Abstract
Background
Pain due to knee and / or hip osteoarthritis (HKOA) is the most common symptom for seeking healthcare. Pain interferes on daily activities, social and occupational participation in people with HKOA. The goal of this study is to estimate the prevalence of unmanageable pain levels (UPL) among people with HKOA), characterize this population and identify factors associated with UPL, and compare therapeutic strategies used by people with UPL versus manageable pain levels (MPL).
Methods
We analysed data from the EpiReumaPt study (n = 10,661), that included a representative sample of the Portuguese population. Among these, 1081 participants had a validated diagnosis of HKOA by a rheumatologist.. Sociodemographic, lifestyle and health-related data were collected in a structured interview. Pain intensity (NPRS) data were collected in a medical appointment. Painmedication (last month), physiotherapy and surgery were considered as therapies for pain management. UPL was defined as a mean pain intensity in the previous week of ≥5 points on 11-point numeric pain rating scale. The factors associated with UPL were analyzed with logistic regression (p < 0.05, 95%CI). The effect of unmanageable pain levels was assessed by the HOOS/KOOS activities of daily living and quality of life subscales. Symptoms of anxiety and depression were assessed by the Hospital Anxiety and Depression Scale (HADS). Analysis was completed with linear and logistic regression. All analysis were weighted.
Results
The estimated prevalence of UPL among people with HKOA was 68.8%. UPL was associated with being female (odds ratio (OR) = 2.36, p < 0.001), being overweight (OR = 1.84, p = 0.035) or obese (OR = 2.26, p = 0.006), and having multimorbidity (OR = 2.08, p = 0.002). People with UPL reported worse performance in activities of daily living and lower quality of life (β = − 21.28, p < 0.001 and β = − 21.19, p < 0.001, respectively) than people with MPL. People with UPL consumed more NSAIDs (22.0%, p = 0.003), opioids (4.8%, p = 0.008), paracetamol (2.7%, p = 0.033), and overall analgesics (7.3%, p = 0.013) than people with MPL. A higher proportion of people with UPL underwent physiotherapy (17.5%, p = 0.002) than people with MPL.
Conclusion
Two-thirds of people with HKOA in Portugal have poor management of their pain levels. Clinical and lifestyle factors, that are highly presented in individuals with HKOA, are associated with unmanageable pain. Our results highlighting the need for further research and implementation of effective interventions to improve pain, function and quality of life in people with HKOA.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is the most common joint disease, affecting more than 300 million people worldwide. The hip and knee joints are the most affected and combined reflect 9.6 million years lived with disability [1]. The direct annual costs of hip and/or knee OA (HKOA) per patient are estimated at 6.7 K€ worldwide, which reaches 10.8 K€ if total joint replacement surgery is considered [2]. Indirect annual costs per patient are estimated between 0.2 K–12.3 K€. In Portugal, indirect costs represent 0.4% of the national gross domestic product [3]. Moreover, the incidence of total joint replacement surgery in Portugal has increased by 20% annually in the period between1990–2011, which represents the highest growth rate among Organisation for Economic Co-operation and Development countries [4].
HKOA often results with chronic pain, physical disability, and mental health and sleep problems, which impairs quality of life (QoL) and prevents participation in social and occupational activities [5]. Pain is the most disabling symptom of OA and a major driver of clinical decision-making and healthcare resources [5].
Pain severity is more indicative of functional impairment than radiographic severity [6,7,8]. Pain severity is also strongly associated with reported disability, medication use [9, 10], healthcare utilization, impact on daily and occupational activities, loss of productivity, early retirement, and absenteeism [11, 12]. Poor pain management is a major predictor of total joint replacement surgery [13].
Recent literature raises concerns over the pain management and low QoL among people with HKOA [10, 14]. Current pain management focus on symptom control that incorporates medication as the first-line intervention increases the risk of opioid prescription [14, 15]. The use of end-stage interventions such as surgery is becoming more common, even among people with early-stage OA [14, 15]. The knowledge of pain management and therapeutic strategies in Portugal is scarce. There is a critical need to better understand patients’ associated risk factors, characteristics, and available therapeutic interventions for people enduring HKOA in Portugal. Therefore, the aims of this study were to: 1) estimate the prevalence of unmanageable pain levels (UPL) among Portuguese population with HKOA, 2) characterize the HKOA population in terms of sociodemographic, lifestyle, and health-related variables and identify factors associated with UPL; and 3) compare performance in activities of daily living (ADL), QoL, anxiety and depression symptoms, and therapies used between people with UPL versus people with manageable pain levels (MPL). This knowledge will help to understand which factors undermine patient’s ability to manage pain levels and how traditional therapies used either facilitate or fail to facilitate successful management of pain. The results of this study may also indicate whether the associated therapeutic interventions account for the factors associated with poor pain management and if improvements in offered interventions to people with HKOA are needed.
Methods
Data source
We analysed data from the EpiReumaPt, a national cross-sectional, population based study with a representative sample of the Portuguese population that aimed to investigate the burden of rheumatic and musculoskeletal diseases (RMDs) in Portugal. As described in detail elsewhere [16], participant recruitment was conducted between September 2011 and December 2013 using a random selection of private households in Portugal stratified by administrative territorial units (NUTS II: Norte, Centro, Lisboa and Vale do Tejo, Alentejo, Algarve, Azores, and Madeira) and the size of the population within each locality. In each household, the permantent resident ≥18 years old who most recently celebrated birthday was selected to participate in the study. In total, 28,502 households were contacted, 8041 individuals refused to participate, and 10,661 were included in the study. The EpiReumaPt population was similar to the Portuguese population (Census 2011) in age strata, sex, and NUTII distribution [16].
