Abstract
Background
Femur fracture is a major burden among elderly people, leading patients to be bedridden for a long time in the hospital. The body is more likely to be in a catabolic state as a result of the prolonged fasting period required for surgery, leading to an increase in insulin resistance. Pre-operative carbohydrate loading has been shown to improve postoperative outcomes in several countries. The study aimed to evaluate the effect of pre-operative carbohydrate loading in femur fracture surgery.
Methods
This study was single-center, hospital-based, open-label, parallel-group randomized controlled trial conducted between August 2020 and November 2021. A total of 66 participants, aged 50 years and above having femur fractures planned for surgery were included in this study and assigned to the control (n = 33) and study (n = 33) groups through computer-generated random numbers. The control group was kept fasting from midnight to the next morning as in existence while the study group was intervened with carbohydrate loading according to the Enhanced Recovery After Surgery (ERAS) protocol. The pre-operative nutritional status was identified and the postoperative outcomes were measured using the Visual Analogue Score (VAS), Cumulative Ambulatory Score (CAS), and Modified Barthel Index (MBI) scoring systems. Statistical analyses were performed using the Chi-square test and the Student’s two-sample t-test to compare the outcomes between the two groups.
Results
All the participants completed the study. There was a significant reduction in the average postoperative pain in the carbohydrate loading group (VAS: 4.8 (SD ± 1.8), 95% CI: 4.7–5.4) as compared to the control group (VAS: 6.1 (SD ± 2.1), 95% CI: 5.3–6.8). The average CAS showed a significant improvement in regaining the mobility function of participants in the study group (CAS: 8.1 (SD ± 2.8), 95% CI: 7.1–9.1) than that of the control group (CAS: 6.8 (SD ± 2.8), 95% CI: 5.8–7.8). The mean MBI score of the participants at the time of discharge from the hospital was higher in the study group (MBI:13.1 (SD ± 2.3), 95% CI: 12.2–13.9) compared to the control group (MBI: 11.8 (SD ± 3.1), 95% CI:10.6–12.9). Similarly, the length of hospital stay after surgery had decreased in the study group than in the control group.
Conclusions
The uptake of carbohydrate loading showed reduced post-operative pain, enhanced functional mobility, and decreased length of hospital stay. This study warrants larger trials to show the effect of pre-operative carbohydrate loading in a clinical setting.
Trial registration
NCT04838366, first registered on 09/042021 (https://clinicaltrials.gov/ct2/show/NCT04838366).
Similar content being viewed by others
Introduction
Femur fracture leads to significant morbidity and mortality and represents one of the leading causes of hospital stay in older people [1]. The annual incidence of femur fracture ranges from 10 to 21 per 100,000 in the world [2, 3]. The annual crude hip fracture is 129 per 100,000 people aged 50 years in India [4]. It is mostly managed by a surgical procedure that creates stress among both patients and relatives. Moreover, people in older life have multi-morbidities such as type-2 diabetes (15%) [5], hypertension (44.9%) [6], thyroid disorder (15.9%) [7], osteoporosis (37.3%) [8] and hypomagnesaemia (48%) [9]. These types of age-related diseases make the treatment of femur fractures more risky and complicated.
According to the current protocol for surgery of femur fracture, the patients are kept in a fasting state from midnight to avoid the risk of pulmonary aspiration during surgery. This causes physical as well as mental discomfort among patients. This is an old technique that has been carried out for many years. Patients undergo a catabolic state after surgery, which can worsen the stress response and contribute to insulin resistance and hyperglycemia lengthening the recovery period [10]. Prolonged fasting for surgery may create different complications such as distress, confusion, instability, headache, dehydration, electrolyte imbalance, postoperative nausea, and vomiting [11]. The procedure of carbohydrate loading is only one small component of a new concept called Enhanced Recovery After Surgery (ERAS) that allows the patients to consume orally 100 g and 50 g of carbohydrates the night before and two hours before surgery respectively [12]. This modern approach has many advantages over traditional practice. Bisch et al., 2019 have mentioned that the physiological reason to provide the evening dose of carbohydrate beverage is to create glycogen stores in the body and the morning dose is to change the body to a “fed” state [13]. Mean gastric emptying time in the pre-operative carbohydrate loading (study) group and two control groups of elderly people having hip fractures showed no clinically important difference [14]. It justifies the findings of a study that prolonged fasting for surgery is unnecessary [11]. Preoperative carbohydrate loading decreases insulin resistance by up to 50% [15] and improves metabolic functions [16]. In cardiac patients, the use of ERAS protocol results in a 35% reduction in postoperative insulin doses [17]. The preoperative carbohydrate loading reduces the expression of Human leukocyte antigen (HLA)-DR on monocytes which decreases the risk of postoperative infection [18] and reduces the intraoperative core body temperature [19]. In addition, it improves muscle function because of less post-operative protein and nitrogen loss [20], which facilitates wound healing. It improves the recovery rate, hence decreasing the length of postoperative stay at hospital [21], and reduces the treatment cost to 15.2% [22]. Similarly, it is also associated with significantly better well-being [23].
