Abstract
Background
Pelvic fractures are often associated with spine injury in polytrauma patients. This study aimed to determine whether concomitant spine injury influence the surgical outcome of pelvic fracture.
Methods
We performed a retrospective analysis of data of patients registered in the German Pelvic Registry between January 2003 and December 2017. Clinical characteristics, surgical parameters, and outcomes were compared between patients with isolated pelvic fracture (group A) and patients with pelvic fracture plus spine injury (group B). We also compared apart patients with isolated acetabular fracture (group C) versus patients with acetabular fracture plus spine injury (group D).
Results
Surgery for pelvic fracture was significantly more common in group B than in group A (38.3% vs. 36.6%; p = 0.0002), as also emergency pelvic stabilizations (9.5% vs. 6.7%; p < 0.0001). The mean time to emergency stabilization was longer in group B (137 ± 106 min vs. 113 ± 97 min; p < 0.0001), as well as the mean time until definitive stabilization of the pelvic fracture (7.3 ± 4 days vs. 5.4 ± 8.0 days; p = 0.147). The mean duration of treatment and the morbidity and mortality rates were all significantly higher in group B (p < 0.0001). Operation time was significantly shorter in group C than in group D (176 ± 81 min vs. 203 ± 119 min, p < 0.0001). Intraoperative blood loss was not significantly different between the two groups with acetabular injuries. Although preoperative acetabular fracture dislocation was slightly less common in group D, postoperative fracture dislocation was slightly more common. The distribution of Matta grades was significantly different between the two groups. Patients with isolated acetabular injuries were significantly less likely to have neurological deficit at discharge (94.5%; p < 0.0001). In-hospital complications were more common in patients with combined spine plus pelvic injuries (groups B and D) than in patients with isolated pelvic and acetabular injury (groups A and C).
Conclusions
Delaying definitive surgical treatment of pelvic fractures due to spinal cord injury appears to have a negative impact on the outcome of pelvic fractures, especially on the quality of reduction of acetabular fractures.
Similar content being viewed by others
Introduction
In the case of a polytrauma patient, all possibly life-threatening injuries must be identified and treated as quickly as possible. Spinal cord injury should always be considered in patients with multiple injuries, even if no neurological deficit is present [1]. About 5% of polytrauma patients with pelvic and/or acetabular fracture will have spinal injury [29, 42]. Pelvic fractures as well as spine injuries occur generally in road traffic accidents or falls from heights, and the combination of both injuries can be life-threatening due to the force exerted to cause these injuries [18, 54]. Approximately 55% of spinal cord injuries occur in the cervical region, 15% in the thoracic region, 15% in the thoracolumbar junction, and 15% in the lumbosacral region. Up to 10% of patients with a cervical spine fracture will have a second, non-contiguous spine fracture [1, 13].
Due to the complex anatomy of the pelvis, pelvic fractures are often divided into pelvic ring fractures and acetabular fractures, as depending on the area of injury the surrounding tissues play an important role in concomitant injuries. Due to these characteristics and how scarcity these are, the treatment of such fractures depends on a certain degree of surgical expertise.
The most favorable time for osteosynthetic stabilization—performed to restore the pelvic ring stability and/or anatomic acetabular restoration—is determined by the gravity of adjuvant injuries and hemodynamic stability.
The stability of the pelvic ring is graded using the Tile classification, for which the integrity of the posterior pelvic ring dictates the stability grade of the entire pelvic ring [34]. Tile A lesions can be managed conservatively, but Tile B or C lesions will require surgical stabilization, usually by percutaneous insertion of sacroiliac screws for the posterior pelvic ring [10, 21]. In some cases, open reduction and internal fixation (ORIF) for the anterior pelvic ring may be required; however, an important requisite for ORIF is a hemodynamically stable patient. A supraacetabular external fixator is sometimes used for temporary or definitive treatment of the anterior pelvic ring injuries [43, 44].
In acetabular fractures, the essential objective of treatment is anatomical restoration of the joint line to avoid development of post-traumatic osteoarthritis.