EpireumaPt data collection was performed using a three-staged approach. In the first stage, participants completed a face-to-face interview to collect sociodemographic and health-related information and to screen for RMDs. Interviews were conducted by a team of non-medical healthcare professionals trained for this purpose, and data were collected using a computer-assisted personal interview system. Screening was considered positive if a participant mentioned a previously known RMD, if any algorithm in the screening questionnaires was positive, or if the participant reported muscle, vertebral, or peripheral joint pain in the previous 4 weeks.
In the second stage, participants who screened positive for at least one RMD (n = 7451) and approximately 20% of participants who screened negative for RMDs (n = 701) were invited to a clinical appointment at the primary care center of the participant’s neighborhood. Participants were seen by a multidisciplinary team consisting of a rheumatologist, X-ray technician, and nurse. Clinical assessment consisted of a structured evaluation, laboratory tests, and imaging exams, if needed, to establish a diagnosis and evaluate disease-related information. According to participants’ complaints, simple radiographs were performed in 122 hips and 479 knees, among other joints. Rheumatologists were blind to prior health-related data. Of the participants in the second stage, 4275 did not attend the clinical appointment. Therefore, at the end of the second stage, there were 3877 clinical observations: 3198 participants received an RMD diagnosis, and 679 did not receive an RMD diagnosis.
In the third stage, three experienced rheumatologists reviewed all data and validated the RMD diagnosis of individuals that participated in the clinical appointment – second stage. Diagnostic agreement among the three rheumatologists was 98.3%, with a Cohen’s K coefficient of 10.87 (95% confidence interval (CI): 0.83, 0.91) [16]. When data were insufficient to fulfill international classification criteria for an RMD, five rheumatologists met to reach agreement on the final diagnosis. When doubts persisted, the opinion of the rheumatologist who performed the clinical assessment in the second stage prevailed. From the individuals that participated in the clinical appointment (n = 3.877), a total of 1087 participants had a validated diagnosis of HKOA, 199 had a validated diagnosis of hip OA, and 981 had a validated diagnosis of knee OA (Fig. 1). When the overall performance of the RDM screening algorithm was evaluated, using final diagnosis after the third stage as the gold standard, its sensitivity and specificity were 98 and 22% and positive and negative predictive value were 85 and 71%, respectively.
Study population
This study included participants of EpiReumaPt with validated a diagnosis of HKOA according to American College of Rheumatology criteria [17, 18].
Case definition and measurement
Mean pain intensity in the previous week, measured on a 11-point numeric pain rating scale (NPRS) in the second stage of EpiReumaPt, was used to categorize participants with HKOA into MPL (< 5 points) and UPL (≥5 points), which was validated by Zelman et al. (2003) using the question 5 of Brief Pain Inventory (BPI) scale, as the average pain in the previous week on an 11-point NPRS. The optimal cut-off point found for manageable day pain in OA was 5 [F(7, 90)= 7.08, p<0.0001] [19]. In the validation of this cut-off Zelman et al., statistically derived the 11-point NPRS with BPI interference scale measures, WOMAC-physical function and SF-36 and reach the final cut off of 5 in average pain intensity that best separate the groups with manageable pain and not manageable pain. This cut-off represent a “Manageable Day” or, in other words, in people with HKOA, pain intensity less than 5 on a 11-point NPRS permit an increased function and quality of life [19].
When both the hip and knee were affected, the worst score was considered.
Sociodemographic, clinical, and lifestyle variables
Sociodemographic, clinical, and lifestyle variables were collected during the first and second phases of EpiReumaPt. To assure better clinical interpretation, some variables were subjected to categorical transformation.
Sociodemographic and anthropometric variables
Sociodemographic variables were age, sex, and geographic location according to NUTS II territorial units. Madeira and Azores were merged in the analysis as the Islands region. Marital status was categorized as “partner” (married or consensual union) or “no partner” (single, widowed, or divorced). Education level was categorized according to years of education completed: < 4 years (less than primary education), 4–9 years (primary or secondary education), or ≥ 10 years (secondary or higher education).
Body mass index (BMI) was categorized as underweight (≤18.49 kg/m2), healthy weight (≥18.50 and ≤ 24.99 kg/m2), overweight (≥25.00 and ≤ 29.99 kg/m2), or obese (≥30.00 kg/m2).
Lifestyle and clinical variables
Lifestyle variables were alcohol intake (“no” or “occasionally or daily”), smoking habits (“never” and “occasionally or daily”), and regular exercise/sports (“yes” or “no”).
The number of chronic non-communicable diseases was calculated as the numeric count of the following self-reported conditions: high blood pressure, high cholesterol, cardiac disease, diabetes mellitus, chronic lung disease, problems in the digestive tract, renal colic, neurological disease, allergies, mental or psychiatric illness, cancer, thyroid or parathyroid problems, hypogonadism, and hyperuricemia. Multimorbidity was defined as having two or more chronic non-communicable diseases [20].
In addition to pain intensity, other clinical variables were considered: performance in ADL, QoL, and the presence of depression and/or anxiety symptoms. Performance in ADL and QoL related to HKOA were evaluated with the Portuguese version of the Knee Injury and Osteoarthritis Outcome Scale (KOOS) [21] and Hip Disability and Osteoarthritis Outcome Scale (HOOS) [22]. These self-reported clinical outcome measures evaluate short- and long-term consequences of HKOA in five dimensions: pain, symptoms, ADL, sports and leisure, and QoL. For this study, we used only the HOOS/KOOS ADL and HOOS/KOOS QoL subscales. Scores for each dimension were transformed on a 0–100 scale, with 0 representing extreme hip/knee problems and 100 representing no hip/knee problems [21, 22]. For both subscales, if more than one joint was affected, the worst score was considered.