In Europe, ERAS is a novel and scientific approach that is mostly used in general surgery, obstetrics, and gynecology [24]. Nutritional support, on the other hand, is considered less important for patients' fast recovery in most orthopedic programs [25]. In Nepal, the traditional approach of administering anesthesia to the patient in prolonged fasting is still in use. To the best of our knowledge, this study is the first of its kind to assess the efficacy of pre-operative carbohydrate loading for femur fracture. The study aimed to assess the effect of pre-operative carbohydrate loading on the improvement of postoperative pain, functional mobility, and the recovery rate among patients undergoing surgery for femur fracture management.
Methods
Study design, sample size, and setting
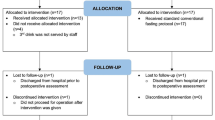
The report of this trial follows the Consolidated Standards of Reporting Trials (CONSORT) 2010 updated guidelines for reporting of randomized controlled trials [26] (Additional file 1). This study was single-center, hospital-based, open-label, parallel-group randomized controlled trial conducted between August 2020 and November 2021 (Fig .1). The study was conducted at the in-patient department of Nepal Orthopaedic Hospital, Kathmandu, Nepal. Nepal Orthopaedic Hospital was selected purposively because it is one of the Orthopaedics and Trauma Care Super-specialty centers in Nepal. According to hospital record, about 10 patients are operated on each day, with one or two cases of femur fracture [27]. The patients aged 50 years and above having a femur fracture planned for surgery, those patients who were mentally fit, and those patients who provided written informed consent were included in the study. Patients with pre-existing diabetes (Type 1 or 2), past carbohydrate intolerance, pathological fracture or any suspected pathology, and surgery failure or non-union cases were excluded from the study. These underlying conditions of the patients were assessed based on medical record and also verified by asking the patient or patient party verbally.
The sample size was determined based on a similar study with the primary outcome being the Cumulative Ambulatory Score (Mean ± SE) of the study group versus the control group as 12.76 ± 0.33 and 12.02 ± 0.32 respectively [23]. Considering this data and taking a level of significance at 5% and power of 80%, the sample size was calculated using a test comparing independent two means in Stata/MP version 14.1 (StataCorp LP, College Station, Texas). The calculated sample size was 60. Taking into account a 10% loss to follow-up and dropout, the total sample size was 66 (33 participants in each group).
Randomization
Participants were randomized in a 1:1 ratio and assigned to a study and control group randomly. Individual randomization was performed using a computer-generated random number. We created the computer-generated random number using a Microsoft excel sheet and coded control as ‘C’ and study as ‘S’. After that, we prepared envelopes according to a random number, and the participants 1 to 66 were allocated to either control or study group based on the random number. We used an envelope to minimize the selection bias by the researcher. Random numbers were kept in an envelope. Upon confirmation of a participant’s eligibility, the next envelope in the sequence was opened, and the intervention or the control allocation was entered on a randomization list.
Study variables
Outcome variables
The primary outcomes were postoperative pain and functional mobility; serum albumin level was a secondary outcome. The pain on the first postoperative day was assessed during the doctor's round at 10 o’clock in the morning through a visual analog scale (VAS) [28]. It consisted of a 10 cm straight line with the endpoints defining the intensity of pain from zero to 10 indicating that zero as “no pain at all’ and 10 as ‘worst pain’. They were asked to express their severity of pain at the time of data collection in a descriptive term as no pain, mild pain, moderate pain, severe pain, or worst pain, and they were ranked to numerical scores for analysis. Similarly, the Cumulative Ambulatory Score (CAS) was applied to find out the regaining basic mobility independence on the first, second, and third postoperative day like the VAS assessment done at the same time during the doctor's round [29]. It consisted of three aspects of activities; getting in and out of bed, sit-to-stand from a chair, and indoor walking. Each activity was assessed on a three-point ordinal scale from zero to two (0 = “not able”, 1 = “human assistance” and 2 = “independent”), hence a total of daily CAS score ranging from zero to six and zero to 18 for three days assessment [30]. The Modified Barthel Index-Activities of Daily Living (MBI-ADL) was also used to measure independence at the time of discharge from the hospital [31]. The score ranges from 0 to 100; 0–20 indicate “total” dependency, 21–60 indicate “severe” dependency, 61–90 indicate “moderate” dependency and 91–99 indicate “slight” dependency [32]. A score from 0 to 20 for “total dependency” was considered for the study; the higher the score, better the self-care activity.