ORIF is the gold standard treatment for displaced acetabular fractures. The quality of reduction achieved is recorded by the Matta grading score, which describes the postoperative step-off in the joint in Grade 1 (anatomical reconstruction: < 2 mm), Grade 2 (imperfect reduction: 2 – 3 mm), and Grade 3 (poor reduction > 3 mm) [3, 19, 28, 37, 48].
In patients with combined pelvic fracture and spine injury, treatment of the pelvic fracture is often delayed until the life-threatening spine injury has been dealt with, but whether this results in worse postoperative outcome of the pelvic fracture is not known [33, 41, 42]. The aim of this multicenter cohort study was to investigate how the postoperative outcome, follow-up and surgical treatment are influenced with a concomitant spine injury.
Our primary hypothesis was that an associated spine injury leads to delayed definitive surgical treatment of the pelvic fracture and that this unfavorably affects reduction quality of acetabular fractures.
Patients and methods
The Working Group Pelvis (AG Becken) of the German Society for Traumatology (Deutsche Gesellschaft für Unfallchirurgie) established a multicenter prospective registry in 1991 to improve the quality of care for pelvic and acetabular injuries. The Pelvic III Working Group prospectively records all pelvic and acetabular fractures in the participating hospitals (currently, 39 hospitals) [7, 8, 26]. The database is maintained since 2018 by the AUC GmbH (Academy of Trauma Surgery [Akademie der Unfallchirurgie]) with the sponsoring of the German Society for Traumatology and the Data used were collected in Bern, Switzerland by MEMdoc (medical Registries and Data Linkage). The German Pelvic Registry (GPR) has been approved by the Ethics Committee of the Chamber of Physicians of the Federal State of Saarland (No. 29/14). Inclusion criteria for the registry are pelvic ring and/or acetabular fracture and informed consent. Follow-up is determined for each patient individually conform to the duration of stationary treatment for the pelvic injury. The data of 16.359 patients with pelvic fractures were recorded correctly and entirely in the GPR from January 2003 to December 2017. These included 4.547 (27.8%) with acetabular fracture. We identified those with and without associated spine injury. In the GPR, spine injury is defined based on the criteria of the Injury Severity Scores (ISS) as an Abbreviated Injury Score (AIS Spine) > 0 for each spine segment (cervical, thoracic and lumbar) [22]. The data of the patients were extracted for retrospective analysis.
The Ethics Committee of the Eberhard-Karls-University in Tübingen, Germany, approved this cohort study (No. 968/2018BO2).
Evaluated parameters
The following parameters were analyzed:
-
Age
-
Gender
-
Injury Severity Score (ISS)
-
Hemoglobin level (Hb) at admission
-
Systolic blood pressure (SBP) at admission
-
Number of emergency stabilizations
-
Number of definitive surgical stabilizations
-
Time until emergency fracture stabilization (in minutes)
-
Time until definitive stabilization (in days)
-
Length of hospital stay (in days)
-
Overall complication rate (except osteosynthesis-associated complications)
-
Rate of osteosynthesis-associated complications
-
Mortality
The following complications were evaluated:
-
Hemorrhagic events
-
Thromboembolic events
-
Surgical site infection (superficial and deep)
-
Fracture-associated neurologic complications (preoperatively existing)
-
Iatrogenic neurologic complication
-
Pulmonary complications
-
Cardiac complications
-
Multiorgan failure
The following complications associated with osteosynthesis were evaluated:
-
Implant loosening
-
Implant failure
-
Secondary displacement of the fracture after definitive surgical fixation
To evaluate the quality of surgery in the acetabular fractures subgroup, the following surgical parameters were evaluated, focusing on the quality of the postoperative reposition:
-
Lenght of surgery (minutes)
-
Blood loss (milliliters)
-
Preoperative maximal fracture step-off (millimeters)
-
Postoperative maximal fracture step-off (millimeters)
-
Reduction quality based on Matta classification
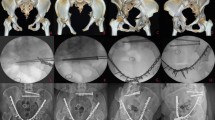
Pre- and postoperative fracture step-offs were measured on pelvic radiographs (including oblique/iliac views) or CT scans by surgeons experienced in acetabular injuries. The maximum step-offs were recorded into the database.
