Abstract
Background
Between 2 to 10% of non-displaced femoral neck fractures (nFNF) cannot be diagnosed on plain radiographs and require further imaging investigation to be detected or verified. These fractures are referred to as occult hip fractures. This study aimed to report treatment failures, reoperations and mortality in a consecutive series of occult femoral neck fractures (FNF) treated with internal fixation (IF).
Methods
A retrospective multicenter study was performed based on a consecutive series of patients aged ≥ 60 years with an occult magnetic resonance imaging (MRI) verified Garden I and II FNF sustained after a trauma and treated with primary IF. We included 93 patients with a minimum 2-year follow-up. Radiographic assessment encompassed pre- and postoperative tilt, implant inclination, MRI and treatment failure. Data on reoperation and mortality were collected. Treatment failure was defined as fixation failure, nonunion, avascular necrosis or posttraumatic osteoarthritis.
Results
The study comprised of 93 patients (72% women, 67/93) with a mean age of 82 (range, 60–97) years. Overall, 6 (6%) patients had major reoperations. 2 (2%) had minor reoperations. One-month mortality was 7%, 1-year mortality was 20% and 2-year mortality was 31%.
Conclusion
This multicenter cohort study identifies a subgroup of elderly patients with MRI verified Garden I and II FNFs sustained after trauma, i.e. occult fractures. These fractures seem to have a lower complication rate compared to nFNF identified on plain radiographs.
Level of evidence
Prognostic Level V. See Instructions to Authors for a complete description of levels of evidence.
Similar content being viewed by others
Background
Femoral neck fractures (FNFs) are commonly encountered in orthopedic practice and the absolute numbers are expected to increase further as there is a growing elderly population worldwide [1]. Most FNFs can receive adequate treatment after being diagnosed with plain radiographs [2]. A small group of non-displaced (nFNF) or minimally displaced FNFs sustained after trauma cannot be diagnosed on plain radiographs and require further investigation with computed tomography (CT), radionuclide bone scan or magnetic resonance imaging (MRI). These fractures are referred to as occult hip fractures and represent 2–10% of all nFNF [2,3,4,5,6]. MRI is more accurate than both CT and radionuclide bone scans to detect occult fractures and also reduce time to diagnosis [2, 7, 8]. Reoperation rates after internal fixation (IF) of nFNFs detected on plain radiographs range from 8 to 19% in previous reports [9]. However, there may be subgroups of nFNFs whose fracture characteristics may lead to different outcomes, complications and reoperation rates [10, 11]. The MRI verified nFNFs, i.e. the occult hip fractures, is a potential subgroup. There are few reports on the outcome of these fractures [12, 13]. Therefore, our study aimed to describe treatment failures and reoperations in patients with MRI verified FNFs treated with IF.
Method
Study settings
A retrospective multicenter cohort study was performed including patients ≥ 60 years with an MRI verified FNF treated with IF between January 2003 and October 2018 at four orthopedic departments in Sweden: Umeå University Hospital (2003–2018) a third-level university hospital with a catchment area of about 160,000 inhabitants, Danderyd Hospital (2010–2018) a third-level university hospital with a catchment area of about 500,000 inhabitants, Skåne University Hospital in Malmö (2005–2014) a third-level university hospital with a catchment area of about 450,000 inhabitants and Skellefteå Hospital (2004–2018) a first-level hospital with a catchment area of about 80,000 inhabitants.
Patients and data collection
A consecutive series of patients ≥ 60 years with an MRI verified FNF were included. Only patients treated with IF by either cannulated screws or pins were included and followed until death or December 2020. Patient demographics were collected by a review of the surgical and medical charts. We collected data including age, sex, ASA classification, cognitive impairment (diagnosis in medical records prior to fracture), use of a walking aid prior to fracture, admission from sheltered housing or a nursing home, the use of MRI for diagnosis, method of surgical treatment, reoperation, treatment failure and date of death.
Radiographic assessment
The plain anteroposterior (AP) radiographs were used to classify fractures according to the Garden classification system (Fig. 1 a, b) [14]. The pre- and postoperative tilt of the femoral head was measured on a lateral radiograph of the hip using the method described by Palm et al. [10, 11, 15]. If a postoperative lateral radiograph was missing, the postoperative tilt was measured on the intraoperative image documentation. For implant inclination we performed measurements on the inferior pin or screw on the postoperative AP radiograph [16]. Three raters (JS, PS, AP), who were not blinded, performed all measurements. At the time of the study no national guidelines on diagnosing fractures with MRI were present, however, in most cases T1, T2 and STIR weighted sequences were used (Fig. 2a, b). All images were digitally acquired using a Picture Archiving and Communication System (PACS, Impax, Agfa, Antwerp, Belgium).