Predictor variables
Socio-demographic information of the respondents such as age, sex, Body Mass Index (BMI), occupation, ethnicity, religion, residence area, and educational level were collected using a semi-structured questionnaire interview. Nutritional assessments were done with a Mini Nutritional Assessment Scale (MNA) [33]. It has 18 items related to four different aspects; anthropometric measurement (BMI, weight loss, and arm and calf circumferences); general assessment (lifestyle, medication, mobility, and presence of signs of depression or dementia); short dietary assessment (number of meals, food and fluid intake and autonomy of feeding); and subjective assessment (self-perception of health and nutrition) [34]. They were categorized as having normal nutritional status (if MNA score was 24–30), at risk of malnutrition (if MNA score was 17–23.9), and malnourished ( if MNA score < 17). The clinical parameters such as the site and side of femur fracture, types of fracture, number of fractures, and biochemical parameters like preoperative hemoglobin level and serum albumin level were recorded from the hospital record file.
Intervention
Having assessed the patients, they were randomized either to the control group or the study group if they met the inclusion criteria. The control group was kept fasting from midnight to the next morning as in existence while the study group was intervened with carbohydrate loading according to the ERAS protocol [35]. We used the glucose-D as a carbohydrate-rich drink of Nepali product (Reg. No.: 3506/045/046, Department of Food Technology and Quality Control, DFTQC No.: 01–33-55–03-218). It contains Dextrose Monohydrate (99.4%), Calcium Phosphate (0.6%) and Vitamin D (0.0001%). The participants were operated on under spinal anesthesia as usual in the hospital setup condition. The intra-operative data regarding the types of surgery, types of implants used, duration of surgery, amount of blood loss, blood transfusion and adverse effect were collected. The hemoglobin and serum albumin level were recorded in the morning of the first post-operative day. The VAS score for pain on the first postoperative day, the CAS score for regaining the mobility function on the first, second and third post-operative days were measured during doctors round at 10 o’clock in the morning. The MBI score was also considered to find out the mobility independence on the day of discharge. Subsequently, all these scoring systems were used to identify the association of pre-operative carbohydrate loading with the recovery rate of patients in terms of the well-being of patients and functional mobility as outcome variables which were further evaluated by the length of hospital stay after surgery.
Statistical analysis
The data entry was done using EpiData version 3.0, and analyzed based on the intention-to-treat (ITT) approach using Stata/MP version 14.1 (StataCorp LP, College Station, Texas). Descriptive statistics such as frequency, percentage, and mean (standard deviation) were used. Chi-square and Student’s two-sample t-tests were used to compare the outcomes between the study and control groups. All p-values less than 0.05 were considered statistically significant and no adjustment was made for multiple testing.
Ethical consideration
The ethical approval was obtained from the Ethical Review Board (ERB) of the Nepal Health Research Council (NHRC) (Reg. Number: 3104, approved on 11/05/2021). We also took permission to conduct the research from Nepal Orthopaedic Hospital, Kathmandu, Nepal. We constituted a Data and Safety Monitoring Board (DSMB) consisting of an orthopedic surgeon, dietitian, and statistician. The DSMB members prepared study-stopping rules and reviewed all the possible effects reported in the study. The respondents were informed about the purpose of this study. After obtaining written informed consent, they were recruited as eligible candidates for the study. Voluntary informed participation and freedom of refusal at any time during the study were strongly applied without giving reason and fear. Privacy and confidentiality of the collected information were ensured at all levels. The purpose of the study, benefits, and harm to the participants were properly explained in simple and understandable terms by the team members of the research. No financial benefits or burdens concerned with the study were provided to the patients.
Results
Socio-demographic characteristics of the participants
More than half participants were female in the study group while there were more male participants in the control group. The study group had slightly more participants as literate, however, both groups had nearly half of the participants unemployed. Similarly, more participants were from the mountain region in the study group while participants from the Terai region were higher in the control group. (Table1).