Anxiety and depression symptoms were evaluated using the Hospital Anxiety and Depression Scale subscales for depression (HADS-D) and anxiety (HADS-A). Both scales have a range of 0 to 21, with higher values representing more severe symptoms of anxiety or depression. Final HADS-A and HADS-D scores were categorized using validated cut-offs as: “with anxiety” (HADS-A ≥ 11) or “without anxiety” (HADS-A < 11) and “with depression” (HADS-D ≥ 11) or “without depression” (HADS-D < 11) [23].
Use of therapies
Information on pharmacological therapies, defined as daily medications taken in the previous month, was collected in the first-stage interviews. Medication for pain relief was classified according to the Anatomical Therapeutic Chemical Classification System as: glucosamine (M01AX05); analgesics/antipyretics (N02B), specifically paracetamol (N02BE01); simple (N02A) and combined (N02AJ) opioids; non-steroidal anti-inflammatory drugs (NSAIDs; M01A); and topical agents (M02A). Information on physiotherapy attendance in the previous 12 months, was also collected in the first-stage interviews. Information on any previous hip or knee surgery was collected during the second-stage clinical appointments, which occurred no more than 15 days after the first stage. Surgery variable (yes/no) was related to any hip or knee surgical procedure that the participants have had in their life, this may include, for example, replacement surgery, meniscectomy or ligament reconstruction surgery.
Data analysis
After participants were categorized into UPL and MPL subgroups, weighted proportions of participants with UPL were computed taking sampling design into account as described in the EpiReumaPt methodologic protocol [16]. The logit transformation method was used to calculate 95% CIs. Analysis of the proportion of participants with UPL and MPL (relative and absolute frequencies) was conducted separately for participants with hip OA and those with knee OA.
Descriptive statistics were used to characterize all participants and separate, the MPL and UPL subgroups, according to sociodemographic, lifestyle, health-related variables as well as use of pain medication, physiotherapy and surgery. Differences between subgroups were analyzed using independent samples t-tests for continuous variables and Chi-square tests for categorical variables.We first analyzed associations between sociodemographic, lifestyle, and health-related variables and pain levels subgroups. Variables with p < 0.25 were included in a univariate logistic regression model in a forward selection process [24] to avoid early exclusion of potentially important variables (Additional file 1). These variables were selected in this stage since they are previously known associated with HKOA outcomes [25]. Variables with p < 0.05 were then kept in a backward selection process to construct a multivariable model [26].
We next analyzed associations between UPL and clinical outcomes, having MPL subgroup as reference. Associations between UPL and HOOS/KOOS ADL and QoL subscale scores were analyzed using linear regression models adjusted for the variables retained in the multivariable model. Associations between UPL and the presence of anxiety and depression symptoms were analyzed using logistic regression models adjusted for the same variables. This adjustment was made since the variables retained in the first multivariate model showed statistical associations with the outcome. The adjustment analyzed any confounder effect on the association between UPL/MPL with other clinical outcomes.
Given the scarcity of data, normal and underweight BMI categories were merged into a single category (< 25.00 kg/m2). A sensitivity analysis was additionally performed for participants with hip OA and for those with knee OA (Additional file 2).
All analyses were weighted and performed with SPSS 26 complex samples for MacOS (IBM Corp., Armonk, NY, USA). Statistical significance was defined as p < 0.05.
Results
The prevalence of UPL among people with HKOA was 68.8%. People with UPL reported a mean pain intensity of 6.85 ± 1.54 on a 0- to 10-point numeric pain rating scale. The proportions of people with UPL who had hip OA (n = 144, 69.7%) or knee OA (n = 694, 69.5%) were similar (Table 1).
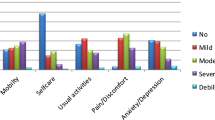
The proportion of people with UPL increased with age, reaching 73.3% in the oldest age class (≥75 years of age). UPL was more common in female than in male subjects, as shown in Fig. 2.
Mean age and age class distributions were similar between UPL and MPL subgroups (Table 2). The UPL subgroup contained a larger proportion of people with a lower level of education (< 4 years of completed schooling) than the MPL subgroup. Overweight and obesity were highly prevalent among people with HKOA and were present at similar proportions between UPL and MPL subgroups.
The UPL subgroup contained smaller proportions of people who smoked or consumed alcohol daily than the MPL subgroup. Although regular exercise was more common within the MPL subgroup than within the UPL subgroup, this difference was not significant. The presence of multimorbidity was more common within the UPL subgroup than within the MPL subgroup.
When analyzing associations between UPL and sociodemographic, lifestyle, and health-related variables, female participants, being overweight or obese, and having multimorbidity were independently associated with UPL (Table 3).
When adjusting for sex, BMI, and multimorbidity, significant negative associations between UPL and HOOS/KOOS ADL and QoL scores remained (Table 4). Thus, people with UPL were more likely to have worse HOOS/KOOS ADL and QoL scores than people with MPL. Although there was a significant association between UPL and anxiety symptoms in the unadjusted model, no significant association was found in the adjusted model, having the MPL subgroup as reference. No statistically significant associations were found in the unadjusted or in the adjusted model between depression symptoms and UPL, having MPL subgroup as reference. No differences were found in the sensitivity analysis (Additional file 2).
Overall, NSAIDs, analgesics, and physiotherapy were the most used therapies by people with HKOA (Table 5). Higher proportions of people within the UPL subgroup regularly took NSAIDS, simple opioids, and analgesics, specifically paracetamol, than within the MPL subgroup. Physiotherapy was also more commonly used by people with UPL than by people with MPL. There were no significant differences in the proportions of people who underwent hip or knee surgery between UPL and MPL subgroups.
