Abstract
Background
Spine disorders are becoming more prevalent in today’s ageing society. Motion abnormalities have been linked to the prevalence and recurrence of these disorders. Various protocols exist to measure thoracolumbar spine motion, but a standard multi-segmental approach is still missing. This study aims to systematically evaluate the literature on stereophotogrammetric motion analysis approaches to quantify thoracolumbar spine kinematics in terms of measurement reliability, suitability of protocols for clinical application and clinical significance of the resulting functional assessment.
Methods
Electronic databases (PubMed, Scopus and ScienceDirect) were searched until February 2022. Studies published in English, investigating the intersegmental kinematics of the thoracolumbar spine using stereophotogrammetric motion analysis were identified. All information relating to measurement reliability; measurement suitability and clinical significance was extracted from the studies identified.
Results
Seventy-four studies met the inclusion criteria. 33% of the studies reported on the repeatability of their measurement. In terms of suitability, only 35% of protocols were deemed suitable for clinical application. The spinous processes of C7, T3, T6, T12, L1, L3 and L5 were the most widely used landmarks. The spine segment definitions were, however, found to be inconsistent among studies. Activities of daily living were the main tasks performed. Comparable results between protocols are however still missing.
Conclusion
The literature to date offers various stereophotogrammetric protocols to quantify the multi-segmental motion of the thoracolumbar spine, without a standard guideline being followed. From a clinical point of view, the approaches are still limited. Further research is needed to define a precise motion analysis protocol in terms of segment definition and clinical relevance.
Similar content being viewed by others
Background
Spinal disorders such as low back pain (LBP) and adult spine deformity (ASD) are becoming more prevalent in today’s ageing society [1, 2], with LBP being the leading global cause of years lived with disease [3, 4] and ASD prevalence rates ranging between 32 and 68% in individuals over the age of 60 [5, 6]. Patients could present with mild to severe symptoms [7] impairing their mobility from gait disturbances to limitations in the spine range of motion (ROM) [8, 9]. Treatment for spinal disorders depends on the severity of the disease [1], when non-operative treatments are exhausted, surgical interventions are needed to provide pain relief or correct deformity [1, 10]; however, the failure rates remain high following surgery ranging between 10 and 46% [7] due to instrumentation failure or sagittal imbalance [7, 10]. These disorders include a wide range of clinical and radiographical characteristics [6]. However, current research suggests that movement abnormalities impact the prevalence of spinal disorders and the recurrence of the disease following treatment [11, 12], hence the need for a better understanding of spine kinematics to improve treatment decisions and outcomes [13, 14].
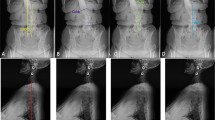
Different quantification methods are available to quantitatively characterize spine kinematics and posture. i) Spinal alignment angles in the frontal and sagittal planes are quantified in static conditions by means of imaging techniques [15], such as X-rays, CT or MRI scans [9, 15, 16]. These angles are commonly used in clinical practice to support diagnosis, surgical planning, and pre- and post-intervention assessment [9], but do not provide any characterization of spine function in dynamic conditions [16]. Static measurements are also affected by the limited repeatability of the measurements [15] with up to 20% change in lumbar lordosis values in subjects inter-session [17]. Additionally, depending on the spine pathology, imaging techniques are highly affected by lower levels of sensitivity, specificity and an increased rate of false positives with MRI being the most specific and sensitive test for LBP [18]. ii) Intervertebral 3D kinematics can be quantified using video-fluoroscopy [15, 16].This technique is highly accurate, detecting intervertebral ROM with a measurement error varying between 0.32° and 0.52° in the coronal and sagittal plane, respectively [19], but it is not exploited in clinical practice due to the small imaging volume preventing the analysis of spine segments, and due to the critical ionizing radiations exposure [20]. iii) Spine 3D angles can be quantified non-invasively using stereophotogrammetric motion analysis [21] without field of view limitations, allowing also for the assessment during daily living activities [22, 23], but can potentially be affected by significant experimental errors [24]. An overview of stereophotogrammetric motion analysis of the spine can be seen in Fig. 1.
Stereophotogrammetric motion analysis is extensively used for the assessment of body segment kinematics during gait and other functional tasks [25, 26]; although specific protocols and biomechanical models used for the assessment can differ [27]. Body segments (i.e. trunk, pelvis and limb segments) and joint definitions are consistent among protocols [28, 29], while, for spine kinematics, a standard multi-segmental approach is still missing [24, 30].
To assess thoracolumbar spine kinematics in an everyday clinical setting, reliable, clinically significant, and comparable data need to be reported by spinal motion protocols to provide a functional assessment of each spine segment and supply clinicians with a tool to characterize thoracolumbar kinematics changed by different pathologies. To achieve this, a set of standards and guidelines need to be agreed upon with recommendations on the motion tasks to carry out, optimal segment definitions, data to be generated and requirements for a protocol to be suitable for clinical application. Some previous review papers assessing spine motion analysis partially covered the clinical significance of thoracolumbar spine kinematic protocols [24, 31,32,33,34] or provided methodological information on the protocols available [24, 25]. However, this review aims to provide a complete assessment of available protocols in terms of 1) reliability of the measurement, 2) suitability of the protocol for clinical application and 3) clinical significance of the reported results to unravel comparable outcomes between the protocols found and ultimately provide recommendations on the standards needed for thoracolumbar motion analysis. As LBP and ASD are pathologies that affect the thoracolumbar spine [1, 35], motion protocols of only the cervical spine were not included in this review.
The review uncovers information relating to the measurement repeatability and accuracy approaches, number of markers used, segment definitions, degrees of freedom assessed, motion analysis system used, task choice, number of participants included, main measurements reported, pathologies assessed, and clinical findings.
Methods
This systematic review was conducted in accordance with the PRISMA statement [36].
Study selection and research criteria
Article search was completed on the 7th of February 2022 on Scopus, PubMed, and Science Direct databases. The research keywords were customised to match each of the databases. Details of the research strings on each of the databases could be seen in Table 1. To understand the effect of LBP and ASD on the motion of the spine studies focusing solely on the cervical spine were excluded.
The outcomes of the searches on the different databases were merged into a single list.
Studies were included in the review if they met the following inclusion criteria:
-
1)
journal papers written in English,
-
2)
assessing the intersegmental motion of the thoracolumbar spine,
-
3)
using stereophotogrammetric motion analysis,
Articles passing inclusion criteria were retained as full-text documents.
Quality assessment
The quality of the included studies was assessed by one reviewer using a customised quality assessment questionnaire including 19 questions. Questions 1–12 were designed to appraise the general quality of the studies in terms of study design and reproducibility of the method used. Questions 13 to 19 were specifically designed to assess the reliability of the measurement approach, the suitability of the approach to be used in a clinical setting and the clinical significance of the measurement. Quality assessment questions are listed in Table 2.
Each question was scored on a three-level basis: 2 = yes, 1 = limited detail, 0 = no, for an overall score of up to 38 possible points for each article. Bishop et al. [37] rating score was used to classify studies by their quality: high quality was associated to articles with a score higher than 80% (31/38), medium quality articles had a score between 51 and 79% (19–30/38) while low quality was associated with a score lower than 50% (18/38).
Data extraction
A standardised extraction form was used by one reviewer to identify and report relevant information from each study. The extraction form points are listed in Table 3.
The study details extracted could be divided into three categories: reliability of the measurement (points 1 to 3), suitability of the approach to be used in a clinical setting (points 4 to 9) and the clinical significance of the results reported (points 10 to 12). Some of the data extracted were related to more than one category; this was the case for points 4,5,6,8 which related to both the repeatability and suitability of the measurement, points 9 and 10 related to both the suitability of the measurement and the clinical significance of the reported results. Since none of the studies assessed in this review reported on the suitability of the measurement to be used in a clinical setting in terms of time needed to attach the markers and the ease of use of their data processing approach by clinicians, the number of markers used, segments defined, and degrees of freedom studied were reported instead to determine this suitability. Studies using the same protocol as previous ones were grouped into a separate list.