Clinical assessment of the participants
Both groups had comparable types of femur fractures; proximal femur fracture (neck of femur fracture, inter-trochanteric fracture, and sub-trochanteric fracture), the shaft of femur fracture, and distal femur fracture. Similarly, both groups had a similar pattern of clinical characteristics such as fracture side (left or right), the number of bone fractures, types of implants used, types of surgery performed (Open reduction and internal fixation/Closed reduction and internal fixation), blood loss, blood transfusion, adverse effect, and duration of surgery. However, there was a difference in the pre-nutritional status of the participants. The control group had more participants having normal nutritional status than that of the study group but no difference in malnutrition and risk of malnutrition (Table 2).
Biochemical parameters of the participants
There were comparable pre-nutritional status, pre-operative as well as post-operative hemoglobin and pre-operative serum albumin. However, the control group showed more loss of serum albumin than the study group in surgery (Table 3).
Primary outcomes after carbohydrate loading
The post-operative pain through VAS was significantly reduced in the study group compared to the control group on the next day of surgery. The cumulative ambulatory score (CAS) showed a significant improvement in regaining the mobility function of participants in the study group than that of the control group. The mean modified Barthel Index (MBI) score of the participants at the time of discharge from the hospital was higher in the study groups. Similarly, the length of hospital stay after surgery was shorter in the study group than in the control group. (Fig. 2 and Table4).
Discussion
Pre-operative carbohydrate loading had no adverse effects in our study, which is consistent with prior findings [36, 37]. According to Loodin and Hommel, the carbohydrate loading reduced post-operative complications associated with hip fracture by 50% [38]. In our study, two participants experienced hypoglycemia during surgery, which was managed by the attending anesthesiologist in the operation theater (Table 2). A systematic review by Sebranek et al., 2013 showed that the alterations in blood glucose might be multifactorial and other modifiers may be concerned with its homeostasis [39].
Postoperative pain reduction or elimination with minimum side effects is an important quality measure of patients’ well-being and satisfaction that leads to a shorter length of hospital stay and reduced hospital costs [40]. This research showed that pre-operative carbohydrate loading significantly reduced post-operative pain, which is in line with previous findings [23, 41]. The spectrum of fasting induces the C-Reactive Protein (CRP), a marker of subclinical inflammation [42], which is the underlying origin of all pain [43]. The higher the CRP level, the more the oxidative stress [44]. Perrone et al., 2011 found a higher postoperative serum CRP in the control group than that of the preoperative carbohydrate drinks group [45]. Hence, preoperative carbohydrate drinks reduce postoperative oxidative stress, [46] and it is related to the reduction of functional pain [47]. Besides these, it can be explained that dietary intake can promote the function of the nervous system, immune system, and endocrine system which has an impact on pain experience [48].
The regaining of functional mobility after the surgery is a milestone in hospital rehabilitation [49]. We assessed the mobility function with the cumulative ambulatory scores on the 1st, 2nd, and 3rd postoperative days. The CAS score of the study group was significantly higher than that of the control group. This finding is consistent with the study of Chada et.al in India [23]. The carbohydrate drinks before surgery improve carbohydrate uptake, utilization, storage, and protein metabolism with a 50% reduction in loss of lean body mass [50]. Preoperative carbohydrate beverages help to store glycogen in the muscle [13] and prevent the loss of lower limb mass leading to better postoperative recovery [19].
The MBI scoring system evaluates the activities of daily living (ADL) based on the degree of assistance required to perform the task after a stroke or surgery [51]. Our study found a higher value of MBI-ADL index score in the study group than that of the control group. Ping et, al (2021) also found a dramatically higher Barthel score of self-care ability among the elderly patients with the ERAS approach in total hip replacement surgery [24].
Due to the occurrence of a more catabolic state during the surgery period, there occurs the destruction of many important inorganic as well as organic elements (for example nitrogen and protein loss) in the body, altering the speed of wound healing [52]. One of them is the decrement of serum albumin, commonly observed in most patients [53] which is the result of intense surgical stress predicting increased postoperative complications [54]. The present study found that the preoperative carbohydrate prevented the decrease of serum albumin in the body during surgery, consistent with the study [45]. It can be explained through the mechanism that preoperative fasting induces perioperative insulin resistivity which inhibits the synthesis of serum albumin [55]. Serum albumin has several physiological functions and the determined serum albumin reflects the physical or health status, predicting the prognosis [56]. Low serum albumin leads to a poor prognosis [57]. It is the marker for surgical stress that may delay the clinical outcome [58] and occur the mortality of patients [59].
The reduction of hospital stay facilitates financial, operational, and clinical outcomes [60]. This study reveals the decrease in hospital stay with carbohydrate loading supported by different studies [21, 22, 61,62,63]. Amer et. al find that pre-operative carbohydrate drinks reduce the length of postoperative stay at the hospital from 0.4 to 0.2 days compared with fasting [64]. Kotfish et al., 2020 find a 50% reduction in the length of ICU stay after cardiac surgery [17].
