourdes RK, Ram GG. Incidence of calcaneal spur in indian population with heel pain. Int J Res Orthop. 2016;2:173.
Goweda R, Alfalogy E, Filfilan R, Hariri G. Prevalence and risk factors of Plantar Fasciitis among patients with Heel Pain Attending Primary Health Care Centers of Makkah, Kingdom of Saudi Arabia. J High Inst Public Heal. 2015;45:71–5.
SUNG K-C, CHUNG J-Y, FENG I-J, YANG S-H, HSU C-C, LIN, H-J, et al. Plantar fasciitis in physicians and nurses: a nationwide population-based study. Ind Health. 2020;58:153–60.
Klein SE, Dale AM, Hayes MH, Johnson JE, McCormick JJ, Racette BA. Clinical presentation and self-reported patterns of pain and function in patients with plantar heel pain. Foot Ankle Int. 2012;33:693–8.
Davis PF, Severud E, Baxter DE. Painful Heel Syndrome: Results of Nonoperative Treatment. 2016;151:531–5.
Thompson JV, Saini SS, Reb CW, Daniel JN. Diagnosis and management of plantar fasciitis. J Am Osteopath Assoc. 2014;114:900–6.
Ali Tahririan M, Motififard M, Tahmasebi MN, Siavashi B. Plantar Fasciitis. J Res Med Sci. 2012;17:799–804.
Gupta R, Malhotra A, Masih GD, Khanna T, Kaur H, Gupta P, et al. Comparing the role of different treatment modalities for Plantar Fasciitis: a double blind randomized controlled trial. Indian J Orthop. 2020;54:31–7.
Yelverton C, Rama S, Zipfel B. Manual therapy interventions in the treatment of plantar fasciitis: A comparison of three approaches. Heal SA Gesondheid. 2019;24.
Healey K, Chen K. Plantar Fasciitis: current diagnostic Modalities and Treatments. Clin Podiatr Med Surg. 2010;27:369–80.
MacRae CS, Roche AJ, Sinnett TJ, O’Connell NE. What is the evidence for efficacy, effectiveness and safety of surgical interventions for plantar fasciopathy? A systematic review. PLoS One. 2022;17.
Lareau CR, Sawyer GA, Wang JH, DiGiovanni CW. Plantar and medial heel pain: diagnosis and management. J Am Acad Orthop Surg. 2014;22:372–80.
Hurley ET, Shimozono Y, Hannon CP, Smyth NA, Murawski CD, Kennedy JG. Platelet-Rich Plasma Versus Corticosteroids for Plantar Fasciitis: A Systematic Review of Randomized Controlled Trials. Orthop J Sport Med. 2020;8.
Ang TWA. The effectiveness of corticosteroid injection in the treatment of plantar fasciitis. Singap Med J. 2015;56:423–32.
Wronka KS, Sinha A. Calcaneal osteomyelitis following steroid injection for Plantar Fasciitis: a Case Report. Foot Ankle Spec. 2012;5:253–5.
David JA, Sankarapandian V, Christopher PRH, Chatterjee A, Macaden AS. Injected corticosteroids for treating plantar heel pain in adults. Cochrane Database Syst Rev. 2017;2017.
Baksh N, Hannon CP, Murawski CD, Smyth NA, Kennedy JG. Platelet-Rich plasma in Tendon Models: a systematic review of Basic Science Literature. Arthrosc J Arthrosc Relat Surg. 2013;29:596–607.
Zhang W, Guo Y, Kuss M, Shi W, Aldrich AL, Untrauer J, et al. Platelet-rich plasma for the treatment of tissue infection: Preparation and clinical evaluation. Tissue Eng - Part B Rev. 2019;25:225–36.
Peerbooms JC, Van Laar W, Faber F, Schuller HM, Van Der Hoeven H, Gosens T. Use of platelet rich plasma to treat plantar fasciitis: Design of a multi centre randomized controlled trial. BMC Musculoskelet Disord. 2010;11.
Zhang JY, Fabricant PD, Ishmael CR, Wang JC, Petrigliano FA, Jones KJ. Utilization of platelet-rich plasma for Musculoskeletal Injuries: an analysis of current treatment Trends in the United States. Orthop J Sport Med. 2016;4:24–6.
Pavlovic V, Milan C, Vladimir J, Predrag S. Platelet Rich plasma: a short overview of certain bioactive components. Open Med. 2016;11:242–7.
Dhillon MS, Patel S, John R. PRP in OA knee - Update, current confusions and future options. Sicot-J. 2017;3.
Madhi MI, Yausep OE, Khamdan K, Trigkilidas D. The use of PRP in treatment of Achilles Tendinopathy: a systematic review of literature. Study design: systematic review of literature. Ann Med Surg. 2020;55:320–6.