Results
Data acquisition and research strategy
The selection process identified a total of 10,465 records, resulting in 8937 after duplicate removal. After screening titles and abstracts, 8827 studies were excluded as they were deemed irrelevant for the purposes of this review. Inclusion criteria were applied to 110 full-text articles. Seventy-four papers were found to match the inclusion criteria established while 36 studies were excluded as these did not report information on their marker setup, did not use an optoelectronic technique or defined the spine as one moving segment. The process for study selection is shown in the PRISMA flow chart (Fig. 2). Of the 74 articles found, 44 articles proposed new protocols for multi-segments spine motion analysis.
Quality assessment
The 74 articles were assessed using the quality assessment questionnaire. Of those, 12 studies [12,13,14, 38,39,40,41,42,43,44,45,46] were found to be of high quality. Sixty studies [23, 26, 30, 47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95] were deemed as medium quality studies and 2 studies [96, 97] had a low-quality score below 50% (Fig. 3).
The number of articles answering yes to the quality assessment questions could be seen in Fig. 4.
Quality Assessment Questionnaire. The number of articles answering yes to each of the questions. Blue bar plots indicate overall quality questions, orange bar plots indicate reliability related questions, green bar plots indicate suitability related questions and yellow bar plots indicate clinical relevance related questions
The details and study characteristics obtained from the extraction form of the 74 articles reviewed could be found in Tables 4 and 5.
Reliability of the motion capture setup
Repeatability
Thirty-one studies asked their participants to repeat the motion tasks three times [12,13,14, 40,41,42,43,44, 47, 54, 55, 58,59,60,61, 65,66,67,68, 70, 78, 82, 83, 94], 12 studies did 5 repetitions of the motion tasks [26, 39, 46, 53, 69, 75, 76, 80, 88, 89, 95, 97], 7 studies had 10 repetitions [23, 30, 52, 62, 72, 85], 1 study only asked participants to complete the motion task once [86] while 12 studies did not mention the number of task repetitions made [38, 45, 48, 49, 57, 64, 73, 74, 91,92,93, 96]. Ten studies reported their intra-subject repeatability measures [23, 38, 46, 69, 70, 72, 85, 89, 95, 105], 3 studies measured their inter-rater reliability [38, 82, 95] while 5 studies assessed the repeatability of the findings when measured across different days [26, 30, 38, 82, 91].
Accuracy
Fifteen studies evaluated the accuracy of their marker setups [26, 38, 50, 53, 54, 56, 59, 63, 68, 69, 73, 75, 82, 84, 87, 93]. The soft tissue artefact associated with the motion was quantified using imaging techniques in 3 studies [53, 63, 82]. Two studies used electromagnetic sensors along with passive markers to cross-check the values generated by both systems [84, 93]. Two studies compared the kinematic variables collected from participants to those collected from markers placed on custom-built mechanical models of the spine [26, 53]. One study used the medimouse apparatus to compute spinal angles and cross-check with the values generated by the motion analysis [50]. Only 1 study inserted wires into the vertebral body to quantify soft tissue artefact (STA) [68].
Suitability of the approach
Marker setup
Most studies used clusters of single markers for their setups, only 7 studies used marker triads to define spine segments [38, 53, 55, 68, 72, 83, 88]. The spinous processes of C7, T3, T6, T12, L1, L3 and L5 were the most widely used. All studies reported marker positioning by palpation of the anatomical landmark surface. Two studies positioned markers following the curvature of the spine, at the points of most thoracic kyphosis and lumbar lordosis [23, 64]. Information on the time needed to position the markers was not reported by any of the studies.
Segment definition
The majority of studies [13, 14, 40, 41, 45, 48, 57, 58, 62, 63, 65, 66, 77, 81, 82, 87, 89, 90, 94, 96] used 4 markers to define a spinal segment using 2 markers on the spinous processes and 2 lateral markers midway between these to form a diamond shaped segment. Eleven studies [38, 39, 43, 47, 50, 51, 54, 55, 64, 67, 72, 75, 80, 93, 97] used only 2 markers on the spinal processes to form a segment line. While 12 other studies [12, 23, 26, 42, 44, 49, 53, 56, 70, 71, 79, 83, 88, 92] used 3 markers to define their segments by using 1 marker on the spine and 2 lateral markers to form a triangular shape. It is worth noting that 12 studies used anterior markers on the sternum to define their spinal segments [23, 30, 46, 52, 56, 71, 73, 76, 85,86,87, 91].
The most common segment definition used was dividing the kinematic model of the spine into 2 distinct segments, either the thoracic and lumbar spines [30, 45, 48, 49, 56, 61,62,63, 71, 74, 78, 83,84,85,86] or the upper lumbar and lower lumbar spines [69, 82].
Another common segment definition was dividing the back into 3 parts and these were: Upper thoracic, Lower Thoracic and Lumbar [26, 40, 52, 57, 64, 77, 79, 80, 87, 88, 94, 95]. Some studies further divided the lumbar spine into upper and lower lumbar, to have a total of 4 segments [12,13,14, 41,42,43,44, 59, 60, 81, 90, 94, 97]. Only 5 papers further defined the cervical spine in addition to the thoracic and lumbar segments and analysed it in their models [46, 73, 76, 91, 92]. Three studies considered each lumbar vertebra as a single segment [54, 67, 68].
Data processing
The kinematic data collected from markers was low pass filtered using Butterworth Filters with a cut-off frequency ranging between 2 and 10 Hz depending on the motion capture setup. Most studies defined the pelvis as the local coordinate system for their data analysis [12,13,14, 23, 26, 30, 38, 41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59, 61,62,63,64,65,66,67, 69,70,71,72,73,74,75, 77,78,79,80,81,82,83, 89, 92,93,94, 96, 97]. The Grood and Suntay convention was mentioned in 14 studies to calculate intersegmental angles to obtain the flexion/extension, lateral bending, and axial rotations of the defined segments in all 3 anatomical planes [13, 14, 22, 23, 26, 51, 59, 60, 69, 92, 94, 95, 106, 107].
Some studies reported subtracting the static standing trial of participants from the dynamic trials to normalize the angle of motion [13, 14, 41, 60, 76]. None of the studies included in this review commented on the ease of use of their data processing procedure for use in clinical practice.
Participant cohorts
Thirty-five studies had only healthy participants in their cohorts [23, 26, 30, 47, 48, 50, 51, 56,57,58, 64,65,66,67,68,69,70,71,72, 74, 75, 77, 78, 82, 84, 85, 87, 89, 91,92,93,94,95,96,97]. Twenty-seven studies compared pathological participants to healthy participants [12,13,14, 38,39,40,41,42,43,44,45,46, 52, 55, 59,60,61, 76, 79,80,81, 83, 86, 88, 90] while only 3 studies assessed the motion of only pathological subjects [49, 63, 73]. Details of participant cohorts can be found in Table 6.
Tasks conducted
The majority of studies [12,13,14, 23, 26, 41,42,43,44,45,46,47,48,49, 51, 53,54,55, 57, 59,60,61, 63, 64, 67,68,69, 73, 75,76,77, 86, 89, 91,92,93,94,95] looked at the motion of the spine segments during activities of daily living (ADL), as these were considered routine and repetitive motions where the spine plays a key role to assure equilibrium and are affected in spine pathology cases. Some of these studies [12, 26, 41, 45,46,47,48,49, 53, 54, 59,60,61, 63, 64, 67,68,69, 73, 76, 92, 94, 95] looked at the active role the spine segments play during gait to maintain equilibrium and the compensation mechanism used by patients to achieve it.
When it comes to the studies that recruited patients undergoing spine surgery [45, 49, 52, 53, 61, 83], ADL tasks were used to assess improvement or deterioration of neurological symptoms, changes in motion patterns and the compensation mechanisms involved in the motion.
