Abstract
Background
Anterior cruciate ligament reconstruction (ACLR) together with concomitant meniscal injury are risk factors for the development of tibiofemoral (TF) osteoarthritis (OA), but the potential effect on the patellofemoral (PF) joint is unclear. The aim of this study was to: (i) investigate change in patellar cartilage morphology in individuals 2.5 to 4.5 years after ACLR with or without concomitant meniscal pathology and in healthy controls, and (ii) examine the association between baseline patellar cartilage defects and patellar cartilage volume change.
Methods
Thirty two isolated ACLR participants, 25 ACLR participants with combined meniscal pathology and nine healthy controls underwent knee magnetic resonance imaging (MRI) with 2-year intervals (baseline = 2.5 years post-ACLR). Patellar cartilage volume and cartilage defects were assessed from MRI using validated methods.
Results
Both ACLR groups showed patellar cartilage volume increased over 2 years (p < 0.05), and isolated ACLR group had greater annual percentage cartilage volume increase compared with controls (mean difference 3.6, 95% confidence interval (CI) 1.0, 6.3%, p = 0.008) and combined ACLR group (mean difference 2.2, 95% CI 0.2, 4.2%, p = 0.028). Patellar cartilage defects regressed in the isolated ACLR group over 2 years (p = 0.02; Z = − 2.33; r = 0.3). Baseline patellar cartilage defect score was positively associated with annual percentage cartilage volume increase (Regression coefficient B = 0.014; 95% CI 0.001, 0.027; p = 0.03) in the pooled ACLR participants.
Conclusions
Hypertrophic response was evident in the patellar cartilage of ACLR participants with and without meniscal pathology. Surprisingly, the increase in patellar cartilage volume was more pronounced in those with isolated ACLR. Although cartilage defects stabilised in the majority of ACLR participants, the severity of patellar cartilage defects at baseline influenced the magnitude of the cartilage hypertrophic response over the subsequent ~ 2 years.
Similar content being viewed by others
Background
Anterior cruciate ligament reconstruction (ACLR) is a common treatment following ACL injury. Whilst ACLR is typically effective in restoring anterior knee stability, a substantial portion of ACLR patients will develop early onset knee osteoarthritis (OA) – a painful and debilitating condition for which there is no known cure [1,2,3,4]. Traditionally, research has focused on tibiofemoral (TF) joint OA following ACLR; however, a high prevalence of OA in the patellofemoral (PF) joint following ACLR has been reported [5, 6] and which is characterised by knee symptoms such as pain and reduced function [5].
Meniscal injury frequently occurs at the time of the ACL injury and has been recognised as a risk factor for knee OA [1, 7, 8]. Biomechanical changes following meniscal injury or resection are thought to influence anterior-posterior laxity of the PF joint and internal-external rotation of the TF joint [9, 10]; thus, altered PF and TF joint biomechanics likely predispose the knee joint to OA development [11]. A previous study [5] reported that medial meniscal injury increased the risk of developing PF joint OA and medial TF joint OA at 5–10 years post-ACLR. A prospective evaluation of PF cartilage changes in ACLR knees with and without concomitant meniscal injury is warranted to understand PF joint OA cartilage pathophysiology.
Magnetic resonance imaging (MRI) is a non-invasive method to assess knee cartilage morphology with demonstrated sensitivity and reliability [12]. MRI studies have revealed alterations in cartilage morphology in the early years following ACL injury and ACLR [13, 14]. Morphological changes vary according to the knee compartment as both cartilage increases and decreases have been reported at 1–5 years post-surgery [15,16,17,18]. In particular, a longitudinal study demonstrated a general increase in TF joint cartilage thickness over a 5-year post-operative period [15], suggesting a alteration of cartilage homeostasis [15] prior to cartilage breakdown [15,16,17]. By contrast, a recent study reported a decreased in total PF joint cartilage thickness over 5 years following ACL injury [14]. Cartilage defects, a MRI-derived semi-quantitative cartilage morphology measurement, indicate early pathology following joint injury [18, 19]. Potter et al. [20] reported progressive worsening of patella cartilage defects following ACL injury over 11 years regardless of treatment (i.e., ACLR or conservative management). These findings demonstrated PF joint cartilage loss and degeneration following ACL injury/ACLR. In addition, the detrimental long-term effects of cartilage defects have been established in the TF joint. Whilst severe baseline cartilage defects were associated with cartilage loss in knee OA populations [21, 22], we found that mild baseline cartilage defects were associated with greater increases in cartilage volume in an ACLR cohort [23]. Overall, tibial cartilage volume increased after ACLR, and those with isolated ACLR exhibit greater increases in cartilage volume than those with ACLR combined with commitment meniscal pathology at the lateral tibia [23]. Thus, it is of interest to examine whether similar responses are apparent in the patellar cartilage.