Statistical analysis
Normally distributed data were expressed as means ± standard deviation, and non-normally distributed data as medians (range). Differences between group median values were analyzed using ANOVA with the Bonferroni and Tukey correction, as well as t-test and chi-square test. A p value < 0.05 was accepted as statistically significant. Data collection and tabulation were performed using Microsoft Excel.
Statistical analysis was performed using SPSS Statistics® (SPSS GmbH, Munich), with the help of Prof. Dr. Wolf-Dieter Heller (KIT Karlsruhe Institute of Technology).
Results
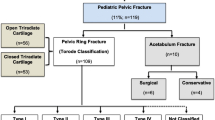
Of the 16.359 patients with pelvic fracture, 5. 927 (36.2%) had associated non-spinal injuries and so were excluded. Among the remaining patients, 8. 151 (49.8%, group A) had isolated pelvic ring and/or acetabular fracture and 2. 281 (13.6%, group B) had pelvic ring and/or acetabular fracture plus spine injury (Fig. 1).
Of the 4. 547 patients with acetabular fractures, 2.558 (56.3%) had associated non-spinal injuries and so were excluded from the analysis. While 1.370 (30.1%; group C) had isolated acetabular fracture, 619 (13.6%; group D) had acetabular fracture plus spine injury (Fig. 2).
Basic data and fracture distribution
Mean age was significantly lower and ISS significantly higher in group B than in group A (p < 0.0001 for both). Pelvic ring fractures were the most common fracture type, being present in 73% of the total cohort. The dispersion of fracture types (isolated pelvic ring fracture, isolated acetabular fracture, or combined pelvic ring and acetabular fracture) was comparable in the two groups. Nevertheless, the proportion of unstable pelvic ring fractures (Tile B or C) was significantly lower in group A than in group B (55% vs. 92%, p < 0.0001; Table 1).
Concerning to the hemodynamic status of patients at the hospital admission, only data for 49 patients in group A and for 353 patients in group B were available and valid. Hemodynamic instability (Hb < 8.0 g/dL and/or SBP < 100 mm Hg) was significantly more common in group B patients than in group A patients (56% vs. 15%, p < 0.0001). Surgery for pelvic injury was performed more often in group B than in group A (38.3% vs. 36.6%; p = 0.0002), as also emergency pelvic stabilizations (9.5% vs. 6.7%; p = 0.176). The mean time until emergency stabilization was longer in group B (137 ± 106 min vs. 113 ± 97 min; p < 0.0001), as well as the mean time until definitive stabilization of the pelvic fracture (7.3 ± 4 days vs. 5.4 ± 8.0 days; p = 0.147). The mean duration of treatment and the morbidity and mortality were all significantly higher in group B than in group A (p < 0.0001; Table 2).
Quality of surgery in acetabular fractures
Operation time was significantly shorter in group C than in group D (176 ± 81 min vs. 203 ± 119 min, p < 0.0001), but intraoperative blood loss was not significantly different between the two groups. Although preoperative fracture dislocation was slightly less common in group D, postoperative fracture dislocation was slightly more common. The distribution of Matta grades was significantly different between the two groups (Table 3).
Spinal injury
Of the 2.224 patients in group B, 380 (17%) had isolated cervical spine injury, 680 (31%) had isolated thoracic spine injury, and 1.224 (52%) had isolated lumbar spine injury. While 84 patients had combined cervical and thoracic spine injuries, 103 had combined cervical and lumbar spine injuries, and 340 had combined thoracic and lumbar spine injuries. A total of 479 patients had injury of all three spinal segments (cervical, thoracic, and lumbar).
Neurological deficits and other complications
Respecting the neurological disability of the patients at admission within the groups, the patients with isolated acetabular injuries present a significantly lower neurological disability at discharge (94.5%; p < 0.0001). Compared to the other groups, it was a significantly higher neurological disability at discharge (group B: 843 vs. 862 patients; group C: 74 vs. 99 patients; group D: 270 vs. 280 patients; p < 0.0001). Complications were more common in patients with spine plus pelvic injuries (groups B and D) than in patients with isolated pelvic injury (groups A and C) (Table 4).
