Abstract
Background
Minimal important difference (MID) is a concept used inconsistently and arbitrarily in tendinopathy research. Our aim was to determine the MIDs for the most commonly used tendinopathy outcome measures using data-driven approaches.
Methods
Recently published systematic reviews of randomised controlled trials (RCTs) on tendinopathy management were identified and used for extraction of eligible studies through a literature search. Each eligible RCT was used to obtain information on MID where this was used and it also contributed data for the calculation of the baseline pooled standard deviation (SD) for each tendinopathy (shoulder, lateral elbow, patellar and Achilles). The rule of “half SD” was used for the computation of MIDs for patient-reported pain (visual analogue scale, VAS 0–10, single-item questionnaire) and function (multi-item questionnaires) and the rule of “one standard error of measurement (SEM)” was additionally used for the multi-item functional outcome measures.
Results
A total of 119 RCTs were included for the 4 tendinopathies. MID was defined and used by 58 studies (49%) and there were significant inconsistencies amongst studies where the same outcome measure was used as MID. From our data-driven methods the following suggested MIDs were obtained: a) Shoulder tendinopathy, pain VAS (combined) 1.3 points, Constant-Murley score 6.9 (half SD) and 7.0 (one SEM) points; b) lateral elbow tendinopathy, pain VAS (combined) 1.0 point, Disabilities of Arm, Shoulder and Hand questionnaire 8.9 (half SD) and 4.1 (one SEM) points; c) Patellar tendinopathy, pain VAS (combined) 1.2 points, Victorian Institute of Sport Assessment – Patella (VISA-P) 7.3 (half SD) and 6.6 points (one SEM); d) Achilles tendinopathy, pain VAS (combined) 1.1 points, VISA-Achilles (VISA-A) 8.2 (half SD) and 7.8 points (one SEM). The rules of half SD and one SEM produced very similar MIDs except for DASH due to its very high internal consistency. MIDs were also calculated for different pain settings for each tendinopathy.
Conclusions
Our computed MIDs can be used in tendinopathy research to increase consistency. Clearly defined MIDs should be used with consistency in tendinopathy management studies in the future.
Similar content being viewed by others
Keypoints
We provide proposed MIDs for patient-reported instruments in tendinopathy using data-driven approaches, which had not previously been used for this purpose.
We call for the complicated, yet important concept of MID to receive greater attention in the future from researchers, publishing journals and outcome measure creators.
Both anchor- and data-driven methods have their strengths and drawbacks and a “hybrid” approach using aspects from both may be best.
Introduction
The concept of minimal clinically important difference (MCID) was introduced by Jaeschke et al. (1989) and was defined as “the smallest difference in score in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in the patient's management” [1]. The authors used global ratings of change (GROC) to establish plausible ranges within which the MCID should fall, and their argument for the relevance of MCID was that statistically significant changes during use of instruments assessing interventions do not always translate to clinically important differences. With the constant emergence of patient-reported outcome measures over the last decades, the use of MCID is becoming increasingly relevant and important; however, the concept of MCID in research remains controversial because of its inherent complexity and difficulty defining.
A minimal important difference (MID), which represents the minimum meaningful change of an outcome measure, should not be confused with the smallest/minimum detectable change (SDC or MDC), which is a measure of the measurement error of the instrument [2]. A change in any given score can only be considered to represent a real change when it’s larger than the SDC [2]. A MID should only be referred to as MCID when clinical methods are used for its computation [3]. The term MID will be used throughout the present article as only non-clinical data-driven methods were employed.
In tendinopathy, the existence of a myriad outcome measures and the continuous introduction of new interventions necessitate objective and consistent assessment of their effectiveness. The use of MID is relevant both in research and clinical practice in the following contexts: a) as part of the power calculation in clinical trials; b) as part of strength of evidence assessment in systematic reviews (e.g. assessment of “imprecision” using the GRADE (Grading of Recommendations, Assessment, Development and Evaluations) tool); c) deciding on the effectiveness of assessed interventions in clinical trials, combined with statistical significance; and d) in clinical practice to assess improvement and guide management [4]. In the existing tendinopathy literature, MIDs have mostly been used arbitrarily and inconsistently [5,6,7].
