Abstract
Background
Fragility fractures of the sacrum (FFS) have been detected more and more frequently in recent times, and the incidence will continue to increase due to increasing life expectancy. The aim of this study was to compare the clinical outcome of conservative, interventional and surgical treatment of FFS.
Methods
Retrospectively, 292 patients (276 women, 16 men) with confirmed FFS were followed up over a period of 2 years. The age of the women was Ø 81.2 (58 - 99) and that of the men Ø 78.1 (76 - 85) years. The pain was quantified using a VAS. Fractures were classified in accordance with the Rommens and Hofmann and with the Denis classification using conventional X-rays, CT and MRI. A QCT of the lumbar spine was performed to quantify bone mineral density. Concomitant diseases of every patient were recorded. An interdisciplinary case conference determined the individual treatment concept considering the age, type of fracture, pain level and comorbidities with classification into conservative, interventional (any type of sacroplasty) or surgical treatment. Over the course pain and independence were measured, complications and patient satisfaction were documented. A vitamin D determination was done, and existing comorbidities were included.
Results
Patients with a pain level of ≤5 benefited from the conservative therapy measures, with pain levels > 5 significantly delaying the development of mobility. After sacroplasty, the pain reduced significantly, which caused a rapid improvement in mobility without any significant difference being found between vertebro- (VSP), balloon (BSP), radiofrequency (RFS) and cement sacroplasty (CSP). In terms of pain reduction and mobilization, the surgical treated patients benefited from osteosynthesis, although more complex fracture types with lumbopelvic stabilization took longer. Overall, there were no deaths during the hospital stay. Mortality after 12 months was 21.7% for the conservative, 8.4% for the interventional and 13.6% for the surgical therapy group; the differences are significant. For patients in the conservative therapy group who were difficult to mobilize due to pain, the mortality increased to 24.3%. Over 24 months, patients achieved the best independence after sacroplasty. At 12 and 24 months, subjective satisfaction with the therapies was best after sacroplasty, followed by osteosynthesis and conservative measures. All patients had a pronounced vitamin D deficiency and manifest osteoporosis. Cardiovascular pathologies were the main concomitant diseases.
Conclusions
Patients with FFS with a low level of pain benefit from conservative therapy measures, whereby complications and mortality increase significantly in the case of persistent immobilizing pain. Patients with an unacceptable level of pain resulting from non-dislocated fractures benefit significantly from sacroplasty. Patients with unstable and displaced fractures (Rommens and Hofmann type III and IV) should be operated on promptly. Different techniques are available for sacroplasty and osteosynthesis, which lead to an improvement of independence and a reduction in mortality.
Similar content being viewed by others
Background
Fragility fractures of the sacrum (FFS, synonym: sacral insufficiency fractures, osteoporotic sacral fractures) are increasingly being found in patients with reduced bone quality, rheumatoid arthritis, condition after radiotherapy on the pelvis and after cortisone medication, whereby older postmenopausal women with osteoporosis show the highest risk profile [1,2,3,4,5,6,7,8]. In patients from such risk groups, an incidence of up to around 5% is suspected [9], although precise figures are not available at present. On the basis of demographic development, with the proportion of over 80-year-olds roughly doubling up to the year 2040 [10], a marked increase in FFS is to be expected in the coming years [11, 12]. Since the first description of three osteoporosis patients with sacral insufficiency fractures by Lourie in 1982 [7], doctors have been becoming increasingly aware of this type of fracture as a result of the growing sensitisation for the clinical signs and more targeted imaging diagnostics [11, 13]. The fracture is often the first manifestation site in the pelvis, followed by fractures in the pubic ramus, the parasymphyseal region, the acetabulum and the iliac crest, while conversely 56-90% of FFS are found after previously described fractures in the anterior pelvic ring [14,15,16,17]. The fracture develops without or after low-energy trauma in a structurally and substance rarefied bone [18] and is itself an indicator fracture for the presence of clinically manifest osteoporosis [15]. Severe, disabling pain in the lower back, buttocks and groin, as well as local pain upon pressure to the fracture zone are the primary clinical signs [17, 19,20,21]. Patients are usually unable to stand or walk, with increasing immobilisation in the case of bilateral fracture involvement, whereby neurological deficits are rare and, if present, typically manifest in an isolated S1 syndrome or in a cauda equina syndrome limited to the sacral nerve roots [22].
The aim of the present study was to compare the feasibility and clinical outcome of conservative, interventional and surgical treatment of FFS.
Methods
Recording of patients
Patients with tumour-related osseous destruction or pathologic fractures and courses after high-energy trauma were excluded. Retrospectively, 292 patients (276 women, 16 men) with confirmed FFS were followed up over a period of 2 years after therapy, consultation of the patients took place every 6 months. The recruitment period was from January 2014 until June 2019. The age of the women was Ø 81.2 (58 - 99), that of the men Ø 78.1 (76 - 85) years. Immobilizing pain was quantified on a visual analogue scale (VAS) [23].
Imaging for fracture classification and determination of osteoporosis
On the basis of conventional radiographs (a.p., inlet and outlet images of the pelvis), CT (axial 0.625 mm slice thickness with a 2 mm axial, coronal, semi-coronal slice plane oblique to the sacrum and sagittal reconstruction, with documentation in the bone and soft tissue window) and MRI examinations of the pelvis (with the sequences: T1-, T2-mDIXION axial; STIR semi-coronal oblique to the sacrum and T2 fat-suppressed sagittal; with a respective slice thickness of 4 mm), a classification of Fragility Fractures of the Pelvis (FFP) according to Rommens & Hofmann [14] and categorisation of fractures according to Denis et al. [24] was performed. For osteoporosis diagnosis, a QCT (GE Revolution EVO / 64 line CT, Mindways Software 3D Volumetric QCT Spine) of the lumbar spine was performed. Additional fracture of the axial and peripheral skeleton were also recorded, taking into account X-ray images and medical history.