The aims of this study were twofold. The first aim was to investigate the changes of patellar cartilage volume and cartilage defects from 2.5 to 4.5 years after ACLR in participants with: (i) isolated ACLR without meniscal pathology, (ii) ACLR combined with meniscal pathology, and (iii) healthy controls. It was hypothesised that: H1): ACLR knees would show increased patellar cartilage volume and increased cartilage defects score (progression), whilst control knees would show no change over 2-year; H2): knees with combined ACLR and meniscal pathology would show greater increase in cartilage volume and greater increase in cartilage defect scores compared with ACLR isolated knees. The second aim was to examine the association between baseline patellar cartilage defects scores and cartilage volume change in ACLR knees. It was hypothesised that: H3): higher cartilage defects at baseline would be associated with greater cartilage volume increase after 2 years.
Methods
Participants
One hundred participants who had undergone ACLR were recruited in Melbourne (Epworth Hospital Richmond) and Gold Coast (Pindara Hospital, Pacific Private Hospital, and John Flynn Hospital) Australia. Characteristics of these ACLR participants have been described in detail previously [23, 24]. Briefly, this relatively young cohort (i.e., 18–40 years) had undergone ACLR 2–3 years prior using the combined semitendinosus and gracilis autograft and none had evidence of tibiofemoral OA. Those with concomitant meniscal pathology (i.e., meniscal injury, repair or partial meniscectomy) were categorized to the combined ACLR and meniscal pathology group. A control group consisting of 30 healthy individuals without a history of knee injury and lower-limb surgery were also recruited.
ACLR surgery was arthroscopically assisted and has been previously described [23, 24]. Management of the meniscal injury (i.e., leave as is, repair, or partial meniscectomy) was determined by the surgeon based on the injury appearance at the time of surgery. Partial meniscectomy was performed for non-repairable meniscal injuries. No chondral surgery was performed as all lesions were not considered serious [International Cartilage Repair Society (ICRS) score grade < 3]. After being discharged from hospital, patients were encouraged to participate in weight bearing exercise on an as-tolerated basis without the use of braces or splints. The ACLR rehabilitation protocol targeted on rapid restoration of knee range of motion as well as quadriceps function.
Anthropometry
Mass and height were measured, and then used to calculate BMI (kg/m2).
Magnetic resonance imaging
The MRI protocol and assessment have been presented previously [24] and are briefly summarized below. The MRI scans were performed at baseline (i.e., 2–3 years post-ACLR) and at follow-up 2 years later using whole-body MRI units in Melbourne (3.0 T, Siemens Magenetom Verio, Erlangen, Germany) and the Gold Coast (1.5 T, GE Healthcare Signa, Wisconsin, USA). Knees were imaged using T1-weighted 3-dimensional gradient recall sequences in the sagittal plane [25].
Patella cartilage volume and patella bone volume
Patella cartilage volume was measured based on the T1-weighted images using a previously published method [24, 25]. Images were transferred to Osiris v4.19 software (University Hospital of Geneva, Geneva, Switzerland) and cartilage was manually segmented by tracing the osteochondral interface and articular surface slice-by-slice. Cartilage volume (mm3) was determined by summing segmented areas and multiplying by slice thickness (1.5 mm). Baseline and follow-up cartilage volumes were measured in pairs for each participant by one trained assessor (XW) who was blinded to participant status. Intra-class correlation coefficients (ICC) for intra-rater and inter-rater reliability were 0.997 and 0.993, respectively [24]. Baseline patella bone volume was measured for statistical adjustment using the same method as for cartilage volume with ICCs above 0.98. The annual percentage change in patella cartilage volume was calculated as follows: (follow-up patella cartilage volume minus baseline patella cartilage volume) divided by (baseline patella cartilage volume multiplied by time period between scans). Positive values indicate increased cartilage volume over time.