Our study has a few limitations. We could not evaluate the insulin resistivity and other hematological parameters due to the high cost and also the unavailability of most of the investigations in the laboratory of the study center. Furthermore, the patient's medical co-morbidities based on the American Society of Anesthesiologists (ASA) could not be analyzed to rule out the severity of health [65], which affects the recovery rate. The sample size for this study was limited and the data were collected at the time of the first wave of the COVID-19 pandemic in Nepal which interrupted the data collection process.
Conclusion
Pre-operative carbohydrate loading in femur fractures accelerates recovery rate in terms of postoperative pain and ambulatory function, shortening hospital stay. This study provides preliminary evidence on the benefits of pre-operative carbohydrate loading and warrants larger trials with a higher sample size for stronger evidence. Further research can be conducted using beverages that contain carbohydrates, fat, protein, and other micronutrients to acquire additional better postoperative outcomes.
Availability of data and materials
The data that supports the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restriction.
Abbreviations
- ADL:
-
Activities of Daily Living
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body Mass Index
- CAS:
-
Cumulative Ambulatory Score
- CRP:
-
C-Reactive Protein
- DSMB:
-
Data and Safety Monitoring Board
- ERAS:
-
Enhanced Recovery After Surgery
- ERB:
-
Ethical Review Board
- VAS:
-
Visual Analogue Score
- MBI:
-
Modified Barthel Index
- MNA:
-
Mini Nutritional Assessment
- NHRC:
-
Nepal Health Research Council
References
Breedveld-Peters JJL, Reijven PLM, Wyers CE, van Helden S, Arts JJC, Meesters B, et al. Integrated nutritional intervention in the elderly after hip fracture. A process evaluation Clin Nutr. 2012;31:199–205.
Weiss RJ, Montgomery SM, Al Dabbagh Z, Jansson KÅ. National data of 6409 Swedish inpatients with femoral shaft fractures: Stable incidence between 1998 and 2004. Injury. 2009;40:304–8.
Enninghorst N, McDougall D, Evans JA, Sisak K, Balogh ZJ. Population-based epidemiology of femur shaft fractures. J Trauma Acute Care Surg. 2013;74:1516–20.
Dhanwal D, Dixit V, Mithal A, Siwach R, Jameson K, Cooper C. Incidence of hip fracture in Rohtak district, North India. Arch Osteoporos. 2013;8:135.
Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Kaabi J Al. Epidemiology of Type 2 Diabetes – Global Burden of Disease and Forecasted Trends. J Epidemiol Glob Health. 2020;10:107–11.
Manandhar K, Koju R, Sinha NP, Humagain S. Prevalence and associated risk factors of hypertension among people aged 50 years and more in Banepa Municipality. Nepal Kathmandu Univ Med J. 2012;10:35–8.
Deraz H, Shawk N, Abedlnabi A-S, Ali E-F. Study of Thyroid Profiles in the Elderly. Zagazig Univ Med J. 2019;25:648–56.
Chaudhary NK, Timilsena MN, Sunuwar DR, Pradhan PMS, Sangroula RK. Association of Lifestyle and Food Consumption with Bone Mineral Density among People Aged 50 Years and above Attending the Hospitals of Kathmandu, Nepal. J Osteoporos. 2019;22;2019:1536394.
Scaturro D, Vitagliani F, Terrana P, Tomasello S, Camarda L, Letizia MG. Does the association of therapeutic exercise and supplementation with sucrosomial magnesium improve posture and balance and prevent the risk of new falls? Aging Clin Exp Res. 2022;34:545–53.
Kaye A, Urman R, Cornett E, Hart B, Chami A, Gayle J, et al. Enhanced recovery pathways in orthopedic surgery. J Anaesthesiol Clin Pharmacol. 2019;35:35–9.
Abebe WA, Rukewe A, Bekele NA, Stoffel M, Dichabeng MN, Shifa JZ. Preoperative fasting times in elective surgical patients at a referral hospital in Botswana. Pan Afr Med J. 2016;16;23:102.
Melnyk M, Casey RG, Black P, Koupparis AJ. Enhanced recovery after surgery (eras) protocols: Time to change practice? J Can Urol Assoc. 2011;5:342–8.
Bisch S, Nelson G, Altman A. Impact of nutrition on enhanced recovery after surgery (ERAS) in gynecologic oncology. Nutrients. 2019;16;11(5):1088.