Discussion
Our results indicate that 68.8% of people with HKOA in Portugal live with UPL, which is higher than the prevalence of UPL in Mexico (53%) [27], the Survey of Osteoarthritis Real World Therapies (SORT) cohort from six European countries (54%) [10], and a sample of Portuguese people with knee OA included in the SORT cohort (51%) [28]. All three of these earlier studies included people who were ≥ 50 years old, possibly excluding younger patients with early OA, and who took analgesics regularly, which may explain why we found a higher prevalence of UPL in the present study.Our study included a representative sample of the Portuguese population who live in the community, suggesting that offered interventions do not meet the need for pain control for more than two-thirds of the Portuguese HKOA population.
We found that people with UPL had lower education levels than people with MPL. This finding is consistent with previous literature reporting that low education is associated with more severe OA symptoms, is a social determinant of unhealthy lifestyles and multimorbidity [27, 29], is a determinant of lack of access to and delay in seeking healthcare [30], and is associated with increased pain intensity over time [31].
The multivariable model showed that female sex, overweight and obesity, and multimorbidity were associated with UPL, similar to the results of the SORT study [10]. In our study being female was associated with higher OA-related pain levels, but gender differences on pain intensity in HKOA remain unclear in the literature. Data from quantitative sensory testing in people with knee OA has shown that women have greater sensitivity to pain but no sex differences were found in clinical pain. These authors suggested that women have an enhanced central pain sensitivity [30]. More recently, Mun et al. (2020) concluded that women with knee OA have a greater interleukin 6 activation when compared to men, after laboratory quantitative sensory testing. These authors concluded that this enhanced inflammatory reactivity in women may contribute to exacerbation or maintenance of symptoms [31].
Other factors like psychosocial and genetic factors showed inconsistent gender differences and pain severity [32] [33].. Also, a systematic review of progression phenotypes among people with OA shows that overweight or obesity is a major factor in the progression of OA and is associated with worsening of pain, loss of physical function, and structural deterioration over time [34].
Additionally, our results show that having multimorbidity was associated with UPL. Multimorbidity is associated with chronic pain in a cumulative manner [35] and is related to pain intensity in people with HKOA [36]. People with multimorbidity have a higher likelihood of walking impairments, which can contribute to a worsening of OA and other chronic conditions that occurswith an additional consequence of psychological distress [35, 36].
We found that UPL was negatively associated with performance in ADL and QoL. Previous research reveals that within the OA population, pain severity explains most of the variability in disability and QoL [37]. High pain severity may lead to fear of movement and/or avoidance behaviors, resulting in physical inactivity and less participation in social activities and leads to greater physical disability, psychological distress, and reduced QoL [38].
The sensitivity analysis did not show differences when separating participants with hip OA and with knee OA. This suggests that similar factors were associated with UPL in people with OA in these two joints, separately or together. However, due to the small sample size of participants with hip OA, we were not able to perform multivariable analysis for anxiety and depression symptoms.International clinical practice guidelines recommend that topical NSAIDs be considered before oral NSAIDs consistentwith the least systemic exposure principle, and oral NSAIDs are strongly recommended at the lowest possible dose [39]. Given the limited efficacy of paracetamol and its potentially harmful secondary effects, it is only conditionally recommended for people with OA [39]. Although tramadol is conditionally recommended, non-tramadol opioids are not recommended for the management of pain in people with OA. Tramadol and non-tramadol opioids can be used only when alternatives have been exhausted. Glucosamine is strongly not recommended for people with HKOA [39]. In the present study, oral NSAIDs were the most used medication followed by analgesics/antipyretic medication, whereas topical NSAIDs were the least used pharmacological modality. People with UPL regularly took more medication for pain relief, namely NSAIDS, opioids, and analgesics, specifically paracetamol, than people with MPL, consistent with the results of the SORT study [10]. A cohort study from the Netherlands also shows pain severity is positively related to analgesic intake; however, the authors concluded that most reasons for analgesic prescription are unknown [40].
Even though no temporal relationships can be drawn from a cross-sectional design, this study reveals that a higher proportion of people who took daily pain medication in the previous month had UPL. Additionally, our results suggest that medication is taken by a much lower proportion of people with OA in Portugal than in other European countries [12]. (12)In Europe, medication use seems to be highly variable across countries. Data from five countries included in the National Health and Wellness Survey (n = 37,650), reveal that the minimum and maximum proportions of overall pain medication intake by people with OA was 22% in Germany and 53.2% in Spain. Specifically, NSAID’s were at minimum by 46,5% of people with OA in France and at maximum by 81.9% in Germany; Paracetamol was not used by any participants of Germany, but by 6% of participants from Spain. Opioids were used by 1.8% in Italy at minimum and by 54.5% at maximum of people with HKOA in France. These proportions of medication use were much higher than the ones seen in our findings probably because medication intake was asked as “medication used at the moment” [12] rather than daily use of medication in the previous month, as in our study. Similarly, our findings reveal that NSAID’s are the medication most used by people with HKOA. In other European countries opioids are the second most used pain medication, contrarily to our study (used similarly to analgesics). These findings may suggest that opioids are less prescribed in Portugal than in other countries. However, data from the general population reveal that the prescription of opioids in Portugal has increased by 1.5-fold between 2013 and 2017 [41].
Although randomized controlled trials show that analgesic drugs and other recommended interventions effectively manage pain in individuals with OA, adherence to medication and healthy lifestyle behaviors are a real-world concern that prevent the optimization of pain control in this population. A qualitative meta-ethnographic study points out that factors such as the severity of pain, perceived effect of medication, fear related to side effects, acceptability of dose regimens, education and knowledge about OA and the medication regimen, self-efficacy, and locus of control over OA influence medication adherence [42].