Discussion
In this study, we evaluated the operative and clinical outcomes between patients with pelvic fractures and patients with a combined spine/pelvic injuries in retrospectively collected cohort data from the GPR. We identified a significant association between pelvic fractures and spine injuries. Previous studies have found association between pelvic fractures and other injuries. A radiological study reported that 46% of patients with pelvic fractures had concurrent abdominal injury [31]. The pelvic and abdominal organs most likely to be injured in patients with pelvic fractures are the urogenital tract, major blood vessels, spleen, liver, and kidneys [14, 35, 49]. Meanwhile, extrapelvic injuries mostly to the thorax and head [2, 23, 45]. Although our study identified a significant relationship between pelvic fractures and spine injuries, it must be noted that this association was predominantly determined by the high frequency of lumbar spine injuries.
Literature review revealed similar satisfactory outcomes after both operative and non-operative management of spinal injuries, thus forming a comparative control group [9, 32, 38, 47]. However, the results are not so encouraging for pelvic fractures [12, 15, 16, 50, 51]. The treatment strategy for pelvic ring or acetabular fractures is decided by the degree of instability or dislocation, as well as the presence of other injuries. Although many pelvic fractures can be treated conservatively, when the fracture pattern involves the posterior pelvic ring and/or there is displacement of the acetabular fracture, ORIF is usually required. In the case that patient’s hemodynamic status allows a surgery and enough surgical experience is available, definitive treatment within the first 24 h after the accident guarantee good clinical and surgical results [11]. New operative techniques are on the rise, such as percutaneous fixation using the 3D fluoroscopic image-based navigation system that produces an intraoperative image comparable to that obtained with postoperative CT, thus allowing the best possible anatomical reduction to be achieved in a single surgical procedure [10]. The pelvic fracture that occurs with a high-energy trauma is often accompanied by spinal cord injury, which may delay osteosynthetic fixation of pelvic fractures.
A delay of more than 3 weeks has been shown to be associated with poor fracture reduction quality and surgical outcome [30].
According to the literature, the mortality rate in patients with pelvic fractures is in the range of 6%-13%, with the lower rates being reported in recent decades [4, 5, 20, 27]. Severe bleeding is the leading cause of death, whether caused by the fracture itself or by other related injuries. Application of standardized trauma management strategies (e.g. ATLS®, MARCH®) in prehospital care and emergency departments can significantly improve outcomes; these strategies involve early aggressive blood and clotting factors transfusion regimens, as well as non-invasive pelvic stabilization (e.g. pelvic binder) [6, 17, 24, 25, 46]. The treatment of pelvic fractures depends on the patient’s hemodynamic status and concomitant diseases. Unstable anterior pelvic ring fractures can be urgently stabilized with an external fixator and the posterior pelvic ring fractures with a pelvic C-clamp.
In the case of uncontrollable bleeding in hemodynamically stable patients, interventional radiological embolization is a viable option, but for hemodynamically unstable patients the gold standard is surgical preperitoneal pelvic packing until the patient’s status allows a revision surgery [36, 39].
A cooperative multidisciplinary approach is necessary to improve outcomes. Protocol-guided bleeding management, a decision-making algorithm, and the involvement of specialized orthopedic pelvic surgeons are essential [40]. Delay of fracture fixation because of concomitant injuries leads to increased morbidity, prolonged immobilization [52], and need for intensive unit care. Effective trauma care can ensure an improved outcome with less inpatient complications and briefer hospital stay, as well as a reduce in clinical resource consumption and costs [53].
In our cohort, patients with pelvic fracture plus spine injury were significantly younger; this correlates with the fact that patients with stable pelvic injury were considerably older (> 65 years of age; isolated pelvic injury 44.8% vs. associated pelvic/spine 8%) and patients with an unstable pelvic injury suffer an association of spine/pelvic injury thinkable of the necessary high-energy required trauma forces. In our cohort, patients with spine plus pelvic injuries had lower Hb levels and blood pressure values at admission. Due to the accompanying spine injuries, these patients were more likely to undergo emergency stabilizations (e.g., external fixation or pelvic C-clamp). Meanwhile, patients with isolated pelvic injury were more likely to receive definitive pelvic fixation. The time until emergency stabilization and the time until definitive pelvic stabilization were both significantly longer in patients with pelvic fracture plus spine injury. Even though, the time until definitive surgical treatment of pelvic fracture was delayed in patients with associated spine injury, the surgery was still performed within the recommended 5–8 days after the accident.