Hellström PM, Samuelsson B, Al-Ani AN AN, Hedström M. Normal gastric emptying time of a carbohydrate-rich drink in elderly patients with acute hip fracture: A pilot study. Normal gastric emptying time of a carbohydrate-rich drink in elderly patients with acute hip fracture: A pilot study. 2017;17:0–5.
Nygren J. The metabolic effects of fasting and surgery. Best Pract Res Clin Anaesthesiol. 2006;20:429–38.
Singh M, Chaudhary M, Vashistha A, Kaur G. Evaluation of effects of a preoperative 2-hour fast with glutamine and carbohydrate rich drink on insulin resistance in maxillofacial surgery. J Oral Biol Craniofacial Res. 2015;5:34–9.
Kotfis K, Jamioł-Milc D, Skonieczna-żydecka K, Folwarski M, Stachowska E. The effect of preoperative carbohydrate loading on clinical and biochemical outcomes after cardiac surgery: A systematic review and meta-analysis of randomized trials. Nutrients. 2020;12:1–21.
Pillinger NL, Robson JL, Kam PCA. Nutritional Prehabilitation: Physiological Basis and Clinical Evidence. Anaesth Intensive Care. 2018;46:453–62.
Hamamoto H, Yamamoto M, Masubuchi S, Ishii M, Osumi W, Tanaka K, et al. The impact of preoperative carbohydrate loading on intraoperative body temperature: a randomized controlled clinical trial. Surg Endosc. 2018;32:4393–401.
Moningi S, Patki A, Padhy N, Ramachandran G. Enhanced recovery after surgery: An anesthesiologist’s perspective. J Anaesthesiol Clin Pharmacol. 2019;35:5–13.
Bilku DK, Dennison AR, Hall TC, Metcalfe MS, Garcea G. Role of preoperative carbohydrate loading : a systematic review. 2014;96:15–22.
Tong Y, Fernandez L, Bendo JA, Spivak JM. Enhanced recovery after surgery trends in adult spine surgery: A systematic review. Int J Spine Surg. 2020;14:623–40.
Chada RR, Maryada VR, Mulpur P, Reddy A, Maska A. Does Preoperative Carbohydrate Loading Help Outcomes in Total Knee Replacement Surgery? J Nutr Med Diet Care. 2019;5:36.
Ping H, Ling X, Xue Y, Dong F. Effect of ERAS Combined with Comfortable Nursing on Quality of Life and Complications in Femoral Neck Fractures of the Aged People. Evidence-based Complement Altern Med. 2021;3;2021:8753076.
Briguglio M, Gianola S, Aguirre MFI, Sirtori P, Perazzo P, Pennestri F, et al. Nutritional support for enhanced recovery programs in orthopedics: Future perspectives for implementing clinical practice. Nutr Clin Metab. 2019;33:190–8.
Schulz KF, Altman DG, Moher D. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:834–40.
Nepal Orthopaedic Hospital. Nepal Orthopaedic Hospital. https://www.noh.org.np/. Accessed 6 Aug 2022.
Beletsky A, Lu Y, Nwachukwu BU, Polce E, Maheshwer B, Chahla J, et al. Preoperative psychometric properties of visual analog scale asessments for function, pain, and strength compared with legacy upper extremity outcome measures in glenohumeral osteoarthritis. JSES Int. 2020;4:443–8.
Çolak İ, Mete E, Kristensen MT. Translation, reliability, agreement and validity of the Turkish version of Cumulated Ambulation Score in patients with hip fracture. 2020;31:346–52.
Kristensen MT, Jakobsen, Nielsen JW, Jorgensen LM, Nienhuis RJ, Jonsson LR. Cumulated Ambulation Score to evaluate mobility is feasible in geriatric patients and in patients with hip fracture. Dan Med J. 2012;59(7):A4464.
Ohura T, Hase K, Nakajima Y, Nakayama T. Validity and reliability of a performance evaluation tool based on the modified Barthel Index for stroke patients. 2017;:1–8.
Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42:703–9.
Miu KYD, Lam PS. Effects of nutritional status on 6-month outcome of hip fractures in elderly patients. Ann Rehabil Med. 2017;41:1005–12.
Holvoet E, Wyngaert K Vanden, Van Craenenbroeck AH, Van Biesen W, Eloot S. The screening score of Mini Nutritional Assessment (MNA) is a useful routine screening tool for malnutrition risk in patients on maintenance dialysis. PLoS One. 2020;15.
Li Z, Lu S, Kong C, Sun W, Wang P, Zhang S. Comparative short-term outcomes of enhanced recovery after surgery ( ERAS ) program and non-ERAS traditional care in elderly patients undergoing lumbar arthrodesis : a retrospective study. 2021.