Regarding conservative non-pharmacological therapies used by people with HKOA, we found that < 20% of people with UPL underwent physiotherapy in the last 12 months or regularly exercised. These values are much lower than other European countries. For example, the proportion of people with OA in national cohorts that used physiotherapy in a 12-month time frame was 53.1% in Germany [43] and 32% in the UK [44].
Crrent clinical guidelines recommend physiotherapy and exercise as first-line treatments. Exercise should be maintained during the progression of the disease for pain management purposes [45, 46]. Although, similarly to our results, current literature suggests that exercise and physiotherapy, as part of core non-pharmacological treatments, are uptake by < 50% of people with HKOA [47, 48]. Additionally, healthcare interventions seems to be symptom-driven and segmented [49] centered on pharmacological [47, 48] and surgical options [50]. On the other hand, lack of long-term adherence to behavior-dependent interventions, like exercise has been pointed out as an explanation for poor long-term outcomes in people with HKOA [51, 52]. Therefore, interventions for the management of HKOA should also target behavior changethrough strategies that optimize motivation and overcome barriers of adherence [53].
Limitations
Our study has several limitations that should be considered. A large proportion of participants included in the first phase of the study and invited for the second phase did not show up in the rheumatologist appointment. Therefore, we should hypothesize a selection bias, since the subjects who were willing to participate in the appointment might be the most severe cases.
Due to its cross-sectional design, no cause-effect relationships can be established between UPL and sociodemographic, lifestyle, and health-related variables. Additionally, identification of variables with direct and indirect effect on the outcome is not possible with this study design and was not accounted in the regression models [54]. Also, giving the cross-sectional design of the study, the variables related with the use of therapies were considered only to describe and compare UPL/MPL subgroups and no associations with the outcome variables were explored. Also, estimation of the proportion of people with UPL in the Portuguese population using sample weights is not free from error, although sample weights are recommended for all statistical analyses using complex samples data [55].
[1, 43](58)We used the validated cut-off by Zelman et al. (2003), to define people with UPL and MPL. However, in this validation study the eligible criteria included people with HKOA that have at least 1 year pain duration, that have a daily use of some form of analgesic and that reported average daily pain of 4 at least in the 11-point NPRS [19]. Notwithstanding, the cut-off “5” was previously validated in other populations as pain intensity that interferes with function and QoL - musculoskeletal pain in general [56], in patients with knee OA [10] and in those with HKOA waiting for surgery [57]. In this late study the authors concluded that the interference of pain in function (using the same cut-off) was independent from pain duration. Therefore, we cautiously believe that this cut-off is valid also in the population of our study.
We asked participants about their use of “regular medication”. However, as people with OA often use analgesic medication sporadically for pain flares rather than daily, our results may underestimate the proportion of people that use medication for symptomatic control. On the other hand, we did not control for other pain conditions like fibromyalgia or widespread pain syndromes, pain duration or pain frequency (e.g. daily or constant pain) that may increase the intake of medication. Also, as physiotherapy attendance in the last 12 months was self-reported, we acknowledge the possibility that memory bias may compromise the accuracy of our results. Additionally, we did not investigate the reason for medication use or physiotherapy.
Surgery procedure was not specified, and this variable (surgery - yes/no) was not related to a specific time frame. Additionally, since the causes of surgery are not known our results were purposively descriptive and no hypothesis can be drawn. “Regular exercise” was self-reported by participants and did not consider the precise amount and intensity. Hence, our data may overestimate the proportion of people who exercised. Moreover, pain intensity is multifactorial [38], and several potentially important factors were not considered in the analysis, such as fear avoidance beliefs, catastrophizing, or coping strategies.
The analyzed data were collected in 2011–2013, but due to few specific strategies directed to RMDs in the last decade in Portugal, we cautiously believe that the current management of OA does not differ from that reflected in this study.
Strengths and implications
This is the first population-based study in Portugal analyzing outcomes of current interventions offered to community-dwelling people with HKOA. The results of this study raise concerns regarding important factors that should be further explored in future research and addressed in national health policies to optimize the outcomes of people with HKOA, namely:
1) The high proportion of people with UPL, suggest a poor control of pain levels in people with HKOA;
2) The high proportion of people with UPL who use pharmacological and non-pharmacological therapiesmay indicate that pain management is suboptimal;
3) Besides the low proportion of people who use therapy, the interventions offered do not seem to be aligned with international recommendations [39, 45] considering the small proportion of people who underwent physiotherapy, exercised, and used pain medication and the large proportion of people who were overweight or obese.
Conclusion
Approximately two-thirds of the Portuguese population with HKOA have UPL, despite the higher use of medication and physiotherapy in the UPL subgroup, when compared with theMPL subgroup. Being overweight and having multimorbidity are modifiable risk factors associated with UPL. Overall, recommended management strategies appear to be offered to a small proportion of people with HKOA. Our results may seemingly suggest that current therapies are sub-optimal and that lifestyle behaviour change may be neglected, but longitudinal research is needed to corroborate these hypotheses. Our findings reveal an opportunity for pain management improvement in the HKOA population and highlight the need for further research on effective pain management interventions.
Availability of data and materials
The data underlying this article were provided by the EpiDoc Unit - CEDOC by permission. Data will be shared upon request to the corresponding author with the permission of EpiDoc Unit group leaders.