Twenty-two studies [39, 40, 50, 51, 58, 61, 65, 66, 68, 72, 75, 78,79,80,81,82,83,84, 86, 89, 96, 97] included spine range of motion tasks such as forward flexion, lateral bending, or spine rotation. These tasks were implemented to report normal spine segment kinematics, investigate the role of each spine segment in spine motion and assess the reliability of motion capture setups. Eight studies [30, 52, 62, 74, 76, 85, 87, 91] looked at the motion of the spine during running trials while 2 studies [56, 71] assessed spine motion during the squat exercise, 2 studies [81, 90] assessed spine motion while their participants performed dancing tasks while 1 study assessed the motion of the spine during rowing [88].
Patient considerations
Studies involving patients and healthy subjects [12,13,14, 38,39,40,41,42,43,44,45,46, 52, 55, 59,60,61, 76, 79,80,81, 83, 86] had the same tasks for both cohorts. Participants were asked to perform their tasks at their self-selected speed. One study involving patients asked their participants to perform a lifting task only in their most comfortable approach [55].
Main measurements
Eighteen studies calculated the angles between the spine segments defined [23, 26, 42, 47, 53, 56, 61, 64, 65, 69, 70, 72, 74, 84, 90, 91, 93,94,95, 97] while 33 studies [12,13,14, 30, 39,40,41, 43, 44, 46, 48,49,50,51,52, 55, 57,58,59,60, 62, 66,67,68, 75, 77, 78, 82, 83, 85, 86, 88, 92, 96] calculated the range of motion of the segments during the tasks conducted.
The ROM of segments during walking tasks ranged from 2.3° to 7.9° in the sagittal plane, 1.8° to 10.8° in the frontal plan while most of the motion was recorded in the transverse plane ranging from 2.6° to 13.5°. Detailed ROMs of the spine segments defined in the studies extracted can be found in Table 7.
Four studies [63, 71, 73, 76] reported the angle of inclination between the segments and as such calculated the angles of lumbar lordosis or thoracic kyphosis.
Of the 24 studies that conducted walking trials [12, 26, 41, 45,46,47,48,49, 53, 54, 59,60,61, 63, 64, 67,68,69, 73, 76, 91, 92, 94, 95], only 5 assessed the kinematics of the lower limbs and reported the gait parameters generated.
Clinical significance
Pathologies assessed
The majority of studies involving pathology assessed subjects with LBP or chronic low back pain (CLPB) [12,13,14, 40,41,42,43,44, 59, 60, 62, 76, 79, 81, 88, 90]. Eight studies had teenagers with adolescent idiopathic scoliosis (AIS) [46, 49, 52, 61, 63, 73, 80, 83]. Two studies assessed ASD [38, 53]. One study assessed ankylosing spondylitis [55], another focused only on lumbar disc herniation subjects [54], 1 study assessed lumbar spinal stenosis patients [45] and one study assessed patients with axial spondyloarthropathy (axSpa) with two patient cohorts in the active inflammation or the bone formation phases [39]. Only one study assessed the changes in spine motion due to obesity [86].
Six studies assessed patients undergoing spine surgery, 5 of them had patients who underwent posterior spinal fusion surgery [49, 52, 53, 61, 83] while 1 study had patients undergoing two different decompression surgery approaches [45].
Four studies assessed patient motion before and after surgery. One study measured patients before and 1 month after [45], another measured patients before, 3 months and 12 months after surgery [49], Patel et al. [61] measured patients before and 12 months following surgery while Konz et al. [53] analysed their subject before and 6 months after surgery.
Clinical findings
The studies including patients assessed the kinematics of the multi-segmental spine to help clinical decisions, provide more information on motion compensation, evaluate treatment, and monitor pathology outcome. Kuwahara et al. [45] used the multi-segmental motion approach to compare two decompression surgery techniques and measure the improvement of neurological symptoms following surgery of the two-patient cohort. Hemming et al. [43] found evidence to support subgrouping LBP patients to better refine intervention approaches. Christe et al. [14] suggested that CLBP patient rehabilitation could benefit from targeting specific motion deficits in functional activities.
Of the 29 studies assessing patients, 3 studies [40, 41, 61] reported motion asymmetry at the levels of the lumbar and thoracic spine between the patient and control cohorts, Christe et al. [41] reported a 20% increase in transverse plane asymmetry in CLBP patients (Table 7) while Patel et al. [61] reported asymmetric axial plane motion in LBP patients. 4 studies assessed spine rotation abilities depending on the pathology, 3 of these [12, 41, 42] reported up to 15% decrease in segment rotation either after a surgical intervention or due to LBP (Table 7). Only 1 study [79] reported an increase in lumbar and thoracic rotations in patients with LBP. The motion profile of axial spondylopathy patients was seen to be similar to the maladaptive motion profiles of patients with CLBP with a significant decrease in motion velocity when compared to controls [39].
When it comes to the motion of the lumbar spine, 3 studies reported a decrease in lumbar spine flexion in LBP patients [13, 41, 44] (Table 7), while 1 study [42] reported a decrease in lower lumbar flexion but an increase in upper lumbar flexion. One study [60] found an increase in the upper lumbar and lower lumbar ROM during walking, sit-to-stand and running tasks in patients with LBP (Table 7).
Five studies reported the motion coordination present between the spinal segments [55, 59, 62, 80, 88]. Of these, two studies [59, 80] found a lack of coordination between the lumbar and thoracic segments in LBP and AIS patients. One study [62] found that the pattern of coordination between segments is different for LBP patients when compared to the control and 1 study [55] found evidence of coordination between the upper lumbar, thoracic and pelvis to stabilize the trunk in ankylosing spondylitis patients. One study assessing the motion of rowers with CLBP [88] found a lack of coordination between the spinal segments when the intensity of the motion is increased while also finding that the lower spine segments could not work as supports for the upper segments.
Five studies [23, 38, 46, 63, 73] reported the changes in spine curvature during dynamic trials when compared to static posture. These were able to show that curvature angles of the spine could be measured with high accuracy and that regional differences exist depending on the pathology. One study [76] reported a decrease in the lumbar lordosis angle during walking and running in patients with non-specific LBP.Two studies [49, 83] reported the motion of the spine following fusion surgery, one with AIS patients and the other with ASD patients, both did not report any hypermobility in the unfused spinal segment. Only one study [81] found no significant spine kinematic differences between the LBP group and the control group.
Discussion
Motion abnormalities of the spine impact the onset and recurrence of spinal disorders [11, 12], therefore analysing the kinematics of the thoracolumbar spine gives an insight into the causes of these disorders and aids in the choice of treatment [13, 14]. Stereophotogrammetric motion analysis could objectively quantify this motion [22, 23], however numerous methods and protocols are found in the literature. The current review aims to evaluate these studies and assess their reliability, suitability in a clinical setting and clinical significance. Seventy-four articles were identified focusing on the multi-segmental motion of the thoracolumbar spine of which 44 articles proposed a different protocol to quantify this motion. These protocols differed in the number of markers used, segments defined, participant cohorts recruited, disorders analysed, kinematic variables assessed, and outcome measurements reported highlighting the need for a set of standard principles to provide reliable and reproducible kinematic information on various motions, spine segments and spine disorders.