Various different methods have been used in the literature for determining MIDs. These are largely divided into “within patients” and “across groups of patients” methods or into data-driven (distribution-based) and anchor-based methods. Anchor-based approaches consider patient perspectives (or less commonly clinician perspectives) and they are the most frequently used methods for the computation of MIDs [8]. Data-driven approaches consider changes within individuals, as opposed to changes across groups, and the main one is “the rule of one standard error of measurement (SEM)’’ as proposed by Wyrwich et al. (1999), who validated this method against Jaeschke’s approach and cutpoints [9]. The main advantage of this approach is that it is standardised and the least subjective as it considers the internal consistency of the instrument itself and the baseline standard deviation (SD) of the population of interest and is the least dependent on population characteristics. This was subsequently simplified as “the rule of half SD”, according to which the MID of most instruments or scales is very close to a value of half the baseline SD of the studied population [10,11,12]. Its main disadvantage compared to anchor-based methods, which usually use GROC as the “anchor”, is that they do not consider the importance of the observed change [13].
Our aim with the present study was two-fold: a) to investigate and present what previously published tendinopathy trials defined as MID and see whether their use has been consistent; and b) to determine MID values for patient-reported pain and commonly used patient-reported function scales for shoulder, lateral elbow, patellar and Achilles tendinopathies separately using data-driven approaches. We expect this will be helpful for future research and clinical practice in tendinopathy, will provide further insights into computation of MID and will enhance consistency and comparability among clinical trials.
Methods
Eligibility
Studies were eligible if they were randomised controlled trials (RCTs), included patients with shoulder, lateral elbow, patellar or mid-portion Achilles tendinopathy and reported variability statistics (SD; standard error of mean, SEMean; confidence interval, CI; interquartile range, IQR) of the outcomes of interest at baseline. The tendinopathy locations were chosen as the four most prevalent. Studies on insertional Achilles tendinopathy were excluded as it represents a separate pathological condition.
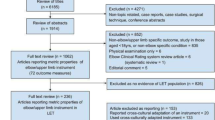
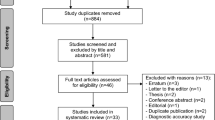
Study identification
Eligible studies were identified using previously published systematic reviews of RCTs for each tendinopathy. Searches were conducted separately for each tendinopathy in Medline with the following boolean operators used in “all fields”: a) (Patellar tendin* OR Patellar tendin jumper’s knee) AND (review OR systematic review OR meta-analysis); b) Achilles tendin* OR Achilles tendon*) AND (review OR systematic review OR meta-analysis); c) (Elbow tendin* OR elbow tendon* OR tennis elbow OR lateral epicondyl*) AND (review OR systematic review OR meta-analysis); d) (shoulder tendin* OR shoulder tendon* OR rotator cuff tendin* OR rotator cuff tendon* OR subacromial impingement OR subacromial pain) AND (review OR systematic review OR meta-analysis).
The searches were not systematic as the aim was not to identify all eligible RCTs; we aimed to identify a sufficient number of studies for a sufficiently large, combined population size (at least 200 patients for each instrument). We chose to include RCTs instead of observational studies for two reasons: a) the power calculations used in RCTs was used for the first part of our study looking at definition of MIDs; b) RCTs are generally superior methodologically and their baseline measurements are therefore more likely to be accurate. The largest, recently published systematic reviews of RCTs were selected for each one of the 4 tendinopathies.
Outcome measures
The primary outcome for which MIDs were to be determined was patient-reported pain (visual analogue scale, VAS, or equivalent). The secondary outcome was function/functional disabilities; for each tendinopathy, the instruments used were those most commonly encountered in the included RCTs.
Data handling
For each RCT, the following data were extracted and tabulated into Microsoft Excel: a) sample size of each treatment group, b) baseline mean and standard deviation for each outcome measure of interest, and c) what the study authors defined as MID for their power calculation where that was performed. Follow up study data were ignored as they were irrelevant for the purposes of our study.