Abbreviations
- ADL:
-
Activities of Daily Living
- BMI:
-
Body Mass Index
- CI:
-
Confidence Interval
- HADS-A:
-
Hospital Anxiety and Depression Scale subscale for anxiety
- HADS-D:
-
Hospital Anxiety and Depression Scale subscale for depression
- HKOA:
-
Hip and/or Knee Osteoarthritis
- HOOS:
-
Hip Disability and Osteoarthritis Outcome Scale
- KOOS:
-
Knee Injury and Osteoarthritis Outcome Scale
- MPL:
-
Manageable pain levels
- NPRS:
-
Numerical Pain Rating Scale
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- OA:
-
Osteoarthritis
- OR:
-
Odds Ratio
- QoL:
-
Quality of Life
- RMD:
-
Rhematic and Musculoskeletal Diseases
- SD:
-
Standard Deviation
- SORT:
-
Survey of Osteoarthritis Real World Therapies
- UPL:
-
Unmanageable Pain Levels
References
Safiri S, Kolahi AA, Smith E, Hill C, Bettampadi D, Mansournia MA, et al. Global, regional and national burden of osteoarthritis 1990-2017: a systematic analysis of the global burden of disease study 2017. Ann Rheum Dis. 2020;79(6):819–28.
Salmon JH, Rat AC, Sellam J, Michel M, Eschard JP, Guillemin F, et al. Economic impact of lower-limb osteoarthritis worldwide: a systematic review of cost-of-illness studies. Vol. 24, Osteoarthritis and Cartilage. W.B. Saunders Ltd. 2016:1500–8.
Laires PA, Canhao H, Rodrigues AM, Eusebio M, Gouveia M, Branco JC. The impact of osteoarthritis on early exit from work: results from a population-based study. BMC Public Health. 2018;18(1):472.
Pabinger C, Lothaller H, Geissler A. Utilization rates of knee-arthroplasty in OECD countries. Osteoarthr Cartil. 2015;23(10):1664–73.
March L, Cross M, Lo C, Arden NK, Gates L, Leyland KM, et al. Osteoarthritis: a serious Disease: submitted to the U.S. Food and Drug Admin. 2016. Available from: https://oarsi.org/oarsi-white-paper-oa-serious-disease.
Cubukcu D, Sarsan A, Alkan H. Relationships between Pain , Function and Radiographic Findings in Osteoarthritis of the Knee : A Cross-Sectional Study. Arthritis. 2012;2012:1–5.
Creamer P, Hochberg MC. Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology. 2000;39(5):490–6.
Barthel HR, Peniston JH, Clark MB, Gold MS, Altman RD. Correlation of pain relief with physical function in hand osteoarthritis: randomized controlled trial post hoc analysis. Arthritis Res Ther. 2010;12(1):R7–8.
Kingsbury SR, Hensor EMA, Walsh CAE, Hochberg MC, Conaghan PG. How do people with knee osteoarthritis use osteoarthritis pain medications and does this change over time ? Data from the Osteoarthritis initiative. Arthritis Res Ther. 2013;15(5):R106.
Conaghan PG, Peloso PM, Everett SV, Rajagopalan S, Black CM, Mavros P, et al. Inadequate pain relief and large functional loss among patients with knee osteoarthritis: evidence from a prospective multinational longitudinal study of osteoarthritis real-world therapies. Rheumatology (United Kingdom). 2015;54(2):270–7.
Dibonaventura M, Gupta S, Mcdonald M, Sadosky A, Pettitt D, Silverman S. Impact of self-rated osteoarthritis severity in an employed population: Cross-sectional analysis of data from the national health and wellness survey. Health Qual Life Outcomes. 2012;15:1–12.
Kingsbury SR, Gross HJ, Isherwood G, Conaghan PG. Osteoarthritis in Europe: impact on health status, work productivity and use of pharmacotherapies in five European countries. Rheumatology (Oxford). 2014;53(5):937–47.
Fu K, Robbins SR. Mcdougall JJ. Osteoarthritis: the genesis of pain. Rheumatology. 2018;57(suppl_4):iv43–iv50. https://doi.org/10.1093/rheumatology/kex419.
Hagen KB, Smedslund G, Osteras N, Jamtvedt G. Quality of community-based Osteoarthritis care: a systematic review and Meta-analysis. Arthritis Care Res (Hoboken). 2016;68(10):1443–52.
Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393(10182):1745–59.
Rodrigues AM, Gouveia N, da Costa LP, Eusébio M, Ramiro S, Machado P, et al. EpiReumaPt- the study of rheumatic and musculoskeletal diseases in Portugal: a detailed view of the methodology. Acta Reumatol Port. 2015;40(2):110–24.
Altman R, Alarcón G, Appelrouth D, Bloch D, Borenstein D, Brandt K, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34(5):505–14.
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Arthritis Rheum [Internet]. 1986;29(8):1039–49 Available from: https://onlinelibrary.wiley.com/doi/10.1002/art.1780290816.
Zelman DC, Hoffman DL, Seifeldin R, Dukes EM. Development of a metric for a day of manageable pain control: derivation of pain severity cut-points for low back pain and osteoarthritis. Pain. 2003;106(1–2):35–42.
Diederichs C, Berger K, Bartels DB. The Measurement of Multiple Chronic Diseases--A Systematic Review on Existing Multimorbidity Indices. J Gerontol A Biol Sci Med Sci 2011 ;66A(3):301–311.
Gonçalves RS, Fau JC, Pinheiro JP, Ferreira PL, Gil J. Reliability, validity and responsiveness of the Portuguese version of the Knee injury and Osteoarthritis Outcome Score--Physical Function Short-form (KOOS-PS). Osteoarthr Cartil. 2010;18(3):372–6.
Cavalheiro L, Gil J, Nunes S, Ferreira P, Gonçalves R. Measuring Health-Related Quality of Life in Patients With Hip Osteoarthritis and Total Hip Replacement: Adaption and Validation of the Hip Disability and Osteoarthritis Outcome Source LK 2.0 (HOOS 2.0) to the Portuguese Culture. In: 18th Annual Conference of the International Society of Quality of Life (ISOQOL 2011). 2011.
