Abstract
Background
Cardiovascular diseases are the leading cause of death and comorbidity worldwide. High blood pressure and resting heart rate are risk factors (or vital signs) critical to cardiovascular health, patient safety, and medical management. Physiotherapists play a fundamental role in risk factor identification, early diagnosis, and subsequent management of cardiovascular disease. To date there is limited research in Europe investigating the level of knowledge and skills possessed by physiotherapists regarding cardiovascular disease screening. Three studies previously observed inadequate vital signs screening behaviors of physiotherapists practicing in the United States and Saudi Arabia. The primary aim of this study was to investigate cardiovascular knowledge and screening practices among Italian physiotherapists, according to the current practice recommendations.
Methods
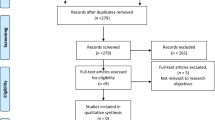
A Cross-Sectional Survey was developed adapting two previous surveys. The survey was administered to members of the Italian Physiotherapy Association. Chi squared test, Mann-Whitney test or Kruskal-Wallis test were used to study differences among subgroups and question responses.
Results
The required sample size was met with total of 387 Italian physiotherapists completing the survey. 80% consider relevant cardiovascular assessment. However, 72.2% were not familiar to guidelines recommendations and only 50% screen vital signs routinely. Their knowledge of normative blood pressure (high-normal, 16%; hypertension, 12%) and heart rate values (bradycardia, 24%; tachycardia, 26%) were low. Although participants reported being skilled for blood pressure measurement (quite sure, 52%; sure, 27%), their adherence to guidelines is low (baseline measurement on both arm, 25%; 3 repeated measures, 46%). Only 27.8% reported to measure exercise related BP and 21.3% of them understood the concept of exaggerated BP. No significant differences between subgroups were found.
Conclusions
Our study revealed that a concerning proportion of Italian physiotherapists are not versed in fundamentals of properly performing cardiovascular screenings. This lack of knowledge is present across the profession and may impact on appropriate triage and management. The poorly executed screening has the potential to negatively impact the patient and the practitioner. Given the absence of Italian guidelines, we produced and implemented three infographics for public use, which have the dual objective of raising awareness about this subject and providing practical resources for everyday practice.
Similar content being viewed by others
Background
Patients with musculoskeletal disorders frequently present with significant cardiovascular risk factors and disease (CVD). Patients may also present with unrecognized or undiagnosed risk factors and disease, which may require referral [1,2,3,4,5]. An estimated 69% of outpatient musculoskeletal physical therapists encounter patients daily if not twice per week with an established diagnosis of or moderate/high risk factors for cardiovascular disease [2]. Early detection and timely referral of unrecognized CVD ensures patient safety and appropriate medical management [6, 7]. Physiotherapists, particularly with direct access, must routinely screen for blood pressure (BP) and heart rate (HR) to identify risk factors, support recommended management, and ensure medical referrals [1, 8,9,10,11,12,13].
CVD arises from an interplay between a multitude of factors and is the leading cause of disability-adjusted life years worldwide, morbidity and mortality [14,15,16,17]. High blood pressure (HBP) is the leading risk factor for CVD among the most common risk factors (i.e., smoking, diabetes, dyslipidemia/hypercholesterolemia, obesity, physical inactivity/low fitness, unhealthy diet, family history, male sex, obstructive sleep apnea, psychological stress) [18]. The prevalence of HBP in central and eastern Europe is estimated to be over 150 million, reaching 30-45% in adulthood, with a peak of 60% in ages over 60 years old [19].
Recent estimations suggest a positive correlation between increased systolic (SBP) and diastolic blood pressure (DBP) and CVD, i.e. the higher the pressure, the greater the risk [6]. For prevention and treatment purposes, the most recent guidelines developed by the International and the European society of Hypertension (ISH and ESH) recommended to categorize HBP as normal, elevated, or stage 1 or 2 hypertension. Based on a careful reading obtained on the average of ≥2 occasions, after having selected the arm with the higher reading, normal blood pressure for most adults is defined as a SBP of <130mmHg and a DBP of <85mmHg. HBP should be categorized as high-normal (130–139mmHg and/or <85-89mmHg), hypertension grade 1 (140–159mmHg and/or 90–99 mm Hg), and hypertension grade 2 (≥160mmHg and/or ≥100mmHg) [20]. Notably, when SBP and DBP measurements are recorded in 2 different categories, the individual should be designated to the higher one [18]. A report suggests over 55% of patients are unaware of having HBP due to its often asymptomatic nature which may contribute to an increased risk of mortality [6]. Furthermore, masked hypertension (MH) is a common event (14-30% in normotensive population) which occurs when a hypertensive patient presents with a normal BP reading [18, 21]. It was estimated that an exaggerated BP response to exercise and physical activity could detect 41% of MH [17, 22, 23]. Exercise BP response is unscreened by both medical doctors and physiotherapists although the American Heart Association (AHA) strongly recommends MH detection, [2, 18]. Exaggerated BP increase to exercise has also been found to be a valuable screening and prognostic tool for both unmanifested CVD and future cardiovascular events [24]. The AHA defined exaggerated increases in BP in response to exercise as SBP >210mmHg for men and >190mmHg for women, and a DBP increase >10mmHg above resting values [25].
Heart rate (HR) is a parameter/vital sign important to those patients at risk of CVD. An elevated resting heart rate increases the likelihood of future cardiovascular pathologies and becomes particularly significant above 90 beats per minute [26]. HR is an indirect parameter of myocardial oxygen demand, coronary blood flow and myocardial performance that can be easily and non-invasively measured. Elevated resting heart rate in combination with HBP is associated with a further increased risk of mortality [26].