Cartilage defects
Cartilage defects were assessed in T1-weighted images using the ICRS cartilage defect grade (score 0–4) as previously described [18, 24, 26]. The cartilage defects were graded as follows [18, 26]: grade 0, normal cartilage; grade 1, focal blistering and intra-cartilaginous low-signal intensity area with an intact surface and base; grade 2, irregularities on the surface or base thickness < 50%; grade 3, deep ulceration with loss of thickness > 50%; grade 4, full-thickness cartilage wear with exposure of subchondral bone (Fig. 1 Patellar cartilage defect grade 0 (left), grade 2 (middle, arrow) and grade 3 (right, arrow)). Intra-observer and inter-observer reliability, expressed as ICCs, were 0.94 and 0.93, respectively [24]. Cartilage defects were considered to have: 1) ‘progressed’ if defect grade increased (i.e., worsened), 2) ‘regressed’ if the defect grade decreased (i.e., improved), or 3) ‘stable’ if defect grade did not change over 2 years.
Statistical analysis
Mean ± standard deviation was calculated for parametric variables, and changes over time were assessed using paired samples T-tests. Median ± interquartile range was calculated for non-parametric variables, and changes over time were assessed using Wilcoxon signed-rank tests. Participant characteristics were compared using independent samples T-tests or Chi-squared tests. Group-differences in annual percentage change in cartilage volume were compared using an analysis of covariance (ANCOVA) adjusting for the covariates of age, gender, BMI, baseline cartilage defect grade, and baseline patella bone volume. To explore between group differences in cartilage defect changes (i.e., progression and regression), Chi-squared and Fisher’s exact tests were used. If significant main effects were identified, post hoc comparisons were performed using Fisher’s least significant difference (LSD). Univariate and multivariate linear regression was used to examine the relationship between baseline cartilage defects and cartilage volume annual percentage change in all ACLR participants before and after adjusting for age, gender, BMI, baseline patella bone volume, and presence of meniscal pathology. All statistical analyses were performed in SPSS (IBM, Chicago, USA) version 24.0 with significance set to p < 0.05.
Results
As per our previous study [23], 66 participants returned for follow-up assessment (32 ACLR isolated, 25 ACLR combined, and 9 controls) and their characteristics are shown in Table 1. Between-group differences have been outlined previously [23] and included i) a higher BMI for the ACLR combined group compared to the ACLR isolated group (p = 0.007) and, ii) longer follow-up time interval between MRI assessments for the control group compared to both ACLR groups (p < 0.001). Reasons for drop-out have also been previously reported [23] and there was no significant difference in the characteristics of ACLR and control participants of those who completed follow-up assessment and those who did not (Supplementary File Table A1; Table A2).
Within-group comparisons
Cartilage volume
As shown in Table 2, mean patellar cartilage volume increased in both the ACLR isolated group [mean change (95% confidence interval, CI) 220 (139, 301) mm3] and the ACLR combined group [126 (26, 226) mm3] while the control group showed no significant change over follow up period [9 (− 165, 183) mm3].
Cartilage defects
ACLR isolated group showed a decrease in patellar cartilage defect scores (p = 0.02; Z = − 2.33; r = 0.3; Supplementary File Table A3).
Between-group comparisons
Cartilage volume
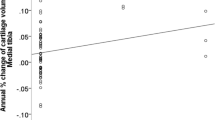
The ACLR isolated group had greater annual percentage change in cartilage volume than the control group (p = 0.008, mean difference 3.6, 95% CI 1.0, 6.3%) and ACLR combined group (p = 0.028, mean difference 2.2, 95% CI 0.2, 4.2%). However, no significant differences were found between the ACLR combined and control groups (Table 2). The same finding was observed in the adjusted annual changes in patellar cartilage volume (Fig. 2 Adjusted annual changes of cartilage volume in the three groups. * Significant difference (p < 0.05)).