Reliability of the motion capture setup
The reliability of the identified studies was first evaluated. It was defined as the repeatability and accuracy of the measurement approach in addition to the analysis of sources of error. Most studies did not report on these three reliability aspects scoring 32%, 18% and 18% respectively in the quality assessment questionnaire. To quantify the repeatability of the measurement, we first looked at task repetitions; most studies asked their participants to repeat the motion at least three times [12,13,14, 23, 26, 30, 39,40,41,42,43,44, 46, 47, 52,53,54,55, 58,59,60,61,62, 65,66,67,68,69,70, 72, 75, 76, 78, 80, 82, 83, 85, 89, 94, 95, 97] and ultimately based their measurements on the average of trials, however, the repetitions of tasks were unrelated to the number of participants in the cohorts. Some of the studies succeeded in analysing the repeatability of the outcome measurement either by studying the intra-subject variability [23, 38, 46, 69, 70, 72, 85, 89, 95, 105], the inter-rater reliability [38, 82, 95] or the repeatability of the findings when measured across different days [26, 30, 38, 82, 91]. When it comes to the accuracy of the optoelectronic protocol, 11 studies [26, 46, 53, 54, 63, 67, 68, 71, 73, 82, 84] compared their results to more conventional imaging techniques to show the accuracy of the marker setup and their reported outcomes; however, the remaining studies did not report on these differences as they were investigating the changes in spine motion between cohorts and were not reporting the absolute angle of motion of spinal segments [12,13,14, 38, 40,41,42,43,44,45,46, 55, 59, 61, 79,80,81, 83]. Deane et al. [95] was the only study to quantify the standard error associated with spine motion ranging between 0.8° and 5.5° for gait and between 1° and 12.6° for sit-to-stand motion compared to imaging techniques that account for a < 1° of error during static measurements [19]. Only 9 studies [38, 40, 50, 53, 66, 73, 84, 87, 94] reported the marker placement error associated with the setup, this is especially important as the spine region is greatly affected by STA [72] and hence would be expected to be more thoroughly reported. None of the studies identified in this review however was found to report on all three reliability aspects assessed in the quality questionnaire. These shortcomings affect the reliability of the protocols suggested and make implementing a standard protocol in a clinical setting even more difficult.
Suitability of the approach
When assessing the suitability of the protocols suggested for a clinical setting, we looked at marker configurations, segment definitions, participant cohorts, tasks conducted outcome measures and the ease of use of the methodology in a clinical setting. Major differences in marker setups were seen across studies, with different numbers of markers on the thoracolumbar spine and their location on the anatomical landmarks; the most common anatomical landmarks to attach the markers on were C7/T1, T6/T7, T12/L1, L3, L5. Only 11 studies [23, 30, 46, 52, 56, 71, 73, 76, 85,86,87] reported positioning of markers anteriorly to the spine on the sternum to decrease the effect of STA on the measurement while the majority of the studies positioned markers laterally to the spine [13, 14, 40, 41, 45, 48, 57, 58, 62, 63, 65, 66, 77, 81, 82, 88, 89, 94, 96]. Some of these marker setups were seen to be very complex for a clinical setting and are more suited for research purposes as they require more time to position due to the high number of marker [38, 46, 50, 51, 55, 56, 67, 68, 73, 79, 80, 88, 90, 91], other studies [12,13,14, 23, 39, 41,42,43,44, 57,58,59, 64,65,66, 75, 81, 92, 94, 97] were seen to be successful in limiting the number of markers on the spine or by using 3D clusters. This limitation was mentioned by Glover et al., [87], who saw that a higher number of markers on the spine decreases marker tracking error but the implementation of the protocol and processing the data would take a significantly longer time. A poor consistency was found in terms of thoracolumbar segment definition. These changed depending on the study cohorts and tasks of interest. The majority of studies tried to define at least the thoracic and lumbar spines [30, 45, 48, 49, 56, 61,62,63, 71, 74, 78, 83,84,85,86], the lumbar spine was further divided into upper and lower segments [12,13,14, 41,42,43,44, 59, 60, 81, 90, 94, 97] especially when investigating patients with LBP due to the changes in motion seen at each level [12, 42, 43, 59, 60, 90]. The thoracic spine was also divided into upper and lower segments to have a better understanding of the less studied kinematics of the thoracic spine and help in the investigation of kyphotic and scoliotic spines [13, 14, 23, 41, 50, 56, 81, 90]. When it comes to participant considerations, most of the studies tried to match the age of participants with only 9 studies including participants with an age range difference exceeding 10 years [38, 39, 43, 45, 47, 55, 75, 79, 94]. More than half of the studies investigated ADLs such as lifting, sit-to-stand, stair climbing and walking. These tasks had been seen to present a challenge to spine pathology patients and could highlight the differences in segment ROM and coordination when compared to controls [13, 14, 23, 31, 41]. The angle between the defined segment was the main outcome reported by studies independent of the tasks conducted, marker setup used, or segments defined. Despite ROM being a straightforward indication of motion ability and is easily estimated even in a clinical setting, it can limit our understanding of motion contribution, compensation mechanisms and coordination between the spine segments [31]. The coordination between the segments wasn’t as widely reported although evidence has been found to show changes in coordination due to age and spine pathology [55, 59, 62, 80, 88]. None of the studies in this review reported on the time needed for each measurement or the ease of use of their processing approach in a clinical setting. Hence after assessing the suitability of the studies found, ADLs remain the most useful tasks to understand spine motion and its pathologies [13, 14, 23, 31, 41] while more investigations are needed to agree on marker setups and segments definitions to be used in a clinical setting in addition to what to report when it comes to outcome measurements.
Clinical significance
When it comes to the clinical significance of the studies evaluated, this was defined as the relevancy of the study and its outcome measurements to a certain spine pathology. Different kinematic findings were reported by the studies depending on the spine pathology, the multi-segmental approach and the marker setup used. When considered as one moving segment, the lumbar spine flexion was seen to decrease overall in subjects with LBP [13, 41, 44]; however, when further dividing the lumbar spine into upper and lower segments, motion contribution by the UL was seen to be greater than the LL segment [12, 42]. As such, segment definition plays a key role in understanding the effects of pathology on spine motion; it is advised to divide the spine into more than 2 segments to be able to describe the motion of the whole spine and understand the contribution of each segment [46]. Besides, grouping patients into subcategories depending on their motion impairments [43] or surgical treatments [45] could reveal the similarities in the kinematic findings against healthy controls [31]. Considerations for the changes in spine motion due to age were limited. Only 2 studies reported the differences in spine ROM between older and younger adults [50, 51] while the majority of the studies reported the motion of the spine in healthy younger adults under the age of 35 [23, 47, 48, 53, 56,57,58, 65,66,67, 71, 72, 77, 78, 82, 89, 93, 95,96,97]. Significant age-related lumbar segment reductions in motions have however been reported in the literature [32], it is therefore advised to investigate the spine motion of both older and younger adults and spine pathology subjects to define the motions of each segment of the spine and the coordination between the segments. When looking at the differences between patients and controls, distinct motion perturbations were found in the axial and sagittal plane during spine motion in addition to transverse plane asymmetry in subjects with spine pathologies [12,13,14, 39,40,41,42, 44, 79, 80, 88]. Hence it is advised to investigate the motion of the defined segments in the three dimensions of motion in addition to studying the coordination between spine segments and to the pelvis to ultimately define distinct motion characteristics for LBP, AIS, ASD or spine surgery patients. The use of a multi-segmental spine motion protocol was seen to be successful in a clinical setting to accurately assess spine curvature [23, 38, 46, 63, 73] and the effect of surgical treatment on the patient motion [45, 49, 83]. Evidence has been found in this review to support the use of a multi-segmental approach for spine motion analysis to help clinicians in the diagnosis and treatment of spine disorders.
Limitations
The present study has a few limitations. Only three research databases were queried for articles published in a peer-reviewed journal and only in English. Hence, a publication or language bias might have occurred. The quality assessment questionnaire developed was not assessed for objective reliability and validity although it was constructed using prior assessments found in the literature [31, 37]. A reliability assessment of the extracted data and the quality assessment questionnaire was not carried out as they were completed by only one reviewer. The review only included studies using passive markers and an optoelectronic system. Studies assessing multi-segmental spine motion using inertial markers or wearable technology were not assessed due to the high signal to nose ratio linked to these sensors especially when attached to a vertebral landmark [65]. Additionally, studies assessing only the motion of the cervical spine were not included as only the motion of the thoracolumbar spine was found to be relevant to the onset of LBP and ASD [1, 35].