To date there is limited research investigating the level of cardiovascular screening knowledge and psychomotor skills possessed by practicing physiotherapists. Two studies previously observed inadequate screening behaviors of physiotherapists in the United States and Saudi Arabia towards BP and HR assessment observing inadequate screening behaviors [2, 27]. However, this question has not been investigated in Europe. In Italy cardiovascular rehabilitation is included during the entry level training for physiotherapists. Italian physiotherapists are also increasingly practicing as direct access providers, which potentially makes them the first point of contact within the healthcare system [28,29,30]. Therefore, it is imperative that Italian physiotherapists understand the importance of CVD screening, and demonstrate competency with examination techniques in order to safely manage these cases, and confidently communicates the need for referral when necessary [31]. Therefore, the purposes of our study were to 1) investigate the knowledge and the utilization of cardiovascular screening among Italian physiotherapists and 2) to develop a resource to improve clinical practice for cardiovascular screening in the physiotherapy outpatient setting.
Methods
We developed an online cross-sectional survey using the online platform Survey Monkey (SVMK Inc., San Mateo, USA) addressed to Italian physiotherapists. The investigation was designed in line with the Checklist for Reporting Results of Internet E-Surveys [32] and the Strengthening the Reporting of Observational studies in Epidemiology guidelines [33]. The sample was comprised of physiotherapists practicing in Italy, all other healthcare professionals were excluded.
Survey development
We adapted two previous published surveys (with permission from the authors) to develop our version for the Italian population [2, 34]. Given the different Italian socio-legal and cultural context, based on the ISH and ESH guidelines [20, 35] and the clinical recommendations by Severin et al. [1], we adapted the questionnaire on current recommendations on CVD screening by physiotherapists to investigate the Italian physiotherapists knowledge of cardiovascular assessment and interpretation of its results. The questionnaire was revised by two authors (native English and Italian, and specialized orthopedic manipulative physical therapy—OMPT--) with experience in education and research (FM and AF). Finally, it was piloted by five experienced Italian, American and Spanish physiotherapists and one physician (EG, CF, JD, GB, RS, and MG) for additional feedback on procedural and logical accuracy and fulfillment duration. The combined use of previous surveys and expert opinion provided during the piloting process strengthened the content and face validity of the survey [2, 34].
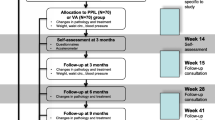
The questionnaire was divided into three sections. The first section investigated demographics, practice settings and education level. The second addressed the knowledge of current practice recommendations, cardiovascular parameters, risk factors, blood pressure measurement technique and clinical management. The last one focused on formal education and personal opinions. The survey consisted of 32 questions using a combination of close-ended (few of them with multiple selection) and Likert-scale (Additional file 1). All questions were presented in the same order and full completion was mandatory to be considered eligible.
Setting and recruitment
The web-link to the survey was distributed via mailing list of the Italian Physiotherapists Association on 23rd of March 2020. To take advantage of the forced lock-down period due to the Covid-19 pandemic and to maximize the response rate, invitations to participate were frequently re-published one per week via social media networks (Facebook, Twitter, LinkedIn, and Instagram). The survey was open for one month and the closing date was the 26th of April 2020. Consistent with previous similar survey studies, we adopted this methodological approach with the aim to collect the maximum number of answers within a given period as the majority of responses tend to occur early after posting [36,37,38]. A priori, a sample size was calculated using the e-survey Dillman’s formula with a 95% confidence level and a 5% of margin of error. At the time of the survey, the number of physiotherapists registered to the association was 7398; therefore, the required sample size for this study was 366 [39].
After reviewing the introduction (background, aims and content) participants had the opportunity to ask any questions and to provide their consent to proceed. The questionnaire could be completed on any electronic device with internet access; as Survey Monkey was used without collecting respondents’ IP addresses. The recruitment was anonymous and voluntary, but the same IP was not allowed to access to the survey more than once. The completion took approximately 10-15 minutes. No compensation or reimbursement were offered. Participants were able to provide as much information as they prefer and could stop completion of the survey at any point.
Data processing and statistical analysis
There was no hard copy of the data and no sensitive information were collected. All data were organized and analyzed in Microsoft Excel 2020. Categorical data were reported as frequencies. All graphs and tables were created using the same software. Descriptive statistics were used to describe the sample; especially, absolute frequency with its percentage was calculated for each categorical variable and mean±standard deviation (SD) was computed for answers to Likert-question.
In order to study differences among sample subgroups (OMPT qualification, patients access regimen, and years of practice) and the response to the categorical questions, a Chi squared was performed. When significant differences were detected (p<0.05), adjusted standardized residuals with Bonferroni-corrected p-values were calculated in order to identify which cells of contingency table contributed most to the significant effect [40, 41].
As the Kolmogorov-Smirnov test showed a non-normal data distribution, a Mann-Whitney test or a Kruskal-Wallis test with Bonferroni-corrected post-hoc comparisons was run for two-categories (i.e., OMPT qualification, access regimen) or five-categories subsample (i.e., years of practice), respectively, to study any difference between sample subgroups and the response to the ordinal (i.e., Likert) questions.
All statistical analyses were performed with SPSS software (SPSS. Version 20 for Windows; SPSS Inc., Chicago, IL, USA, 2004), and the level was set at p-value < 0.05 for all comparisons.
Results
Responses
Of the 764 different IP addresses that provided consent and accessed the survey, 387 completed the questionnaire (5.2%, n=387/7398). Although available for a very short period, our sample was in line with previous Italian surveys, and reached the required sample size [42,43,44].