Internal fixation
IF was performed according to the same principles at the 4 hospitals. With the patient on a fracture table and under intra operative imaging 2 or 3 pins/screws were placed along the femoral neck transfixing the fracture. Either Hansson Pins; Swemac Orthopaedics AB, Sweden or Olmed Screws; DePuy/Johnson & Johnson, Sollentuna, Sweden were used.
Outcome measurements
The primary end-point was a major reoperation due to avascular necrosis (AVN), fixation failure, posttraumatic osteoarthritis or nonunion. Major reoperation was defined as hip arthroplasty, excision arthroplasty or re-osteosynthesis due to peri-implant fractures. The definition of minor reoperation was removal or adjustment of implant.
Statistical analysis
Variables are presented as proportions of all fractures. Nominal variables are presented as proportions of all fractures and scale variables as means ± standard deviation (± SD) and range. We used SPSS (IBM SPSS Statistics for Mac, Version 26.0, Armonk, NY: IBM Corp. USA) for statistical analyses.
Results
Patients and descriptive data
We included 93 patients (72% females) with a mean age of 82 (range, 60–97) (Table 1). The median follow-up was 74 (range, 0–190) months. One-third of the patients suffered from cognitive impairment and 23% were admitted from sheltered housing. The 30-day mortality was 7%, 1-year mortality was 20% and 2-year mortality was 31%.
Radiographic assessment
We found all of the included fractures to be non-displaced on the AP radiograph and used the method described by Palm et al. [15] to verify that the fractures were non-displaced or minimally displaced on the lateral radiograph (Table 2).
Treatment failure and reoperations
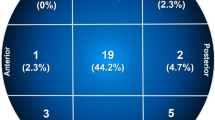
Overall, 6 (6%) patients were classified as treatment failure and were treated with reoperations (Fig. 3). In total, 8 (8%) patients had reoperation as two patients had implant removal (Table 3). 1 patient with AVN, 1 with non-union, 2 suffered fixation failure and 1 a peri-implant fracture. 1 developed post-traumatic osteoarthritis. 8 (8%) patients underwent a reoperation, including minor procedures during the study period. 6 patients had a major reoperation during the first 2 years after IF, 2 patients received a total hip arthroplasty, 2 patients hemiarthroplasty and 2 patients underwent re-osteosynthesis. Minor reoperation with removal of implants was performed in 2 patients.
Discussion
The main finding in this study is that MRI verified nFNFs, i.e. occult hip fractures, have a low but not insignificant rate of complications and reoperations when compared to nFNFs verified with plain radiographs [9]. In the present study the complication rate was 6%, major reoperations were evenly distributed between AVN, fixation failure, peri-implant fractures and post-traumatic arthritis resulting in 2 cases of re-osteosynthesis and 4 cases of hip arthroplasty. 2 patients had minor reoperation defined as implant removal. It has previously been reported that nFNFs treated with IF have reoperation rates between 8 and 19% [9]. These reoperation rates are higher than those presented in our cohort due to our selection of patients. We suggest that the MRI verified occult fracture may be a subgroup of nFNF with a relatively low rate of reoperations following IF. Other subgroups of nFNFs treated with IF have been identified with significant reoperation rates. A preoperative posterior tilt over 20° on the lateral radiograph has been shown to increase the risk of treatment failure and major reoperation [17,18,19,20]. An anterior tilt of at least 10° is associated with up to 40% suffering a treatment failure [10, 11]. However, these reoperation rates in combination with the limited literature comparing IF with hip arthroplasty in the elderly population, warrant further comparative studies [21, 22]. Limitations of the present study include the retrospective design. In addition, the limited sample size which prevents us from performing any in-depth analysis of risk factors associated with treatment failure and reoperations. We did not perform any intra- or interobserver reliability testing of the obtained measurements. However, interobserver reliability has been presented in a previous study from our institution [11]. Nevertheless, this is, to our knowledge, the largest consecutive series of MRI verified nFNFs presented to date. The sample size included offers a rough model of the outcome of these fractures which represents the”best possible” clinical results of a FNF treated with IF. We believe our data is highly reliable, as we used the unique Swedish personal identity number to collect data by reviewing the hospital records of all contributing departments. In addition, the hospitals provide all acute orthopaedic care in the catchment area to ensure completeness of data. However, this fragile group of patients, with a relatively large share living in sheltered housing, are often unfit to seek healthcare services actively. This could mask the identification of failures and potential major reoperations related to nFNF.