The MIDs of each outcome measure of interest were calculated as follows:
-
a)
for all outcome measures (single-item and multi-item patient-reported) the MID was assumed to be equal to half the pooled SD at baseline based on the rule of half SD [5]; where the reliability of the instrument is very high (which is generally the case for single-item outcome measures, such as pain VAS), using the one SEM rule would result in a very small value of MID and therefore the half SD threshold is a more stringent criterion [10].
-
b)
for multi-item patient-reported outcome measures (e.g. Victorian Institute of Sport Assessment, VISA), the one SEM rule was also used to calculate the MID to see how that compares to the corresponding value deriving from the rule of half SD [10]. Cronbach’s alpha was used as an internal consistency measure in the equation.
The SEM is a statistic used to estimate how reliably an instrument measures an individual’s “true score”. The Cronbach’s alpha, which measures the internal consistency of an instrument, is the degree of the inter-relatedness among the items of the instrument [14]. In contrast to test–retest statistics (e.g. intraclass correlation coefficient, ICC), using Cronbach’s alpha is especially useful when the assessed parameters can change over short periods of time [15].
For each tendinopathy separately, pooled SDs of VAS at the most commonly reported specific settings (e.g. at rest, with activity etc.) were also computed and presented separately where there was a sufficiently large pooled population size (n > 200 patients). We standardised pain VAS scores by using an 11-point scale (0–10) as this was the most commonly used scale; where a 0–100 scale was used by studies, reported values were converted to their equivalent on a 0–10 scale by dividing them by “10”.
Statistical analysis
All variability statistics were converted to SDs. When IQRs or data ranges were reported, the SD was calculated as IQR divided by 1.35 and length of range divided by 4 respectively. When CIs of means were reported, SDs were calculated by dividing the length of the CI by 3.92 and then multiplying by the square root of the sample size. When SEmean was given, this were converted to SD by multiplying it by the square root of the sample size.
Pooled SDs were calculated with the following formula: SDpooled = √(SD12[n1-1]) + (SD22[n2-1]) + … + (SDk2[nk-1]) / (n1 + n2 + … + nk – k), where n indicates sample size and k, the number of samples.
SEM for each multi-item patient-reported outcome measure was calculated with the formula:
SEM = SD√ (1-rxx), where rxx is the internal consistency of the scale (Cronbach’s alpha coefficient) and SD the pooled SD for that instrument from the included RCTs. The Cronbach’s alpha coefficient for each instrument was obtained from reliability data in the published literature and where more than one studies reported internal consistency values (e.g. different language versions of the instrument), the average of these values was calculated and used [16,17,18,19,20,21,22,23,24].
Results
A total of 119 RCTs (Supplementary Table 1) were included and reviewed for all 4 tendinopathies [25,26,27,28]. MID was defined and used by 58 studies (49%), of which only 20% provided a reference to justify their chosen MID (studies that previously used it or studies that computed it with anchor-based methods). Data for each tendinopathy are presented below.
Shoulder tendinopathy
A total of 33 studies were reviewed, of which 8 (24%) defined and used MIDs [25]. One study used MID for two outcomes. Thirty (30) studies contributed data to pain VAS (106 samples, pooled population 3404 patients). The most common settings where pain was reported were “at rest” (10 studies, 22 samples, pooled population n = 567 patients) and “with activity/movement” (13 studies, 28 samples, population n = 695 patients). The most commonly used functional instrument was the Constant Murley Score (CMS; 15 studies, 32 samples, pooled population n = 1412 patients),
Criteria used for MID were as follows: n = 2 pain VAS 1.4 points, n = 1 pain VAS 1.3 points, n = 1 quick Disabilities of Arm, Shoulder and Hand (qDASH) questionnaire 8 points, n = 1 Adolfsson-Lysholm (AL) shoulder assessment score 15 points, n = 1 shoulder disability questionnaire (SDQ) 3 points, n = 1 shoulder pain and disability index (SPADI) 19.6 points, n = 1 CMS 9–10 points, n = 1 University of California Los Angeles (UCLA) shoulder score 5 points.