Respondent characteristics
Around half of the participants (56%, n=220; 95%CI 51.6-61.5) possessed only bachelor degree; only 35% (n=139; 95%CI 31.0–40.5) had an OMPT qualification [38]; nearly two thirds worked in private practice (66%; n=258; 95%CI 61.6–71.0); and about half (57%, n=223; 95%CI 52.4-62.2) primarily as direct access practitioner. Twenty-seven percent (n=106; 95%CI 22.8–31.7) of respondents had been practicing for 5 to 10 years. Further demographic data are reported in Table 1.
Table 2 provide the responses of section 2 and 3 of the survey.
Knowledge, understanding and skills towards cardiovascular assessment
The majority of participants (72%, n=281; 95%CI 67.8–76.7) were not up to date with international recommendations for the assessment of cardiovascular parameters; among those who were (55%; n=58; 95%CI 45.2–64.2), the AHA guidelines was one known the best.
A great proportion of physiotherapists (80%; n=311; 95%CI 76.0–83.9) reported that they take cardiovascular parameters into account in their everyday practice; of those, 80% (n=249; 95%CI 75.6–84.5) reported measuring the HR and 86% (n=266; 95%CI 81.6–89.4) the BP. For those who did not consider them (20%; n=76; 95%CI 15.6–23.5), the most common reason was “not relevant for clinical practice” (73%; n=56; 95%CI 63.8–83.6). Smoking (86%; n=266; 95%CI 81.6–89.4) and obesity (78%; n=241; 95%CI 72.9–82.1) were the most reported risk factors. When compared against the ISH guidelines, their knowledge of normative BP values is respectively 66% (n=260; 95%CI 62.2–71.5) for normal range, 16% (n=64; 95%CI 12.8–20.1) for high-normal BP, and 12% (n=47; 95%CI 8.8–15.3) for hypertension. Note that hypertension was asked as a grouped item (i.e., not as 2 separate grades). Interestingly, 78% (n=305; 95%CI 74.3–82.5) of the respondents were aware of the HR normal value; however only 24% (n=95; 95%CI 20.2–28.7) and 26% (n=102; 95%CI 21.9–30.6) responded adequately respectively for bradycardia and tachycardia values. Only 31% (n=121; 95%CI 26.5–35.7) admitted having received adequate training in appraising cardiovascular parameters, and the majority were trained during their bachelor degree course (75%, n=91; 95%CI 67.5–82.9).
Although a moderate number considered cardiovascular parameters assessment relevant for their routine practice (mean=7.4/10 points; SD=2.1), only 50% (n=196; 95% CI 45.4 – 55.4) routinely measure BP and/or HR. Being outside physiotherapists’ scope of practice was the leading justification reported for not performing these assessments (60%, n=112; 95% CI 53.2 – 67.2).
The participants reported being skilled for both BP (“quite sure” and “sure” respectively, 52%; n=204; 95%CI 47.5–57.4, and 27%; n=104; 95%CI 22.3–31.1) and HR measurements (“quite sure” and “sure” respectively, 51%; n=199; 95%CI 46.2–56.1, and 30%; n=116; 95%CI 25.3–34.4). The majority reported being “quite sure” in interpreting and managing BP measurement (respectively, 55%; n=213; 95%CI 49.8–59.7, and 48%; n=188; 95%CI 43.4–53.3) and HR measurement (respectively, 48%; n=189; 95%CI 43.6–53.6, and 42%; n=166; 95%CI 37.8–47.6). Only 25% (n=97; 95%CI 20.6–29.2) measured BP on both arms at the initial examination, and only 46% (n=181; 95%CI 41.6–51.5) of them reported that they repeat measurements three times as recommended. Notably, of those that measure on both arms, only 46% (n=45; 95%CI 36.5–56.3) reported that they continued assessing the limb with the highest BP for future screening.
Physiotherapists’ opinion towards the relevance of the assessment for cardiovascular risk factors was scored at 4.2/10 (SD=2.3). Of the respondents, 70% (n=273; 95%CI 65.6–74.7) screened for cardiovascular risk in clinical practice, but only 33% (n=130; 95%CI 28.7–38.1) assessed their patients’ cardiovascular fitness before exercising. When this assessment is performed the tool reported being used the most is the 6 minutes walking test (66%; n=86; 95%CI 18.0–26.2). Furthermore, only 28% (n=108; 95%CI 23.3–32.2) declared to monitor BP during and/or post-exercise, and of them only 21% (n=23; 95%CI 13.6–29.0) acknowledged the most accepted values of exaggerated increases in BP in response to exercise.
Cardiovascular assessment training
Our participants considered that training in cardiovascular assessment was highly relevant for physiotherapists (mean 8.3/10; SD=1.9). Most of them (82%; n=320; 95%CI 78.5–86.1) reported that training in cardiovascular assessment should be provided during a physiotherapy degree as part of the core curriculum.
Differences between sample subgroups
The non-parametric tests did not reveal any significant differences (p>0.05) for the subgroup samples (i.e., highest earned degree, OMPT qualification, access regimen, and years of practice) (Additional file 2).