Procedure for therapy planning
An interdisciplinary case conference determined the individual treatment concept with classification for conservative, interventional or surgical treatment, taking into account the fracture morphology, pain, concomitant diseases and the will of the patient.
Depending on the intensity of pain, the conservative treatment included bed rest, adjuvant medicinal pain therapy according to the WHO schedule [25] and mobilisation using a walker or on forearm crutches with pain-adapted weight-bearing.
The various different methods available for interventional treatment by means of sacroplasty are described by Andresen et al. [26] and those for surgical treatment using different osteosyntheses are described by Oberkircher et al. [27].
Pain intensity was measured with the VAS score at different time-points after diagnosis, self-reliance was measured by means of a modified Hamburg Barthel Index (HBI, Table 1) [28], while complications including death, and patient satisfaction were recorded.
Vitamin D was determined in all patients. Any vitamin D deficiency was immediately corrected, and permanent medication was continued according to the DVO guideline [29]; further anti-osteoporotic drug therapy was recommended. Any concomitant diseases present were also recorded.
Statistics
Statistical analysis of the results was performed using Prism 8 software (GraphPad). The Mann Whitney test was used for unpaired samples to compare the individual therapies and the Wilcoxon rank sum test was used for paired samples to determine changes over time. The students t-test was used to compare means between two groups (bone mineral density (BMD) or vitamin D values between patients with a unilateral and bilateral fracture). For comparisons between individual groups (mortality rate after conventional, interventional and osteosynthetic therapy), the one-factor analysis of variance (ANOVA) was used. At the same time, the effect sizes were calculated according to Cohen and values < 0.5 were assumed to be a small effect, between 0.5 and 0.8 a medium effect and > 0.8 a large effect. Statistical significance was marked as significant = p < 0.05, highly significant = p < 0.005 and very highly significant = p < 0.0005.
Results
Fracture classification
According to the classification of Rommens & Hofmann, FFP type II with unilateral and/or bilateral fractures (type II a, type II b and type II c) was found in 250 of 292 (85.7%), FFP type III c in 14 of 292 (4.8%) and FFP type IV (type IV b and type IV c) in 28 of 292 (9.5%) of the patients treated (Fig. 1).
Number of patients with corresponding FFP types according to Rommens & Hofmann [17]. Only FFP types with involvement of an FFS are included; FFP types without a sacral insufficiency fracture were not considered
Of the 292 patients treated, 91 (31.2%) had unilateral and 201 (68.8%) had bilateral FFS, totalling 493 FFS.
As an indication of the different ages of the FFS, the bilateral fractures usually showed varying degrees of oedema and in some cases laterally differentiated sclerosis in the area of the fracture zones on CT and MRI imaging (Fig. 2).
With a distribution of 208 out of 493 of the FFS, 42.4% were found to have a Denis type 1, 21 out of 493 or 4.2% had a Denis type 2, 0 out of 493 or 0% had a Denis type 3, 214 out of 493 or 43.3% had a Denis type 1 – 2, and 50 out of 493 or 10.1% had a Denis type 1 - 2 - 3 fracture zone (Fig. 3).
Frequency distribution of the fracture zones according to Denis et al. [24]. Image top right: Fracture zones marked on a semi-coronal MRI scan oblique to the sacrum. STIR weighting shows clear oedema on the right as an expression of a non-displaced fracture in the type 1 zone and on the left in the type 1 and 2 zones. A small area of oedema is also found in the caudal region of the type 3 zone
Pain and mobility development
Conservative
Consecutively, 50 patients with a pain level ≤ 5 (Group 1) and 100 patients with a pain level > 5 (Group 2) were included. Patients with a pain level of ≤5 benefited from the conservative therapy measures, whereby pain levels > 5 significantly delayed the development of mobility (Fig. 4 a and b).
A threshold for pain at 5 score points is marked in the graph by a solid horizontal line.
The patients in Group 2, starting from a high level of pain, only fell below a pain threshold of 5 score points after 6 months on average.
A total of 88 out of 114 (77.2%) patients could still be contacted after 24 months.
Comparison of the mean HBI values of patients with moderate (Group 1) and moderate to severe immobilising functional impairments (Group 2). The mean HBI of all patients was 55 +/− 15 at baseline, with a significant difference of 65 +/− 10 for Group 1 and 48 +/− 14 for Group 2, at p < 0.001. After 24 months, the scores increased to 76 +/− 13, with score points remaining significantly different (p < 0.05) between Group 1 and Group 2 at all-time points, with significantly lower scores for Group 2 patients.
Over the course of the study, 36 (4 Group I, 32 Group II) out of 150 (24%) patients were referred for interventional (10 out of 36) and osteosynthetic therapy (26 out of 36), due to increasing fracture extension, pain > 7 and pronounced immobility (Fig. 5). In the interventional group, 3/10 had a FFP IIa, 4/10 a FFP IIb and 3/10 a FFP IIc fracture. In the surgical group, 6/26 had a FFP IIb and 20/26 a FFP IIc fracture.
Interventional
After sacroplasty, pain was reduced rapidly and significantly (p < 0.001), which quickly allowed a marked improvement in mobility, with no significant difference found between vertebro- (VSP), balloon (BSP), radiofrequency (RFS) and cement (CSP) sacroplasty (Fig. 6 a and b).
A threshold value for pain at 5 score points is marked in the graph by a solid horizontal line.
Patients in Groups 3 to 6 showed a significant (p < 0.001) reduction in pain as early as the second post-interventional day with a stable sustained effect over time, with no difference between groups.
A total of 109 out of 119 (91.6%) patients treated could still be contacted after 24 months.
The average HBI of all patients was 37 +/− 6 at baseline and 83 +/− 6 after 24 months. After 6 days, there was a significant (p < 0.001) improvement, with a sustained effect over 24 months. There was no significant difference between Groups 3 to 6 at p > 0.87.
A total of 119 patients underwent cement augmentation (Fig. 5). Cement leakage was found in 4 out of 20 patients (20%) after VSP (Group 3) and in 6 out of 49 patients (12.2%) after CSP (Group 4). None of the leaks were symptomatic. For BSP (Group 5) and RFS (Group 6) with 25 patients each, leakage was ruled out.