Conclusions
The current review showed a shortage in standard protocols to assess spine motion using optoelectronic techniques to identify and support clinical investigations. The findings mentioned in the review could be used when trying to choose the most fitting protocol to assess the motion of the thoracic and lumbar spines. Based on the studies assessed in the review, separating each of the thoracic and lumbar segments into upper and lower parts is essential to accurately describe the motion of the spine. Markers attached to C7/T1, T6/T7, T12/L1, L3, L5 in addition to anterior markers on the sternum are needed to describe this motion. This limited number of markers would allow for easier application in a clinical setting. In terms of instrumentation, a motion analysis system made up of at least 6 cameras is needed. However, no study in this review mentioned the cost incurred by such an analysis and a cost effectiveness study would need to be completed to assess the feasibility of using spine motion analysis in a clinical setting. Additionally standardizing the marker setups, segment definitions and tasks conducted as part of a multicentric study could prove to help identify more accurate clinical applications for spine motion analysis.
Availability of data and materials
There is no specific data to share, however, datasets supporting the conclusions of this review article could all be found in the reference list included within the article.
Abbreviations
- LBP:
-
Low Back Pain
- ASD:
-
Adult Spine Deformity
- ROM:
-
Range of Motion
- CT:
-
Computer tomography
- MRI:
-
Magnetic Resonance Imaging
- LPSI:
-
Left Posterior Superior Iliac Spine
- RPSI:
-
Right Posterior Superior Iliac Spine
- RBAK:
-
Right Back
- UT:
-
Upper Thoracic
- LT:
-
Lower Thoracic
- UL:
-
Upper Lumbar
- LL:
-
Lower Lumbar
- MUT:
-
Middle Upper Thoracic
- MLT:
-
Middle Lower Thoracic
- STA:
-
Soft Tissue Artefact
- M:
-
Male
- F:
-
Female
- AEP:
-
Active extension pattern
- FP:
-
Flexion pattern
- AK:
-
Ankylosed axial spondyloarthropathy
- Inf:
-
Inflamed axial spondyloarthropathy
- ADL:
-
Activities of Daily Living
- CLPB:
-
Chronic Low Back Pain
- AIS:
-
Adolescent Idiopathic Scoliosis
References
Cerpa M, Sardar Z, Lenke L. Revision surgery in proximal junctional kyphosis. Eur Spine J. 2020;29(s1):78–85. Available from: https://doi.org/10.1007/s00586-020-06320-y.
Dagdia L, Kokabu T, Ito M. Classification of adult spinal deformity: Review of current concepts and future directions. Spine Surg Relat Res. 2019;3(1):17–26.
Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: Estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):968–74.
Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med. 2020;8(6):299–299.
Schwab F, Dubey A, Gamez L, El Fegoun AB, Hwang K, Pagala M, et al. Adult scoliosis: Prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30(9):1082–5.
Barreto MVA, De Rezende PR, Barsotti CEG, Dos Santos FPE, De Oliveira CEAS, Nogueira MP. Incidence of spinal deformity in adults and its distribution according srs-schwab classification. Coluna/ Columna. 2015;14(2):93–6.
Daniell JR, Osti OL. Failed back surgery syndrome: A review article. Asian Spine J. 2018;12(2):372–9.
Haddas R, Ju KL, Belanger T, Lieberman IH. The use of gait analysis in the assessment of patients afflicted with spinal disorders. Eur Spine J. 2018;27(8):1712–23.
Diebo BG, Shah NV, Pivec R, Naziri Q, Patel A, Post NH, et al. From static spinal alignment to dynamic body balance: Utilizing motion analysis in spinal deformity surgery. JBJS Rev. 2018;6(7):1–12.
Diebo BG, Shah NV, Stroud SG, Paulino CB, Schwab FJ, Lafage V. Realignment surgery in adult spinal deformity. Orthopade. 2018;(February):301–9. Available from:https://doi.org/10.1007/s00132-018-3536-5
Mitchell K, Porter M, Anderson L, Phillips C, Arceo G, Montz B, et al. Differences in lumbar spine and lower extremity kinematics in people with and without low back pain during a step-up task: A cross-sectional study. BMC Musculoskelet Disord. 2017;18(1):1–9.
Gombatto SP, Brock T, DeLork A, Jones G, Madden E, Rinere C. Lumbar spine kinematics during walking in people with and people without low back pain. Gait Posture. 2015;42(4):539–44. Available from: https://doi.org/10.1016/j.gaitpost.2015.08.010.
Christe G, Redhead L, Legrand T, Jolles BM, Favre J. Multi-segment analysis of spinal kinematics during sit-to-stand in patients with chronic low back pain. J Biomech. 2016;49(10):2060–7. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84973923065&doi=10.1016%2Fj.jbiomech.2016.05.015&partnerID=40&md5=43a961d1da7ba3dae555b042f67378a7.
Christe G, Rochat V, Jolles BM, Favre J. Lumbar and thoracic kinematics during step-up: Comparison of three-dimensional angles between patients with chronic low back pain and asymptomatic individuals. J Orthop Res. 2020;38(6):1248–56. Available from: https://doi.org/10.1002/jor.24575.
Miura K, Kadone H, Koda M, Abe T, Funayama T, Noguchi H, et al. Thoracic kyphosis and pelvic anteversion in patients with adult spinal deformity increase while walking: analyses of dynamic alignment change using a three-dimensional gait motion analysis system. Eur Spine J. 2020;29(4):840–8. Available from: https://doi.org/10.1007/s00586-020-06312-y.
Hidalgo B, Gilliaux M, Poncin W, Detrembleur C. Reliability and validity of a kinematic spine model during active trunk movement in healthy subjects and patients with chronic non-specific low back pain. J Rehabil Med. 2012;44(9):756–63. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84866039756&doi=10.2340%2F16501977-1015&partnerID=40&md5=904c92e973a8858671864da76b6d6f77.
Pumberger M, Schmidt H, Putzier M. Spinal Deformity Surgery: A Critical review of Alignment and Balance. Asian Spine J. 2018;12(4):775–83.
Jarvik JG, Deyo RA. Diagnostic Evaluation of Low Back Pain with Emphasis on Imaging. Ann Intern Med. 2002;137(November):586–97.
Mellor FE, Thomas P, Breen A. Moving back: The radiation dose received from lumbar spine quantitative fluoroscopy compared to lumbar spine radiographs with suggestions for dose reduction. Radiography. 2014;20(3):251–7. Available from: https://doi.org/10.1016/j.radi.2014.03.010.
Hadelsberg UP, Harel R. Hazards of Ionizing Radiation and its Impact on Spine Surgery. World Neurosurg. 2016;92:353–9. Available from: http://www.sciencedirect.com/science/article/pii/S1878875016302996.
Lee S, Wong KWN, Chan M, Yeung H, Chiu JLF, Leong JCY. Development and validation of a new technique for assessing lumbar spine motion. Spine (Phila Pa 1976). 2002;27(8):E215-20.
Leardini A, Biagi F, Belvedere C, Benedetti MG. Quantitative comparison of current models for trunk motion in human movement analysis. Clin Biomech. 2009;24(7):542–50. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-67649452490&doi=10.1016%2Fj.clinbiomech.2009.05.005&partnerID=40&md5=f44e4f0792622a9e5a2587c66ecbc213.
Leardini A, Biagi F, Merlo A, Belvedere C, Grazia M, Benedetti MG. Multi-segment trunk kinematics during locomotion and elementary exercises. Clin Biomech. 2011;26(6):562–71. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-79959354374&doi=10.1016%2Fj.clinbiomech.2011.01.015&partnerID=40&md5=398a78805cf2aae6d4319d6d065fe745.
Negrini S, Piovanelli B, Amici C, Cappellini V. Trunk motion analysis: a systematic review from a clinical and metholodgical perspective. Eur J Phys Rehabil Med. 2016;52(4):3–5.