Lateral elbow tendinopathy
A total of 21 studies were reviewed [26]. Of these, 8 (38%) defined and used MIDs. Twelve (12) studies contributed data to pain VAS (38 samples, pooled population n = 1704 patients). The most common settings where pain was reported were “worst” (6 studies, 17 samples, pooled population n = 614 patients) and “at rest” (4 studies, 11 samples, pooled population n = 361 patients). The most commonly used functional instrument was the Disabilities of the Arm, Shoulder and Hand (DASH) scale (4 studies, 9 samples, pooled population n = 316 patients).
Criteria used as MID were as follows: n = 1 37% improvement in patient-rated tennis elbow evaluation (PRTEE) score, n = 1 between-group difference of 6.8 kg in pain-free grip strength, n = 1 13 points improvement in PRTEE, n = 1 40% improvement in DASH score, n = 1 “50% improvement in lateral epicondylalgia cases in the treatment group vs 10% reduction in the control group”, n = 1 “50% improvement from baseline”, n = 1 “difference in success rate of 25% with the least effective treatment”, n = 1 “effect size of 1 on PRTEE questionnaire”.
Patellar tendinopathy
A total of 37 studies were reviewed, of which 22 (59%) defined and used MIDs [27]. Three studies used MID for two outcomes. Twenty-seven (27) studies contributed data to pain (92 samples, pooled population n = 1736 patients). The most common setting where pain was reported was “with single leg decline squat” (8 studies, 16 samples, pooled population n = 306 patients). The most commonly used functional instrument was VISA-Patella (VISA-P; 30 studies, 63 samples, pooled population n = 1120 patients).
Criteria used as MID were as follows: n = 8 VISA-P 13 points, n = 4 VISA-P 15 points, n = 4 VISA-P 20 points, n = 1 VISA-P 11 points, n = 5 pain VAS 2 points, n = 1 pain VAS 5 points, n = 1 12-item short-form survey (SF-12) 6.8 points, n = 1 short-form McGill pain questionnaire (SF-MPQ) 4.54 points.
Achilles tendinopathy
A total of 28 studies were reviewed; 20 (71%) of them defined and used MID [28]. Nineteen (19) studies contributed data to pain (45 samples, pooled population n = 1090 patients) with the most commonly used settings being “pain at rest” (11 studies, 27 samples, pooled population n = 569 patients) and “with activity” (4 studies, 9 samples, pooled population n = 295 patients). The most commonly used functional instrument was VISA-Achilles (VISA-A; 18 studies, 41 samples, pooled population n = 1008 patients).
Criteria used for MID were as follows: n = 7 VISA-A 10 points, n = 3 VISA-A 20 points, n = 2 VISA-A 16 points, n = 1 VISA-A 20 points, n = 1 pain VAS 1 point, n = 1 pain VAS 1.2 points, n = 2 pain VAS 10% change, n = 1 pain VAS 1.5 points, n = 1 pain VAS 2 points, n = 1 pain VAS 2–3 points.
Our computed MIDs for each tendinopathy are presented in Table 1, which also shows the method used for the calculation and other relevant data.
Discussion
To our knowledge, this is the first study using data-driven approaches to determine MIDs for tendinopathies. Our computed MIDs can be used along with those previously calculated from anchor-based approaches to guide further relevant research.
The concept of MID remains controversial and poorly used. In the present study, fewer than half of the included RCTs defined and used a MID for their power calculation. Where the same instruments were used, we identified big discrepancies in the values used, e.g. change of VISA-A of 10 points in a study and 20 points in another. Where clinical significance is considered along statistical significance, this discrepancy will have important consequences on what magnitude of within-group or between-groups difference is considered significant. Additionally, this substantially influences the power calculation; a MID in VISA-A of 10 points will result in a much larger minimum population required to be recruited compared to a MID of 20 points.
Proposed MIDs for commonly used patient-reported function instruments in tendinopathy have been previously published using anchor-based methods. In Achilles tendinopathy, a MID of 6.5 points was previously determined by McCormack et al. (2015) for insertional tendinopathy [29]. For mid-portion Achilles tendinopathy, Lagas et al. (2021) used similar anchor-based methods in 64 patients and calculated a VISA-A MID of 14 points at 12 weeks and 7 points at 24 weeks [30]. A recent review article by Murphy et al. (2018) found that, among 46 included studies (randomised and non-randomised), the most commonly used MID for VISA-A was 10 points (n = 6), which is in agreement with our findings (n = 7) [31]. Other authors arbitrarily suggested a MID of 12 and 20 for VISA-A [32,33,34].