Discussion
Key findings
This is the first study which provides insights from an Italian physiotherapists cohort about their knowledge, understanding and screening behaviors in the assessment of cardiovascular parameters and risks factors. Our results highlight that cardiovascular assessment is considered relevant by 80% of physiotherapists. Fifty percent of the respondents reported that they routinely include cardiovascular assessment in their initial examination. However, given the number of professionals who work in a first contact role, it is concerning that 72.2% were not familiar to current practice recommendations and a substantial proportion were not familiar with the fundamentals of cardiovascular measurements when compared against the ISH guidelines. Clinical Practice Guidelines are paramount to implement the most updated available knowledge in clinical practice [45, 46]. Additionally, as the Italian Physiotherapy Association advocates for direct access [28,29,30], Clinical Practice Guidelines knowledge is a professional responsibility [47]. Surprisingly, 60.2% reported that cardiovascular measurements are outside their scope of practice. This finding is similar across the profession as indicated by previous studies conducted in other countries [1, 10, 34, 48]. For example, although the American Physical Therapist Association Guide to Physical Therapist Practice encourages early screening for medical conditions, including a review of the cardio-vascular/pulmonary system by measuring HR and BP [8], it was observed that only 10-15% of U.S. outpatient physiotherapists did perform a routine cardiovascular assessment because it is believed to be beyond their competence [1]. Similar findings were found in Saudi Arabia [27]. Our results highlight a large discrepancy between the number of physiotherapists that consider cardiovascular assessment and that actually do it. Even more importantly, there is a large discrepancy between those that consider cardiovascular assessment and those skilled to measure it and that understand what it means. These barriers seem to result from gaps in knowledge and policy. Changing the perception of the importance of cardiovascular assessment can be addressed through education and knowledge translation of both clinicians and students [2, 49]. Also, Institutional or professional polices can be developed to require cardiovascular assessment, thus helping to include cardiovascular assessment in clinical policies and standards [2]. Furthermore, the development of clinical practice guidelines specifically directed to physiotherapists could assist with this process by making the clinical understanding and application of cardiovascular assessment better understood in order to follow through with appropriate recommendations for education, exercise, and referrals.
Notably, most of participants from the current cohort felt confident in conducting and interpreting cardiovascular measurements. However, a very small proportion were updated on how to perform a thorough BP assessment (i.e., the average of three measurements of the arm with the highest blood pressure) and on the knowledge of the BP and HR normative values [20, 35]. The absence of significant differences between groups (e.g., possessing a specialization or working in a direct access setting) suggests that this inadequacy is homogeneously distributed across the profession. This may reflect the absence of Italian recommendations for the best practice on the subject.
As physiotherapy practice advances to a more independent care model [31], the screening for cardiovascular risk factors and related serious pathologies become of paramount importance to ensure patient safety and effective medical management [20]. This becomes even more relevant in light of the alarming number of CVD-related deaths [50]. Given that hypertension is frequently asymptomatic, even at critical high values (SBP 180 mm/Hg - DBP 120 mm/Hg), its early detection is fundamental for a prompt medical treatment and associated reduction of mortality and morbidity [7]. Physiotherapists, as first contact health-care professionals, especially when working in a direct access setting, could ensure timely medical referral for further investigations through an accurate screening [1].
Furthermore, commonly treated musculoskeletal presentations such as neck pain, could potentially hide more serious pathologies related to the cardiovascular system [51,52,53]. That is, HBP and elevated HR are relevant in the pathogenesis of either an aneurysm or a vascular stenosis that underlie a spontaneous cervical artery dissection in older adults, and are important predictors to inform for any acute damage/trauma of cervical arteries in younger population [54, 55]. Also, It has been reported that some patients with neck disorders who underwent cervical traction may experience a significant drop in their HR and BP resulting from temporary alteration of the autonomic nervous system processes [56]. These temporary responses to very commonly utilized musculoskeletal treatments, in highly predisposed subjects (e.g., elderly patients or patients undertaking medications, such as non-steroidal anti-inflammatory or corticosteroids drugs), may increase the risk of falling, which could result in serious and potentially fatal complications. This emphasizes the importance of physiotherapists possessing strong knowledge of the cardiovascular system and routinely implementing CVD assessment during their daily practice irrespective of the work setting. Patients can be seen by a physiotherapist for a wide range of different disorders—back pain, knee pain, mobility issues, etc.— while, in the meantime, being managed by medical doctors for other comorbidities [57, 58]. Sixty-two percent of patients who attended an orthopedic or a direct access physiotherapy consultation also had a clinical history of cardiovascular disease [4]. Twenty-one percent of U.S. adults aged >35 years with a diagnosis of osteoarthritis also have hypertension, smoking habit and diabetes with a prevalence of 40%, 20% and 11% respectively [59]. The belief that cardiovascular screening does not apply to all physiotherapists does not truly reflect the role of a profession, which plays a pivotal role in both primary and secondary care in promoting an healthy lifestyle especially when battling physical inactivity [11, 60].
Physical inactivity alongside increasing time of sedentary behavior can have, in isolation or combination, a repercussion on the cardiovascular system with an increased disease incidence and deaths [48]. This tendency of sedentary behavior has been recently amplified by the recent Covid-19 pandemic [61, 62]. Alongside the advice of sitting less and being more physically active, the introduction of a light or moderate-vigorous intensity exercise routine has shown to be as an effective strategy to reduce the number of the aforementioned cardiovascular deaths and cardiometabolic risk factors [63,64,65,66]. Regular exercise does not only lower/optimize BP values [67] but it is also recommended as a first-line treatment for numerous musculoskeletal disorders and in the management of chronic pain [68,69,70]. Furthermore, the American College of Cardiology and the American College of Sports Medicine guidelines recommend regular exposure to physical activity for a period of up to 6 months before considering any pharmacological treatment, for the management of BP in low-risk category (10-year CVD risk <10%) adults with stage 1 hypertension (BP 130-139/80-89 mmHg) [71, 72].