Silva I, Pais-Ribeiro J, Cardoso H. Contributo para a adaptação da Hospital Anxiety and Depression Scale à população portuguesa com doença crónica. Psychologica. 2006;41:193–204.
Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:1–8.
O’Neill TW, McCabe PS, McBeth J. Update on the epidemiology, risk factors and disease outcomes of osteoarthritis. Best Pract Res Clin Rheumatol. 2018;32(2):312–26.
Marôco J. Análise Estatística com o SPSS Statistics. 7th Editio ed. ReportNumber; 2018.
Luong MLN, Cleveland RJ, Nyrop KA, Callahan LF. Social determinants and osteoarthritis outcomes. Aging Health. 2012;8(4):413–37.
Laires PA, Laíns J, Miranda LC, Cernadas R, Rajagopalan S, Taylor SD, et al. Inadequate pain relief among patients with primary knee osteoarthritis. Revista Brasileira de Reumatologia (English Edition). 2017;57(3):229–37.
Guillemin F, Carruthers E, Li LC. Determinants of MSK health and disability - social determinants of inequities in MSK health. Best Pract Res Clin Rheumatol. 2014;28(3):411–33.
Bartley EJ, King CD, Sibille KT, Cruz-Almeida Y, Riley JL, Glover TL, et al. Enhanced pain sensitivity among individuals with symptomatic knee Osteoarthritis: potential sex differences in central sensitization. Arthritis Care Res (Hoboken). 2016;68(4):472–80.
Mun CJ, Letzen JE, Nance S, Smith MT, Khanuja HS, Sterling RS, et al. Sex differences in Interleukin-6 responses over time following laboratory pain testing among patients with knee Osteoarthritis. J Pain. 2020;21(5–6):731–41.
Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choinière M. A systematic literature review of 10 years of research on sex/gender and pain perception – part 2: do biopsychosocial factors alter pain sensitivity differently in women and men? Pain. 2012;153(3):619–35.
Hashmi JA, Davis KD. Deconstructing sex differences in pain sensitivity. Pain. 2014;155(1):10–3.
Deveza LA, Melo L, Yamato TP, Mills K, Ravi V, Hunter DJ. Knee osteoarthritis phenotypes and their relevance for outcomes: a systematic review. Osteoarthr Cartil. 2017;25(12):1926–41.
Dominick CH, Blyth FM, Nicholas MK. Unpacking the burden: understanding the relationships between chronic pain and comorbidity in the general population. Pain. 2012;153(2):293–304.
Muckelt PE, Roos E, Stokes M, McDonough S, Grønne D, Ewings S, et al. Comorbidities and their link with individual health status: a cross-sectional analysis of 23,892 people with knee and hip osteoarthritis from primary care. J Comorb. 2020;1:10.
Montero A, Mulero JF, Tornero C, Guitart J, Serrano M. Pain, disability and health-related quality of life in osteoarthritis—joint matters: an observational, multi-specialty trans-national follow-up study. Clin Rheumatol. 2016;35(9):2293–305.
Hawker GA. Osteoarthritis is a serious disease. Clin Exp Rheumatol. 2019;37(Suppl 120):3–6.
Kolasinski SL, Neogi T, Hochberg MC, Oatis C, Guyatt G, Block J, et al. 2019 American College of Rheumatology/Arthritis Foundation guideline for the Management of Osteoarthritis of the hand, hip, and knee. Arthritis & Rheumat. 2020;72(2):220–33.
Knoop J, van Tunen J, van der Esch M, Roorda LD, Dekker J, van der Leeden M, et al. Analgesic use in patients with knee and/or hip osteoarthritis referred to an outpatient center: a cross-sectional study within the Amsterdam Osteoarthritis cohort. Rheumatol Int 2017 ;37(10):1747–1755.
Caldeira D, Broeiro P, Cimadeira F, Costa J, Lourenço A, Meireles C, et al. Opioids prescribing trend between 2013 and 2017 in the Lisbon and Tagus Valley region. Portugal Int J Clin Pharm. 2021;43(2):323–7.
Dockerty T, Latham SK, Smith TO. Why don’t patients take their analgesics? A meta-ethnography assessing the perceptions of medication adherence in patients with osteoarthritis. Rheumatol Int. 2016;36(5):731–9.
Postler A, Ramos AL, Goronzy J, Gunther KP, Lange T, Schmitt J, et al. Prevalence and treatment of hip and knee osteoarthritis in people aged 60 years or older in Germany: an analysis based on health insurance claims data. Clin Interv Aging. 2018;13:2339–49.
Abraham L, Halsby K, Stein N, Wrona B, Emir B, Stevenson H. An observational retrospective matched cohort study of healthcare resource utilisation and costs in UK patients with moderate to severe Osteoarthritis pain. Rheumatol Ther. 2022;9(3):851–74.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthr Cartil. 2019;27(11):1578–89.
Geenen R, Overman CL, Christensen R, Åsenlöf P, Capela S, Huisinga KL, et al. EULAR recommendations for the health professional’s approach to pain management in inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77(6):797–807.
Basedow M, Esterman A. Assessing appropriateness of osteoarthritis care using quality indicators: a systematic review. J Eval Clin Pract. 2015;21(5):782–9.
Edwards JJ, Khanna M, Jordan KP, Jordan JL, Bedson J, Dziedzic KS. Quality indicators for the primary care of osteoarthritis: a systematic review. Ann Rheum Dis. 2013;74(3):490–8.
Hunter DJ. Osteoarthritis management: time to change the deck. J Orthop Sports Phys Ther. 2017;47(6):370–2.