Cartilage defects
Most participants in each group exhibited stable cartilage defects (Table 3). Although ACLR groups showed cartilage defect regression in a quarter of participants (25% of ACLR isolated and 24% of ACLR combined), no significant difference was found.
Associations between baseline patellar cartilage defects and annual percentage change in patellar cartilage volume amongst ACLR groups
Among ACLR participants, baseline patellar cartilage defect score was positively associated with annual percentage patellar cartilage volume change in univariate analysis (regression coefficient (B) = 0.013; 95% CI 0.001, 0.026; p = 0.04). The significant association remained after adjustment for age, gender, BMI, baseline patella bone volume, and presence of meniscal pathology, where higher baseline patella cartilage defect score was associated with an increase in patellar cartilage volume over 2 years (B = 0.014; 95% CI 0.001, 0.027; p = 0.03).
Discussion
This longitudinal study examined changes in patellar cartilage morphologic features (i.e., cartilage volume and cartilage defects) in ACLR knees with or without combined meniscal pathology from 2.5 to 4.5 years post-surgery, as well as a control group assessed over 2 years. ACLR groups demonstrated an increase in patella cartilage volume whilst control participants exhibited no change over the study period. Moreover, the isolated ACLR group showed a higher level of patella cartilage volume increase than the combined ACLR and control groups. Patellar cartilage defect scores significantly regressed in the isolated ACLR group. Finally, in ACLR participants, a positive association was identified between baseline patellar cartilage defect scores and the increase in patellar cartilage volume over the 2-year study period.
Consistent with H1, both isolated and combined ACLR knees showed significant increases in patellar cartilage volume at follow-up compared to baseline, while the patellar cartilage volume of the control group exhibited no significant change. Increase in patellar cartilage volume in ACLR knees is consistent with results of several recent longitudinal studies that have also reported increased knee cartilage volume or thickness within 1–5 years post-ACLR [15,16,17, 23] - albeit in the TF joint compartments. These findings may be indicative of early OA development that where cartilage increases have been reported prior to cartilage loss and may be due to tissue hypertrophy, repair and swelling [15]. In contrast to the current study, Culvenor et al. [14] reported decreased PF cartilage thickness at 5-years following ACLR- a finding which, given the follow-up period, may be reflective of a more advanced stage of cartilage degeneration than the current study. In the early stages of cartilage degeneration, cartilage increase is suggestive of accelerated metabolism and increased water - an adaptive response to repair cartilage damage and withstanding mechanical load [27, 28]. Whilst identifying the biomechanical mechanisms contributing to patella cartilage increase are beyond the scope of this study, PFJ ‘underloading’ during running in a comparable cohort of ACLR patients has been reported [29]. Decreased PFJ loading has been associated with early degenerative changes in ACL-transected animals [30, 31]. In humans, a relationship between TF joint underloading and the development of early-onset TF osteoarthritis has been identified [32]. Clearly, the definitive biomechanical conditions that contribute to the pathogenesis of PFJ OA post-ACLR need to be the focus of future studies.
In contrast to H2, ACLR isolated knees exhibited a greater increase in annual percentage change in patella cartilage volume than the combined ACLR and control knees. Meniscectomy and meniscal injuries have been associated with a higher prevalence of TF and PF joint OA following ACLR [7, 33, 34]. For this reason, we hypothesised (H2) that combined ACLR knees would demonstrate more pronounced cartilage volume change compared to isolated ACLR and control knees. However, our results indicate the opposite, and no differences were found between combined ACLR and control knees. This unexpected finding may be related to the fact that degenerative changes occur across cartilage sub-regions at different rates. In this respect, Eckstein et al. [15] whilst adopting a different technique for quantifying cartilage morphology, reported concurrent TF cartilage thickening and thinning in different sub-regions within the same cartilage compartment in post-ACLR participants. It has been widely accepted that an increase in cartilage volume precedes cartilage thinning during the process of cartilage degeneration [28]. Overall cartilage morphology is a direct result of the balance between cartilage hypertrophy and loss.
The isolated ACLR group experienced greater patellar cartilage volume increase suggesting that, on balance, increasing cartilage volume was the predominant change across the plate sub-regions. In contrast, combined ACLR knees may have been undergoing a higher level of cartilage thinning in some sub-regions due to more rapid degeneration compared with isolated ACLR knees. This argument is also supported in the TF joint, as our previous research has demonstrated the same between-group difference in the lateral tibia [23].