As hypothesized, the outcome was clearly worse when pelvic fracture was associated with spine injury. Patients with combined spine and pelvic injury had longer hospital stay, more blood transfusion within 12 h of admission, more inpatient complications, and higher overall morbidity, mortality, and neurological disability rates.
Limitations
The main strength of this study is the inclusion of a large sample number of patients from several centers. However, there are limitations. Besides the retrospective nature of the study, one of the main deficiencies is the fact that the German Pelvic Register does not have detailed data related to adjuvant spinal injuries, as it focuses on the treatment of pelvic fractures. To evaluate the effect of different spinal injuries on the quality of care of pelvic fractures, a prospective detailed study will be necessary.
Conclusion
Delaying definitive surgical treatment of pelvic fractures due to spinal cord injury appears to have a negative impact on the outcome of pelvic fractures, especially on the quality of reduction of acetabular fractures. Severe accompanying injuries increase morbidity and mortality risk thereby prolonging hospital stay. Interdisciplinary consultation and management are necessary to improve outcomes.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Akademie für unfallchirurgie (Academy of trauma surgery)
- AIS:
-
Abbreviated injury score
- ATLS:
-
Advanced trauma life support
- ANOVA:
-
Analysis of variance
- CT:
-
Computer-tomography
- GPR:
-
German pelvic registry
- Hb:
-
Hemoglobin
- ISS:
-
Injury severity score
- KIT:
-
Karlsruhe institute of technology)
- MARCH®:
-
Algorithm for massive hemorrhage, airway, respiration, circulation, head injury/hypothermia
- ORIF:
-
Open reduction and internal fixation
- SBP:
-
Systolic blood pressure
References
Andrich S, Haastert B, Neuhaus E, et al. Epidemiology of Pelvic Fractures in Germany: Considerably High Incidence Rates among Older People. PLoS ONE. 2015;10(9):e0139078. https://doi.org/10.1371/journal.pone.0139078.
Ashkal A, Kong VY, Blodgett JM, et al. A review of blunt pelvic injuries at a major trauma centre in South Africa. S Afr J Surg. 2021;59(1):26a–26e.
Badami DRN, Shetty DMS, Kumar DMA. Functional and radiological outcome of acetabular fractures and the factors affecting the outcome. Int J Orthop Sci. 2017;3(4e):314–20. https://doi.org/10.22271/ortho.2017.v3.i4e.42.
Black SR, Sathy AK, Jo C, Wiley MR, Minei JP, Starr AJ. Improved Survival After Pelvic Fracture: 13-Year Experience at a Single Trauma Center Using a Multidisciplinary Institutional Protocol. J Orthop Trauma. 2016;30(1):22–8. https://doi.org/10.1097/BOT.0000000000000443.
Blackmore CC, Jurkovich GJ, Linnau KF, Cummings P, Hoffer EK, Rivara FP. Assessment of volume of hemorrhage and outcome from pelvic fracture. Arch Surg. 2003;138(5):504–9. https://doi.org/10.1001/archsurg.138.5.504.
Borgman MA, Spinella PC, Perkins JG, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805–13. https://doi.org/10.1097/TA.0b013e3181271ba3.
Burkhardt M, Nienaber U, Krause J, et al. Das komplexe Beckentrauma: Matching des Beckenregisters DGU mit dem TraumaRegister DGU®. Unfallchirurg. 2015;118(11):957–62. https://doi.org/10.1007/s00113-014-2565-8.
Burkhardt M, Nienaber U, Holstein JH, et al. Trauma registry record linkage: Methodological approach to benefit from complementary data using the example of the German Pelvic Injury Register and the TraumaRegister DGU®. BMC Med Res Methodol. 2013;13(1):1. https://doi.org/10.1186/1471-2288-13-30.
Cantor JB, Lebwoh NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine (Phila Pa 1976). 1993;18(8):971–6.