Conclusion
Based on our results, MRI verified nFNFs have a lower reoperation rate than nFNF seen on conventional radiographs. Still, MRI verified nFNF are not exempt from hip related complications and clinicians and patients need to be aware that even these perceived benign fractures are at risk of reoperation.
Availability of data and materials
Due to Swedish legislation, the datasets used and/or analyzed during the current study are not publicly available. Data is available from the corresponding author on reasonable request.
Abbreviations
- NFNF:
-
Non-displaced femoral neck fracture
- FNF:
-
Femoral neck fracture
- IF:
-
Internal fixation
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- RCT:
-
Randomized clinical trial
- ASA:
-
American Society of Anesthesiologists
- AP:
-
Anteroposterior
- PACS:
-
Picture Archiving and Communication System
- SPSS:
-
Statistical Package for the Social Sciences
References
Chen IJ, Chiang CY, Li YH, Chang CH, Hu CC, Chen DW, Chang Y, Yang WE, Shih HN, Ueng SW, Hsieh PH. Nationwide cohort study of hip fractures: time trends in the incidence rates and projections up to 2035. Osteoporos Int. 2015;26(2):681–8. https://doi.org/10.1007/s00198-014-2930-z Epub 2014 Oct 30.
Lubovsky O, Liebergall M, Mattan Y, Weil Y, Mosheiff R. Early diagnosis of occult hip fractures MRI versus CT scan. Injury 2005;36(6):788–92)
Parker MJ. Missed hip fractures. Arch Emerg Med. 1992;9(1):23–7.
Gill SK, Smith J, Fox R, Chesser TJ. Investigation of occult hip fractures: the use of CT and MRI. ScientificWorldJournal. 2013;2013:830319.
Hossain M, Barwick C, Sinha AK, Andrew JG. Is magnetic resonance imaging (MRI) necessary to exclude occult hip fracture? Injury. 2007;38(10):1204–8.
Frihagen F, Nordsletten L, Tariq R, Madsen JE. MRI diagnosis of occult hip fractures. Acta Orthop. 2005;76(4):524–30.
Verbeeten KM, Hermann KL, Hasselqvist M, Lausten GS, Joergensen P, Jensen CM, et al. The advantages of MRI in the detection of occult hip fractures. Eur Radiol. 2005;15(1):165–9.
Haubro M, Stougaard C, Torfing T, Overgaard S. Sensitivity and specificity of CT- and MRI-scanning in evaluation of occult fracture of the proximal femur. Injury. 2015;46(8):1557–61.
Onativia IJ, Slullitel PA, Dilernia FD, Viezcas JMG, Vietto V, Ramkumar PN, Buttaro MA, Piuzzi NS. Outcomes of nondisplaced intracapsular femoral neck fractures with internal screw fixation in elderly patients: a systematic review. Hip Int. 2018;28(1):18–28.
Sjöholm P, Otten V, Wolf O, Gordon M, Karsten G, Sköldenberg O, Mukka S. Posterior and anterior tilt increases the risk of failure after internal fixation of Garden I and II femoral neck fracture. Acta Orthop. 2019;90(6):537–41. https://doi.org/10.1080/17453674.2019.1637469.
Sjöholm P, Sundkvist J, Wolf O, Sköldenberg O, Gordon M, Mukka S. Preoperative Anterior and Posterior Tilt of Garden I-II Femoral Neck Fractures Predict Treatment Failure and Need for Reoperation in Patients Over 60 Years. JB JS Open Access. 2021 Oct 28;6(4):e21.00045. doi: https://doi.org/10.2106/JBJS.OA.21.00045.
Pejic A, Hansson S, Rogmark C. Magnetic resonance imaging for verifying hip fracture diagnosis why, when and how? Injury. 2017;48(3):687–91. https://doi.org/10.1016/j.injury.2017.01.025 Epub 2017 Jan 17.