Needham R, Stebbins J, Chockalingam N. Three-dimensional kinematics of the lumbar spine during gait using marker-based systems: A systematic review. J Med Eng Technol. 2016;40(4):172–85.
Needham R, Naemi R, Healy A, Chockalingam N. Multi-segment kinematic model to assess three-dimensional movement of the spine and back during gait. Prosthet Orthot Int. 2016;40(5):624-35. https://doi.org/10.1177/0309364615579319.
Baker R, Esquenazi A, Benedetti MG, Desloovere K. Gait analysis: clinical facts. Eur J Phys Rehabil Med. 2016;52(4):560–74. Available from: http://www.ncbi.nlm.nih.gov/pubmed/27618499).
Ferrari A, Benedetti MG, Pavan E, Frigo C, Bettinelli D, Rabuffetti M, et al. Quantitative comparison of five current protocols in gait analysis. Gait Posture. 2008;28(2):207–16.
Wu G, Van Der Helm FCT, Veeger HEJD, Makhsous M, Van Roy P, Anglin C, et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion — Part II : shoulder, elbow, wrist and hand. J Biomech. 2005;38:981–92.
Mason DL, Preece SJ, Bramah CA, Herrington LC. Reproducibility of kinematic measures of the thoracic spine, lumbar spine and pelvis during fast running. Gait Posture. 2014;43:96–100. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84954374275&doi=10.1016%2Fj.gaitpost.2013.11.007&partnerID=40&md5=5a1f36471867d26c30cf8f9570a28091.
Papi E, Bull AMJ, McGregor AH. Is there evidence to use kinematic/kinetic measures clinically in low back pain patients? A systematic review. Clin Biomech. 2018;55(April):53–64. Available from: https://doi.org/10.1016/j.clinbiomech.2018.04.006.
Intolo P, Milosavljevic S, Baxter DG, Carman AB, Pal P, Munn J. The effect of age on lumbar range of motion: A systematic review. Man Ther. 2009;14(6):596–604. Available from: https://doi.org/10.1016/j.math.2009.08.006.
Pourahmadi MR, EbrahimiTakamjani I, Jaberzadeh S, Sarrafzadeh J, Sanjari MA, Bagheri R, et al. Kinematics of the Spine During Sit-to-Stand Movement Using Motion Analysis Systems: A Systematic Review of Literature. J Sport Rehabil. 2019;28(1):77–93. Available from: http://www.epistemonikos.org/documents/7d70c2d568bef2661603e34af15d483cfb31d636.
Maaswinkel E, Griffioen M, Perez RSGM, van Dieën JH. Methods for assessment of trunk stabilization, a systematic review. J Electromyogr Kinesiol. 2016;26:18–35. Available from: http://www.sciencedirect.com/science/article/pii/S105064111600002X.
Jin H, Kim HJ, Yang JH, Chang D, Suk S, Suh SW, et al. Adult Spinal Deformity : Current Concepts and Decision-Making Strategies for Management. Asian Spine J. 2020;14(6):886–97.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLOS Med. 2021;18(3):e1003583. Available from: https://doi.org/10.1371/journal.pmed.1003583.
Bishop C, Paul G, Thewlis D. Recommendations for the reporting of foot and ankle models. J Biomech. 2012;45(13):2185–94. Available from: https://doi.org/10.1016/j.jbiomech.2012.06.019.
Severijns P, Overbergh T, Thauvoye A, Baudewijns J, Monari D, Moke L, et al. A subject-specific method to measure dynamic spinal alignment in adult spinal deformity. Spine J. 2020;20(6):934–46.
Seerden SFL, Dankaerts W, Swinnen TW, Westhovens R, De Vlam K, Vanwanseele B. Differences in multi-segmental spine kinematics between patients with different stages of axial spondyloarthritis and healthy controls. Musculoskelet Sci Pract. 2021;53(April 2020):102368. Available from: https://doi.org/10.1016/j.msksp.2021.102368.
Al-eisa E, Egan D, Deluzio K, Wassersug R. Effects of Pelvic Asymmetry and Low Back Pain on Trunk Kinematics During Sitting : A Comparison With Standing. Spine (Phila Pa 1976). 2006;31(5):135–43.
Christe G, Kade F, Jolles BM, Favre J. Chronic low back pain patients walk with locally altered spinal kinematics. J Biomech. 2017;60:211–8. Available from: https://doi.org/10.1016/j.jbiomech.2017.06.042.
Gombatto SP, Arpa ND, Landerholm S, Mateo C, Connor RO, Tokunaga J, et al. Differences in kinematics of the lumbar spine and lower extremities between people with and without low back pain during the down phase of a pick up task, an observational study. Musculoskelet Sci Pract. 2017;28:25–31. Available from: https://doi.org/10.1016/j.msksp.2016.12.017.
Hemming R. Non-specific chronic low back pain : differences in spinal kinematics in subgroups during functional tasks. Eur Spine J. 2018;27(1):163–70.
Hernandez A, Gross K, Gombatto S. Clinical Biomechanics Differences in lumbar spine and lower extremity kinematics during a step down functional task in people with and people without low back pain. Clin Biomech. 2017;47(June 2016):46–52. Available from: https://doi.org/10.1016/j.clinbiomech.2017.05.012.
Kuwahara W, Deie M, Fujita N, Tanaka N, Nakanishi K, Sunagawa T, et al. Characteristics of thoracic and lumbar movements during gait in lumbar spinal stenosis patients before and after decompression surgery. Clin Biomech. 2016;40:45–51. Available from: https://doi.org/10.1016/j.clinbiomech.2016.10.016.
Schmid S, Studer D, Hasler CC, Romkes J, Taylor WR, Lorenzetti S, et al. Quantifying spinal gait kinematics using an enhanced optical motion capture approach in adolescent idiopathic scoliosis. Gait Posture. 2016;44:231–7. Available from: https://doi.org/10.1016/j.gaitpost.2015.12.036.
Frigo C, Carabalon R, Dalla Mura M, Negrini, Carabalona R, Dalla Mura M, et al. The upper body segmental movements during walking by young females. Clin Biomech (Bristol, Avon). 2003;18(5):419–25.
Gilleard WL. Trunk motion and gait characteristics of pregnant women when walking: Report of a longitudinal study with a control group. BMC Pregnancy Childbirth. 2013;13:71.
Holewijn RM, Kingma I, de Kleuver M, Keijsers NLW. Posterior spinal surgery for adolescent idiopathic scoliosis does not induce compensatory increases in distal adjacent segment motion: a prospective gait analysis study. Spine J. 2018;0031. Available from: https://doi.org/10.1016/j.spinee.2018.05.010
Ignasiak D, Rüeger A, Ferguson SJ. Multi-segmental thoracic spine kinematics measured dynamically in the young and elderly during flexion. Hum Mov Sci. 2017;54(September 2016):230–9. Available from: https://doi.org/10.1016/j.humov.2017.05.011.
Ignasiak D, Rüeger A, Sperr R, Ferguson SJ. Thoracolumbar spine loading associated with kinematics of the young and the elderly during activities of daily living. J Biomech. 2018;70:175–84 Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85039055346&doi=10.1016%2Fj.jbiomech.2017.11.033&partnerID=40&md5=e79ac4e011509b39cb2d28c141aeb266.
Kakar RS, Li Y, Brown CN, Oswald TS, Simpson KJ. Spine and Lower Extremity Kinematics Exhibited During Running by Adolescent Idiopathic Scoliosis Patients With Spinal Fusion. Spine Deform. 2019;7(2):254–61. Available from: https://doi.org/10.1016/j.jspd.2018.08.015.
Konz RJ, Fatone S, Stine RL, Ganju A, Gard SA, Ondra SL. A kinematic model to assess spinal motion during walking. Spine Spine (Phila Pa 1976). 2006;31(24):E898-906.