For patellar tendinopathy, Hernandez-Sanchez et al. (2014) used a similar approach to McCormack et al. (2015) and Lagas et al. (2021) to determine a MID for VISA-P [29, 30, 35]. They administered a VISA-P questionnaire to 98 athletes with patellar tendinopathy along with a 15-point Likert scale; important change was defined as a change of 3 points or more on the Likert scale. The respective VISA-P absolute change was 13 points, which they defined as MID. This was also equivalent to a relative change of 15.4–27% of the baseline score.
MIDs for patient-reported function instruments have not been defined for shoulder tendinopathy specifically. The CMS MID was defined as 10.4 points by Kukkonen et al. (2013) in their prospective study of patients undergoing rotator cuff surgery; they employed a “patient perspective” approach, correlating CMS scores with a simple question: “is the pain better or worse after the operation compared with the pre-operative state?” [36]. Tashjian et al. (2009) determined a MID for pain VAS in patients treated for rotator cuff disease also using an anchor-based method; they found a difference of 1.4 points in pain VAS being a change that patients perceived as clinically beneficial [37].
The DASH questionnaire was the most commonly encountered instrument assessing function in the included trials on lateral elbow tendinopathy. MIDs of 9 or 10 points have commonly been reported for the DASH questionnaire in the literature, which are very close to our MID computed using the rule of half SD (8.9 points) but significantly higher than the one calculated with the one SEM rule (4.1 points). This latter very small figure is due to the very high internal consistency of the instrument which yields a MID that is unrealistically small to represent a clinically important change for patients; therefore we would recommend the use of our result deriving from the rule of half SD (8.9 points). The DASH website recommends a MID of 15 points [38]. Farzad et al. (2020) suggested a DASH MID of 18 for patients with lateral elbow tendinopathy, having correlated DASH scores with GROC scale results in 64 patients [39]. Using a similar method in a larger population (255 patients) suffering from upper limb musculoskeletal disorders, Franchignoni et al. (2014) computed an MID of 10.83 points using an anchor-based method and a SEM of 4.63 using a data-driven method [40]. For the SEM calculation, they used test–retest reliability instead of Cronbach’s alpha coefficient. Finally, Rysstad et al. (2017) found a difference of 4.4 points in the Norwegian version of the DASH questionnaire corresponding to minimal important change, which is similar to our result deriving from the one SEM method [22]. The results of these two last studies are very similar to our own computed MID for the DASH questionnaire deriving from the one SEM method.
Studies have previously attempted to determine MIDs for patient-reported pain in the literature. In a population of 825 patients with chronic musculoskeletal pain (mostly osteoarthritis), Salaffi et al. (2004) reported a change of 1 point in the numerical rating scale (NRS, same as VAS) or a 15% improvement from baseline reflecting a slight clinical improvement based on the patients’ corresponding results in a global impression of change questionnaire and they defined this as MID [41]. However, the authors found that a change of 2 points in the pain NRS or a 33% improvement from baseline was equivalent to a “much better” outcome in the global impression of change questionnaire. Farrar et al. (2001) used a data-driven approach and found that, having used data from 2724 patients with diabetic neuropathy from 10 RCTs, a reduction of 2 points (or 30%) in pain VAS was equivalent to a “much improved” and “very much improved” outcome on GROC scales [42]. Although the authors refer to their approach as data-driven, we argue that this is a hybrid approach as they use pooled data from several studies (data-driven approach) as well as GROC scale results (anchor-based approach). We would encourage the use of different MIDs for each pain setting (e.g. with activity, with sports, at rest etc.) as we argue these represent different outcome measures.