Li A, Wang H, Yu Z, Zhang G, Feng S, Gao Y. Platelet-rich plasma vs corticosteroids for elbow epicondylitis. Med. 2019;98.
Dhurat R, Sukesh M. Principles and methods of preparation of platelet-rich plasma: a review and author′s perspective. J Cutan Aesthet Surg. 2014;7:189–97.
Mota M, de Barreto L, Leite RB, Cavalcante BR. Desenvolvimento de um dispositivo para obter plasma rico em plaquetas (PRP). Rev Bras Ortop. 2022;57:289–94.
Francis P, Schofield G, Mackay L. Being barefoot. Prevalence at home, in school and during sport: a cross-sectional survey of 714 New Zealand secondary school boys. J Foot Ankle Res. 2018;11:42.
Franklin S, Grey MJ, Heneghan N, Bowen L, Li F-X. Barefoot vs common footwear: a systematic review of the kinematic, kinetic and muscle activity differences during walking. Gait Posture. 2015;42:230–9.
Rani P, Shakya P. Obese pronated foot posture may increase the risk of chronic plantar heel pain than normal pronated foot posture: a case control study. Med Sport J Rom Sport Med Soc. 2012;8:1873–82.
Buldt AK, Menz HB. Incorrectly fitted footwear, foot pain and foot disorders: a systematic search and narrative review of the literature. J Foot Ankle Res. 2018;11.
Umar H, Idrees W, Umar W, Khalil A, Rizvi Z. Impact of routine footwear on foot health: a study on plantar fasciitis. J Fam Med Prim Care. 2022;11:3851.
Puzzitiello RN, Patel BH, Forlenza EM, Nwachukwu BU, Allen AA, Forsythe B, et al. Adverse impact of Corticosteroids on Rotator Cuff Tendon Health and Repair: a systematic review of Basic Science Studies. Arthrosc Sport Med Rehabil. 2020;2:e161–9.
Thomas K, Schonmann Y. Orthopaedic corticosteroid injections and risk of acute coronary syndrome: a cohort study. Br J Gen Pract. 2021;71:E128–33.
Zhao Z, Winget M. Economic burden of illness of acute coronary syndromes: medical and productivity costs. BMC Health Serv Res. 2011;35.
Mehrabani D, Seghatchian J, Acker JP. Platelet rich plasma in treatment of musculoskeletal pathologies. Transfus Apher Sci. 2019;58.
Ling JF, Wininger AE, Hirase T. Platelet-Rich plasma Versus Corticosteroid injection for lumbar spondylosis and sacroiliac arthropathy: a systematic review of comparative studies. Cureus. 2021. https://doi.org/10.7759/cureus.14062.
Ben-Nafa W, Munro W. The effect of corticosteroid versus platelet-rich plasma injection therapies for the management of lateral epicondylitis: A systematic review. Sicot-J. 2018;4.
Yang W-Y, Han Y-H, Cao X-W, Pan J-K, Zeng L-F, Lin J-T et al. Platelet-rich plasma as a treatment for plantar fasciitis. Med. 2017;96.
Bohlen HL, Schwartz ZE, Wu VJ, Thon SG, Finley ZJ, O’Brien MJ et al. Platelet-Rich Plasma Is an Equal Alternative to Surgery in the Treatment of Type 1 Medial Epicondylitis. Orthop J Sport Med. 2020;8.
Sampson S, Gerhardt M, Mandelbaum B. Platelet rich plasma injection grafts for musculoskeletal injuries: a review. Curr Rev Musculoskelet Med. 2008;1:165–74.
Alzahrani WM. Platelet-Rich Plasma Injections as an Alternative to Surgery in Treating Patients With Medial Epicondylitis: A Systematic Review. Cureus. 2022;14.
Kim C-H, Park Y-B, Lee J-S, Jung H-S. Platelet-rich plasma injection vs. operative treatment for lateral elbow tendinosis: a systematic review and meta-analysis. J shoulder Elb Surg. 2022;31:428–36.
Eltabl M, Saif D, Alemam S. Platelet-rich plasma injection versus surgical and medical treatment of mild-moderate carpal tunnel syndrome. Egypt J Neurol Psychiatry Neurosurg. 2020;56.
Lal Sahu R. Percutaneous planter fasciitis release under local anesthesia: a prospective study. Chin J Traumatol. 2017;20:87–9.
Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:834–40.
Nepal Orthopaedic Hospital. Nepal Orthopaedic Hospital. https://www.noh.org.np/. Accessed 6 Aug 2022.
Jain K, Murphy PN, Clough TM. Platelet rich plasma versus corticosteroid injection for plantar fasciitis: a comparative study. Foot. 2015;25:235–7.
Kim J, Shin W. How to do random allocation (randomization). Clin Orthop Surg. 2014;6:103–9.