Kuai S, Guan X, Zhou W, Zhang R, Ji R, Liao Z, et al. Continuous lumbar spine rhythms during level walking, stair climbing and trunk flexion in people with and without lumbar disc herniation. Gait Posture. 2018;63(May):296–301. Available from: https://doi.org/10.1016/j.gaitpost.2018.05.006.
Lin H, Seerden S, Zhang X, Fu W, Vanwanseele B. Inter-segmental coordination of the spine is altered during lifting in patients with ankylosing spondylitis A cross-sectional study. Med (United States). 2020;99(5):e18941.
List R, Gülay T, Stoop M, Lorenzetti S. Kinematics of the Trunk and the Lower During Restricted and Unrestricted Squats. J Strength Cond Res. 2013;27(6):1529–38.
Müller J, Müller S, Engel T, Reschke A, Baur H, Mayer F. Stumbling reactions during perturbed walking: Neuromuscular reflex activity and 3-D kinematics of the trunk - A pilot study. J Biomech. 2016;49(6):933–8. Available from: https://doi.org/10.1016/j.jbiomech.2015.09.041.
Noamani A, Vette AH, Preuss R, Popovic MR, Rouhani H. Quantification of multi-segment trunk kinetics during multi-directional trunk bending. Gait Posture. 2018;64(June):205–12. Available from: https://doi.org/10.1016/j.gaitpost.2018.06.027.
Papi E, Bull AMJ, McGregor AH. Spinal segments do not move together predictably during daily activities. Gait Posture. 2019;67(July 2018):277–83. Available from: https://doi.org/10.1016/j.gaitpost.2018.10.031.
Papi E, Bull AMJ, McGregor AH. Alteration of movement patterns in low back pain assessed by Statistical Parametric Mapping. J Biomech. 2020;100:109597. Available from: https://doi.org/10.1016/j.jbiomech.2019.109597.
Patel A, Pivec R, Shah NV, Leven DM, Margalit A, Day LM, et al. Motion analysis in the axial plane after realignment surgery for adolescent idiopathic scoliosis. Gait Posture. 2018;66(August):181–8. Available from: https://doi.org/10.1016/j.gaitpost.2018.08.015.
Pelegrinelli ARM, Silva MF, Guenka LC, Carrasco AC, Moura FA, Cardoso JR. Low back pain affects coordination between the trunk segments but not variability during running. J Biomech. 2020;101:109605. Available from: https://doi.org/10.1016/j.jbiomech.2020.109605.
Pesenti S, Prost S, Pomero V, Authier G, Roscigni L, Viehweger E, et al. Does static trunk motion analysis reflect its true position during daily activities in adolescent with idiopathic scoliosis? Orthop Traumatol Surg Res. 2020; Available from: https://doi.org/10.1016/j.otsr.2019.12.023
Pollock R, Heneghan P, Riches PE. Under-arm partial body weight unloading causes spinal elongation and vibration attenuation during treadmill walking. Gait Posture. 2008;28(2):271–7.
Preuss RA, Popovic MR. Three-dimensional spine kinematics during multidirectional, target-directed trunk movement in sitting. J Electromyogr Kinesiol. 2010;20(5):823–32. Available from: https://doi.org/10.1016/j.jelekin.2009.07.005.
Rouhani H, Mahallati S, Preuss R, Masani K, Popovic MR. Sensitivity of Intersegmental Angles of the Spinal Column to Errors Due to Marker Misplacement. J Biomech Eng. 2015;137(7). Available from: https://doi.org/10.1115/1.4030406/442561/Sensitivity-of-Intersegmental-Angles-of-the-Spinal
Arshad R, Angelini L, Zander T, Di Puccio F, El-Rich M, Schmidt H. Spinal loads and trunk muscles forces during level walking – A combined in vivo and in silico study on six subjects. J Biomech. 2018;70:113–23 Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85029750836&doi=10.1016%2Fj.jbiomech.2017.08.020&partnerID=40&md5=92e91d480d0230719167349ac01e08f4.
Rozumalski A, Schwartz MH, Wervey R, Swanson A, Dykes DC, Novacheck T. The in vivo three-dimensional motion of the human lumbar spine during gait. Gait Posture. 2008;28(3):378–84.
Ryan N, Bruno P. Analysis of 3D multi-segment lumbar spine motion during gait and prone hip extension. J Electromyogr Kinesiol. 2017;33:111–7. Available from: https://doi.org/10.1016/j.jelekin.2017.02.005.
Saad WAA, Mat Dzahir MA, Yamamoto S, Hussein M, Mohamad M, Saad SM, et al. Differences of spinal kinematics contribution between cervical and multi-segmental thoracic spine during Sit-To-Stand (STS) & Stand-To-Flexion (STF). IOP Conf Ser Mater Sci Eng. 2020;788(1):012026.
Sayers MGL, Bachem C, Schütz P, Taylor WR, List R, Lorenzetti S, et al. The effect of elevating the heels on spinal kinematics and kinetics during the back squat in trained and novice weight trainers. J Sports Sci. 2020;38(9):1000–8. Available from: https://doi.org/10.1080/02640414.2020.1738675.
Schinkel-ivy A, Drake JDM. Which motion segments are required to sufficiently characterize the kinematic behavior of the trunk? J Electromyogr Kinesiol. 2015;25(2):239–46. Available from: https://doi.org/10.1016/j.jelekin.2014.12.008.
Schmid S, Studer D, Hasler CC, Romkes J, Taylor WR, Brunner R, et al. Using skin markers for spinal curvature quantification in main thoracic adolescent idiopathic scoliosis: An explorative radiographic study. PLoS ONE. 2015;10(8):1–12.
Seay J, Selbie WS, Hamill J. In vivo lumbo-sacral forces and moments during constant speed running at different stride lengths. J Sports Sci. 2008;26(14):1519-29. https://doi.org/10.1080/02640410802298235.
Seerden SFL, Dankaerts W, Swinnen TW, Westhovens R, de Vlam K, Vanwanseele B. Multi-segment spine and hip kinematics in asymptomatic individuals during standardized return from forward bending versus functional box lifting. J Electromyogr Kinesiol. 2019;49(August):102352. Available from: https://doi.org/10.1016/j.jelekin.2019.102352.
Simonet E, Winteler B, Frangi J, Suter M, Meier ML, Eichelberger P, et al. Walking and running with non-specific chronic low back pain: What about the lumbar lordosis angle? J Biomech. 2020;108:109883. Available from: https://doi.org/10.1016/j.jbiomech.2020.109883.
Stoll J, Rector M, Baur H, Mayer F, Orthopaedics S, Müller J, et al. Influence of load on three-dimensional segmental trunk kinematics in one-handed lifting: A pilot study. J Appl Biomech. 2016;32(5):520–5 Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84991292346&doi=10.1123%2Fjab.2015-0227&partnerID=40&md5=75b8b7bc3446e074318affc8f292df8c.
Beaudette SM, Zwambag DP, Graham RB, Brown SHM. Discriminating spatiotemporal movement strategies during spine flexion-extension in healthy individuals. Spine J. 2019;19(7):1264–75. Available from: https://doi.org/10.1016/j.spinee.2019.02.002.
Sung PS, Danial P, Lee DC. Comparison of the different kinematic patterns during lateral bending between subjects with and without recurrent low back pain. Clin Biomech. 2016;38:50–5. Available from: https://doi.org/10.1016/j.clinbiomech.2016.08.006.
Sung PS, Park MS. Lumbar spine coordination during axial trunk rotation in adolescents with and without right thoracic idiopathic scoliosis. Hum Mov Sci. 2020;73(1S):102680. Available from: https://doi.org/10.1016/j.humov.2020.102680.
Swain CTVV, Whyte DG, Ekegren CL, Taylor P, McMaster K, Lee Dow C, et al. Multi-segment spine kinematics: relationship with dance training and low back pain. Gait Posture. 2018;68:274–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0966636218311512.