Ciolli G, Caviglia D, Vitiello C, et al. Navigated percutaneous screw fixation of the pelvis with o-arm 2: Two years’ experience. Med Glas. 2021;18(1):1–7. https://doi.org/10.17392/1326-21.
Coccolini F, Stahel PF, Montori G, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12:5. https://doi.org/10.1186/s13017-017-0117-6.
Cole JD, Blum DA, Ansel LJ. Outcome after fixation of unstable posterior pelvic ring injuries. Clin Orthop Relat Res. 1996;329:160–79. https://doi.org/10.1097/00003086-199608000-00020.
Cooper C, Dunham CM, Rodriguez A. Falls and major injuries are risk factors for thoracolumbar fractures: cognitive impairment and multiple injuries impede the detection of back pain and tenderness. J Trauma. 1995;38(5):692–6. https://doi.org/10.1097/00005373-199505000-00003.
Culemann U, Scola A, Tosounidis G, Pohlemann T, Gebhard F. Concept for treatment of pelvic ring injuries in elderly patients. A challenge. Unfallchirurg. 2010;113(4):258–71. https://doi.org/10.1007/s00113-010-1762-3.
Draijer F, Egbers HJ, Havemann D. Quality of life after pelvic ring injuries: follow-up results of a prospective study. Arch Orthop Trauma Surg. 1997;116(1–2):22–6. https://doi.org/10.1007/BF00434095.
Dujardin FH, Hossenbaccus M, Duparc F, Biga N, Thomine JM. Long-term functional prognosis of posterior injuries in high-energy pelvic disruption. J Orthop Trauma. 1998;12(3):141–5. https://doi.org/10.1097/00005131-199803000-00001.
Eastridge BJ, Starr A, Minei JP, O’Keefe GE, Scalea TM. The importance of fracture pattern in guiding therapeutic decision-making in patients with hemorrhagic shock and pelvic ring disruptions. J Trauma. 2002;53(3):441–6. https://doi.org/10.1097/00005373-200209000-00009.
Fernandez-de Thomas RJ, De Jesus O. Thoracolumbar Spine Fracture. 2021 Aug 30. In: StatPearls (Internet). Treasure Island: StatPearls Publishing; 2022.
Gänsslen A, Oestern HJ. Azetabulumfrakturen. Chirurg. 2011;82(12):1133–50. https://doi.org/10.1007/s00104-011-2135-3.
Gaski IA, Barckman J, Naess PA, et al. Reduced need for extraperitoneal pelvic packing for severe pelvic fractures is associated with improved resuscitation strategies. J Trauma Acute Care Surg. 2016;81(4):644–51. https://doi.org/10.1097/TA.0000000000001139.
Giráldez-Sánchez MA, Lázaro-Gonzálvez Á, Martínez-Reina J, et al. Percutaneous iliosacral fixation in external rotational pelvic fractures A biomechanical analysis. Injury. 2015;46(2):327–32. https://doi.org/10.1016/j.injury.2014.10.058.
Greenspan L, McLellan B, Greig H. AIS and ISS - A scoring chart.pdf. J Trauma. 1985;25(1):60–4.
Gustavo Parreira J, Coimbra R, Rasslan S, Oliveira A, Fregoneze M, Mercadante M. The role of associated injuries on outcome of blunt trauma patients sustaining pelvic fractures. Injury. 2000;31(9):677–82. https://doi.org/10.1016/s0020-1383(00)00074-7.
Holcomb JB, Tilley BC, Baraniuk S, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471–82. https://doi.org/10.1001/jama.2015.12.
Holcomb JB, Wade CE, Michalek JE, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008;248(3):447–58. https://doi.org/10.1097/SLA.0b013e318185a9ad.
Holstein JH, Stuby FM, Herath SC, Culemann U, Aghayev E, Pohlemann T. Einfluss des Beckenregisters der DGU auf die Versorgung von Beckenringfrakturen. Unfallchirurg. 2016;119(6):475–81. https://doi.org/10.1007/s00113-016-0168-2.
Holstein JH, Culemann U, Pohlemann T. What are predictors of mortality in patients with pelvic fractures? Clin Orthop Relat Res. 2012;470(8):2090–7. https://doi.org/10.1007/s11999-012-2276-9.