Our data-driven methods do not come without limitations. In contrast to the more commonly employed anchor-based approaches that correlate instrument scores with patient satisfaction/improvement questionnaires, it is based purely on variability statistics of the population of interest and the intrinsic characteristics of the instrument. Indeed, VISA-A and VISA-P for example have low-quality evidence for their internal consistency. However, it eliminates subjectivity that comes with simple patient satisfaction/improvement questionnaires and, additionally, we have used large pooled populations of the same condition for each instrument to make the SD as representative of the population of interest as possible. The validity of previously used methods that utilise GROC is questionable as this may not be the best external standard of change; additionally, studies using such patient perspective methods usually have a small population which may not be representative of the wider population of interest, and finally, there may be recall bias or patients not understanding the context of improvement [29, 40]. To complicate things further, other parameters should ideally be considered for the application of MIDs, including, but not limited to, age, nature, chronicity and severity of disease, potential for improvement, type of intervention and follow up time point [40, 43]. Additionally, although we identified a large number of trials from recently published systematic reviews for each tendinopathy, our search was not systematic, therefore not all eligible studies in the literature have been included.
Finally, even though in reality MIDs may be different at various follow up time points for the same population undergoing the same intervention, setting specific MIDs for each time point will only overcomplicate things. Ranges of MIDs instead of specific values have also been suggested, which would also lead to confusion and inconsistent use, especially when they are wide [40]. Our computed MIDs can be used by clinicians and researchers in the future as they derive from reliable methodology. Going forward, triangulation methods using both anchor-based and distribution-based approaches that will produce either single values or small ranges would be the most accurate determination of MIDs. This should be further re-inforced with Delphi studies including expert clinicians involved in the management of tendinopathy and tendinopathy patient groups [3].
Conclusions
We demonstrated that MIDs are being used inconcistently in tendinopathy research. We used data-driven approaches and computed MIDs for commonly used outcome measures in shoulder, lateral elbow, patellar and Achilles tendinopathies and these can be used in both clinical and research settings. In the future, more attention should be given to the use of MIDs and their computation through the use of both anchor-based and data-driven approaches.
Availability of data and materials
Data is available from DC upon request.
References
Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Controlled Clin Trials. 1989;10:407–5.
van Kampen DA, Willems WJ, van Beers LW, Castelein RM, Scholtes VA, Terwee CB. Determination and comparison of the smallest detectable change (SDC) and the minimal important change (MIC) of four-shoulder patient-reported outcome measures (PROMs). J Orthop Surg Res. 2013;8:40.
Revicki D, Hays RD, Cella D, Sloan J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J Clin Epidemiol. 2008;61(2):102–9.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ (Clinical research ed). 2008;336(7650):924–6.
Krogh TP, Ellingsen T, Christensen R, Jensen P, Fredberg U. Ultrasound-guided injection therapy of Achilles tendinopathy with platelet-rich plasma or saline: a randomized, blinded Placebo-controlled trial. Am J Sports Med. 2016;44(8):1990–7.
Munteanu SE, Scott LA, Bonanno DR, Landorf KB, Pizzari T, Cook JL, Menz HB. Effectiveness of customised foot orthoses for Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2015;49(15):989–94.
Pearson J, Rowlands D, Highet R. Autologous blood injection to treat achilles tendinopathy? A randomized controlled trial. J Sport Rehabil. 2012;21(3):218–24.
Wells G, Beaton D, Shea B, Boers M, Simon L, Strand V, Brooks P, Tugwell P. Minimal clinically important differences: review of methods. J Rheumatol. 2001;28(2):406–12.
Wyrwich KW, Nienaber NA, Tierney WM, Wolinsky FD. Linking clinical relevance and statistical significance in evaluating intra-individual changes in health-related quality of life. Med Care. 1999;37(5):469–78.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92.
Howard R, Phillips P, Johnson T, O’Brien J, Sheehan B, Lindesay J, Bentham P, Burns A, Ballard C, Holmes C, et al. Determining the minimum clinically important differences for outcomes in the DOMINO trial. Int J Geriatr Psychiatry. 2011;26(8):812–7.
Ballard C, Banister C, Khan Z, Cummings J, Demos G, Coate B, Youakim JM, Owen R, Stankovic S, Tomkinson EB, et al. Evaluation of the safety, tolerability, and efficacy of pimavanserin versus placebo in patients with Alzheimer’s disease psychosis: a phase 2, randomised, placebo-controlled, double-blind study. The Lancet Neurology. 2018;17(3):213–22.
de Vet HC, Terwee CB, Ostelo RW, Beckerman H, Knol DL, Bouter LM. Minimal changes in health status questionnaires: distinction between minimally detectable change and minimally important change. Health Qual Life Outcomes. 2006;4:54.