Tojima M, Ogata N, Yozu A, Sumitani M, Haga N. Novel 3-Dimensional Motion Analysis Method for Measuring the Lumbar Spine Range of Motion. Spine (Phila Pa 1976). 2013;38(21):E1327-33. Available from: https://insights.ovid.com/crossref?an=00007632-201310010-00008.
Wilk B, Karol LA, Johnston CE II, Colby S, Haideri N, Johnston CE, et al. The effect of scoliosis fusion on spinal motion: A comparison of fused and nonfused patients with idiopathic scoliosis. Spine (Phila Pa 1976). 2006;31(3):309–14. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-32244434091&doi=10.1097%2F01.brs.0000197168.11815.ec&partnerID=40&md5=15ea54bd083d9b3cc94175292acf3509.
Zwambag DP, Beaudette SM, Gregory DE, Brown SHM. Development of a Novel Technique to Record 3D Intersegmental Angular Kinematics During Dynamic Spine Movements. Ann Biomed Eng. 2018;46(2):298–309.
Preece SJ, Bramah C, Mason D. A marker set for measuring the kinematics of the lumbar spine and thoracic spine during running: a technical note. J Hum Sport Exerc. 2016;11(3):390–6. Available from: http://hdl.handle.net/10045/65034.
Ghasemi M, Arjmand N. Spinal segment ranges of motion, movement coordination, and three-dimensional kinematics during occupational activities in normal-weight and obese individuals. J Biomech. 2021;123:110539. Available from: https://doi.org/10.1016/j.jbiomech.2021.110539.
Glover NA, Kakar RS, Chaudhari AMW. Effects of spinal coupling and marker set on tracking of spine models during running. J Biomech. 2021;116:110217. Available from: https://doi.org/10.1016/j.jbiomech.2020.110217.
Alijanpour E, Abbasi A, Needham RA, Naemi R. Spine and pelvis coordination variability in rowers with and without chronic low back pain during rowing. J Biomech. 2021;120:110356. Available from: https://doi.org/10.1016/j.jbiomech.2021.110356.
Breloff SP, Chou L-S. a Multi-Segmented Approach To the Quantification of Trunk Movement During Gait. J Musculoskelet Res. 2015;18(02):1550009. Available from: https://doi.org/10.1142/S0218957715500098.
Hagins M, Swain CTV, Orishimo KF, Kremenic IJ, Liederbach M. Motion of the multi-segmented spine in elite dancers during passé and arabesque. Gait Posture. 2021;88(June):198–202. Available from: https://doi.org/10.1016/j.gaitpost.2021.05.032.
Niggli LA, Eichelberger P, Bangerter C, Baur H, Schmid S. Between-session reliability of skin marker-derived spinal kinematics during functional activities. Gait Posture. 2021;85(February):280–4. Available from: https://doi.org/10.1016/j.gaitpost.2021.02.008.
Choi AR, Kim YJ, Rim YH, Kang TG, Min K, Lee S, et al. Development of a spine kinematic model for the clinical estimation of abnormal curvature. IFMBE Proc. 2007;14:2892–5.
Claus AP, Hides JA, Moseley GL, Hodges PW. Thoracic and lumbar posture behaviour in sitting tasks and standing: Progressing the biomechanics from observations to measurements. Appl Ergon. 2016;53:161–8. Available from: https://doi.org/10.1016/j.apergo.2015.09.006.
Crosbie J, Vachalathiti R, Smith R. Patterns of spinal motion during walking. Gait Posture. 1997;5(1):6–12.
Deane JA, Papi E, Phillips ATM, McGregor AH. Reliability and minimal detectable change of the ‘Imperial Spine’ marker set for the evaluation of spinal and lower limb kinematics in adults. BMC Res Notes. 2020;13(1):1–8. Available from: https://doi.org/10.1186/s13104-020-05295-9.
Sugaya T, Sakamoto M, Nakazawa R, Wada N. Relationship between spinal range of motion and trunk muscle activity during trunk rotation. J Phys Ther Sci. 2016;28(2):589–95. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-84959331450&doi=10.1589%2Fjpts.28.589&partnerID=40&md5=69190964aa44699b2e63ec93c392ff30.
Peharec S, Jerković R, Bacić P, Azman J, Bobinac D. Kinematic measurement of the lumbar spine and pelvis in the normal population. Coll Antropol. 2007;31(4):1039–42. Available from: http://www.ncbi.nlm.nih.gov/pubmed/18217455.
Alemi MM, Burkhart KA, Lynch AC, Allaire BT, Mousavi SJ, Zhang C, et al. The Influence of Kinematic Constraints on Model Performance During Inverse Kinematics Analysis of the Thoracolumbar Spine. Front Bioeng Biotechnol. 2021;9(July):1–15.
Kudo S, Fujimoto M, Sato T, Nagano A. Quantitative evaluation of linked rigid-body representations of the trunk. Gait Posture. 2018;63:119–23. Available from: https://www.scopus.com/inward/record.uri?eid=2-s2.0-85055605442&doi=10.1016%2Fj.gaitpost.2018.04.046&partnerID=40&md5=7c7af07407c71972808233e1139e4b43.
Marich AV, Hwang CT, Salsich GB, Lang CE, Van Dillen LR. Consistency of a lumbar movement pattern across functional activities in people with low back pain. Clin Biomech. 2017;44:45–51. Available from: https://doi.org/10.1016/j.clinbiomech.2017.03.004.
Bagheri R, Takamjani IE, Dadgoo M, Sarrafzadeh J, Ahmadi A, Pourahmadi MR, et al. A protocol for clinical trial study of the effect of core stabilization exercises on spine kinematics during gait with and without load in patients with non-specific chronic low back pain. Chiropr Man Ther. 2017;25(1):1–8.
Hooker QL, Lanier VM, van Dillen LR. Consistent differences in lumbar spine alignment between low back pain subgroups and genders during clinical and functional activity sitting tests. Musculoskelet Sci Pract. 2021;52(October 2020):102336. https://doi.org/10.1016/j.msksp.2021.102336.
Knechtle D, Schmid S, Suter M, Riner F, Moschini G, Senteler M, et al. Fear-avoidance beliefs are associated with reduced lumbar spine flexion during object lifting in pain-free adults. Pain. 2021;162(6):1621–31.
Marich AV, Hwang CT, Sorensen CJ, van Dillen LR. Examination of the Lumbar Movement Pattern during a Clinical Test and a Functional Activity Test in People with and without Low Back Pain. PM R. 2020;12(2):140–6.
Seerden S, Dankaerts W, Vanwanseele B. Reliability of a multi-segmental kinematic model to analyse 3D movement in the lumbar spine. Gait Posture. 2016;49:53. Available from: https://doi.org/10.1016/j.gaitpost.2016.07.117.
Leardini A, Berti L, Begon M, Allard P. Effect of trunk sagittal attitude on shoulder, thorax and pelvis three-dimensional kinematics in able-bodied subjects during gait. PLoS ONE. 2013;8(10):1–7.
Connolly M, Middleton K, Spence G, Cant O, Reid M. Effects of Lumbar Spine Abnormality and Serve Types on Lumbar Kinematics in Elite Adolescent Tennis Players. Sport Med - Open. 2021;7(1):7.
Acknowledgements
None.
Funding
The project leading to the scientific results was supported by the European Commission (766012- SPINNER-H2020-MSCAITN-2017).
Author information
Authors and Affiliations
Contributions
JF carried out the main research and drafted the initial article. RS was involved in designing the study, coordinating the research process, and improving the initial article. PE and AL were involved in designing the study and providing valuable information that contributed to the paper. LC was involved in study design and improving the final article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that the research was conducted in the absence of any potential conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fayad, J., Eltes, P.E., Lazary, A. et al. Stereophotogrammetric approaches to multi-segmental kinematics of the thoracolumbar spine: a systematic review. BMC Musculoskelet Disord 23, 1080 (2022). https://doi.org/10.1186/s12891-022-05925-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05925-2