Bruyere O, Honvo G, Veronese N, Arden NK, Branco J, Curtis EM, et al. An updated algorithm recommendation for the management of knee osteoarthritis from the European Society for Clinical and Economic Aspects of osteoporosis, Osteoarthritis and musculoskeletal diseases (ESCEO). Semin Arthritis Rheum. 2019;49(3):337–50.
Fransen M, McConnell S, Hernandez-Molina G, Reichenbach S. Exercise for osteoarthritis of the hip. Cochrane Database Syst Rev. 2014;(4).
Moseng T, Dagfinrud H, Osteras N. Implementing international osteoarthritis guidelines in primary care: uptake and fidelity among health professionals and patients. Osteoarthritis Cartilage [Internet]. 2019; Available from: https://www.cochranelibrary.com/central/doi/10.1002/central/CN-01940747/full
Eisele A, Schagg D, Krämer LV, Bengel J, Göhner W. Behaviour change techniques applied in interventions to enhance physical activity adherence in patients with chronic musculoskeletal conditions: a systematic review and meta-analysis. Patient Educ Couns. 2019;102(1):25–36.
Ponkilainen VT, Uimonen M, Raittio L, Kuitunen I, Eskelinen A, Reito A. Multivariable models in orthopaedic research: a methodological review of covariate selection and causal relationships. Osteoarthr Cartil. 2021;29(7):939–45.
Lavallée P, Beaumont JF. Why We Should Put Some Weight on Weights. In: Survey Insights: Methods from the Field, Weighting: Practical Issues and ‘How to’ Approach. 2015. Available from: https://surveyinsights.org/?p=6255.
Boonstra AM, Stewart RE, Köke AJA, Oosterwijk RFA, Swaan JL, Schreurs KMG, et al. Cut-off points for mild, moderate, and severe pain on the numeric rating scale for pain in patients with chronic musculoskeletal pain: variability and influence of sex and catastrophizing. Front Psychol. 2016;30:7.
Kapstad H, Hanestad BR, Langeland N, Rustøen T, Stavem K. Cutpoints for mild, moderate and severe pain in patients with osteoarthritis of the hip or knee ready for joint replacement surgery. BMC Musculoskelet Disord. 2008;9(1):55.
Burgos-Vargas R, Aggarwal J, Johnson KD, Ramey D, Lozano F, Macahilig C, et al. Results from a cross-sectional, observational study to assess inadequate pain relief in patients with knee and/or hip osteoarthritis in Mexico. Reumatología Clínica (English Edition). 2021;17(7):397–403.
Pan F, Tian J, Aitken D, Cicuttini F, Jones G. Predictors of pain severity trajectory in older adults: a 10.7-year follow-up study. Osteoarthr Cartil. 2018;26(12):1619–26.
Dabare C, le Marshall K, Leung A, Page CJ, Choong PF, Lim KK. Differences in presentation, progression and rates of arthroplasty between hip and knee osteoarthritis: observations from an osteoarthritis cohort study-a clear role for conservative management. Int J Rheum Dis. 2017;20(10):1350–60.
Acknowledgements
We thank Prof. Carla Nunes (NOVA National School of Public Health – Universidade NOVA de Lisboa) for the valuable insights and discussions in the conceptualization of this project. We thank the EpiDoc Unit and EpiReumaPt team for conceptualizing, planning, and implementing the main research project. We also acknowledge the support of CHRC (UIDP/04923/2020), granted by national funds through Fundação Ciência e Tecnologia, IP.
Funding
This study received funding from an independent research grant (ID: 64165707) by Pfizer, and the first author received a grant from Fundação Ciência e Tecnologia, IP under the PhD grant SFRH/BD/148420/2019. The funders were not involved in study design; collection, analysis, or interpretation of data; or writing this article or the decision to submit it for publication.
Author information
Authors and Affiliations
Contributions
DC, DGL, and CNS contributed to the drafting of the manuscript. DC, EBC, DL and AMR contributed to the analysis and interpretation of the data. DC, DGL, and ARH contributed to statistical analysis. HC, JB, and AMR contributed to the conception and design of the main project (EpiReumaPt), provision of study materials, obtaining funding for the main project, administrative/logistic support, and collection of data. All authors critically revised and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The EpiReumaPt study was approved by the Ethics Committee of NOVA Medical School and the Portuguese Data Protection Authority (Comissão Nacional de Proteção de Dados). This secondary analysis of EpiReumaPt database presented in this study was additionally approved by the Ethics Committee of NOVA Medical School. This study was performed in accordance with the Declaration of Helsinki and revised in 2013 in Fortaleza. Written informed consent was obtained from all participants before entering in EpiReumaPt study, as described elsewhere [16].
Consent for publication
Not Applicable.
Competing interests
All authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Univariate Logistic Regression analysis. Table S1. Factors associated with unmanageable pain levels in univariate logistic regression analysis.
Additional file 2.
Sensitivity Analysis of participants with hip OA and with knee OA. Table S.2 a). Sociodemographic, lifestyle, and health-related variables for people with Hip OA. Table S.2 b) Sociodemographic, lifestyle, and health-related variables for people with Knee OA. Table S.3- Univariable models factors associated with UPL in people with Knee OA or Hip OA. Table S.4- Multivariable models factors associated with UPL in people with Knee OA or Hip OA. Table S.5. HOOS/KOOS ADL and QoL subscale scores and anxiety and depression symptoms in people with Hip OA and UPL or MPL and people with Knee OA and UPL or MPL.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Costa, D., Cruz, E.B., Lopes, D.G. et al. Prevalence of and factors associated with unmanageable pain levels in people with knee or hip osteoarthritis: a cross-sectional population-based study. BMC Musculoskelet Disord 24, 60 (2023). https://doi.org/10.1186/s12891-022-06110-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-06110-1