Mokkink LB, Terwee CB, Patrick DL, Alonso J, Stratford PW, Knol DL, Bouter LM, de Vet HC. The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. J Clin Epidemiol. 2010;63(7):737–45.
Roddey TS, Olson SL, Cook KF, Gartsman GM, Hanten W. Comparison of the University of California-Los Angeles shoulder scale and the simple shoulder test with the shoulder pain and disability index: single-administration reliability and validity. Phys Ther. 2000;80(8):759–68.
Palazón-Bru A, Tomás Rodríguez MI, Mares-García E, Hernández-Sánchez S, Carbonell-Torregrosa MÁ, Gil-Guillén VF. The Victorian Institute of Sport Assessment Scale for Patellar Tendinopathy (VISA-P): a reliability generalization meta-analysis. Clin J Sport Med. 2021;31(5):455–64.
Robinson JM, Cook JL, Purdam C, Visentini PJ, Ross J, Maffulli N, Taunton JE, Khan KM, Victorian Institute Of Sport Tendon Study Group. The VISA-A questionnaire: a valid and reliable index of the clinical severity of Achilles tendinopathy. Br J Sports Med. 2001;35(5):335–41.
Roy JS, MacDermid JC, Woodhouse LJ. A systematic review of the psychometric properties of the Constant-Murley score. J Shoulder Elbow Surg. 2010;19(1):157–64.
Maqdes A, Hanna SS, Bouhamra AK, Khaja AF. Cross-cultural adaptation and translation of the Constant Murley score into Arabic. SICOT J. 2020;6:44.
Vrotsou K, Ávila M, Machón M, Mateo-Abad M, Pardo Y, Garin O, Zaror C, González N, Escobar A, Cuéllar R. Constant-Murley Score: systematic review and standardized evaluation in different shoulder pathologies. Qual Life Res. 2018;27(9):2217–26.
Carosi M, Galeoto G, Gennaro SD, Berardi A, Valente D, Servadio A. Transcultural reliability and validity of an Italian language version of the Constant–Murley Score. J Orthop Trauma Rehab. 2020;(214):186–91.
Rysstad T, Røe Y, Haldorsen B, Svege I, Strand LI. Responsiveness and minimal important change of the Norwegian version of the Disabilities of the Arm, Shoulder and Hand questionnaire (DASH) in patients with subacromial pain syndrome. BMC Musculoskelet Disord. 2017;18(1):248.
Fernandes MR, Barbosa MA, Faria RM. Quality of life and functional capacity of patients with adhesive capsulitis: identifying risk factors associated to better outcomes after treatment with nerve blocking. Rev Bras Reumatol Engl Ed. 2017;57(5):445–51.
Kitis A, Celik E, Aslan UB, Zencir M. DASH questionnaire for the analysis of musculoskeletal symptoms in industry workers: a validity and reliability study. Appl Ergon. 2019;40:251–5.
Dong W, Goost H, Lin XB, Burger C, Paul C, Wang ZL, Zhang TY, Jiang ZC, Welle K, Kabir K. Treatments for shoulder impingement syndrome: a PRISMA systematic review and network meta-analysis. Medicine (Baltimore). 2015;94(10): e510.
Karanasios S, Korakakis V, Whiteley R, Vasilogeorgis I, Woodbridge S, Gioftsos G. Exercise interventions in lateral elbow tendinopathy have better outcomes than passive interventions, but the effects are small: a systematic review and meta-analysis of 2123 subjects in 30 trials. Br J Sports Med. 2021;55(9):477–85.
Challoumas D, Pedret C, Biddle M, Ng NYB, Kirwan P, Cooper B, Nicholas P, Wilson S, Clifford C, Millar NL. Management of patellar tendinopathy: a systematic review and network meta-analysis of randomised studies. BMJ Open Sport Exerc Med. 2021;7(4): e001110.
van der Vlist AC, Winters M, Weir A, Ardern CL, Welton NJ, Caldwell DM, Verhaar JAN, de Vos RJ. Which treatment is most effective for patients with Achilles tendinopathy? A living systematic review with network meta-analysis of 29 randomised controlled trials. Br J Sports Med. 2021;55(5):249–56.