Chaudhary NK, Sunuwar DR, Sharma R, Karki M, Timilsena MN, Gurung A et al. The effect of pre-operative carbohydrate loading in femur fracture: a randomized controlled trial. BMC Musculoskelet Disord. 2022;23.
Nishanth S, Vikram S, Siddharth S. A comparative prospective study of platelet Rich plasma vs. corticosteroid injection in Plantar Fasciitis not responding to 6 weeks of conservative treatment. Int J Foot Ankle. 2018;2:1–9.
Sengodan VC, Thiagarajan N, Raajendiren IP. Evaluating the efficacy of platelet Rich plasma injection for the treatment of chronic Plantar Fasciitis. J Nat Sci Biol Med. 2020;11:135–9.
Van Lieshout EMM, De Boer AS, Meuffels DE, Den Hoed PT, Van Der Vlies CH, Tuinebreijer WE et al. American Orthopaedic Foot and Ankle Society (AOFAS) Ankle-Hindfoot Score: A study protocol for the translation and validation of the Dutch language version. BMJ Open. 2017;7.
Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF. Arthritis Care Res. 2011;63 SUPPL. 11:240–52.
Aggarwal P, Jirankali V, Garg SK. Evaluation of plantar fascia using high-resolution ultrasonography in clinically diagnosed cases of plantar fasciitis. Pol J Radiol. 2020;85:e375–80.
Hynes JP, Kavanagh EC. Complications in image-guided musculoskeletal injections. Skeletal Radiol. 2022;51:2097–104.
Stout A, Friedly J, Standaert CJ. Systemic absorption and side Effects of locally injected glucocorticoids. PM R. 2019;11:409–19.
Kallock E, Neher JO, Anna LS. Do intra-articular steroid injections affect glycemic control in patients with diabetes? Clin Inq. 2010.
Catalano LW, Glickel SZ, Barron OA, Harrison R, Marshall A, Purcelli-Lafer M. Effect of local corticosteroid injection of the hand and wrist on blood glucose in patients with diabetes mellitus. Orthopedics. 2012;35.
Kim C, Cashdollar MR, Mendicino RW, Catanzariti AR, Fuge L. Incidence of Plantar Fascia Ruptures following corticosteroid injection. Foot Ankle Spec. 2010;3:335–7.
Bani Hani DA, Alawneh KZ, Aleshawi AJ, Ahmad AI, Raffee LA, Alhowary A ”A, et al. Successful and complete recovery of the Ulnar nerve after eight years of chronic Injury through local steroid injections: a Case Report. Pain Ther. 2020;9:327–32.
Park SK, Choi YS, Kim HJ. Hypopigmentation and subcutaneous fat, muscle atrophy after local corticosteroid injection. Korean J Anesthesiol. 2014;65 6 SUPPL.
Gupta A, Garg M, Johnson N, Vignesh P. Hypopigmentation after intra-articular corticosteroid injection. BMJ Case Rep. 2019;12.
Jang WS, Park J, Yoo KH, Han TY, Li K, Seo SJ, et al. Branch-shaped cutaneous hypopigmentation and atrophy after intralesional triamcinolone injection. Ann Dermatol. 2011;23:111–4.
Salvatierra ARA, Alweis R. Permanent hypopigmentation after triamcinolone injection for tennis elbow. J Community Hosp Intern Med Perspect. 2016;6:31814.
Margulies SL, Morris A. Successful treatment of lipoatrophy with normal saline. JAAD Case Reports. 2015;1:415–7.
Monto RR. Platelet-rich plasma efficacy versus corticosteroid injection treatment for chronic severe plantar fasciitis. Foot Ankle Int. 2014;35:313–8.
Wang C, Zhang Z, Ma Y, Liu X, Zhu Q. Platelet-rich plasma injection vs corticosteroid injection for conservative treatment of rotator cuff lesions. Med (Baltim). 2021;100:e24680.
Yun Q, Qixin H, Wei C, Jialin S, Xiaotian Z, Yuanming O et al. Platelet-Rich Plasma Derived Growth Factors Contribute to Stem Cell Differentiation in Musculoskeletal Regeneration. Front Chem. 2017;5.
Malanga GA, Goldin M. PRP: review of the current evidence for musculoskeletal conditions. Curr Phys Med Rehabil Reports. 2014;2:1–15.
Ayhan E, Kesmezacar H, Akgun I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop. 2014;5:351–61.
Latt LD, Jaffe DE, Tang Y, Taljanovic MS. Evaluation and Treatment of Chronic Plantar Fasciitis. Foot Ankle Orthop. 2020;5.
Soraganvi P, Nagakiran KV, Raghavendra-Raju RP, Anilkumar D, Wooly S, Basti BD, et al. Is platelet-rich plasma injection more effective than steroid injection in the treatment of chronic plantar fasciitis in achieving long-term relief? Malaysian Orthop J. 2019;13:8–14.