Osteosynthetic
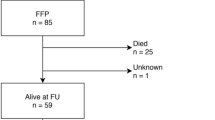
The planned osteosyntheses of 59 patients with the following fracture morphology:
-
FFP type II = Group 7: 2 FFP type II a, 3 FFP type II b and 9 FFP type II c;
-
FFP type III = Group 8: 14 FFP type III c and.
-
FFP type IV = Group 9: 26 FFP type IV b and 5 FFP type IV c
were carried out as planned (Fig. 5).
Iliosacral screw fixation was performed 38 times (with additional cement augmentation in 32 of 38), transsacral screw fixation 8 times, a transsacral positioning rod 3 times, percutaneous plate osteosynthesis once, lumbopelvic stabilisation 8, and an internal fixator with additional transiliac screw fixation once.
In terms of pain reduction and mobilisation capacity, patients benefited from osteosynthesis, although more complex fracture types with lumbopelvic stabilisation performed required a longer period of recovery (Fig. 7 a and b).
A threshold value for pain at 5 score points is marked in the graph by a solid horizontal line.
Baseline pain is most pronounced in patients with more complex fractures (Group 9 - FFP type IV), with pain declining less rapidly over the postoperative course compared to Group 7 - FFP type II and Group 8 - FFP type III, the differences were not significant. After 12 months, the pain levels were more or less evened out at a low level. Forty five of 59 (76.3%) patients could still be contacted after 24 months.
The average HBI of all patients was 35 +/− 4 at baseline and 84 +/− 6 after 24 months, with no relevant difference between the groups at these points.
The patients in Group 9 - FFP type IV were significantly less mobile on postoperative day 6 than the patients in Group 7 - FFP type II and Group 8 - FFP type III.
Material loosening occurred in 8 of 59 patients, but this did not require revision.
There were no deaths during the hospital stay.
In the assessment of self-reliance, patients achieved an average of 76 score points after conservative therapy, 83 score points after sacroplasty and 84 score points after osteosynthesis at the end of 24 months.
However, of the 292 patients treated, only 81 patients (27.7%) achieved the same physical fitness as before the fracture event.
Mortality
The mortality rate after 12 months was 21.7% for the conservative, 8.4% for the interventional and 13.6% for the surgical therapy group; the differences are significant. In patients in the conservative therapy group who were difficult to mobilise due to pain, the mortality rate increased to 24.3% (Table 2).
Over a period of 12 months after the start of therapy, the deceased could be clearly recorded.
The average percentages differed significantly between Groups 1 and 2 at p < 0.05. No significant difference was found between Groups 3 to 6 and Groups 7 to 9 at p > 0.83.
The conservatively treated patients showed a significant difference compared to the interventionally treated patients at p < 0.001 and compared to the osteosynthetic treated patients at p < 0.05, with an effect size of 0.87 and 0.74, respectively.
Patient satisfaction
Subjective satisfaction with the therapies was best after sacroplasty at 12 and 24 months, followed by osteosynthesis and conservative measures (Table 3).
Vitamin D and BMD
All patients had a pronounced vitamin D deficiency and manifest osteoporosis.
Vitamin D
The vitamin D level was significantly (p < 0.001) lower than 30 nmol/l ≙ 12 ng/ml in all patients. Vitamin D levels were 8 - 28 (Ø 14.1) nmol/l ≙ 3.2 - 11.2 (Ø 5.6) ng/ml in unilateral fractures and 0 - 18 (Ø 7.2) nmol/l ≙ 0 - 7.2 (Ø 2.9) ng/ml in bilateral, more complex fractures (Fig. 8), the difference in mean vitamin D levels being significant (p < 0.05).
BMD
The BMD was 12-74 (Ø 44.3) mg/ml in the patients with a unilateral fracture and 2 - 54 (Ø 31.3) mg/ml in the patients with a bilateral fracture (Fig. 8), the difference in mean BMC values being significant (p < 0.05).
Disease profile
In 128 of 292 (43.8%) patients in total, at least one previous sintering fracture was found in the thoracic and lumbar spine. Other osteoporosis-associated fractures such as distal radius, proximal humerus, femoral neck, rib and sternal fractures were found in 142 of the 292 (48.6%) patients. Hypocalcaemia was found in 35% and secondary hyperparathyroidism in 48% of all patients. Additional lung disease was found in 23.6%, cardiovascular disease in 45.2%, hypertension in 77.1%, renal insufficiency in 34.2%, diabetes mellitus type II in 72.8%, PAOD in 70.3% and obesity in 60.2% of all patients. A varying degree of nicotine consumption was reported by 48.3% of all patients.
Discussion
Up to our knowledge, this is the first study which compared the outcome of three different therapy options for the treatment of FFS.
Clinical aspects and profile of the patients
As in other publications, the risk factors confirmed in our patient population with sacral insufficiency fractures were advanced age [1, 5, 12, 30], female gender [9, 12, 31], drastic vitamin D deficiency [32, 33] and osteoporosis [30, 33, 34]. As in Maier et al. [33], where the measurement was done by DXA, all our patients also showed osteoporosis in the osteodensitometric measurement by QCT. The BMD values of the QCT measurement on the axial skeleton were clearly below the threshold for osteoporosis of 80 mg/ml [35], whereby the significantly lowest values were found in complex sacral fractures, with an average of 31.3 mg/ml. The additional sintering fractures of 43.8% of all patients in the axial skeleton and fractures of 48.6% of all patients in the peripheral skeletal region support the presence of clinically manifest osteoporosis in the patient collective.
The fracture types found most frequently were a Denis 1 in 42.4% and Denis 1-2 in 43.3% and an FFP II in 85.7%, this distribution also being found by other working groups [26, 36]. With generally preceding fracture dynamics [37, 38], which were shown by varying degrees of oedema and sclerosis of individual fracture zones in contralateral comparison, bilateral sacral fractures were clearly predominant, with 68.8% in 292 patients. Since bilateral fractures are more unstable [38] and allow more micromovements in the fracture zones, this also explains the high level of pain and the pain-related immobility of our patients, which was comparable to the findings of a previous study [34]. The number and percentage distribution of additional concomitant diseases are similar to those found by Maier et al. [33].
