Abstract
Background
Anatomical variations of the attachment of medial meniscus are a common finding. However, anomalies of the posterior horn are extremely rare. Only two cases of posterior root anomaly have been described prior to the routine use of arthroscopy for evaluation and treatment of meniscal pathology. In this report, we present an anomaly of both the anterior and posterior roots of the medial meniscus that posed both a diagnostic and therapeutic dilemma.
Case presentation
The patient is young male soccer player who is currently 16 years of age and began having the atraumatic onset of pain and symptoms that limited performance starting at age 14 and was referred for failure of response to nonoperative treatment. Diagnostic arthroscopy revealed the presence of an anteromedial meniscofemoral ligament whereas the posterior root showed no bony attachment. The radiographic and arthroscopic findings are described. The clinical decision was made after to proceed with observation, reassurance, and gradual return to full activity with physiotherapy guidance.
Discussion and conclusion
The absence of injury, the mild complaints reported by the patient, his age, skeletal immaturity, and remaining growth led us to adopt a conservative approach to treating this anatomic variant and currently the patient is able to participate fully in sports without symptoms or restrictions.
Similar content being viewed by others
Background
Anomalies of the medial meniscus are rare compared with those of the lateral meniscus. They include discoid variants, hypoplasia of anterior horn, and anomalous attachment of the anterior horn. Usually, the most common anomaly of medial meniscus is related to the anterior insertion that often shows anatomic variability [1,2,3]. However, anomalous attachment of posterior horn has been reported in only two cases [4, 5]. In the first case [4], the authors described the presence of a fibro-cartilaginous fold covering the medial femoral condyle. The posterior horn was described as normal. In the second case [5], the authors described the presence of a fibrous band arising from the posterior horn and inserting to femoral insertion of the ACL. Both cases were described prior to the common use of arthroscopy. Recently, Sadigursky et al. [6] reported a case of abnormality in medial and lateral posterior horns. We present the first report of an anomaly of both the anterior and posterior roots of the medial meniscus, documented by MRI and confirmed by arthroscopy.
Case presentation
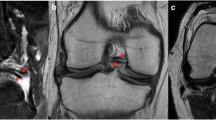
A 14-year old male soccer player was referred to our orthopedic tertiary care referral facility as a result of failure to respond to non-operative management. He first experienced pain on the medial side two years prior that was noted after sports activities although no clear injury was identified. The knee was intermittently painful and with time these symptoms progressively worsened despite several attempts at non-operative management to include anti-inflammatories and physical therapy. The symptoms limited the ability of the patient to participate in sports. Physical examination revealed no effusion, complete range of motion, and no signs of meniscal pathology. There was no tenderness to palpation of the medial or lateral joint line, a negative McMurray, and a normal ligamentous examination. There was no pain with hyperextension, and the only positive examination finding was mild pain on hyperflexion. Radiographs were normal. Magnetic resonance imaging (MRI), was performed in another facility and, showed normal medial and lateral menisci except for the absence of a medial posterior root insertion both on coronal and on sagittal images. There was no evidence of meniscal extrusion or a meniscal ghost sign (Fig. 1). On sagittal magnetic resonance images, the presence of thin low-signal band was identified just anterior to the ACL (Fig. 2). Diagnostic arthroscopy was performed secondary to failure of nonoperative management and revealed a white rounded band that was noted to extend from the anterior horn of the medial meniscus to the intercondylar notch adjacent to the femoral insertion of the ACL (Fig. 3A). This band was clearly a distinct structure from the ACL with probing. Next careful examination of medial compartment revealed that the meniscus did not have evidence of tearing or degenerative changes and appeared to be floating into the medial compartment without the typical anterior bony attachment. The posterior horn showed absence of any firm bony attachment as well. Some fibers were detected below the anterior aspect of posterior cruciate running towards the lateral compartment (Fig. 3B). No chondral pathology was detected. Because of absence of meniscal lesions or other intrarticular abnormalities, we elected close observation rather than surgical intervention. The patient made rapid recovery after diagnostic arthroscopy and returned to his soccer activity after 2 months without any pain, discomfort, or limitation of activity. At 4-year follow-up, he had no symptoms or abnormal findings and he was still playing soccer at a youth competitive level. On the follow-up MRI there no meniscal or chondral lesions and no significative change of the appearance of the meniscal roots from the index MRI.