McCormack J, Underwood F, Slaven E, Cappaert T. The minimum clinically important difference on the VISA-A and Lefs for patients with Insertional Achilles Tendinopathy. Int J Sports Phys Ther. 2015;10(5):639–44.
Lagas IF, van der Vlist AC, van Oosterom RF, van Veldhoven PLJ, Reijman M, Verhaar JAN, de Vos RJ. Victorian Institute of Sport Assessment-Achilles (VISA-A) questionnaire-minimal clinically important difference for active people with midportion achilles tendinopathy: a prospective cohort study. J Orthop Sports Phys Ther. 2021;51(10):510–6.
Murphy M, Rio E, Debenham J, Docking S, Travers M, Gibson W. Evaluating the progress of MID-Portion Achilles tendinopathy during rehabilitation: a review of outcome measures for self- reported pain and function. Int J Sports Phys Ther. 2018;13(2):283–92 PMID: 30090686; PMCID: PMC6063067.
Tumilty S, Munn J, Abbott JH, McDonough S, Hurley DA, Baxter GD. Laser therapy in the treatment of achilles tendinopathy: a pilot study. Photomed Laser Surg. 2008;26(1):25–30.
de Vos RJ, Weir A, van Schie HT, Bierma-Zeinstra SM, Verhaar JA, Weinans H, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy: a randomized controlled trial. JAMA. 2010;303:144–9.
Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles tendinopathy. J Sci Med Sport. 2007;10(1):52–8.
Hernandez-Sanchez S, Hidalgo MD, Gomez A. Responsiveness of the VISA-P scale for patellar tendinopathy in athletes. Br J Sports Med. 2014;48(6):453–7.
Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aärimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22(12):1650–5.
Tashjian RZ, Deloach J, Porucznik CA, Powell AP. Minimal clinically important differences (MCID) and patient acceptable symptomatic state (PASS) for visual analog scales (VAS) measuring pain in patients treated for rotator cuff disease. J Shoulder Elbow Surg. 2009;18(6):927–32.
Institute for Work and Health. Disabilities of the Arm, Shoulder and Hand outcome measure. Available at: http://www.dash.iwh.on.ca/. Accessed 25 July 2013.
Farzad M, MacDermid JC, Shafiee E, Beygi AS, Vafaei A, Varahra A, Beikpour H. Clinimetric testing of the Persian version of the Patient-Rated Tennis Elbow Evaluation (PRTEE) and the Disabilities of the Arm, Shoulder, and Hand (DASH) questionnaires in patients with lateral elbow tendinopathy. Disabil Rehabil. 2020;(14):1–6.
Franchignoni F, Vercelli S, Giordano A, Sartorio F, Bravini E, Ferriero G. Minimal clinically important difference of the disabilities of the arm, shoulder and hand outcome measure (DASH) and its shortened version (QuickDASH). J Orthop Sports Phys Ther. 2014;44(1):30–9.
Salaffi F, Stancati A, Silvestri CA, Ciapetti A, Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8(4):283–91.
Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58.
Wang YC, Hart DL, Stratford PW, Mioduski JE. Baseline dependency of minimal clinically important improvement. Phys Ther. 2011;91:675–88.
Acknowledgements
None
Funding
This work was funded by Medical Research Council grant MR/R020515/1 (NLM).
Author information
Authors and Affiliations
Contributions
DC, GC conceived and designed the study. DC,AZ,KC,EM,GC and NN, performed analysis. NLM provided expert advice. All authors analysed the data. DC,AZ,KC,EM,GC and NN and NLM wrote the paper. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Challoumas, D., Zouvani, A., Creavin, K. et al. Determining minimal important differences for patient-reported outcome measures in shoulder, lateral elbow, patellar and Achilles tendinopathies using distribution-based methods. BMC Musculoskelet Disord 24, 158 (2023). https://doi.org/10.1186/s12891-023-06261-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-023-06261-9