Despite the benefits of physical activity being well known, a review of the cardiovascular system is essential before prescribing any exercise. Exercise induced hypertension (namely, exaggerated BP) has been shown to increase the risk of cardiovascular events by 1.4-3 times. Further, the risk of an exercise induced acute heart attack is seven times more likely compared to a sudden cardiac death at rest [73,74,75]. Hypertension is associated with a rise in cardiac infarcts and arrhythmias, which are the two major causes of sudden cardiac death during exercise among individuals aged >35 years [76,77,78]. Physiotherapists are uniquely positioned to screen exaggerated BP responses to physical activity and MH because exercise is an important part of physiotherapy treatment sessions. Although too little considered in our cohort, BP measurement during and after exercises plays a fundamental preventative role being able to unmask BP abnormalities in individuals with MH even during low intensity exercises [1, 79, 80]. Furthermore, an abnormal low BP response to exercise is prognostically associated with cardiovascular events and mortality regardless of exercise intensity [81]. A decrease in SBP ≥ 10 mmHg accompanied by evidence of ischemia during exercise is an absolute indication to stop all exercise [82]. Also, a decrease in BP during exercise or an increase >20-30 mmHg may indicate multiple underlying pathologies, such as myocardial ischemia [82]. Our results are in line with a previous survey which found that only 12% and 35% of U.S. physiotherapists reported monitoring BP, respectively, during and following exercises [2].
In our study, only 27.8% reported to measure BP prior, during, and/or post-exercise; 21.3% of them understood the concept of exaggerated BP values during or post exercise. As physiotherapists often prescribe exercise as part of a plan of care and decide on the intensity and type of exercise, it is imperative that physiotherapists monitor BP exercise response during their treatments for safety reasons. Obtaining information on the cardiovascular system status allows the physiotherapists to monitor normal and abnormal physiological responses to the exercise [83]. This type of screening would have the benefits of uncovering potential hidden risk factors, detecting already established CVD and triggering a timely onward referral. This would also allow a more tailored exercise prescription in order reduce the occurrence of adverse events and sudden deaths [1].
Recommendations for clinical practice
This study has revealed an inadequate level of knowledge among Italian physiotherapists regarding cardiovascular assessment and screening. This discrepancy appears to be driven by the belief that it is not part of their professional role and does not influence their clinical practice and decision-making process. Given the increasing incidence of CVD in the general population, we strongly advise physiotherapists to perform a screening of the cardiovascular system for all patients. Specifically, BP and HR measurements must be routinely taken and documented. Despite the perceived importance of training on this topic by our cohort, training in this area needs to be strengthened to guarantee the correct identification of risk factors, recognition of red-flags, onward medical referral and, above all, patient safety. Our results show that Italian physiotherapists are still lacking specific training on this topic and how this affects their clinical decision-making process.
Further studies are needed to investigate whether differences in cardiovascular screening among physiotherapists exist depending on the work setting and how this may affect clinical practice when patients are affected by either musculoskeletal or other age-related degenerative diseases. More studies in other countries and/or based on different socio-legal background are also welcomed in order to allow a generalization of results.
Given the absence of Italian guidelines, we have produced and implemented in the article three infographics for public use, which have the dual objective of raising awareness among Italian physiotherapists and provides practical resources for everyday practice [84]. Two infographics explain the correct procedure for measuring the parameters both at rest and during exercises (Additional file 3 and 4). Also, an adjunctive infographic provides a decision tool for early identification of potential cardiovascular adverse events (Additional file 5).
Strengths and limitations
This is the first published study conducted in Europe which describes the current knowledge and ability of physiotherapists to conduct cardiovascular assessment. The methodology used and the adaptation of previous online surveys to collect the opinion of Italian physiotherapists allowed us to successfully capture the perspective of the target population. Although we obtained the required sample size calculation, this study present limitation in the generalization on the results. Where the purpose of a study is to gain a general sense of a belief or attitude, a lower level of precision may be acceptable, and then a smaller sample size may be drawn [39]. The small response rate of our study could challenge our results in representing the target population and the generalisability of the results. We did not send personal invitations, and this may explain the low number of completed surveys. The survey completion could have also been influenced by the very detailed and specific questions that were employed. There is also a high potential for responder bias as those with stronger positive or negative opinion on the topic may be more likely to respond to the survey, or to give more detail. The used methodology may have potentially led to a selection bias. Additionally, similar to previous studies [2, 34], although the survey underwent a rigorous piloting and development process that involved a representative piloting group of European physiotherapists and physicians, the reliability of the survey was not quantified.
Conclusions
Our study revealed that a concerning proportion of Italian physiotherapists, even those working as first line practitioners, are not trained to the fundamentals of and do not perform properly cardiovascular assessment. This appears to be driven by the belief that it is not part of their professional scope of practice. This lack of knowledge is present across the profession and having a specialized post-graduate training does not guarantee the achievement of the required competence. All the above may impact on appropriate triage and management and in some cases have the potential to negatively impact both patient and practitioner. We strongly encourage Italian public administrators and national council representatives to utilize our study as a starting point for the implementation of a stronger cardiovascular screening competencies framework within the Italian physiotherapy core curriculum.
Availability of data and materials
The datasets generated and/or analysed during the current study are available and provided are as a supplementary file.
Abbreviations
- CVD:
-
Cardiovascular disease
- BP:
-
Blood pressure
- HR:
-
Heart rate
- HBP:
-
High blood pressure
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- ISH:
-
International society of Hypertension
- ESH:
-
European society of Hypertension
- AHA:
-
American Heart Association
- OMPT:
-
Orthopedic manipulative physical therapy
References
Severin R, Sabbahi A, Albarrati A, Phillips SA, Arena S. Blood pressure screening by outpatient physical therapists: a call to action and clinical recommendations. Phys Ther. 2020;100:1008–19.
Severin R, Wang E, Wielechowski A, Phillips SA. Outpatient physical therapist attitudes toward and behaviors in cardiovascular disease screening: a national survey. Phys Ther. 2019;99:833–48.
Leino-Arjas P, Solovieva S, Kirjonen J, Reunanen A, Riihimaki H. Cardiovascular risk factors and low-back pain in a long-term follow-up of industrial employees. Scand J Work Environ Health. 2006;32:12–9.
Fernandes GS, Valdes AM. Cardiovascular disease and osteoarthritis: common pathways and patient outcomes. Eur J Clin Invest. 2015;45:405–14.