Arthroscopic finding of the left knee joint. In (A) view of anterior horn and the probe indicates the presence of anterior meniscofemoral ligament whereas on the back it is visible the posterior horn (ph) present but raised up for absence of bony attachment. In (B) detail of posterior root with presence of some fibrous tissue connecting the posterior horn to posterior cruciate ligament and a thin band below the undersurface of the meniscus (arrow)
Discussion and conclusion
There were two different challenges that needed to be addressed in treating this patient. The first one was the diagnostic issue secondary to the vague and nonspecific symptoms of the patient and lack of clear identifiable objective pathology. The only positive finding was the presence of an anomalous anterior horn insertion on MRI scan. The anatomy of the anterior meniscal root has been described by Berlet and Fowler [1]: they distinguished four different types, three with bony insertion and the fourth type inserting into the soft type (intermeniscal ligament). In addition to differences of anatomical insertions of anterior medial meniscus horn, in 1993 McCormack and McGrath [7] described a further type of the anterior horn attachment without bony insertion but with a strong ligament-like tissue attachment to the posterolateral wall of the femoral intercondylar fossa, covering the anterior portion of the ACL. They named this anomaly as the anteromedial meniscofemoral ligament (AMMFL). Following this first report, many other observations of this anatomical variant have been described [8,9,10,11,12]. The true incidence of AMMFL is not yet known. Rainio et al. [13] reported an incidence of 1.2 % in 987 consecutive arthroscopies. Cha et al. [14] in a cohort of 1,326 arthroscopic examinations reported the incidence to be 2.3 %. More recently, Kim and Joo [15] have reported that in their patient population, the presence of AMMFL was detected only in 0.5 % of cases. The ability of the MR scan to detect an anomalous insertion of the medial meniscus is challenging [16] with a 74 % false-positive rate for anterior horn tears [17]. Moreover, the AMMFL may easily be confused as fibers of the ACL [18]. The senior author has performed over 4000 arthroscopies in the past 20 years and only identified 0.3 % which is consistent with published literature. In all cases described in the literature, the AMMFL was an incidental finding and its clinical significance remains unknown. The symptoms are often vague and often referred to the anterior knee. The cause of symptoms is hypothesized to be related to impingement against the femoral condyle [19] or to abnormal mobility of the anterior horn that may predispose the meniscus to a possible rupture or to progressive degeneration [7]. The pain is often reported after athletic activity, but a clear traumatic incident is seldom reported.
In our case, the diagnostic dilemma was complicated by the concomitant lack of attachment of the posterior horn of the meniscus to the tibia. On index MRI, because of presence of an intact posterior horn, the classic signs of meniscal root pathology, such as meniscal extrusion or meniscus ghost, were absent. When probed, it was possible to detect only few fibers running in front of the anterior portion of posterior cruciate ligament toward the posterior horn of the lateral meniscus. These fibers could be interpreted as a rare posterior transverse ligament or meniscomeniscal ligament [20]. Apart from these fibers, no other bands or anomalies of the posterior horn were detected. In the literature, anomalous attachment of the posterior horn is extremely rare and only two cases have been reported. In 1963 Riach and Phares [4] described a case in which the posterior horn continued through a fold to cover the articular surface of the medial femoral condyle. In 1998, Bhagava and Ferrari [5] described a case of an anomalous band from the posterior horn area of the medial meniscus to insert into the midportion of anterior cruciate ligament.
For this particular patient, the main problem we faced was the choice of treatment given the intermittent symptoms. Generally, an AMMFL does not seem to be related to knee symptoms, and because is often an incidental finding it may be left in situ. However, in some reports, the ligament has been cut and removed with reported improvement of symptoms [13, 19, 21, 22]. It is our opinion that is difficult to support resection as an option in a young patient with remaining growth given the lack of consensus in the literature. We agree with other authors who consider the AMMFL to have a biomechanical effect as a ligamentous anchor of the anterior horn [10, 15]. In our particular case, where a combined anomaly of both horns was present, the AMMFL was the only meniscal attachment. Therefore, to remove this isolated fibrous insertion could potentially increase hypermobility of the medial meniscus and therefore be counterproductive.
Because of the young age of our patient with open physes there were potential deleterious effects that could result from the absence of definitive attachment of anterior or posterior horn. The absence of injury, the mild complaints reported by the patient, his age, skeletal immaturity, and remaining growth led us to adopt a conservative approach to treating this anatomic variant. At the present time, the patient still actively practices and competes in soccer with no symptoms that limit participation.
Availability of data and materials
No dataset analysis was carried out for the current study. Clinical and radiological reports are available from the corresponding author on reasonable request.
Abbreviations
- ACL:
-
anterior cruciate ligament.
- MRI:
-
magnetic resonance images.
- AMMFL:
-
anteromedial meniscofemoral ligament.
References
Berlet GC, Fowler PJ. The anterior horn of the medial meniscus. An anatomical study of its insertion. Am J Sports Med. 1998;26:540–3.
Ryu K, Iriuchishima T, Oshida M, Saito M, KatoY, Tokuhashi Y, Aizawa S. Evaluation of the morphological variations of the meniscus: a cadaver study. Knee Surg Sports Traumatol Arthrosc. 2015;23:15–9.