Lende TH, Austdal M, Varhaugvik AE, Skaland I, Gudlaugsson E, Kvaløy JT, et al. Preoperative carbohydrate loading and intraoperative goal-directed fluid therapy for elderly patients undergoing open gastrointestinal surgery: a prospective randomized controlled trial. BMC Cancer. 2019;19.
Liu X, Zhang P, Liu MX, Ma JL, Wei XC, Fan D. Preoperative carbohydrate loading and intraoperative goal-directed fluid therapy for elderly patients undergoing open gastrointestinal surgery: a prospective randomized controlled trial. BMC Anesthesiol. 2021;21.
Loodin Å, Hommel A. The effects of preoperative oral carbohydrate drinks on energy intake and postoperative complications after hip fracture surgery: A pilot study. Int J Orthop Trauma Nurs. 2021;41:100834.
Sebranek JJ, Lugli AK, Coursin DB. Glycaemic control in the perioperative period. Br J Anaesth. 2013;111 SUPPL.1.
Garimella V, Cellini C. Postoperative pain control. Clin Colon Rectal Surg. 2013;26:191–6.
Pachella LA, Mehran RJ, Curtin K, Schneider SM. Preoperative Carbohydrate Loading in Patients Undergoing Thoracic Surgery: A Quality-Improvement Project. J Perianesthesia Nurs. 2019;34:1250–6.
Aronson D, Bartha P, Zinder O, Kerner A, Shitman E, Markiewicz W, et al. Association between fasting glucose and C-reactive protein in middle-aged subjects. Diabet Med. 2004;21:39–44.
Omoigui S. The biochemical origin of pain: the origin of all pain is inflammation and the inflammatory response. Part 2 of 3 - inflammatory profile of pain syndromes. Med Hypotheses. 2007;69:1169–78.
Abramson JL, Hooper WC, Jones DP, Ashfaq S, Rhodes SD, Weintraub WS, et al. Association between novel oxidative stress markers and C-reactive protein among adults without clinical coronary heart disease. Atherosclerosis. 2005;178:115–21.
Perrone F, Da-Silva-Filho AC, Adôrno IF, Anabuki NT, Leal FS, Colombo T, et al. Effects of preoperative feeding with a whey protein plus carbohydrate drink on the acute phase response and insulin resistance. A randomized trial. Nutr J. 2011;10.
Nijs J, Tumkaya Yilmaz S, Elma Ö, Tatta J, Mullie P, Vanderweeën L, et al. Nutritional intervention in chronic pain: an innovative way of targeting central nervous system sensitization? Expert Opin Ther Targets. 2020;24:793–803.
Strath LJ, Jones CD, George AP, Lukens SL, Morrison SA, Soleymani T, et al. The effect of low-carbohydrate and low-fat diets on pain in individuals with knee osteoarthritis. Pain Med (United States). 2020;21:150–60.
International Association for the Study of Pain (IASP). Nutrition and Chronic Pain. Int Assoc Study Pain. 2020;1–5.
Hulsbæk S, Larsen RF, Troelsen A. Predictors of not regaining basic mobility after hip fracture surgery. Disabil Rehabil. 2015;37:1739–44.
Kratzing C. Pre-operative nutrition and carbohydrate loading. Proc Nutr Soc. 2011;70:311–5.
Lee SY, Kim DY, Sohn MK, Lee J, Lee SG, Shin Y Il, et al. Determining the cut-off score for the Modified Barthel Index and the Modified Rankin Scale for assessment of functional independence and residual disability after stroke. PLoS One. 2020;15(1):e0226324.
Hirsch KR, Wolfe RR, Ferrando AA. Pre-and post-surgical nutrition for preservation of muscle mass, strength, and functionality following orthopedic surgery. Nutrients. 2021;15;13(5):1675.
Ge X, Dai X, Ding C, Tian H, Yang J, Gong J, et al. Early postoperative decrease of serum albumin predicts surgical outcome in patients undergoing colorectal resection. Dis Colon Rectum. 2017;60:326–34.
Labgaa I, Joliat GR, Kefleyesus A, Mantziari S, Schäfer M, Demartines N, et al. Is postoperative decrease of serum albumin an early predictor of complications after major abdominal surgery? A prospective cohort study in a European centre. BMJ Open. 2017;7(4):e013966.
Rizvanović N, Nesek Adam V, Čaušević S, Dervišević S, Delibegović S. A randomised controlled study of preoperative oral carbohydrate loading versus fasting in patients undergoing colorectal surgery. Int J Colorectal Dis. 2019;34:1551–61.