Feller D, Giudice A, Faletra A, Salomon M, Galeno E, Rossettini G, et al. Identifying peripheral arterial diseases or flow limitations of the lower limb: Important aspects for cardiovascular screening for referral in physiotherapy. Musculoskelet Sci Pract. 2022;61:102611.
Jones NR, McCormack T, Constanti M, McManus RJ. Diagnosis and management of hypertension in adults: NICE guideline update 2019. Br J Gen Pract. 2020;70:90–1.
Kessler CS, Joudeh Y. Evaluation and treatment of severe asymptomatic hypertension. Am Fam Physician. 2010;81:470–6.
American Physical Therapy A. Guide to physical therapist practice. second edition. american physical therapy association. Phys Ther. 2001;81:9–746.
Black B, Ingman M, Janes J. Physical therapists’ role in health promotion as perceived by the patient: descriptive survey. Phys Ther. 2016;96:1588–96.
Black B, Marcoux BC, Stiller C, Qu X, Gellish R. Personal health behaviors and role-modeling attitudes of physical therapists and physical therapist students: a cross-sectional study. Phys Ther. 2012;92:1419–36.
Frerichs W, Kaltenbacher E, van de Leur JP, Dean E. Can physical therapists counsel patients with lifestyle-related health conditions effectively? A systematic review and implications. Physiother Theory Pract. 2012;28:571–87.
Scherer S. Addressing cardiovascular risk as part of physical therapist practice-what about practice recommendations for physical therapists? Cardiopulm Phys Ther J. 2009;20:27–9.
Fleming S, Atherton H, McCartney D, Hodgkinson J, Greenfield S, Hobbs FD, et al. Self-screening and non-physician screening for hypertension in communities: a systematic review. Am J Hypertens. 2015;28:1316–24.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the american heart association. Circulation. 2017;135:e146–603.
Bromfield SG, Shimbo D, Booth JN 3rd, Correa A, Ogedegbe G, Carson AP, et al. Cardiovascular risk factors and masked hypertension: the jackson heart study. Hypertension. 2016;68:1475–82.
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Forouzanfar MH, Liu P, Roth GA, Ng M, Biryukov S, Marczak L, et al. Global burden of hypertension and systolic blood pressure of at least 110 to 115 mm Hg, 1990-2015. JAMA. 2017;317:165–82.
Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2018;71:e127–248.
Community Preventive Services Task F. Team-based care to improve blood pressure control: recommendation of the Community Preventive Services Task Force. Am J Prev Med. 2014;47:100–2.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334–57.
O'Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–68.
Peacock J, Diaz KM, Viera AJ, Schwartz JE, Shimbo D. Unmasking masked hypertension: prevalence, clinical implications, diagnosis, correlates and future directions. J Hum Hypertens. 2014;28:521–8.
Kayrak M, Bacaksiz A, Vatankulu MA, Ayhan SS, Kaya Z, Ari H, et al. Exaggerated blood pressure response to exercise--a new portent of masked hypertension. Clin Exp Hypertens. 2010;32:560–8.
Schultz MG, Otahal P, Cleland VJ, Blizzard L, Marwick TH, Sharman JE. Exercise-induced hypertension, cardiovascular events, and mortality in patients undergoing exercise stress testing: a systematic review and meta-analysis. Am J Hypertens. 2013;26:357–66.
Currie KD, Floras JS, La Gerche A, Goodman JM. Exercise Blood Pressure Guidelines: Time to Re-evaluate What is Normal and Exaggerated? Sports Med. 2018;48:1763–71.
Zhang D, Shen X, Qi X. Resting heart rate and all-cause and cardiovascular mortality in the general population: a meta-analysis. CMAJ. 2016;188:E53–63.
Albarrati Am Pt P. Outpatient physical therapy cardiovascular assessment: Physical therapist perspective and experience. Physiother Theory Pract. 2019;35:843–50.
FIsioterapisti AI. Policy Statement AIFI Accesso al Fisioterapista; 2017.
Maselli F, Piano L, Cecchetto S, Storari L, Rossettini G, Mourad F. Reply to Moretti et al. would moving forward mean going back? comment on Maselli et al. direct access to physical therapy: should italy move forward? Int J Environ Res Public Health. 2022;19:555.
Maselli F, Piano L, Cecchetto S, Storari L, Rossettini G, Mourad F. Direct access to physical therapy: should italy move forward? Int J Environ Res Public Health. 2022;19(1):555.
Physiotehrapy W. Direct access and patient/client self-referral to physical therapy; 2019.
Eysenbach G. Improving the quality of Web surveys: the Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6:e34.
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
Frese EM, Richter RR, Burlis TV. Self-reported measurement of heart rate and blood pressure in patients by physical therapy clinical instructors. Phys Ther. 2002;82:1192–200.
Stergiou GS, Palatini P, Parati G, O'Brien E, Januszewicz A, Lurbe E, et al. European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens. 2021;39:1293–302.
Bury J, Littlewood C. Rotator cuff disorders: a survey of current (2016) UK physiotherapy practice. Shoulder Elbow. 2018;10:52–61.
Littlewood C, Bateman M. Rehabilitation following rotator cuff repair: a survey of current UK practice. Shoulder Elbow. 2015;7:193–204.
Smythe A, White J, Littlewood C, Bury J, Haines T, Malliaras P. Physiotherapists deliver management broadly consistent with recommended practice in rotator cuff tendinopathy: An observational study. Musculoskelet Sci Pract. 2020;47:102132.
Dillman D. Mail and Internet Surveys: the Tailored Design Method — 2007 Update with New Internet, Visual, and Mixed-Mode Guide. 2nd ed. New Jersey: John Wiley & Sons; 2011.