Ohkoshi Y, Takeuchi T, Inoue C, Hashimoto T, Shigenobu K, Yamane S. Arthroscopic studies of variants of the anterior horn of the medial meniscus. Arthroscopy. 1997;13:725–30.
Riachi A, Phaires A. An unusual deformity of the medial semilunar cartilage. J Bone Joint Surg Br. 1993;45:146–7.
Bhagava A, Ferrari DA. Posteromedial meniscus-femoral insertion into the anterior cruciate ligament. A case report. Clin Orthop Rel Res. 1998;348:176–9.
Sadigursky D, Garcia LC, Martins RR, De Queiroz GC, Carneiro RJF, Colavolpe PO. Anatomical variant of the meniscus related to posterior junction: a case report. J Med Case Rep. 2017;18:11. DOI https://doi.org/10.1186/13256-017-1512-z.
McCormack D, McGrath J. Antero-medial menisco-femoral ligament. Clin Anat. 1992;5:485–7.
Anderson AF, Awh MH, Anderson CN. The anterior meniscofemoral ligament of the medial meniscus. Case series. Am J Sports Med. 2004;32:1035–40.
Nagashima M, Otani T, Takeshima K, Seki H, Ishii K. Arthroscopy Sports Med Rehab. 2020;2:e1–6.
Wang JH, Wong AK, Romanowski JR, Fu FH. Meniscus tear developed by pulling of the anomalous insertion of medial meniscus on anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2011;19:1689–92.
Jung YB, Yum JK, Bae YJ, Song KS. Anomalous insertion of the medial menisci. Arthroscopy. 1998;14:505–7.
Tan K, Yoong P, Toms AP. Normal anatomical variants of the menisci and cruciate ligaments that may mimic disease. Clin Radiol. 2014;69:1178–85.
Raino P, Sarimo J, Rantanen J, Alanen J, Orava S. Observation of anomalous insertion of the medial meniscus on the anterior cruciate ligament. Arthroscopy. 2002;18:202-E9.
Cha JG, Min KD, Han JK, Hong HS, Park SJ, Park JS, Paik SH. Anomalous insertion of the medial meniscus into the anterior cruciate ligament: the MRI appearance. Br J Radiol. 2008;81:20–4.
Kim YM, Joo YB. Anteromedial meniscofemoral ligament of the anterior horn of the medial meniscus: clinical magnetic resonance imaging, and arthroscopic features. Arthroscopy 20018;34:1590–1600.
Liu YW, Skalski MR, Patel DB, White EA, Tomasian A, Matcuk GR Jr. The anterior knee: normal, common pathology, and diagnostic pitfalls on MRI. Skeletal Radiol. 2018;47:1069–86.
Shepard MF, Hunter DM, Davies MR, Shapiro MS, Seeger LL. The clinical significance of anterior horn meniscal tears diagnosed on Magnetic Resonance Images. Am J sports Med. 2002;30:189192.
Coulier B, Himmer O. Anteromedial meniscofemoral ligament of the knee: CT and MRI features in 3 cases. JBR-BTR. 2008;91:240–4.
Santi MD, Richardson AB. Bilaterally painful anomalous insertion of the medial meniscus in a volleyball player with Marfanoid features. Arthroscopy. 1993;9:217–9.
Chan CM, Goldblatt JP. Unilateral meniscomeniscal ligament. Orthopaedics. 2012;35:e1815-7.
Shea KG, Westin C, West J. Anomalous insertion of the medial meniscus of the knee. J Bone Joint Surg Am. 1995;77:1894–6.
Soejima T, Murakami H, Tamaka N, Nagata K. Anteromedial meniscofemoral ligament. Case report. Arthroscopy. 2003;19:90–5.
Nakajima T, Nabeshima Y, Fujii H, Ozaki A, Muratsu H, Yoshiya S. Symptomatic anomalous insertion of the medial meniscus. Case report. Arthroscopy 2005;21:629.e1-629.e4.
Acknowledgements
not applicable.
Funding
not applicable.
Author information
Authors and Affiliations
Contributions
PPM and MJB treated the patient, collected the data and wrote the manuscript. GT edited the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate:
Not applicable for observational case report.
Consent for publication
written consent was obtained from the patient’s parent for publication of this case report and any accompanying images. A copy of written consent is available for review.
Competing interest
The authors declare that they have not competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mariani, P.P., Battaglia, M.J. & Torre, G. Anomalous insertion of anterior and posterior horns of medial meniscus. Case report. BMC Musculoskelet Disord 22, 823 (2021). https://doi.org/10.1186/s12891-021-04696-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-021-04696-6