Iqbal F, Taufiq I, Kazim M, Najjad R, Khan N, Zia O Bin. Hp-28–217. 2016;28(4):217–224.
VandenBerg J, Cullison K, Fowler SA, Parsons MS, McAndrew CM, Carpenter CR. Blunt Thoracolumbar-Spine Trauma Evaluation in the Emergency Department: A Meta-Analysis of Diagnostic Accuracy for History, Physical Examination, and Imaging. J Emerg Med. 2019;56(2):153–65. https://doi.org/10.1016/j.jemermed.2018.10.032.
Katsoulis E, Giannoudis PV. Impact of timing of pelvic fixation on functional outcome. Injury. 2006;37(12):1133–42. https://doi.org/10.1016/j.injury.2006.07.017.
Killeen KL, DeMeo JH. CT detection of serious internal and skeletal injuries in patients with pelvic fractures. Acad Radiol. 1999;6(4):224–8. https://doi.org/10.1016/S1076-6332(99)80209-8.
Knight RQ, Stornelli DP, Chan DP, Devanny JR, Jackson KV. Comparison of operative versus nonoperative treatment of lumbar burst fractures. Clin Orthop Relat Res. 1993;293:112–21.
Kumar R, Lim J, Mekary RA, et al. Traumatic Spinal Injury: Global Epidemiology and Worldwide Volume. World Neurosurg. 2018;113:e345–63. https://doi.org/10.1016/j.wneu.2018.02.033.
Lee C-H, Hsu C-C, Huang P-Y. Biomechanical study of different fixation techniques for the treatment of sacroiliac joint injuries using finite element analyses and biomechanical tests. Comput Biol Med. 2017;87:250–7. https://doi.org/10.1016/j.compbiomed.2017.06.007.
Leenen LPH. Pelvic Fractures: Soft Tissue Trauma. Eur J trauma Emerg Surg Off Publ Eur Trauma Soc. 2010;36(2):117–23. https://doi.org/10.1007/s00068-010-1038-0.
Marzi I, Lustenberger T. Management of Bleeding Pelvic Fractures. Scand J Surg SJS Off organ Finnish Surg Soc Scand Surg Soc. 2014;103(2):104–11. https://doi.org/10.1177/1457496914525604.
Matta JM. Fractures of the acetabulum: Accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Jt Surg - Ser A. 1996;78(11):1632–45. https://doi.org/10.1055/s-0030-1267077.
Mumford J, Weinstein JN, Spratt KF, Goel VK. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine (Phila Pa 1976). 1993;18(8):955–70.
Niola R, Pinto A, Sparano A, Ignarra R, Romano L, Maglione F. Arterial bleeding in pelvic trauma: priorities in angiographic embolization. Curr Probl Diagn Radiol. 2012;41(3):93–101. https://doi.org/10.1067/j.cpradiol.2011.07.008.
Perkins ZB, Maytham GD, Koers L, Bates P, Brohi K, Tai NRM. Impact on outcome of a targeted performance improvement programme in haemodynamically unstable patients with a pelvic fracture. Bone Joint J. 2014;96-B(8):1090–7. https://doi.org/10.1302/0301-620X.96B8.33383.
Phruetthiphat O-A, Willey M, Karam MD, Gao Y, Westerlind BO, Marsh JL. Comparison of Outcomes and Complications of Isolated Acetabular Fractures and Acetabular Fractures With Associated Injuries. J Orthop Trauma. 2017;31(1):31–6. https://doi.org/10.1097/BOT.0000000000000720.
Pouw MH, Deunk J, Brink M, et al. Is a pelvic fracture a predictor for thoracolumbar spine fractures after blunt trauma? J Trauma - Inj Infect Crit Care. 2009;67(5):1027–32. https://doi.org/10.1097/TA.0b013e31818cb261.
Rommens PM, Dietz S-O, Ossendorf C, Pairon P, Wagner D, Hofmann A. Fragility fractures of the pelvis: should they be fixed? Acta Chir Orthop Traumatol Cech. 2015;82(2):101–12.