Contrary to H1, the majority of participants in each of the three groups had stable cartilage defects meaning defect grades were unchanged between baseline and follow up assessment time points. The stability of the cartilage defects in both ACLR groups suggests that the cartilage defects persist from 2.5–4.5 years post-ACLR. This notion is supported by Potter et al. (2012) who found cartilage defects in all 40 patients at the time of ACL injury, and minimal subsequent change in cartilage defect size until ~ 7 years post injury, at which point there was a marked increase in defect [20]. It is likely that the increase at this latter time represents acceleration of the degenerative processes, and is consistent with the higher rates of OA development observed around this time period (i.e., over 10 years) post-injury [2, 4].
Notably and contrary to H1, patellar cartilage defect scores significantly regressed in the isolated ACLR group and 25% of knees exhibited improvements in PF cartilage defects from baseline to follow-up. These improvements seem to be independent of concurrent meniscal injury, as 24% of the combined ACLR knees also showed cartilage defect improvement. This finding is different from previous studies showing one-way progression of patellar cartilage defects from 2 to 11 years following ACLR [20, 35]. In support however, another study [36] demonstrated that in a relatively young (i.e., mean age of 45 years) cohort of 325 participants, largely without radiographic OA, 13% of participants showed improvement in patellar cartilage defects over two-year period [36]. Improvement in cartilage defects, due to cartilage synthesis or swelling, reflects an attempt to repair cartilage damage and withstand mechanical load [28]. The natural history of cartilage defects was also age-related. In older groups, improvement of cartilage defects appears to be less common. Specifically, in a study of 395 participants with mean age 62.7 years, 26% cartilage defects progressed at the patella over 3 years, with the majority of defects remaining stable, and defect improvement rarely occurring (~ 1% of participants) [37]. In another study of 86 healthy participants with a mean age of 57 years, approximately 36% had worsening in patellar cartilage defects, while approximately 18% improved over 2 years [38]. Moreover, a recent study reported that 17% of ACLR participants had cartilage defects or osteophytes in the PF joint and, as such, were categorised as exhibiting MRI-defined PF joint OA [6]. Although defining early OA is of great value [39], results of the current study suggest that the definition of early OA should be carefully selected. Specifically, using the presence of mild cartilage defects as a diagnostic criterion for early OA may be inappropriate in either research or clinical setting, considering the regression of cartilage defects in a substantial portion of ACLR patients.
Contrary to H2, there were no differences in changes in cartilage defects between the three groups. This lack of difference between groups may be attributable to the small change in cartilage defects over the 2-years, and/or the relatively small sample size with a lack of power to detect statistical differences.
In support of H3, higher baseline cartilage defect scores at the patella of ACLR participants were associated with greater patellar cartilage volume increases over the following 2 years. The positive relationship indicates that mildly disturbed cartilage homeostasis (i.e., ICRS 1–2 cartilage defects) was associated with cartilage adaptation, which may be indicative of early cartilage degeneration. The positive association between cartilage defects and increases in cartilage volume is consistent with our previous finding in the lateral tibia [22]. It is important to note that ACLR participants in this study were different from those included in previous studies which reported that more severe cartilage defects (i.e., ICRS 3–4) were associated with an increased likelihood of developing radiographic OA [33] and worse patient-report outcomes [40,41,42,43].
This study has several strengths. Firstly, this is the first study to compare the change in patellar cartilage morphology between ACLR participants with and without concomitant meniscal pathology. Secondly, in contrast to most other longitudinal studies, we included an age-matched control group for comparative purposes. By contrast, our study also has several limitations. Firstly, as outlined in our previous study [23], around half of the participants were lost to follow-up. Importantly, no difference in participant characteristics were identified between those participants who remained in the study and those lost to follow-up. Secondly, although gender was included as a covariate in our statistical comparisons, there was an unequal distribution of males and females in the three groups. Thirdly, the sample size was relatively small for the combined ACLR group and the control group, which could reduce the statistical power of the study [23].