Ahn JH, Lee CW, Park CJ, Kim YC. Ultrasonographic examination of plantar fasciitis: A comparison of patient positions during examination. J Foot Ankle Res. 2016;9.
Kalia RB, Singh V, Chowdhury N, Jain A, Singh SK, Das L. Role of platelet Rich plasma in Chronic Plantar Fasciitis: a prospective study. Indian J Orthop. 2021;55:142–8.
McMillan AM, Landorf KB, Gilheany MF, Bird AR, Morrow AD, Menz HB. Ultrasound guided corticosteroid injection for plantar fasciitis: Randomised controlled trial. BMJ. 2012;344.
Abdul Ameer LA, Raheem ZJ, Abdulrazaq SS, Ali BG, Nasser MM, Khairi AWA. The anti-inflammatory effect of the platelet-rich plasma in the periodontal pocket. Eur J Dent. 2018;12:528–31.
Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life. 2021;11.
Peerbooms JC, Lodder P, den Oudsten BL, Doorgeest K, Schuller HM, Gosens T. Positive effect of platelet-rich plasma on Pain in Plantar Fasciitis: a double-blind Multicenter Randomized Controlled Trial. Am J Sports Med. 2019;47:3238–46.
Mulshine JL, Chow G, Tauler J. Cytokines and growth factors stimulate hyaluronan production: Role of hyaluronan in epithelial to mesenchymal-like transition in non-small cell lung cancer. J Biomed Biotechnol. 2010;2010.
Cook CS, Smith PA. Clinical update: why PRP should be your first choice for injection therapy in treating osteoarthritis of the knee. Curr Rev Musculoskelet Med. 2018;11:583–92.
Alves R, Grimalt R. A review of platelet-rich plasma: history, Biology, mechanism of Action, and classification. Ski Appendage Disord. 2018;4:18–24.
Harrison TE, Bowler J, Levins TN, Reeves KD, Cheng A-L. Platelet-Rich Plasma Centrifugation Changes Leukocyte Ratios. Cureus. 2021;13.
Wheeler P. Surgery for Patients With Recalcitrant Plantar Fasciitis. Orthop J Sport Med. 2014;2.
Kumar V, Millar T, Murphy PN, Clough T. The treatment of intractable plantar fasciitis with platelet-rich plasma injection. Foot. 2013;23:74–7.
Taş S, Bek N, Ruhi Onur M, Korkusuz F. Effects of Body Mass Index on Mechanical Properties of the Plantar Fascia and Heel pad in asymptomatic participants. Foot Ankle Int. 2017;38:779–84.
Gupta V, Parihar A, Pathak M, Sharma V. Comparison of platelet-rich plasma prepared using two methods: manual double spin method versus a commercially available automated device. Indian Dermatol Online J. 2020;11:575–9.
Acknowledgements
We would like to heartily thank the administration and laboratory department of Nepal Orthopaedic Hospital, Kathmandu, Nepal who cooperated in the data collection and the study participants who volunteered to participate in this study.
Funding
This research was carried out under the Nepal Health Research Council (NHRC) funding under the Provincial Research Grant (Grant number: 116/2021).
Author information
Authors and Affiliations
Contributions
All the authors contributed to manuscript preparation and editing. RS: conceptualization, study design, methodology application, recruitment, intervention, data collection, outcome assessment, project administration, validation, and manuscript editing. NKC: conceptualization, study design, methodology application, data curation, formal analysis, data interpretation, software utilization, manuscript drafting, and editing. MK: conceptualization, study design, methodology application, recruitment, intervention, data collection, outcome assessment, project administration, validation, and manuscript editing. DRSu: conceptualization, study design, methodology application, data curation, formal analysis, data interpretation, software utilization, manuscript editing, and critical review. DRSi: data interpretation, manuscript editing, and critical review. PMSP: critical review, editing, and overall monitoring and supervision. PG: methodology application, project administration, validation, and manuscript editing SKDS: methodology application, project administration, validation, and manuscript editing KKB: methodology application, project administration, validation, supervision, and manuscript editing. All of the authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
We confirm that all methods were carried out following relevant guidelines and regulations. The ethical approval was obtained from the Ethical Review Board (ERB) of the Nepal Health Research Council (NHRC), Nepal (Reg. Number: 3322, approved on 06/06/2021). The clinical trial registry was done with Clinical Trial.gov (Identifier: NCT04985396), registered on 02/08/2021). Participants were recruited under study only after obtaining written consent. Those patients who provided written informed consent were included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sharma, R., Chaudhary, N.K., Karki, M. et al. Effect of platelet-rich plasma versus steroid injection in plantar fasciitis: a randomized clinical trial. BMC Musculoskelet Disord 24, 172 (2023). https://doi.org/10.1186/s12891-023-06277-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06277-1