Outcome in the comparison of conservative, interventional and osteosynthetic therapies, considering pain, mobility and patient satisfaction
Conservative
Patients with baseline pain ≤5 (Group 1) on the VAS experienced a reduction in pain (Fig. 4a) and an increase in mobility and self-reliance (Fig. 4b) at an acceptable level with moderate patient satisfaction (Table 3). In the patients with initial pain > 5 (Group 2), there was a clearly delayed reduction in pain (Fig. 4a) and a moderate improvement in self-reliance (Fig. 4b) accompanied by poor satisfaction with the situation after the fracture event (Table 3). Maier et al. [33] also found a significant loss of self-reliance under conservative therapy after a fracture event. If there was no response to therapy, 36 out of 100 patients were transferred to the interventional or osteosynthetic therapy group, a procedure also recommended by Josten & Höch [37]. Nuber et al. [39] recommend osteosynthesis if conservative therapy fails, while others prefer sacroplasty [34, 40]. Especially if fracture progression then occurs with increasing instability, osteosynthesis should be performed at an early stage [37, 41].
Interventional
In comparison, after sacroplasty (Group 3 = VSP, Group 4 = BSP, Group 5 = RFS and Group 6 = CSP), the patients experienced a rapid and significant reduction in pain (Fig. 6a) with a rapid and significant improvement in self-reliance (Fig. 6b) and good patient satisfaction (Table 3) without any difference between the groups, as is to be expected given the same mechanism of action [26, 42]. The mechanism of action is based on stabilisation and minimisation of micromovements by the PMMA cement plug inserted into the fracture zone [43,44,45], which leads to a reduction in pain. Rapid, significant and sustained pain reduction is the greatest benefit for patients after sacroplasty. This has been found by many studies [26, 34, 42, 46,47,48,49,50,51,52] and is supported by comparable results from multicentre studies [53, 54], systematic reviews and meta-analyses [8, 55,56,57,58,59]. Schwetje et al. [51] were also able to show a significant increase in mobility after BSP in the absence of an effect under conservative therapy.
Osteosynthetic
Starting from a high level of pain, there was a significant overall reduction in pain after the 6th postoperative day, with patients with FFP type II and FFP type III showing a clearer reduction in pain than patients with FFP type IV (Fig. 7a), which was also reflected in the mobility development based on the HBI (Fig. 7b). The minimally invasive osteosyntheses performed in our patients led to primary stability with the possibility of full weight-bearing and pain-oriented mobilisation. Depending on the extent of fracture classification and assessed instability, as in other study groups [27, 37, 60, 61], iliosacral screw fixation was used most frequently, followed by transsacral screw fixation, transsacral positioning rod, plate osteosynthesis, lumbopelvic stabilisation and internal fixator with transiliac screw fixation. The iliosacral screw osteosynthesis leads to good compression and thus stabilisation, especially in vertically running fracture zones [61, 62]. This can be used to achieve a significant reduction in pain, as in our patients [63]. Due to the pronounced osteopenic bone texture, additional cement augmentation was performed in 32 of 38 iliosacral screws inserted. This procedure appears to be safe, promises greater stability and minimises the risk of complications [64, 65]. As in our case, Höch et al. [64] found a significant and sustained reduction in pain postoperatively in older, osteoporotic patients. Biomechanically, cement augmentation also reduces screw loosening in osteoporotic bone, supporting this approach [66]. In 8 out of 59 osteosyntheses, a transsacral screw fixation was performed, which allows an alternative to the cemented iliosacral screw due to a bilateral anchorage of the screw in the ilium [67], whereby no difference was found in the outcome in our patients. In 8 of 59 patients with a bilateral sacral fracture corresponding to an FFP type IV b without major dislocations of the sacral fracture fragments, good primary stability could be achieved by minimally invasive lumbopelvic stabilisation, as also presented by other working groups [60, 63, 68, 69]. With regard to pain reduction, mobility development and subjective satisfaction, however, an acceptable clinical improvement was only seen over the postoperative course after 6 to 12 months, comparable to the results of Mendel et al. [69].
Outcome considering complications and mortality
With regard to pain reduction and mobility development, patients with baseline pain > 5 on the VAS (Group 2) showed the worst development under conservative therapy, which was already found to be comparable elsewhere [34]. Patients with baseline pain < 5 on the VAS (Group 1) were better mobilised and benefited from conservative therapy [11, 70]. Concomitant diseases such as phlebothrombosis with pulmonary artery embolism, pneumonia and urosepsis were highest in patients with poor mobility development and primarily affected Group 2. After sacroplasty (Groups 3 - 6) and osteosynthesis (Groups 7 - 9) these were less frequent in percentage terms.
A comparison of the mortality rates yielding significant effects appears to be possible for a time span of 12 months after the start of therapy, and they can be reliably assigned to the different therapies, see Table 2.
A mortality rate of 21.7% in the conservative group (average value from Groups 1 and 2) was also found by other research groups [33, 34, 71, 72]. In patients who are difficult to mobilise due to severe pain, the 12-month mortality rate increases under conservative measures to 24.3%.
Patients in Groups 3-6 benefit considerably from the significant, short-term reduction in pain and the resulting rapid mobilisation after sacroplasty; the 12-month mortality rate was 8.4% on average. A similar tendency was already shown in a preliminary study comparing conservative therapy with a mortality of 23.5% against BSP with a mortality of 3% after 12 months [34]. There was no significant difference between VSP, BSP, RFS and CSP.