Conclusions
Patellar cartilage hypertrophy was evident in ACLR participants with and without concomitant meniscal pathology at ~ 4.5 years post-surgery. However, it may be inferred that patellar cartilage degenerative changes occur at different rates given the more pronounced increase in patellar cartilage volume in the ACLR isolated group compared to the ACLR combined group. Cartilage defects were stable in the majority of ACLR participants; however, the severity of patellar cartilage defects at baseline influenced the cartilage hypertrophic response over the subsequent ~ 2 years. Future studies should investigate the relationship between patellar cartilage morphology and gait-related patellofemoral contact forces in the early years following ACLR.
Availability of data and materials
The datasets used and analysed in the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
Anterior cruciate ligament
- ACLR:
-
Anterior cruciate ligament reconstruction
- ANCOVA:
-
Analysis of covariance
- BMI:
-
Body mass index
- CI:
-
Confidence Interval
- ICCs:
-
Intra-class correlation coefficients
- ICRS:
-
International Cartilage Repair Society
- IUD:
-
Intrauterine device
- LSD:
-
Least significant difference
- MRI:
-
Magnetic resonance imaging
- OA:
-
Osteoarthritis
- PF:
-
Patellofemoral
- TF:
-
Tibiofemoral
References
Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–69.
Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, Back D, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42:2242–52.
Chalmers PN, Mall NA, Moric M, Sherman SL, Paletta GP, Cole BJ, et al. Does ACL reconstruction alter natural history?: a systematic literature review of long-term outcomes. J Bone Joint Surg Am. 2014;96:292–300.
Claes S, Hermie L, Verdonk R, Bellemans J, Verdonk P. Is osteoarthritis an inevitable consequence of anterior cruciate ligament reconstruction? A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1967–76.
Culvenor AG, Lai CC, Gabbe BJ, Makdissi M, Collins NJ, Vicenzino B, et al. Patellofemoral osteoarthritis is prevalent and associated with worse symptoms and function after hamstring tendon autograft ACL reconstruction. Br J Sports Med. 2014;48:435–9.
Culvenor AG, Collins NJ, Guermazi A, Cook JL, Vicenzino B, Khan KM, et al. Early knee osteoarthritis is evident one year following anterior cruciate ligament reconstruction: a magnetic resonance imaging evaluation. Arthritis Rheumatol. 2015;67:946–55.
Keays SL, Newcombe PA, Bullock-Saxton JE, Bullock MI, Keays AC. Factors involved in the development of osteoarthritis after anterior cruciate ligament surgery. Am J Sports Med. 2010;38:455–63.
Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37:1434–43.
Arno S, Hadley S, Campbell KA, Bell CP, Hall M, Beltran LS, et al. The effect of arthroscopic partial medial meniscectomy on tibiofemoral stability. Am J Sports Med. 2013;41:73–9.
Netravali NA, Giori NJ, Andriacchi TP. Partial medial meniscectomy and rotational differences at the knee during walking. J Biomech. 2010;43:2948–53.
Culvenor AG, Cook JL, Collins NJ, Crossley KM. Is patellofemoral joint osteoarthritis an under-recognised outcome of anterior cruciate ligament reconstruction? A narrative literature review. Br J Sports Med. 2013;47:66–70.
Eckstein F, Cicuttini F, Raynauld JP, Waterton JC, Peterfy C. Magnetic resonance imaging (MRI) of articular cartilage in knee osteoarthritis (OA): morphological assessment. Osteoarthr Cartil. 2006;14:46–75.
Van Ginckel A, Verdonk P, Witvrouw E. Cartilage adaptation after anterior cruciate ligament injury and reconstruction: implications for clinical management and research? A systematic review of longitudinal MRI studies. Osteoarthr Cartil. 2013;21:1009–24.
Culvenor AG, Eckstein F, Wirth W, Lohmander LS, Frobell R. Loss of patellofemoral cartilage thickness over 5 years following ACL injury depends on the initial treatment strategy: results from the KANON trial. Br J Sports Med. 2019;53:1168–73.
Eckstein F, Wirth W, Lohmander LS, Hudelmaier MI, Frobell RB. Five-year followup of knee joint cartilage thickness changes after acute rupture of the anterior cruciate ligament. Arthritis Rheumatol. 2015;67:152–61.