Beasley TM, Schumacker RE. Multiple Regression Approach to Analyzing Contingency Tables: Post Hoc and Planned Comparison Procedures. J Exp Educ. 1995;64:79–93.
García-pérez MA, Núñez-antón V. Cellwise Residual Analysis in Two-Way Contingency Tables. Educ Psychol Measure. 2016;63:825–39.
Brindisino F, Ristori D, Lorusso M, Miele S, Pellicciari L, Rossettini G, et al. Subacromial impingement syndrome: a survey of Italian physiotherapists and orthopaedics on diagnostic strategies and management modalities. Arch Physiother. 2020;10:16.
Rossettini G, Palese A, Geri T, Fiorio M, Colloca L, Testa M. Physical therapists’ perspectives on using contextual factors in clinical practice: Findings from an Italian national survey. Plos One. 2018;13:e0208159.
Mourad F, Lopez G, Cataldi F, Maselli F, Pellicciari L, Salomon M, et al. Assessing Cranial Nerves in Physical Therapy Practice: Findings from a Cross-Sectional Survey and Implication for Clinical Practice. Healthcare (Basel). 2021;9(10):1262.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–646.
O'Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, et al. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens. 2003;21:821–48.
Disposizioni in materia di sicurezza delle cure e della persona assistita, nonché in materia di responsabilità professionale degli esercenti le professioni sanitarie https://www.gazzettaufficiale.it/eli/id/2017/03/17/17G00041/sg.
Scherer SA, Noteboom JT, Flynn TW. Cardiovascular assessment in the orthopaedic practice setting. J Orthop Sports Phys Ther. 2005;35:730–7.
Tunnecliff J, Weiner J, Gaida JE, Keating JL, Morgan P, Ilic D, et al. Translating evidence to practice in the health professions: a randomized trial of Twitter vs Facebook. J Am Med Inform Assoc. 2017;24:403–8.
Bromfield S, Muntner P. High blood pressure: the leading global burden of disease risk factor and the need for worldwide prevention programs. Curr Hypertens Rep. 2013;15:134–6.
Hutting N, Kerry R, Kranenburg R, Mourad F, Taylor A. Assessing vascular function in patients with neck pain, headache, and/or orofacial pain: part of the job description of all physical therapists. J Orthop Sports Phys Ther. 2021;51:418–21.
Mourad F, Giovannico G, Maselli F, Bonetti F, de las Penas Fernandez C, Dunning J. Basilar impression presenting as intermittent mechanical neck pain: a rare case report. BMC Musculoskelet Disord. 2016;17:7.
Mourad F, Cataldi F, Patuzzo A, Tunnera S, Dunning J, Fernandez-de-Las-Penas C, et al. Craniopharyngioma in a young woman with symptoms presenting as mechanical neck pain associated with cervicogenic headache: a case report. Physiother Theory Pract. 2021;37:549–58.
Arnold M, Bousser MG, Fahrni G, Fischer U, Georgiadis D, Gandjour J, et al. Vertebral artery dissection: presenting findings and predictors of outcome. Stroke. 2006;37:2499–503.
Taylor A, Mourad F, Kerry R, Hutting N. A guide to cranial nerve testing for musculoskeletal clinicians. J Man Manip Ther. 2021;29:376–89.
Frese EM, Fick A, Sadowsky HS. Blood pressure measurement guidelines for physical therapists. Cardiopulm Phys Ther J. 2011;22:5–12.
Boissonnault WG. Prevalence of comorbid conditions, surgeries, and medication use in a physical therapy outpatient population: a multicentered study. J Orthop Sports Phys Ther. 1999;29:506–19 discussion 520-505.
Muckelt PE, Roos EM, Stokes M, McDonough S, Gronne DT, Ewings S, et al. Comorbidities and their link with individual health status: A cross-sectional analysis of 23,892 people with knee and hip osteoarthritis from primary care. J Comorb. 2020;10:2235042X20920456.
Singh G, Miller JD, Lee FH, Pettitt D, Russell MW. Prevalence of cardiovascular disease risk factors among US adults with self-reported osteoarthritis: data from the Third National Health and Nutrition Examination Survey. Am J Manag Care. 2002;8(15 Suppl):S383-91.
Shirley D, van der Ploeg HP, Bauman AE. Physical activity promotion in the physical therapy setting: perspectives from practitioners and students. Phys Ther. 2010;90:1311–22.
Meyer J, McDowell C, Lansing J, Brower C, Smith L, Tully M, et al. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US Adults. Int J Environ Res Public Health. 2020;17(18):6469.
Castaneda-Babarro A, Arbillaga-Etxarri A, Gutierrez-Santamaria B, Coca A. Physical activity change during COVID-19 confinement. Int J Environ Res Public Health. 2020;17(18):6878.
Del Pozo-Cruz J, Garcia-Hermoso A, Alfonso-Rosa RM, Alvarez-Barbosa F, Owen N, Chastin S, et al. Replacing sedentary time: meta-analysis of objective-assessment studies. Am J Prev Med. 2018;55:395–402.
Matthews CE, Moore SC, Sampson J, Blair A, Xiao Q, Keadle SK, et al. Mortality benefits for replacing sitting time with different physical activities. Med Sci Sports Exerc. 2015;47:1833–40.
Rees-Punia E, Evans EM, Schmidt MD, Gay JL, Matthews CE, Gapstur SM, et al. Mortality risk reductions for replacing sedentary time with physical activities. Am J Prev Med. 2019;56:736–41.
Schmid D, Ricci C, Baumeister SE, Leitzmann MF. Replacing sedentary time with physical activity in relation to mortality. Med Sci Sports Exerc. 2016;48:1312–9.