Patients in Groups 7-9 also seem to benefit significantly from surgery compared to conservative therapy, with an average 12-month mortality of 13.6%, despite an initial situation with more complex fractures, a higher pain level and poorer HBI. This is also in line with the results of Bible et al. [73], who were able to show that after conservative fracture treatment, mortality after one year was twice as high (15%) as after surgical stabilisation. Hoech et al. [74] found a significantly higher survival rate for surgically treated patients of 21% compared to conservatively treated patients over a two-year period. With a comparable distribution of FFP types, Rommens et al. [75] also found a lower mortality in surgically treated patients. The one-year mortality rate of surgically treated patients with FFP types II-IV was halved in comparison with conservatively treated patients [76]. As in our case, surgically treated patients benefit from minimally invasive percutaneous procedures in terms of complication rate and mortality [77].
Strengths and limitations
The benefit of our study is the multicenter design and the comparison of three different treatment modalities for addressing FFS with outcome measurements over a period of 24 months.
Limitations are the retrospective study design, the treatment of different fracture types and a bias due to the selection of the type of treatment (surgical versus interventional).
Conclusions
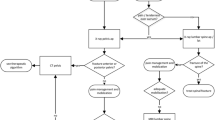
In order to avoid consecutive disablement, prompt diagnostics and multimodal, interdisciplinary therapy are necessary in patients with FFS. Patients with a low level of pain can be treated conservatively [11]. Patients with severe pain and non-dislocated fractures benefit from cement augmentation effectively and sustainably, whereby different methods are available [26]. Patients with disabling pain and unstable fractures should be treated osteosynthetically as early as possible [37]. Regardless of whether a conservative, interventional or osteosynthetic therapy is chosen, a guideline-compliant antiosteoporotic treatment [29] is necessary, whereby to accelerate fracture healing an osteoanabolic treatment [78] should be chosen. A diagnostic and therapeutic algorithm for managing FFS is shown in Fig. 9.
Availability of data and materials
The datasets used and analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- ANOVA:
-
Analysis of variance
- CSP:
-
Cement sacroplasty
- BMD:
-
Bone mineral density
- BSP:
-
Balloon sacroplasty
- CT:
-
Computed tomography
- FFS:
-
Fragility fractures of the sacrum
- FFP:
-
Fragility fractures of the pelvis
- HBI:
-
Hamburg Barthel index
- MRI:
-
Magnetic resonance imaging
- PAOD:
-
Peripheral arterial occlusive disease
- PMMA:
-
Polymethyl methacrylate
- QCT:
-
Quantitative computed tomography
- RFS:
-
Radiofrequency sacroplasty
- STIR:
-
Short-Tau inversion recovery
- VAS:
-
Visual analogue scale
- VSP:
-
Vertebro sacroplasty
- WHO:
-
World Health Organization
References
Gotis-Graham I, McGuigan L, Diamond T, Portek I, Quinn R, Sturgess A, et al. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br. 1994;76:882–6.
West SG, Troutner JL, Baker MR, Place HM. Sacral insufficiency fractures in rheumatoid arthritis. Spine. 1994;19:2117–21. https://doi.org/10.1097/00007632-199409150-00021.
Kim HJ, Boland PJ, Meredith DS, Lis E, Zhang Z, Shi W, et al. Fractures of the sacrum after chemoradiation for rectal carcinoma: incidence, risk factors, and radiographic evaluation. Int J Radiat Oncol Biol Phys. 2012;84:694–9. https://doi.org/10.1016/j.ijrobp.2012.01.021.
Lin JT, Lane JM. Sacral stress fractures. J Women's Health. 2003;12:879–88. https://doi.org/10.1089/154099903770948104.
Andrich S, Haastert B, Neuhaus E, Neidert K, Arend W, Ohmann C, et al. Epidemiology of pelvic fractures in Germany: considerably high incidence rates among older people. PLoS One. 2015;10:e0139078. https://doi.org/10.1371/journal.pone.0139078.
Schindler OS, Watura R, Cobby M. Sacral insufficiency fractures. J Orthopaedic Surg. 2007;15:339–46. https://doi.org/10.1177/230949900701500320.
Lourie H. Spontaneous osteoporotic fracture of the sacrum. An unrecognised syndrome of the elderly. JAMA. 1982;248:715–7.
Urits I, Orhurhu V, Callan J, Maganty NV, Pousti S, Simopoulos T, et al. Sacral insufficiency fractures: a review of risk factors, clinical presentation, and management. Curr Pain Headache Rep. 2020;24:1–9. https://doi.org/10.1007/s11916-020-0848-z.
Grasland A. Sacral insufficiency fractures. Arch Intern Med. 2011;156:668–74.
Coordinated population projection. https://service.destatis.de/bevoelkerungspyramide/. Statistisches Bundesamt 2016; viewed: 10.02.2022.
Kandziora F, Yildiz U. Fractures of the sacrum: operative/conservative. Die Wirbelsäule. 2017;1:41–50.
Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970- 1997 and alarming projections for the new millennium. Osteoporos Int. 2000;11:443–8. https://doi.org/10.1007/s001980070112.
Lyders EM, Whitlow CT, Baker MD, Morris PP. Imaging and treatment of sacral insufficiency fractures. Am J Neuroradiol. 2010;31:201–10. https://doi.org/10.3174/ajnr.A1666.
Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44:1733–44. https://doi.org/10.1016/j.injury.2013.06.023.
Rommens PM, Drees P, Thomczyk S, Betz U, Wagner D, Hofmann A. The fragility fracture of the pelvis is a fracture indicating osteoporosis. Osteol. 2018;27:144–53. https://doi.org/10.1055/s-0038-1673536.
Cosker TD, Ghandour A, Gupta SK, Tayton KJ. Pelvic ramus fractures in the elderly: 50 patients studied with MRI. Acta Orthop. 2005;76:513–6. https://doi.org/10.1080/17453670510044634.
Alnaib M, Waters S, Shanshal Y, Caplan N, Jones S, St Clair Gibson A, et al. Combined pubic rami and sacral osteoporotic fractures: a prospective study. J Orthop Traumatol. 2012;13:97–103. https://doi.org/10.1007/s10195-012-0182-2.
Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Rommens PM. Sacral bone mass distribution assessed by averaged three-dimensional CT models: implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg Am. 2016;98:584–90. https://doi.org/10.2106/JBJS.15.00726.
De Smet AA, Neff JR. Pubic and sacral insufficiency fractures: clinical course and radiologic findings. Am J Roentgenol. 1985;145:601–6. https://doi.org/10.2214/ajr.145.3.601.
Peh WC, Khong PL, Yin Y, Ho WY, Evans NS, Gilula LA, et al. Imaging of pelvic insufficiency fractures. Radiographics. 1996;16:335–48. https://doi.org/10.1148/radiographics.16.2.8966291.
Aretxabala I, Fraiz E, Pérez-Ruiz F, Ríos G, Calabozo M, Alonso-Ruiz A. Sacral insufficiency fractures. High association with pubic rami fractures. Clin Rheumatol. 2000;19:399–401. https://doi.org/10.1007/pl00011178.
Muthukumar T, Butt SH, Cassar-Pullicino VN, McCall IW. Cauda equina syndrome presentation of sacral insufficiency fractures. Skelet Radiol. 2007;36:309–13. https://doi.org/10.1007/s00256-006-0239-5.
Gift AG. Visual analogue scales: measurement of subjective phenomena. Nurs Res. 1989;38:286–8. https://doi.org/10.1097/00006199-198909000-00006.
Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81.
Kumle B, Wilke P, Koppert W, Kumle K, Gries A. Pain therapy in emergency medicine. Focus on emergency admissions. Anaesthesist. 2013;62:902–8. https://doi.org/10.1007/s00101-013-2247-x.
Andresen R, Radmer S, Wollny M, et al. CT-guided balloon sacroplasty (BSP), radiofrequency sacroplasty (RFS), vertebrosacroplasty (VSP) and cement sacroplasty (CSP) in non-dislocated insufficiency fractures - a comparison of methods with regard to outcome, costs and reimbursement. Die Wirbelsäule. 2018;2:75–84.
Oberkircher L, Ruchholtz S, Rommens PM, Hofmann A, Bücking B, Krüger A. Osteoporotic pelvic fractures. Dtsch Arztebl Int. 2018;115:70–80. https://doi.org/10.3238/arztebl.2018.0070.
Lübke N, Meinck M, Von Renteln-Kruse W. The Barthel index in geriatrics. A context analysis for the Hamburg classification manual. Z Gerontol Geriat. 2004;37:316–26. https://doi.org/10.1007/s00391-004-0233-2.
Thomasius F, Baum E, Bernecker P, Böcker W, Brabant T, Clarenz P, et al. S-3 DVO guidelines 2017 in prophylaxis, diagnosis and therapy of osteoporosis in postmenopausal women and men. Osteol. 2018;27:154–60. https://doi.org/10.1055/s-0038-1673537.
Wagner D, Hofmann A, Kamer L, Sawaguchi T, Richards RG, Noser H, et al. Fragility fractures of the sacrum occur in elderly patients with severe loss of sacral bone mass. Arch Orthop Trauma Surg. 2018;138:971–7. https://doi.org/10.1007/s00402-018-2938-5.
Kannus P, Palvanen M, Parkkari J, Niemi S, Järvinen M. Osteoporotic pelvic fractures in elderly women. Osteoporos Int. 2005;16:1304–5. https://doi.org/10.1007/s00198-005-1941-1.
Breuil V, Roux CH, Testa J, Albert C, Chassang M, Brocq O, et al. Outcome of osteoporotic pelvic fractures: an underestimated severity. Survey of 60 cases. Joint Bone Spine. 2008;75:585–8. https://doi.org/10.1016/j.jbspin.2008.01.024.
Maier GS, Kolbow K, Lazovic D, Horas K, Roth KE, Seeger JB, et al. Risk factors for pelvic insufficiency fractures and outcome after conservative therapy. Arch Gerontol Geriatr. 2016;67:80–5. https://doi.org/10.1016/j.archger.2016.06.020.
Andresen R, Radmer S, Lüdtke CW, Kamusella P, Görmez M, Wissgott C, et al. Conservative therapie versus CT guided balloon sacroplasty in the treatment of insufficiency fractures of the sacrum. Osteol. 2015;24:92–8. https://doi.org/10.1055/s-0037-1622046.
Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, et al. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD official positions. J Clin Densitom. 2008;11:123–62. https://doi.org/10.1016/j.jocd.2007.12.010.
Sterneder M, Lang P, Riesner HJ, Hackenbroch C, Friemert B, Palm HG. Insufficiency fractures vs. low-energy pelvic ring fractures - epidemiological, diagnostic and therapeutic characteristics of fragility fractures of the pelvic ring. Z Orthop Unfall. 2022;160:497–506. https://doi.org/10.1055/a-1394-6502.
Josten C, Höch A. Fractures of the sacrum: operative/conservative; pro: why insufficiency fractures of the sacrum should be treated operatively. Die Wirbelsäule. 2017;01:31–40.
Mendel T, Ullrich BW, Hofmann GO, Schenk P, Goehre F, Schwan S, et al. Progressive instability of bilateral sacral fragility fractures in osteoporotic bone: a retrospective analysis of X-ray, CT, and MRI datasets from 78 cases. Eur J Trauma Emerg Surg. 2021;47:11–9. https://doi.org/10.1007/s00068-020-01480-4.
Nuber S, Ritter B, Fenwick A, Förch S, Wanzl M, Nuber M, et al. Midterm follow-up of elderly patients with fragility fractures of the pelvis: a prospective cohort-study comparing operative and non-operative treatment according to a therapeutic algorithm. Injury. 2021;S0020-1383:00825–1. https://doi.org/10.1016/j.injury.2021.09.044.
Sahota O, Leighton P, Cameron M, Taylor R, Ong T, Drummond A, et al. ASSERT (acute sacral inSufficiEncy fractuRe augmenTation): perceptions in the assessment and treatment of pubic rami and sacral fragility fractures amongst healthcare professionals in geriatric medicine and surgery-a qualitative study. Geriatr Orthop Surg Rehabil. 2021;12:21514593211026794. https://doi.org/10.1177/21514593211026794.