Frobell RB, Le Graverand MP, Buck R, Roos EM, Roos HP, Tamez-Pena J, et al. The acutely ACL injured knee assessed by MRI: changes in joint fluid, bone marrow lesions, and cartilage during the first year. Osteoarthr Cartil. 2009;17:161–7.
Frobell RB. Change in cartilage thickness, posttraumatic bone marrow lesions, and joint fluid volumes after acute ACL disruption: a two-year prospective MRI study of sixty-one subjects. J Bone Joint Surg Am. 2011;93:1096–103.
Ding C, Garnero P, Cicuttini F, Scott F, Cooley H, Jones G. Knee cartilage defects: association with early radiographic osteoarthritis, decreased cartilage volume, increased joint surface area and type II collagen breakdown. Osteoarthr Cartil. 2005;13:198–205.
Bekkers JE, Inklaar M, Saris DB. Treatment selection in articular cartilage lesions of the knee: a systematic review. Am J Sports Med. 2009;37(Suppl 1):148s–55s.
Potter HG, Jain SK, Ma Y, Black BR, Fung S, Lyman S. Cartilage injury after acute, isolated anterior cruciate ligament tear: immediate and longitudinal effect with clinical/MRI follow-up. Am J Sports Med. 2012;40:276–85.
Wluka AE, Ding C, Jones G, Cicuttini FM. The clinical correlates of articular cartilage defects in symptomatic knee osteoarthritis: a prospective study. Rheumatology. 2005;44:1311–6.
Roemer FW, Kwoh CK, Hannon MJ, Green SM, Jakicic JM, Boudreau R, et al. Risk factors for magnetic resonance imaging-detected patellofemoral and tibiofemoral cartilage loss during a six-month period: the joints on glucosamine study. Arthritis Rheum. 2012;64:1888–98.
Wang X, Bennell KL, Wang Y, Wrigley TV, Van Ginckel A, Fortin K, et al. Tibiofemoral joint structural change from 2.5 to 4.5 years following ACL reconstruction with and without combined meniscal pathology. BMC Musculoskelet Disord. 2019;20:312.
Wang X, Wang Y, Bennell KL, Wrigley TV, Cicuttini FM, Fortin K, et al. Cartilage morphology at 2-3 years following anterior cruciate ligament reconstruction with or without concomitant meniscal pathology. Knee Surg Sports Traumatol Arthrosc. 2017;25:426–36.
Cicuttini F, Forbes A, Morris K, Darling S, Bailey M, Stuckey S. Gender differences in knee cartilage volume as measured by magnetic resonance imaging. Osteoarthr Cartil. 1999;7:265–71.
Hellio Le Graverand MP, Buck RJ, Wyman BT, Vignon E, Mazzuca SA, Brandt KD, et al. Change in regional cartilage morphology and joint space width in osteoarthritis participants versus healthy controls: a multicentre study using 3.0 tesla MRI and Lyon-schuss radiography. Ann Rheum Dis. 2010;69:155–62.
Sandy JD, Adams ME, Billingham ME, Plaas A, Muir H. In vivo and in vitro stimulation of chondrocyte biosynthetic activity in early experimental osteoarthritis. Arthritis Rheum. 1984;27:388–97.
Madry H, Luyten FP, Facchini A. Biological aspects of early osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2012;20:407–22.
Sritharan P, Schache AG, Culvenor AG, Perraton LG, Bryant AL, Crossley KM. Between-limb differences in patellofemoral joint forces during running at 12 to 24 months after unilateral anterior cruciate ligament reconstruction. Am J Sports Med. 2020;48:1711–9.
Hasler EM, Herzog W. Quantification of in vivo patellofemoral contact forces before and after ACL transection. J Biomech. 1998;31:37–44.
Herzog W, Adams ME, Matyas JR, Brooks JG. Hindlimb loading, morphology and biochemistry of articular cartilage in the ACL-deficient cat knee. Osteoarthr Cartil. 1993;1:243–51.
Wellsandt E, Gardinier ES, Manal K, Axe MJ, Buchanan TS, Snyder-Mackler L. Decreased knee joint loading associated with early knee osteoarthritis after anterior cruciate ligament injury. Am J Sports Med. 2016;44:143–51.