Beloosesky Y, Hershkovitz A, Guz A, Golan H, Salai M, Weiss A. Clinical characteristics and long-term mortality of occult hip fracture elderly patients. Injury. 2010;41(4):343–7. https://doi.org/10.1016/j.injury.2009.08.017.
Garden RS. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br. 1961;43:647–63.
Palm H, Gosvig K, Krasheninnikoff M, Jacobsen S, Gebuhr P. A new measurement for posterior tilt predicts reoperation in undisplaced femoral neck fractures: 113 consecutive patients treated by internal fixation and followed for 1 year. Acta Orthop. 2009;80(3):303–7.
Nyholm AM, Palm H, Sandholdt H, Troelsen A, Gromov K; Danish Fracture Database Collaborators. Osteosynthesis with Parallel Implants in the Treatment of Femoral Neck Fractures: Minimal Effect of Implant Position on Risk of Reoperation. J Bone Joint Surg Am. 2018 Oct 3;100(19):1682–1690. doi: https://doi.org/10.2106/JBJS.18.00270.
Nielsen LL, Smidt NS, Erichsen JL, Palm H, Viberg B. Posterior tilt in nondisplaced femoral neck fractures increases the risk of reoperations after osteosynthesis. A systematic review and meta-analysis Injury. 2020;51(12):2771–8. https://doi.org/10.1016/j.injury.2020.09.033.
Dolatowski FC, Adampour M, Frihagen F, Stavem K, Erik Utvåg S, Hoelsbrekken SE. Preoperative posterior tilt of at least 20° increased the risk of fixation failure in Garden-I and -II femoral neck fractures. Acta Orthop. 2016;87(3):252–6.
Okike K, Udogwu UN, Isaac M, Sprague S, Swiontkowski MF, Bhandari M, Slobogean GP, FAITH Investigators. Not All Garden-I and II Femoral Neck Fractures in the Elderly Should Be Fixed: Effect of Posterior Tilt on Rates of Subsequent Arthroplasty. J Bone Joint Surg Am. 2019 Oct 16;101(20):1852–1859. doi: https://doi.org/10.2106/JBJS.18.01256
Honkanen JS, Ekman EM, Huovinen VK, Mäkelä KT, Koivisto M, Karvonen MP, Laaksonen I. Preoperative Posterior Tilt Increases the Risk of Later Conversion to Arthroplasty After Osteosynthesis for Femoral Neck Fracture. J Arthroplasty. 2021 May 5:S0883–5403(21)00411–3. doi: https://doi.org/10.1016/j.arth.2021.04.039. Epub ahead of print
Wolf O, Sjöholm P, Hailer NP, Möller M, Mukka S. Study protocol: HipSTHeR - a register-based randomised controlled trial - hip screws or (total) hip replacement for undisplaced femoral neck fractures in older patients. BMC Geriatr. 2020;20(1):19. https://doi.org/10.1186/s12877-020-1418-2.
Viberg B, Kold S, Brink O, Larsen MS, Hare KB, Palm H; SENSE collaborators. Is arthroplaSty bEtter than interNal fixation for undiSplaced femoral nEck fracture? A national pragmatic RCT: the SENSE trial. BMJ Open. 2020 Oct 10;10(10):e038442. doi: https://doi.org/10.1136/bmjopen-2020-038442
Acknowledgements
None
Funding
Open access funding provided by Umea University. The study was funded by grants from the regional agreement on medical training and clinical research (ALF) between Västerbotten County Council and Umeå University, and between Skane Region and Lund University.
Author information
Authors and Affiliations
Contributions
JS collected data, performed radiographic measurements, performed statistical analysis and wrote the manuscript. PS, AP performed radiographic measurements, reviewed the manuscript. OW, OS wrote and reviewed the manuscript. CR initiated the study, wrote and reviewed the manuscript. SM initiated the study, supervised JS, performed statistical analysis and wrote and reviewed the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the principles of the Helsinki Declaration and was approved by the Swedish Ethical Review Authority (entry number 2019–06449) and the regional ethical committee in Lund, Sweden (EPN 2015/91). The consent to participate was waived by the Swedish Ethical Review Authority due to the retrospective design of the study.
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sundkvist, J., Sjöholm, P., Pejic, A. et al. Clinical outcomes of patients with Garden I and II femoral neck fractures as verified on MRI: a retrospective case series. BMC Musculoskelet Disord 23, 144 (2022). https://doi.org/10.1186/s12891-022-05088-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05088-0