Dempsey PC, Sacre JW, Larsen RN, Straznicky NE, Sethi P, Cohen ND, et al. Interrupting prolonged sitting with brief bouts of light walking or simple resistance activities reduces resting blood pressure and plasma noradrenaline in type 2 diabetes. J Hypertens. 2016;34:2376–82.
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, et al. What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med. 2020;54:79–86.
Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, Bierma-Zeinstra SMA, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis Cartil. 2019;27:1578–89.
Babatunde OO, Jordan JL, Van der Windt DA, Hill JC, Foster NE, Protheroe J. Effective treatment options for musculoskeletal pain in primary care: a systematic overview of current evidence. Plos One. 2017;12:e0178621.
Medicine ACoS. ACSM's Guidelines for Exercise Testing and Prescription. 10th ed. Philadelphia: Wolters Kluwer; 2018.
Goetsch MR, Tumarkin E, Blumenthal RS, Whelton SP. New guidance on blood pressure management in low-risk adults with stage 1 hypertension. Am Coll Cardiol. 2021. https://www.acc.org/latest-in-cardiology/articles/2021/06/21/13/05/new-guidance-on-bp-management-in-low-riskadults-with-stage-1-htn.
Oja P, Titze S, Kokko S, Kujala UM, Heinonen A, Kelly P, et al. Health benefits of different sport disciplines for adults: systematic review of observational and intervention studies with meta-analysis. Br J Sports Med. 2015;49:434–40.
Khan KM, Thompson AM, Blair SN, Sallis JF, Powell KE, Bull FC, et al. Sport and exercise as contributors to the health of nations. Lancet. 2012;380:59–64.
Keller K, Stelzer K, Ostad MA, Post F. Impact of exaggerated blood pressure response in normotensive individuals on future hypertension and prognosis: systematic review according to PRISMA guideline. Adv Med Sci. 2017;62:317–29.
Ghali JK, Kadakia S, Cooper RS, Liao YL. Impact of left ventricular hypertrophy on ventricular arrhythmias in the absence of coronary artery disease. J Am Coll Cardiol. 1991;17:1277–82.
Jouven X, Desnos M, Guerot C, Ducimetiere P. Predicting sudden death in the population: the Paris Prospective Study I. Circulation. 1999;99:1978–83.
Risgaard B, Winkel BG, Jabbari R, Glinge C, Ingemann-Hansen O, Thomsen JL, et al. Sports-related sudden cardiac death in a competitive and a noncompetitive athlete population aged 12 to 49 years: data from an unselected nationwide study in Denmark. Heart Rhythm. 2014;11:1673–81.
Sharman JE, LaGerche A. Exercise blood pressure: clinical relevance and correct measurement. J Hum Hypertens. 2015;29:351–8.
Schultz MG, Hare JL, Marwick TH, Stowasser M, Sharman JE. Masked hypertension is “unmasked” by low-intensity exercise blood pressure. Blood Press. 2011;20:284–9.
Barlow PA, Otahal P, Schultz MG, Shing CM, Sharman JE. Low exercise blood pressure and risk of cardiovascular events and all-cause mortality: systematic review and meta-analysis. Atherosclerosis. 2014;237:13–22.
Fletcher GF, Ades PA, Kligfield P, Arena R, Balady GJ, Bittner VA, et al. Exercise standards for testing and training: a scientific statement from the American Heart Association. Circulation. 2013;128:873–934.
Miyai N, Arita M, Miyashita K, Morioka I, Shiraishi T, Nishio I. Blood pressure response to heart rate during exercise test and risk of future hypertension. Hypertension. 2002;39:761–6.
Mourad F, Patuzzo A, Tenci A, Turcato G, Faletra A, Valdifiori G, et al. Management of whiplash-associated disorder in the Italian emergency department: the feasibility of an evidence-based continuous professional development course provided by physiotherapists. Disabil Rehabil. 2022;44:2123–30.
Acknowledgments
Not applicable.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FMo conceived the study and was responsible for the project administration. AF, FMo, FMa, and GB designed the study. FMo, FMa, AF and GB developed the survey tool. LP, FMo and GB analyzed the data. All authors overviewed data analysis and interpretation. AF and GB wrote the first draft of the paper. JD, GR, CFDL, FB, EG and RS reviewed and wrote the second draft. FMo, AF and GB were major contributors in writing (original draft). FMo review and completed the final version of the paper. All authors contributed to the investigation and to the writing (review and editing). LP contributed to data curation and formal analysis. FMo is the guarantor. All authors provided final approval of the version to be submitted.
Corresponding author
Ethics declarations
Competing interest
There is no conflict of interest or competing interest to declare.
Ethics approval and consent to participate
This study was approved by the Human Subjects Committee of the Department of Physical Therapy, Occupational Therapy, Rehabilitation and Physical Medicine, Universidad Rey Juan Carlos of Madrid with approval letter URJC – DPTO 55 – 2019. The authors followed the principles outlined in the Declaration of Helsinki for this study. Participants provide written informed consent electronically before proceeding with the questionnaire.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Survey developed based on recent scientific publications and adapted to the Italian socio-economic and cultural context.
Additional file 2.
Results of the non-parametric test to identify any significant difference in responses between subgroups of the sample.
Additional file 3.
Blood pressure screening in physiotherapy practice.
Additional file 4.
Blood pressure screening during exercise in physiotherapy practice.
Additional file 5.
Decision tool for early identification of potential cardiovascular adverse event.
Additional file 6.
Raw dataset.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Faletra, A., Bellin, G., Dunning, J. et al. Assessing cardiovascular parameters and risk factors in physical therapy practice: findings from a cross-sectional national survey and implication for clinical practice. BMC Musculoskelet Disord 23, 749 (2022). https://doi.org/10.1186/s12891-022-05696-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05696-w