Li RT, Lorenz S, Xu Y, Harner CD, Fu FH, Irrgang JJ. Predictors of radiographic knee osteoarthritis after anterior cruciate ligament reconstruction. Am J Sports Med. 2011;39:2595–603.
Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M. Patellofemoral osteoarthritis 15 years after anterior cruciate ligament injury--a prospective cohort study. Osteoarthr Cartil. 2009;17:284–90.
Lee YS, Jeong YM, Sim JA, Kwak JH, Kim KH, Nam SW, et al. Specific compartmental analysis of cartilage status in double-bundle ACL reconstruction patients: a comparative study using pre- and postoperative MR images. Knee Surg Sports Traumatol Arthrosc. 2012;27:1–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4349643/.
Ding C, Cicuttini F, Scott F, Cooley H, Boon C, Jones G. Natural history of knee cartilage defects and factors affecting change. Arch Intern Med. 2006;166:651–8.
Carnes J, Stannus O, Cicuttini F, Ding C, Jones G. Knee cartilage defects in a sample of older adults: natural history, clinical significance and factors influencing change over 2.9 years. Osteoarthr Cartil. 2012;20:1541–7.
Wang Y, Ding C, Wluka AE, Davis S, Ebeling PR, Jones G, et al. Factors affecting progression of knee cartilage defects in normal subjects over 2 years. Rheumatology (Oxford). 2006;45:79–84.
Conaghan PG, Kloppenburg M, Schett G, Bijlsma JW. Osteoarthritis research priorities: a report from a EULAR ad hoc expert committee. Ann Rheum Dis. 2014;73:1442–5.
Shelbourne KD, Gray T. Results of anterior cruciate ligament reconstruction based on meniscus and articular cartilage status at the time of surgery: five- to fifteen-year evaluations. Am J Sports Med. 2000;28:446–52.
Shelbourne KD, Jari S, Gray T. Outcome of untreated traumatic articular cartilage defects of the knee: a natural history study. J Bone Joint Surg Am. 2003;85-A(Suppl 2):8–16.
Rotterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Aroen A. Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med. 2013;41:535–43.
Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42:1058–67.
Acknowledgements
We appreciate all the participants in the study.
Funding
This work was supported by the National Health and Medical Research Council (NHMRC, project grant 628850). YW is the recipient of an NHMRC Career Development Fellowship (Clinical level 1, #1065464). KB is the recipient of a NHMRC Principal Research Fellowship (#1058440). AVG is the recipient of a FWO (Pegasus)2 EU Marie Sklodowska Curie Fellowship (Horizon 2020, grant number 665501). ALB is the recipient of a NHMRC Career Development Fellowship (#1053521). The funding source had no role in the: study design; collection, analysis and interpretation of data; in the writing of the manuscript; and in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
All authors were involved in revising it critically for intellectual content. Study conception and design: XW, ALB, KLB, YW, TVW, FMC, DGL. Provision of patients: JAF, CJV, TW, PG. Acquisition of the data: KF, DJS, XW, BAK. Analysis and interpretation of data: XW, YW, KLB, ALB, AVG, FMC. Draft of the paper: XW, BAK, ALB, DJS, KF. Revision of paper: XW, ALB. Obtaining of funding: ALB, KLB, TVW, FMC, DGL. Final approval of the article: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All research studies have been performed according to the rules of the local ethics committee. The University of Melbourne and Griffith University Human Research Ethics Committees approved the study (0932864.3 and PES/36/10/HREC, respectively). Informed written consent was obtained from participants for research studies and presented data.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table A1. Characteristics of ACLR participants who completed the study and those who were lost to follow-up. Table A2. Characteristics of control participants who completed the study and those who were lost to follow-up.
Additional file 2
: Table A3. Median (IQR) baseline and follow-up patellar cartilage defect score with pre-post Wilcoxon test in each group.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, X., Bennell, K.L., Wang, Y. et al. Patellar cartilage increase following ACL reconstruction with and without meniscal pathology: a two-year prospective MRI morphological study. BMC Musculoskelet Disord 22, 909 (2021). https://doi.org/10.1186/s12891-021-04794-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-021-04794-5