Ueda Y, Inui T, Kurata Y, Tsuji H, Saito J, Shitan Y. Prolonged pain in patients with fragility fractures of the pelvis may be due to fracture progression. Eur J Trauma Emerg Surg. 2021;47:507–13. https://doi.org/10.1007/s00068-019-01150-0.
Andresen R, Radmer S, Andresen JR, Schober HC. Comparison of the 18 months outcome after the treatment of osteoporotic insufficiency fractures by means of balloon sacroplasty (BSP) and radiofrequency sacroplasty (RFS) in comparison: a prospective randomised study. Eur Spine J. 2017;26:3235–40. https://doi.org/10.1007/s00586-016-4935-0.
Whitlow CT, Yazdani SK, Reedy ML, Kaminsky SE, Berry JL, Morris PP. Investigating sacroplasty: technical considerations and finite element analysis of polymethylmethacrylate infusion into cadaveric sacrum. Am J Neuroradiol. 2007;28:1036–41. https://doi.org/10.3174/ajnr.A0500.
Anderson DE, Cotton JR. Mechanical analysis of percutaneous sacroplasty using CT image based finite element models. Med Eng Phys. 2007;29:316–25. https://doi.org/10.1016/j.medengphy.2006.03.008.
Richards AM, Mears SC, Knight TA, Dinah AF, Belkoff SM. Biomechanical analysis of sacroplasty: does volume or location of cement matter? Am J Neuroradiol. 2009;30:315–17. https://doi.org/10.3174/ajnr.A1358.
Andresen R, Radmer S, Andresen JR, Wollny M, Nissen U, Schober HC. Clinical improvement and cost-effectiveness of CT-guided radiofrequency Sacroplasty (RFS) and cement Sacroplasty (CSP) - a prospective randomised comparison of methods. Z Orthop Unfall. 2019;157:524–33. https://doi.org/10.1055/a-0815-5073.
Eichler K, Zangos S, Mack MG, Marzi I, Vogl TJ. Outcome of long-axis percutaneous sacroplasty for the treatment of sacral insufficiency fractures with a radiofrequency-induced, high-viscosity bone cement. Skelet Radiol. 2014;43:493–8. https://doi.org/10.1007/s00256-013-1811-4.
Andresen R, Lüdtke CW, Radmer S, Kamusella P, Schober HC. Radiofrequency sacroplasty (RFS) for the treatment of osteoporotic insufficiency fractures. Eur Spine J. 2015;24:759–63. https://doi.org/10.1007/s00586-014-3638-7.
Yang SC, Tsai TT, Chen HS, Fang CJ, Kao YH, Tu YK. Comparison of sacroplasty with or without balloon assistance for the treatment of sacral insufficiency fractures. J Orthop Surg (Hong Kong). 2018;26:2309499018782575. https://doi.org/10.1177/2309499018782575.
Gibbs WN, Doshi A. Sacral fractures and sacroplasty. Neuroimaging Clin N Am. 2019;29:515–27. https://doi.org/10.1016/j.nic.2019.07.003.
Schwetje D, Wahd YESH, Bornemann R, Jansen TR, Pflugmacher R, Kasapovic A. Balloon-assisted sacroplasty as a successful procedure for osteoporotic sacral insufficiency fractures after failure of the conservative treatment. Sci Rep. 2020;10:18455. https://doi.org/10.1038/s41598-020-75384-z.
Lee J, Lee E, Lee JW, Kang Y, Ahn JM, Kang HS. Percutaneous sacroplasty: effectiveness and long-term outcome predictors. J Korean Neurosurg Soc. 2020;63:747–56. https://doi.org/10.3340/jkns.2020.0014.
Frey ME, Depalma MJ, Cifu DX, Bhagia SM, Carne W, Daitch JS. Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J. 2008;8:367–73. https://doi.org/10.1016/j.spinee.2007.05.011.
Kortman K, Ortiz O, Miller T, Brook A, Tutton S, Mathis J, et al. Multicenter study to assess the efficacy and safety of sacroplasty in patients with osteoporotic sacral insufficiency fractures or pathologic sacral lesions. J Neurointerv Surg. 2013;5:461–6. https://doi.org/10.1136/neurintsurg-2012-010347.
Andresen JR, Radmer S, Prokop A, Wollny M, Nissen U, Schober HC, et al. Diagnostics and treatment of sacral insufficiency fractures with special attention to cement augmentation procedures - an overview. Osteol. 2021;30:163–72. https://doi.org/10.1055/a-1154-9185.
Bayley E, Srinivas S, Boszczyk BM. Clinical outcomes of sacroplasty in sacral insufficiency fractures: a review of the literature. Eur Spine J. 2009;18:1266–71. https://doi.org/10.1007/s00586-009-1048-z.
Chandra V, Wajswol E, Shukla P, Contractor S, Kumar A. Safety and efficacy of sacroplasty for sacral fractures: a systematic review and meta-analysis. J Vasc Interv Radiol. 2019;30:1845–54. https://doi.org/10.1016/j.jvir.2019.06.013.
Mahmood B, Pasternack J, Razi A, Saleh A. Safety and efficacy of percutaneous sacroplasty for treatment of sacral insufficiency fractures: a systematic review. J Spine Surg. 2019;5:365–71. https://doi.org/10.21037/jss.2019.06.05.
Chang S, Doshi AH, Gibbs WN, et al. Sacral augmentation: comprehensive review. In: Khan M, Kushchayev SV, Faro SH, editors. Image guided interventions of the spine. Springer: Cham; 2021. p. 145–58.
Rommens PM, Wagner D, Hofmann A. Minimal invasive surgical treatment of fragility fractures of the pelvis. Chirurgia (Bucur). 2017;112:524–37. https://doi.org/10.21614/chirurgia.112.5.524.