Rommens PM, Wagner D, Hofmann A. Minimal Invasive Surgical Treatment of Fragility Fractures of the Pelvis. Chirurgia (Bucur). 2017;112(5):524–37. https://doi.org/10.21614/chirurgia.112.5.524.
Saydam M, Şahin M, Yilmaz KB, et al. Correlation of pelvic fractures and associated injuries: An analysis of 471 pelvic trauma patients. Ulus travma ve acil cerrahi Derg. 2019;25(5):489–96. https://doi.org/10.5505/tjtes.2018.72505.
Schweigkofler U, Wohlrath B, Trentsch H, et al. Diagnostics and early treatment in prehospital and emergency-room phase in suspicious pelvic ring fractures. Eur J trauma Emerg Surg Off Publ Eur Trauma Soc. 2018;44(5):747–52. https://doi.org/10.1007/s00068-017-0860-0.
Shen WJ, Shen YS. Nonsurgical treatment of three-column thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976). 1999;24(4):412–5. https://doi.org/10.1097/00007632-199902150-00024.
Shi HF, Xiong J, Chen YX, Wang JF, Wang YH. Radiographic analysis of the restoration of hip joint center following open reduction and internal fixation of acetabular fractures: A retrospective cohort study. BMC Musculoskelet Disord. 2014;15(1):277. https://doi.org/10.1186/1471-2474-15-277.
Siegmeth A, Müllner T, Kukla C, Vécsei V. Associated injuries in severe pelvic trauma. Unfallchirurg. 2000;103(7):572–81. https://doi.org/10.1007/s001130050585.
Tee SS, Hyzan Y, Razak M. Functional outcome of open reduction and internal fixation of pelvic ring injuries. Med J Malaysia. 2000;55(Suppl C):49–58.
Tornetta P 3rd, Matta JM. Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res. 1996;329:186–93. https://doi.org/10.1097/00003086-199608000-00022.
Vallier HA, Cureton BA, Ekstein C, Oldenburg FP, Wilber JH. Early definitive stabilization of unstable pelvis and acetabulum fractures reduces morbidity. J Trauma. 2010;69(3):677–84. https://doi.org/10.1097/TA.0b013e3181e50914.
Vallier HA, Dolenc AJ, Moore TA. Early Appropriate Care: A Protocol to Standardize Resuscitation Assessment and to Expedite Fracture Care Reduces Hospital Stay and Enhances Revenue. J Orthop Trauma. 2016;30(6):306–11. https://doi.org/10.1097/BOT.0000000000000524.
VandenBerg J, Cullison K, Fowler SA, Parsons MS, McAndrew CM, Carpenter CR. Blunt Thoracolumbar-Spine Trauma Evaluation in the Emergency Department: A Meta-Analysis of Diagnostic Accuracy for History, Physical Examination, and Imaging. J Emerg Med. 2019;56(2):153–65. https://doi.org/10.1016/j.jemermed.2018.10.032.
Acknowledgements
We sincerely thank Mr. Prof. Dr. Wolf-Dieter Heller for the statistical analysis (Karlsruhe Institute of Technology, Karlsruhe, Germany)
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
LN, NM, MAK, TH, and BU designed the study from an orthopedic and trauma surgeon’s point of view. LN, NM, JNR and BU acquired the data from the German Pelvic Registry. LN, NM, and BU did the data analysis. All authors interpreted the data, revised the manuscript regarding scientific input, and approved the submitted final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The patients gave written informed consent for participation in the GPR. The study was conducted according to the guidelines of the Declaration of Helsinki. The Ethics Committee of the Chamber of Physicians of the Federal State of Saarland approved the GPR (No. 29/14). The Ethics Committee of the Eberhard-Karls-University in Tübingen, Germany, approved this retrospective cohort study (No. 968/2018BO2).
Consent for publication
Consent for publication was part of the written informed consent the patients gave for their participation in the GPR.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Navas, L., Mengis, N., Zimmerer, A. et al. Patients with combined pelvic and spinal injuries have worse clinical and operative outcomes than patients with isolated pelvic injuries analysis of the German Pelvic Registry. BMC Musculoskelet Disord 23, 251 (2022). https://doi.org/10.1186/s12891-022-05193-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05193-0