Chien SC, Chen CY, Lin CF, Yeh HI. Critical appraisal of the role of serum albumin in cardiovascular disease. Biomark Res. 2017;5:31.
Artero A, Zaragoza R, Camarena JJ, Sancho S, González R, Nogueira JM. Prognostic factors of mortality in patients with community-acquired bloodstream infection with severe sepsis and septic shock. J Crit Care. 2010;25:276–81.
Hübner M, Mantziari S, Demartines N, Pralong F, Coti-Bertrand P, Schäfer M. Postoperative Albumin Drop Is a Marker for Surgical Stress and a Predictor for Clinical Outcome: A Pilot Study. Gastroenterol Res Pract. 2016;2016:8743187.
Li G, Zhou X, Hou X, Luo Y, Li D, Fan T. Association between serum albumin and mortality in Japan older people with dysphagia. Sci Rep. 2022;15;12(1):12089.
Abuzied Y, Maymani H, AlMatouq B, AlDosary O. Reducing the Length of Stay by Enhancing the Patient Discharge Process: Using Quality Improvement Tools to Optimize Hospital Efficiency. Glob J Qual Saf Healthc. 2021;4:44–9.
Lui D, Murphy M, McHugh G, Orakzai S, Jan W, Higgins P, Kenny P, Keogh P, O’Flanagan S. PROSPECTIVE RANDOMISED CONTROLLED STUDY: PRE OPERATIVE CARBOHYDRATE LOADING IN HIP AND FEMORAL FRACTURE PATIENTS REDUCES POST OPERATIVE HYPERGLYCAEMIA. Orthop Proc. 2018;92–B, No.
Nasution AH, Hamdi T, Lubis B. Role of preoperative carbohydrate loading for length of hospital stay in elective surgery patient: Meta-analysis study. J Drug Alcohol Res. 2020;9:1–5.
Blum CL, Akerman M, Callari M, Jordan E, Capozzi JD. Association of nausea and length of stay with carbohydrate loading prior to total joint arthroplasty. J Clin Outcomes Manag. 2019;26:175–9.
Amer MA, Smith MD, Herbison GP, Plank LD, McCall JL. Network meta-analysis of the effect of preoperative carbohydrate loading on recovery after elective surgery. Br J Surg. 2017;104:187–97.
Doyle D, Bansal P. American Society of Anesthesiologists Classification. Obstet Anesth Dig. 2021;1:31.
Acknowledgements
We would like to heartily thank the administration, doctors, nurses, and technicians of Nepal Orthopaedic Hospital, Kathmandu, Nepal who cooperated in the data collection and the study participants who volunteered to participate in this study.
Funding
This research was carried out under the funding provided by Nepal Health Research Council (NHRC), Nepal under the Provincial Research Grant (Grant number: 110/2021).
Author information
Authors and Affiliations
Contributions
All the authors contributed to manuscript preparation and editing. NKC: conceptualization, study design, methodology application, recruitment, intervention, data collection, outcome assessment, data curation, formal analysis, data interpretation, software utilization, project administration, validation, drafting manuscript, and editing. DRSu: conceptualization, study design, methodology application, data curation, formal analysis, data interpretation, software utilization, validation, manuscript editing, and overall monitoring and supervision. RS: conceptualization, study design, methodology application, and manuscript editing. MK: conceptualization, study design, methodology application, and manuscript editing. MNT: methodology application, project administration, validation, and manuscript editing. AG: methodology application, project administration, validation, and manuscript editing. SB: methodology application, project administration, validation, and manuscript editing. DRSi: data interpretation, manuscript editing, and critical review. PK: methodology application, project administration, validation, and manuscript editing. KKB: methodology application, project administration, validation, supervision, and manuscript editing. PMSP: critical review, editing, and overall monitoring and supervision. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
We confirm that all methods were carried out in accordance with relevant guidelines and regulations. The ethical approval was obtained from the Ethical Review Board (ERB) of NHRC (Reg. Number: 3104, approved on 11/05/2021). The clinical trial registry was done with Clinical Trial.gov. (Identifier: NCT04838366. Registered on 09/04 2021). Written informed consent was obtained from all patients recruited for this study.
Consent for publication
All participants provided informed consent for publication.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
CONSORT 2010 checklist of information to include when reporting a randomised trial*.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chaudhary, N.K., Sunuwar, D.R., Sharma, R. et al. The effect of pre-operative carbohydrate loading in femur fracture: a randomized controlled trial. BMC Musculoskelet Disord 23, 819 (2022). https://doi.org/10.1186/s12891-022-05766-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05766-z