Spiegl UJA, Schnake KJ, Ullrich B, Scheyerer MJ, Osterhoff G, Siekmann H. Current minimally invasive surgical concepts for sacral insufficiency fractures. Z Orthop Unfall. 2021;xx:xxx–x. https://doi.org/10.1055/a-1498-2975 Epub ahead of print.
Decker S, Krettek C, Stübig T. Minimally invasive stabilization of sacral fractures. Unfallchirurg. 2020;123:774–82. https://doi.org/10.1007/s00113-020-00853-z.
Hopf JC, Krieglstein CF, Müller LP, Koslowsky TC. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury. 2015;46:1631–6. https://doi.org/10.1016/j.injury.2015.04.036.
Höch A, Pieroh P, Henkelmann R, Josten C, Böhme J. In-screw polymethylmethacrylate-augmented sacroiliac screw for the treatment of fragility fractures of the pelvis: a prospective, observational study with 1-year follow-up. BMC Surg. 2017;17:132. https://doi.org/10.1186/s12893-017-0330-y.
Hartensuer R, Lodde MF, Keller J, Eveslage M, Stolberg-Stolberg J, Riesenbeck O, et al. Safety, effect and feasibility of percutaneous SI-screw with and without augmentation - a 15-year retrospective analysis on over 640 screws. J Clin Med. 2020;9:2660. https://doi.org/10.3390/jcm9082660.
Lodde MF, Katthagen JC, Schopper CO, Zderic I, Richards RG, Gueorguiev B, et al. Does cement augmentation of the sacroiliac screw lead to superior biomechanical results for fixation of the posterior pelvic ring? A biomechanical study. Medicina (Kaunas). 2021;57:1368. https://doi.org/10.3390/medicina57121368.
Eckardt H, Egger A, Hasler RM, Zech CJ, Vach W, Suhm N, et al. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: assessment of complications and factors influencing failure. Injury. 2017;48:2717–23. https://doi.org/10.1016/j.injury.2017.11.002.
Riesner HJ, Palm HG, Friemert B, Lang P, Becken AG, DGU®. Triangular minimally invasive spinopelvic stabilization for type C pelvic fractures according to AO/OTA and type IV according to FFP. Unfallchirurg. 2021;124:923–30. https://doi.org/10.1007/s00113-020-00952-x.
Mendel T, Schenk P, Ullrich BW, Hofmann GO, Goehre F, Schwan S, et al. Mid-term outcome of bilateral fragility fractures of the sacrum after bisegmental transsacral stabilization versus spinopelvic fixation. Bone Joint J. 2021;103-B:462–8. https://doi.org/10.1302/0301-620X.103B3.BJJ-2020-1454.R1.
Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures: to ambulate or not to ambulate? Am J Phys Med Rehabil. 2000;79:404–9. https://doi.org/10.1097/00002060-200007000-00014.
Park JW, Park SM, Lee HJ, Lee CK, Chang BS, Kim H. Mortality following benign sacral insufficiency fracture and associated risk factors. Arch Osteoporos. 2017;12:100. https://doi.org/10.1007/s11657-017-0395-3.
Omichi T, Takegami Y, Tokutake K, Saito Y, Ito O, Ando T, et al. Mortality and functional outcomes of fragility fractures of the pelvis by fracture type with conservative treatment: a retrospective, multicenter TRON study. Eur J Trauma Emerg Surg. 2022;48:2897–904. https://doi.org/10.1007/s00068-021-01839-1.
Bible JE, Kadakia RJ, Wegner A, Richards JE, Mir HR. One-year mortality after isolated pelvic fractures with posterior ring involvement in elderly patients. Orthopedics. 2013;36:760–4. https://doi.org/10.3928/01477447-20130523-21.
Höch A, Özkurtul O, Pieroh P, Josten C, Böhme J. Outcome and 2-year survival rate in elderly patients with lateral compression fractures of the pelvis. Geriatr Orthop Surg Rehabil. 2017;8:3–9. https://doi.org/10.1177/2151458516681142.
Rommens PM, Boudissa M, Krämer S, Kisilak M, Hofmann A, Wagner D. Operative treatment of fragility fractures of the pelvis is connected with lower mortality. A single institution experience. PLoS One. 2021;16:e0253408. https://doi.org/10.1371/journal.pone.0253408.
Rommens PM, Hopf JC, Arand C, Handrich K, Boudissa M, Wagner D. Prospective assessment of key factors influencing treatment strategy and outcome of fragility fractures of the pelvis (FFP). Eur J Trauma Emerg Surg. 2022;48:3243–56. https://doi.org/10.1007/s00068-022-01887-1.
Gericke L, Fritz A, Osterhoff G, Josten C, Pieroh P, Höch A. Percutaneous operative treatment of fragility fractures of the pelvis may not increase the general rate of complications compared to non-operative treatment. Eur J Trauma Emerg Surg. 2022;48:3729–35. https://doi.org/10.1007/s00068-021-01660-w.
Yoo JI, Ha YC, Ryu HJ, Chang GW, Lee YK, Yoo MJ, et al. Teriparatide treatment in elderly patients with sacral insufficiency fracture. J Clin Endocrinol Metab. 2017;102:560–5. https://doi.org/10.1210/jc.2016-3582.
Acknowledgements
Not applicable.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
JRA, RA and HCS contributed to conceptualization. SR, AP and GS were involved in data acquisitions. JRA, SR, RA, AP, GS, UN and HCS contributed to data analysis or interpretation. JRA, SR, RA and HCS were involved in drafting of the manuscript. All authors contributed to critical revision of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present research conforms to the principles laid down in the Declaration of Helsinki and its amendments. This study has been approved by the competent institutional ethics committee of the University of Rostock (Trial registration No. A 2020-0015). Written information consent for publication was obtained from all participants.
Consent for publication
All authors gave their consent for this publication.
Competing interests
The author(s) declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Andresen, J.R., Radmer, S., Andresen, R. et al. Comparative outcome of different treatment options for fragility fractures of the sacrum. BMC Musculoskelet Disord 23, 1106 (2022). https://doi.org/10.1186/s12891-022-06039-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-06039-5